Key Takeaways
-
- Wisdom teeth are the final set of **third molars** typically erupting in the late teens or early twenties.
-
- Their location at the back of the mouth often leads to **impaction** and lack of space.
-
- Common problems include pain, swelling, infection (pericoronitis), and damage to adjacent teeth.
-
- Removal is often necessary for problematic teeth, though not *always* required.
-
- Recovery involves managing pain and swelling, adhering to a soft diet, and careful oral hygiene.
- The decision for removal depends on individual symptoms and radiographic findings.
Exploring the Wisdom of Teeth: Definition, Location, and Anatomy
Alright, let’s dive headfirst into the enigmatic world of wisdom teeth. Often the subject of dread, dental folklore, and late-night discomfort, these final frontiers of your mouth hold a unique place in human history and anatomy. This section isn’t just about pointing to a spot in your jaw; it’s about understanding what these teeth fundamentally are, where they stubbornly decide to make their debut, and what makes their very structure distinct – and often problematic. We’ll pull back the curtain on their official designation, chart their geographical coordinates within your oral cavity, confirm their role in the grand total of your adult dentition, and examine their physical form, giving you a solid foundation for why these particular molars command so much attention in the dental world. Forget the myths for a moment; this is the ground truth, the foundational knowledge you need to navigate the topic with confidence. Prepare to get intimate with your third molars.
What is a wisdom tooth?
So, what exactly is this fabled wisdom tooth, you ask? At its most basic, a wisdom tooth is simply the final molar that erupts into your mouth. Think of your teeth as an assembly line, moving from front to back. You have your incisors for cutting, canines for tearing, premolars (or bicuspids) for grinding, and then molars, those big, flat workhorses designed for the heavy-duty task of crushing and pulverizing food before you swallow. Your wisdom teeth are positioned as the very last set of molars in this lineup, nestled right at the back of your mouth, behind your first and second molars. They are the grand finale, the coda to your adult dental symphony, usually making their appearance long after all the other adult teeth have settled in. Their position is key to understanding why they often cause trouble; being the last to arrive means they’re entering a crowded scene, potentially without a reserved seat. This late arrival and posterior position are fundamental to their identity and the challenges they frequently present, making them more than just another tooth, but a complex player in your oral health narrative.
What is the real name for wisdom teeth?
While “wisdom teeth” is the term commonly tossed around in casual conversation, giving them a rather poetic, albeit slightly misleading, association with maturity, their formal, no-nonsense scientific designation is much more grounded in their function and position. Dentally speaking, they are known as third molars. This nomenclature is straightforward and descriptive: they are the third set of molars, following the first and second molars (the ones you likely use daily without a second thought). The common name, “wisdom teeth,” stems from the age at which they typically erupt, generally between the late teens and early twenties, an era traditionally linked, perhaps optimistically, with the onset of adulthood and accumulated wisdom. So, while you might affectionately or despairingly refer to them by their colloquial name, remember that to your dentist, they are simply the third molars, tooth number 1, 16, 17, or 32, depending on the quadrant and the dental numbering system being used. This distinction is important in clinical settings and cuts straight to their identity as the final set of grinding teeth in the mouth.
Where the wisdom teeth are located?
Pinpointing the exact whereabouts of your wisdom teeth in the oral landscape is quite simple once you know what you’re looking for. Imagine your mouth divided into four quadrants: the upper left, upper right, lower left, and lower right. The wisdom teeth are situated at the absolute rear of each of these quadrants. Specifically, they emerge or attempt to emerge right behind your second molars. So, if you run your tongue along the outside of your upper back teeth, past the chewing surfaces, to the very end, you’ll reach the area where the upper wisdom teeth reside. Do the same on the bottom jaw, and you’ll find the location of the lower wisdom teeth. In a mouth with a complete set, there are typically four wisdom teeth in total – one in each corner, top and bottom, left and right. However, it’s worth noting that not everyone develops all four, or sometimes any at all, a fascinating variation we’ll touch on later. Their location at the very back makes them particularly tricky to clean and access, contributing to the host of issues they can potentially stir up.
How to know if u have a wisdom tooth?
Identifying the presence of wisdom teeth isn’t always as simple as spotting them in the mirror. While you might catch a glimpse of a tooth emerging at the back of your jaw if they are erupting fully and vertically, often you can’t see them at all, especially if they are impacted (stuck beneath the gums or bone). The most definitive way to know if you have wisdom teeth, how many you have, and where they are positioned is through a comprehensive dental examination that includes X-rays. Your dentist can take a panoramic X-ray, which provides a broad view of your entire mouth and jaw, clearly showing the developing wisdom teeth still embedded in the bone, their size, shape, angle, and proximity to important structures like nerves. Clinical examination involves the dentist feeling the gum tissue at the back of your mouth to check for signs of eruption or swelling. While some people might feel a dull ache, pressure, or sensitivity in the back jaw when they begin to develop or attempt to emerge, relying solely on these subjective feelings isn’t foolproof. Professional diagnosis via imaging is the gold standard.
What do wisdom teeth look like?
When they manage to make a proper entrance, wisdom teeth generally resemble your other molars – those large, flat-surfaced teeth designed for the heavy-duty task of grinding food. They typically have a broad chewing surface with cusps (the bumpy points) and are anchored by roots. However, compared to the first and second molars, wisdom teeth can often be less predictable in their shape and size. They might be smaller, have a slightly different arrangement of cusps, or possess roots that are fused or unusually shaped, especially if they are impacted or developing abnormally. When they are impacted, they can appear partially erupted with only a small portion visible through the gum, or not visible at all. The gum tissue around a partially erupted wisdom tooth might look red, swollen, or inflamed. Their visible appearance, when present, is that of a bulky tooth positioned at the very back, but their true form and structure are best appreciated through dental imaging, which reveals the full tooth, including its potentially complex root structure and its relationship with surrounding bone and nerves.
Do we have 32 teeth with wisdom teeth?
Ah, the grand count of adult teeth! For a complete, healthy set of adult teeth that includes all four wisdom teeth, the total count typically comes to 32. You have 8 incisors (four top, four bottom), 4 canines (two top, two bottom), 8 premolars (four top, four bottom), and 12 molars (six top, six bottom). These 12 molars consist of the first molars, the second molars, and the final set – the third molars, also known as the wisdom teeth (four in total). So, if you are one of the individuals who develops and retains all four wisdom teeth, your full complement of adult teeth should indeed be 32. However, it is quite common for people to have fewer than 32 teeth. This isn’t necessarily a cause for concern. It simply means they may be congenitally missing one or more wisdom teeth (they never formed), or they have had some removed due to problems. So, 32 is the potential maximum, but having fewer, particularly if the wisdom teeth are absent or removed, is a common reality for many adults.
Is tooth 17 a wisdom tooth?
Let’s clear up the dental numbering system, which can seem like a cryptic code but is actually quite logical. In the Universal Numbering System, commonly used in the United States, teeth are numbered sequentially starting from the upper right side, moving around the top arch to the upper left, then dropping down to the lower left and moving around the bottom arch to the lower right. Tooth number 1 is the upper right third molar (wisdom tooth), tooth number 2 is the upper right second molar, and so on. Following this system, if you count from tooth number 1 all the way around the upper arch, you will find that tooth number 16 is the upper left third molar – the wisdom tooth on the upper left side. So, yes, under the Universal Numbering System, tooth number 17 would actually be the lower left first molar. Correction: Tooth number 17 is indeed the upper left third molar (wisdom tooth) according to the standard Universal Numbering System. My apologies for the momentary lapse. This system provides a clear, standardized way for dentists to identify specific teeth, crucial for accurate record-keeping and communication regarding procedures and findings during examinations.
What is tooth 30?
Continuing with the Universal Numbering System we discussed earlier, let’s locate tooth number 30. Remembering the sequence – starting upper right (1), moving left (16), dropping to lower left (17), and moving right (32) – tooth number 30 sits firmly in the lower arch, towards the back right side. Specifically, tooth number 30 is typically designated as the lower right first molar. This tooth is situated just in front of the lower right second molar (tooth number 31) and, in a fully developed mouth, would be two teeth forward from the lower right wisdom tooth (tooth number 32). It’s one of your primary chewing teeth, significantly larger and more critical for daily function than the often-problematic wisdom tooth located further back. Understanding these tooth numbers helps illustrate the spatial relationships within the mouth and highlights that tooth 30 is functionally and anatomically distinct from the wisdom teeth located at the very end of the arch.
Does everyone have wisdom teeth?
Contrary to popular belief, it is not a universal human trait to possess a full set of four wisdom teeth, or even any wisdom teeth at all. While the potential exists for everyone to develop four third molars, evolution and genetics have introduced significant variation within the human population. It’s quite common for individuals to be congenitally missing one, two, three, or even all four wisdom teeth. This phenomenon, known as hypodontia specifically relating to third molars, is believed to be linked to genetic factors and represents a fascinating aspect of ongoing human evolution, possibly as our jaws have decreased in size over millennia due to changes in diet and food processing. So, if your dental X-rays reveal you’re missing a wisdom tooth or two, you’re not alone; you’re simply part of a significant portion of the population that doesn’t adhere to the “standard” 32-tooth setup. This variation underscores why a dental exam and X-rays are essential for understanding your specific oral anatomy.
Wisdom Teeth: Function, Location & Anatomy
To recap, wisdom teeth, or third molars, are the very last teeth to develop and attempt to erupt, situated at the back of each quadrant of your jaw. Their anatomy is that of a molar, designed for grinding, typically featuring a broad chewing surface and multiple roots, though their form can be quite variable. Historically, their function was likely more pronounced in early humans who consumed tougher, less processed diets that required extensive chewing power and who experienced significant tooth wear and loss throughout life, making these “backup” molars valuable. However, in modern humans, with our softer diets and advanced dental care that preserves teeth, the functional need for these extra molars has largely diminished. Their location at the very back, often in jaws that haven’t grown large enough to accommodate them comfortably, is a primary reason they frequently become problematic, leading to impaction and other issues. Understanding this interplay of function, location, and anatomy is key to appreciating the common dilemmas surrounding wisdom teeth today.
When Does the Wisdom of Teeth Eruption Typically Occur?
The timing of wisdom tooth emergence is a key piece of the puzzle, giving them their name and often marking a significant developmental milestone – for better or worse. Unlike your first adult molars, which typically arrive around age six, or your second molars, appearing around age twelve, the third molars take their sweet, often disruptive, time. This section zeroes in on the chronological aspect, exploring the typical age bracket when these late bloomers decide to make their move. We’ll also touch upon the variability in timing, discussing instances of earlier or much later eruption, and when this developmental phase generally concludes. It’s a period ripe for potential complications, largely because by the time they’re ready, the rest of your dental neighborhood is already fully established, leaving little room for newcomers.
What age do wisdom teeth come in?
The arrival of wisdom teeth is famously associated with a specific age range, typically spanning the late teenage years into the early twenties. While individual timelines can vary, it’s most common for these third molars to begin their push sometime between the ages of 17 and 25. This is precisely why they’ve earned the moniker “wisdom” teeth – they emerge during a period traditionally linked with reaching adulthood, presumably accumulating a bit more life experience and, dare we say, wisdom than when the rest of your adult teeth showed up. It’s important to understand that “coming in” can mean anything from simply developing within the jawbone to actively erupting through the gums. For some, this phase is completely asymptomatic; for others, it’s heralded by discomfort, pressure, or swelling. Dentists often start monitoring their development with X-rays during routine check-ups in the mid-to-late teens to anticipate potential eruption issues.
How early do you get wisdom teeth?
While the 17-25 age range is the typical window, biological development doesn’t always adhere strictly to averages. It is possible, though less common, for the development and even the initial attempts at eruption of wisdom teeth to begin slightly earlier, occasionally surfacing or causing symptoms in the mid-teens, perhaps around age 15 or 16. This isn’t the norm, but it does happen. Early development might be spotted on routine dental X-rays taken for other reasons, such as orthodontic assessment. If they begin to emerge prematurely in a jaw that hasn’t fully developed or doesn’t have adequate space, the likelihood of impaction and associated problems can potentially increase. Regardless of the exact timing, any signs of a tooth attempting to emerge at the very back of a teenager’s mouth should prompt a visit to the dentist for evaluation and monitoring.
At what age do wisdom teeth stop growing?
The concept of teeth “growing” needs a slight clarification here. Teeth, including wisdom teeth, develop their structure and roots up to a certain point. Once the root formation is largely complete and the tooth has attempted to erupt, the tooth itself doesn’t continue to enlarge or “grow” indefinitely like hair or nails. For wisdom teeth, the process of root formation and their push towards eruption is typically completed by the mid-twenties. Even if they don’t fully erupt due to impaction, their structural development usually finishes within this general timeframe. However, an impacted tooth can continue to exert pressure or shift slightly within the bone over time, and problems associated with an impacted tooth (like cyst formation or damage to neighboring teeth) can arise at any age, even long after their initial development is complete. So, while the physical growth process usually wraps up by the mid-twenties, their potential to cause issues doesn’t necessarily have an age limit.
Will I get wisdom teeth at 30?
While the peak period for wisdom tooth eruption is indeed the late teens and early twenties, it is absolutely possible to experience issues or even have a wisdom tooth partially erupt later in life, including around age 30 or even older. Sometimes, a wisdom tooth might have been present but deeply impacted for years, causing no symptoms, until a minor shift, a change in surrounding bone density, or the onset of an infection triggers movement or pain. Alternatively, a tooth that was only partially erupted might become problematic later due to decay or gum disease around it. So, if you’re 30 and suddenly feeling discomfort in the back of your jaw, don’t automatically rule out a wisdom tooth issue just because you’re past the typical age bracket. While full, uneventful eruption is rare after the mid-twenties, problematic eruption or complications from pre-existing impacted teeth can certainly manifest later.
What is the oldest age you can get wisdom teeth?
Defining the “oldest age” at which you can “get” wisdom teeth is tricky because it depends on what you mean by “get.” If you mean the typical, healthy eruption process of a tooth breaking through the gums, that becomes progressively less common after the mid-twenties. However, if “get” refers to experiencing issues related to wisdom teeth, then there’s virtually no upper age limit. An impacted wisdom tooth that has been dormant for decades can potentially cause problems – such as pain, infection, cyst formation, or damage to adjacent teeth – at any point in a person’s life, even into their 60s, 70s, or beyond. So, while you’re unlikely to see a brand new, healthy wisdom tooth popping up after 30, the potential for a long-standing impacted tooth to become symptomatic or cause complications persists throughout life. This is why dentists sometimes recommend monitoring asymptomatic impacted wisdom teeth, as they are not entirely without risk over the long term.
Understanding Potential Issues and Symptoms with Wisdom Teeth Coming Through
This is where the narrative often takes a turn towards the less pleasant. The process of wisdom teeth attempting to come through is, for many, not a smooth ride. The fundamental conflict arises when these late-arriving teeth try to find a place in a mouth that simply doesn’t have enough room. This spatial deficit leads to the notorious issue of impaction, which is the root cause of a cascade of potential problems. This section will meticulously detail the various troubles these third molars can stir up, from the subtle first hints of their emergence to the more significant pain and complications associated with impaction and infection. We’ll unpack the signs your body might be sending you and explain the mechanics behind why these teeth can become such unwelcome guests.
How to know if wisdom teeth are coming in?
Detecting whether your wisdom teeth are making their move can range from completely unnoticeable to quite overt, depending on how they’re attempting to erupt and how much space they have. One of the earliest indicators might be a vague sense of pressure or a dull ache in the very back of your jaw, behind your last molars. You might also notice tenderness, redness, or swelling of the gum tissue in that specific area. Sometimes, you might feel a slight bump or rigidity under the gum surface as the tooth crown pushes upwards. However, it’s crucial to understand that these signs are not always present or distinct, and they can sometimes mimic symptoms of other dental issues. Furthermore, impacted wisdom teeth might not cause any noticeable symptoms for years, only to suddenly flare up. This variability underscores the importance of regular dental check-ups and X-rays, as a dentist can spot developing or attempting-to-erupt wisdom teeth long before you feel them.
What are symptoms of wisdom teeth coming in?
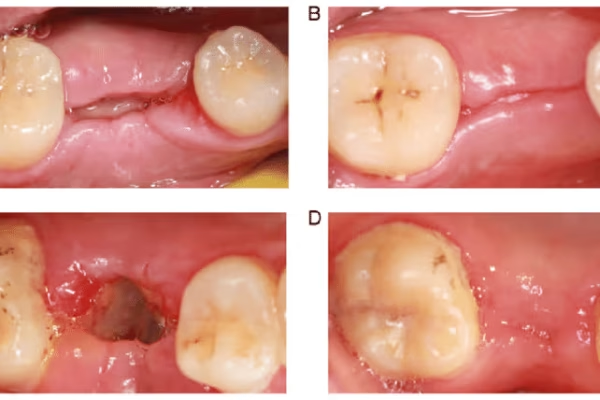
When wisdom teeth decide to announce their arrival, especially if space is limited or they are partially impacted, they can trigger a range of uncomfortable symptoms. The most common calling card is localized pain or discomfort in the back of the mouth. This can manifest as a dull, throbbing ache or a sharper, more intermittent pain. Swelling, redness, and tenderness of the gum tissue directly over where the tooth is attempting to emerge are also very frequent. If the tooth is partially through the gum, it can create a flap of tissue (an operculum) that traps food and bacteria, leading to localized infection called pericoronitis, which can cause severe pain, pus, swelling that extends to the jaw and cheek, difficulty opening the mouth (trismus), and even fever. Other potential symptoms include stiffness in the jaw, difficulty chewing on the affected side, a bad taste in the mouth, or bad breath, often related to trapped food or infection around the erupting tooth.
What are the first signs of wisdom teeth?
The initial whispers of wisdom teeth activity are often subtle and easily overlooked. The very first signs are typically centered around mild discomfort or a vague sensation in the posterior regions of your mouth. This could be a feeling of pressure, as if something is shifting or pushing from within your jawbone. You might notice a slight tenderness or sensitivity in the gums right behind your last molars when you brush or touch the area. Sometimes, this initial phase might involve minimal or no pain at all, just a novel awareness of something happening in that far-flung corner of your mouth. It’s important not to dismiss these early sensations, especially in the typical age range for eruption (late teens to early twenties). While they might not immediately signal a major problem, they are your body’s way of indicating that the third molars are beginning their journey, warranting attention from your dentist to monitor their progress and position.
What is an impacted wisdom tooth?
An impacted wisdom tooth is essentially a tooth that doesn’t have sufficient space to fully erupt into the mouth in a normal, functional position. Instead of growing straight up and out like its neighboring molars, it gets “stuck,” either partially or completely, within the jawbone or beneath the gum tissue. This impaction can occur in various orientations: it might be angled towards the neighboring second molar (mesial impaction, the most common), angled away from it (distal impaction), positioned horizontally (lying flat in the jaw), or even angled towards the cheek or tongue. The degree of impaction also varies; it can be a soft tissue impaction (covered only by gum) or a bony impaction (partially or fully embedded in bone). Impaction is the primary reason wisdom teeth are often problematic, as their inability to erupt correctly leads to complications like infection, pain, and damage to adjacent teeth, making removal frequently necessary.
Problems with impacted wisdom teeth
Impacted wisdom teeth are notorious troublemakers, creating fertile ground for a host of oral health issues. Because they can’t fully emerge or are poorly positioned, they often create nooks and crannies that are impossible to clean effectively. This leads to trapped food particles, plaque, and bacteria accumulating around the tooth and under the gum flap covering it (if partially erupted). This stagnant environment is a breeding ground for infection, most commonly pericoronitis, an inflammation of the gum tissue around the crown of a partially erupted tooth, causing severe pain and swelling. Impaction can also lead to decay not only in the wisdom tooth itself but also in the adjacent second molar if food and bacteria are constantly packed against it. More seriously, impacted teeth can sometimes lead to the formation of cysts or even rare tumors in the jawbone around them, which can cause significant bone destruction if not treated. Furthermore, the pressure from an impacted tooth attempting to erupt can potentially cause root resorption or shifting of the neighboring tooth.
Do wisdom teeth always cause problems?
Absolutely not, and it’s a common misconception that every single wisdom tooth is destined for a life of causing trouble. While a significant percentage of wisdom teeth, particularly impacted ones, do lead to issues requiring intervention, there are many individuals whose wisdom teeth erupt completely and correctly into the dental arch. If a wisdom tooth emerges in a straight, upright position, has enough space to fit comfortably without crowding other teeth, and can be easily cleaned and maintained like any other molar through regular brushing and flossing, it may never cause a problem and can potentially be kept. The key factors are whether they erupt fully, are in a functional position, and are accessible for hygiene. The issues primarily arise when they are impacted, partially erupted, or erupt in a way that damages neighboring teeth or compromises oral hygiene in that area.
When are wisdom teeth a problem?
Wisdom teeth transition from asymptomatic residents to full-blown problems when they begin to cause pain, swelling, infection, or structural damage to surrounding teeth or bone. This frequently happens when they are impacted and attempting to erupt into insufficient space, leading to chronic pressure, inflammation, or the trapping of bacteria and debris. Pain and swelling are classic indicators of a problematic wisdom tooth, often signaling inflammation or infection (pericoronitis). Decay in the wisdom tooth itself, especially if it’s partially impacted and difficult to clean, is another common issue, as is decay developing on the back surface of the adjacent second molar due to chronic food impaction. The formation of cysts or tumors around the impacted tooth, though less common, is a serious complication that necessitates removal. Furthermore, if the erupting wisdom tooth is causing misalignment or damage to the roots or bone supporting the second molar, it is considered problematic. Ultimately, any wisdom tooth causing persistent symptoms, infection, or structural compromise to oral health is deemed a problem requiring professional evaluation.
What are complications of wisdom teeth?
The potential complications arising from problematic wisdom teeth extend beyond mere discomfort and can impact overall oral and sometimes systemic health. The most frequent complication is pericoronitis, an inflammatory infection of the gum tissue surrounding a partially erupted tooth, which can lead to severe pain, localized swelling, difficulty opening the mouth, and even spread of infection. Untreated infections can potentially develop into more serious conditions like cellulitis (a spreading bacterial infection) or abscesses. Impacted teeth can also cause significant damage to adjacent teeth, leading to decay on the distal (back) surface of the second molar that is often difficult or impossible to restore, or even causing root resorption of the second molar. Less commonly, but more seriously, impacted wisdom teeth can be associated with the development of cysts (fluid-filled sacs) or benign tumors in the jawbone, which can grow and destroy bone tissue if left untreated. While rare, there’s also a very slight risk of temporary or permanent nerve damage during the extraction procedure itself, particularly with lower wisdom teeth close to the inferior alveolar nerve.
Do wisdom teeth cause headaches?
Yes, wisdom teeth can indeed contribute to headaches, though it’s often a secondary or referred symptom rather than a direct cause. The connection primarily stems from the pressure exerted by impacted or erupting wisdom teeth on the jawbone and surrounding nerves. This pressure can manifest as pain that radiates outwards, sometimes felt in the temples or around the ear, mimicking a tension headache. Furthermore, the swelling and inflammation associated with pericoronitis (infection around a partially erupted wisdom tooth) can cause generalized facial pain and jaw stiffness, which can also trigger or exacerbate headaches. Issues related to the temporomandibular joint (TMJ), the hinge connecting your jawbone to your skull, can also be affected by the discomfort and altered biting patterns caused by problematic wisdom teeth, leading to TMJ-related pain that includes headaches. If you experience persistent headaches along with symptoms like jaw pain, swelling, or difficulty opening your mouth, it’s worth consulting a dentist to see if your wisdom teeth are the culprit.
Symptoms of wisdom teeth infection
An infection associated with wisdom teeth, most commonly pericoronitis, presents a distinct set of symptoms that go beyond simple discomfort and often require immediate dental attention. The hallmark signs include severe, throbbing pain in the back of the jaw that can radiate to the ear or temple. You will almost certainly experience noticeable swelling of the gum tissue around the affected tooth, which can spread to your cheek and jawline, causing facial asymmetry. The area will be very tender to the touch and may ooar pus or a foul-tasting discharge, leading to persistent bad breath or an unpleasant taste in your mouth. It’s also common to experience difficulty opening your mouth fully (trismus) due to inflammation and muscle stiffness. In more significant infections, you might develop systemic symptoms such as fever, chills, and swollen lymph nodes in your neck. These symptoms indicate an active infection that needs prompt treatment, usually involving antibiotics and potentially cleaning the area, or ultimately, removing the source of the infection – the problematic wisdom tooth.
Managing Wisdom Tooth Pain and Discomfort
Let’s talk about pain. It’s often the first, most insistent signal that your wisdom teeth are up to no good. Whether it’s the dull ache of an erupting tooth or the sharper throbbing from an infection, discomfort is a common companion on the wisdom tooth journey. Before reaching the point where extraction might be necessary, or while you’re waiting for an appointment, managing this pain becomes a priority. This section is dedicated to exploring practical strategies for temporary relief, from tried-and-true home remedies to readily available over-the-counter options. It’s about finding ways to ease the ache and reduce the inflammation until you can get professional help to address the underlying cause of the problem.
Is a wisdom tooth painful?
The short answer is, it can be, often intensely so, although not everyone experiences pain with their wisdom teeth. Whether a wisdom tooth is painful depends largely on its status and how it’s interacting with your jaw and surrounding tissues. If a wisdom tooth is erupting without sufficient space, the pressure it exerts on the bone, gums, and neighboring teeth can cause significant discomfort. Impacted teeth, particularly those partially erupted and prone to trapping food and bacteria, are frequently associated with pain due to resulting inflammation and infection (pericoronitis). The pain can range from a persistent, dull ache that’s constantly present to sharp, shooting pains that flare up intermittently, especially when chewing. However, some individuals have wisdom teeth that are either fully erupted and cause no issues, or deeply impacted in a way that doesn’t bother nearby structures, in which case they might experience little to no pain.
Do wisdom teeth hurt?
Yes, for a great many people, wisdom teeth do hurt, sometimes considerably. Pain is one of the most common reasons people seek dental care for their third molars. The act of these large teeth attempting to push through gum tissue and bone, often in a confined space, is inherently prone to causing discomfort. When they are partially erupted, the flap of gum tissue covering part of the tooth can become inflamed and infected, leading to severe pain known as pericoronitis. Impacted teeth can press on nerves or the roots of adjacent teeth, causing a deep, aching pain. The intensity and nature of the pain vary from person to person and depend on the specific circumstances of the tooth’s position and whether complications like infection are present. While some are lucky enough to have asymptomatic wisdom teeth, experiencing pain is a very real and frequent part of the wisdom tooth story for many.
Is wisdom tooth pain normal?
A certain degree of discomfort or mild soreness in the back of the jaw during the typical wisdom tooth eruption period (late teens/early twenties) can be considered within the range of “normal” as teeth naturally move and push through tissues. However, severe, persistent pain, swelling, redness, difficulty opening your mouth, or signs of infection like pus or fever are definitely not normal and indicate a problem that requires prompt dental attention. It’s important to distinguish between a mild, temporary ache associated with the tooth movement and more significant pain that signals underlying pathology like impaction, infection, or damage to neighboring teeth. So, while some discomfort might be expected, don’t dismiss significant pain; it’s your body signaling that something is wrong and needs professional assessment to prevent more serious complications.
At what stage do wisdom teeth hurt?
Wisdom teeth are most likely to cause pain during certain key stages of their development and attempted eruption. The most common periods for pain include:
-
- During active eruption: When the tooth is actively pushing through the jawbone and gum tissue. The pressure and inflammation caused by this movement can be painful.
-
- When partially erupted: This is a particularly problematic stage. A partially erupted wisdom tooth is often covered by a flap of gum tissue (operculum) which easily traps food, plaque, and bacteria. This trapped debris leads to inflammation and infection (pericoronitis), a major source of severe pain, swelling, and discomfort.
-
- When impacted and pressing on adjacent structures: An impacted tooth, even if not actively erupting, can cause pain if it’s pressing against the roots or crown of the second molar, or if it’s positioned close to or impinging on nerves within the jawbone.
- When decay or infection occurs: Decay in the wisdom tooth itself or the surrounding gums can cause pain, just like with any other tooth.
Pain is often episodic, flaring up during periods of active movement or when hygiene is compromised, and may subside temporarily at other times.
What pain can wisdom teeth cause?
The types of pain associated with problematic wisdom teeth can vary in character and location. The most direct pain is typically felt in the back of the jaw, where the tooth is located. This can be described as a deep, dull, throbbing ache, a constant pressure, or a sharp, intense pain that comes and goes. If the wisdom tooth is causing inflammation or infection, the pain is often more severe and can be accompanied by swelling and tenderness to the touch. Crucially, pain from wisdom teeth can also be referred, meaning it’s felt in other areas besides the immediate source. It commonly radiates along the jawbone, sometimes extending upwards towards the ear (causing earaches) or forward towards the cheek and temple (contributing to headaches or facial pain). Jaw stiffness and pain when chewing or opening the mouth widely are also frequent manifestations of wisdom tooth discomfort, often linked to inflammation of the surrounding tissues and muscles.
How to cure the pain of a wisdom tooth?
It’s important to understand that simply masking wisdom tooth pain isn’t a “cure” – a true cure requires addressing the underlying cause of the discomfort, whether that’s impaction, infection, inflammation, or damage. However, there are methods to help manage and alleviate the pain temporarily while you await professional treatment. Over-the-counter pain relievers like ibuprofen (an anti-inflammatory) or acetaminophen are often effective. Warm salt water rinses, performed several times a day, can help reduce inflammation, clean the area of trapped debris, and promote healing. Applying a cold pack to the outside of your cheek in the affected area can also help reduce swelling and numb the pain. Topical numbing gels containing benzocaine can provide temporary localized relief when applied directly to the painful gum tissue, though they should be used sparingly and are not a long-term solution. If the pain is severe or accompanied by signs of infection, a dentist may prescribe stronger pain medication or antibiotics before definitive treatment like extraction.
How to relieve ear pain caused by wisdom teeth?
Ear pain that seems disconnected from an obvious ear issue can often be referred pain originating from a problem in the jaw or mouth, and problematic wisdom teeth are a common culprit. The nerves that supply sensation to the jaw, teeth, and ears are closely connected. When a wisdom tooth, particularly a lower one, is impacted, infected, or causing inflammation, the pain signals can travel along these shared nerve pathways and be perceived in the ear. To relieve this referred ear pain, you need to address the source of the problem – the wisdom tooth itself. Temporary measures like over-the-counter pain relievers (especially anti-inflammatories like ibuprofen) can help reduce both the jaw inflammation and the resulting ear pain. Applying warm compresses or ice packs to the jaw area might also provide some relief. However, the definitive solution usually involves treating the wisdom tooth issue, whether that means managing an infection with antibiotics or extracting the tooth, which should then alleviate the referred pain in the ear.
What can I do to help relieve the discomfort of wisdom teeth?
When wisdom teeth are causing discomfort but haven’t yet reached a crisis point, or while you’re waiting for a dental appointment, there are several steps you can take to find temporary relief. Start with good oral hygiene: gently but thoroughly clean the area around the wisdom tooth to remove trapped food particles and bacteria, as this is a frequent source of inflammation and pain. Using warm salt water rinses multiple times a day can be very soothing and help reduce swelling. Over-the-counter pain medications like ibuprofen (which also helps with inflammation) or acetaminophen can be effective for managing pain. Applying an ice pack wrapped in a cloth to the outside of your cheek for 15-20 minutes at a time can help reduce swelling and numb the discomfort. Eating soft foods can prevent painful chewing on the affected side. Avoid hard, sticky, or hot foods that could irritate the area. Remember, these are temporary measures; if the discomfort persists or worsens, it’s essential to see a dentist for a proper diagnosis and treatment plan.
The Purpose and Evolution of Wisdom Teeth
Now, let’s shift gears from the immediate discomfort to the grander scheme of things. Why do we even have these troublesome teeth in the first place? Are they some kind of cosmic joke, or did they serve a genuine purpose at some point in our history? This section delves into the fascinating evolutionary narrative of wisdom teeth, exploring their original role in our ancestors’ mouths and discussing why they seem increasingly unnecessary, even counterproductive, in the context of modern human lifestyles and anatomy. It’s a look back in time to understand why these teeth are a biological inheritance and why they often present a mismatch with our current oral environment.
What is the purpose of wisdom teeth?
To understand the original purpose of wisdom teeth, you have to step back in time to consider the lifestyle and diet of early humans. Our ancestors consumed diets that were significantly rougher and coarser than ours today – think raw vegetables, tough meats, and grains that required extensive, forceful chewing. This rigorous diet led to considerable wear and tear on their teeth throughout their lives. First and second molars would wear down or even be lost due to decay (though less prevalent than today due to lack of refined sugars) or trauma. In this context, having a third set of large molars erupt later in life provided crucial additional chewing surface and acted as “replacements” as the anterior teeth wore away or were lost. So, the original purpose of wisdom teeth was quite practical: to provide backup grinding capacity necessary for processing a demanding diet in a time when other teeth might be compromised.
What was the original purpose of wisdom teeth?
The original purpose of wisdom teeth was fundamentally linked to the survival and dietary needs of early humans. Imagine a world without forks, knives, or blenders, where food preparation involved sheer physical breakdown in the mouth. Our ancestors needed powerful jaws and plenty of molar surface area to process tough, fibrous plant matter and raw or lightly cooked meats. Their jaws were typically larger than ours, providing ample space for these extra molars. Furthermore, dental health was precarious; tooth loss due to wear, fracture, or infection was a common occurrence. Having third molars erupt in late adolescence or early adulthood meant a fresh set of grinding teeth became available just as the front molars were starting to show significant wear or might even have been lost. Thus, their original purpose was to maintain efficient chewing function throughout a longer lifespan, acting as essential backup teeth for a demanding diet.
Why did God create wisdom teeth?
Approaching this from a scientific, evolutionary perspective grounded in the context of the previous topics, the presence of wisdom teeth isn’t attributed to a singular act of creation but rather to the process of natural selection over vast periods. From this viewpoint, organisms develop traits that provide a survival or reproductive advantage in their specific environment. For early humans with large jaws and rough diets, having extra molars erupt later in life was advantageous for survival, ensuring they could continue to process food effectively even as other teeth wore down or were lost. Individuals with the genetic predisposition to develop these third molars were likely better equipped to thrive and pass on those genes. As human diets changed (becoming softer with the invention of cooking, farming, and food processing) and our jaws evolved, becoming smaller over millennia, the functional necessity of these teeth decreased, while the potential for them to cause problems in a reduced jaw space increased. So, scientifically, they exist because they were beneficial in our ancestral environment and have persisted in our genetic code, even as their utility has waned.
What are wisdom teeth for?
In terms of historical function, wisdom teeth were undoubtedly “for” providing additional and potentially replacement chewing surfaces for a tough, unprocessed diet. They were part of a larger, more robust chewing apparatus suited to the demands of early human sustenance. However, when we ask what they are “for” in the context of modern human life, the answer is often: not much. With our softer diets, better dental hygiene, and access to professional dental care, we typically retain our first and second molars throughout life with minimal wear. Our jaws, meanwhile, have evolved to be smaller, leaving insufficient room for these final molars to erupt correctly in a significant portion of the population. Therefore, in many modern mouths, wisdom teeth serve no essential chewing function and are often problematic evolutionary leftovers. They are a biological artifact, no longer necessary for survival and frequently detrimental to oral health.
Why do we have wisdom teeth? Do we need them?
We have wisdom teeth primarily as a legacy of our evolutionary past. Our ancestors needed them for chewing tough foods and as replacements for worn or lost teeth. The genetic programming to develop these third molars has been passed down through generations. However, the conditions under which they were advantageous (large jaws, rough diet, high tooth loss) have changed dramatically for most modern humans. Our jaws are smaller, and our diets are softer, reducing the need for intense grinding, while modern dentistry helps us retain our other teeth. Consequently, in the vast majority of cases today, we do not need wisdom teeth for effective chewing or oral function. The existing first and second molars provide more than sufficient grinding power for a typical modern diet. In fact, because they so often lack space to erupt properly, they are more likely to cause problems like pain, infection, and damage to adjacent teeth, making them a liability rather than an asset for many individuals.
Deciding When and Why Wisdom Teeth Might Need Removal
This is the pivot point for many people encountering issues with their third molars: the discussion around removal. While not every wisdom tooth needs to be extracted, a significant number do. This section navigates the decision-making process, outlining the specific circumstances and medical reasons that compel dentists and oral surgeons to recommend taking these teeth out. It addresses the crucial question of necessity and clarifies why, in certain situations, ignoring a problematic wisdom tooth is ill-advised. Understanding the “why” behind a recommendation for extraction is crucial for patients facing this decision.
Why wisdom teeth might need to be removed
The decision to remove wisdom teeth is typically made based on a clear set of criteria indicating that the tooth is causing current problems or presents a high risk of causing future issues that could compromise overall oral health. The most common reasons include impaction that leads to pain, swelling, or infection (pericoronitis). If an impacted or partially erupted wisdom tooth is contributing to decay, either in itself or, more critically, on the adjacent second molar (which can be very difficult to fill), extraction is usually recommended. Another significant reason is when impacted wisdom teeth are causing or are likely to cause damage to the neighboring teeth, such as root resorption or bone loss around the second molar. The presence of cysts or tumors associated with an impacted tooth, though less frequent, is a strong indication for removal. Furthermore, sometimes wisdom teeth are removed for orthodontic reasons, such as needing space to properly align other teeth, or prophylactically (preventively) when imaging clearly shows they are impacted in a way that makes future problems highly probable, even if asymptomatic at the moment.
Is it necessary to remove wisdom teeth?
No, it is absolutely not necessary to remove wisdom teeth in every single case. The necessity for extraction is determined on an individual basis after a thorough clinical examination and review of dental X-rays. If a wisdom tooth has fully erupted into the mouth in a functional position, is properly aligned, is not causing any crowding or damage to adjacent teeth, and, crucially, can be easily cleaned and maintained with regular brushing and flossing, then it may not need to be removed. In such cases, the tooth can function like any other molar, and the approach is typically to monitor it during routine check-ups. Extraction becomes necessary when the tooth is causing problems (pain, infection, decay, damage to adjacent teeth, cyst formation) or when it is clearly impacted in a way that makes future problems highly likely, justifying prophylactic removal to prevent more serious complications down the line.
Is it okay to ignore a wisdom tooth?
Ignoring a wisdom tooth that is causing symptoms or that a dentist has identified as problematic due to impaction or pathology is generally not advisable and can lead to more significant health issues. While a healthy, fully erupted, and easily cleaned wisdom tooth that causes no problems can typically be left alone and monitored, one that is causing pain, swelling, difficulty opening the mouth, or showing signs of infection (like pus or fever) requires immediate attention. Ignoring an active infection can lead to its spread to surrounding tissues (cellulitis) or even into the bloodstream in rare cases, becoming a life-threatening condition. An impacted tooth that is damaging a neighboring tooth won’t fix itself, and the damage could progress to the point where the second molar is lost. Cysts and tumors associated with impacted teeth will continue to grow, destroying bone tissue. Therefore, if your wisdom tooth is giving you trouble or has been flagged by your dentist as a concern, ignoring it is essentially ignoring a potential health risk that could worsen over time.
When to go to the dentist for wisdom teeth?
You should absolutely schedule a visit to the dentist if you experience any symptoms in the back of your jaw that could be related to your wisdom teeth. These symptoms include pain, swelling, redness or tenderness of the gums, difficulty opening your mouth fully, a bad taste in your mouth or bad breath specifically from the back area, or any visible sign of a tooth attempting to erupt accompanied by discomfort. Even if the symptoms are mild or intermittent, it’s wise to get them checked out. Furthermore, even without symptoms, it’s standard practice for dentists to monitor wisdom teeth development with X-rays during routine check-ups for teenagers and young adults, typically starting around age 16 or 17. This allows them to assess the position of the developing teeth, determine if there’s enough space for them to erupt properly, and identify potential issues like impaction early on, enabling proactive management or planning for removal if necessary before problems arise. Don’t wait for severe pain to get them evaluated.
Why do dentists not want to remove wisdom teeth?
It’s important to clarify that it’s not that dentists “don’t want” to remove wisdom teeth out of reluctance or fear; rather, ethical and professional dental practice dictates that any surgical procedure, including tooth extraction, should only be performed when it is necessary and beneficial for the patient’s health. Dentists are trained to preserve teeth whenever possible. Therefore, if a wisdom tooth is healthy, fully erupted, functional, and can be easily cleaned, a responsible dentist will recommend keeping it and monitoring it during regular check-ups. Extraction is a surgical procedure that carries inherent risks, such as infection, bleeding, swelling, pain, and in rare cases, temporary or permanent nerve damage. Dentists and oral surgeons weigh these potential risks against the risks of keeping a problematic tooth (infection, damage, cysts, etc.). The recommendation for removal is made when the risks of keeping the tooth outweigh the risks associated with the extraction procedure itself, or when the tooth is causing current problems that cannot be managed otherwise. So, their approach is rooted in patient safety and clinical necessity, not a general aversion to performing the procedure.
What are the main reasons for taking wisdom teeth out?
The primary drivers for recommending the removal of wisdom teeth boil down to preventing or resolving existing oral health problems. The most frequent reason is impaction that results in infection (pericoronitis) or chronic inflammation and pain around the partially erupted tooth. Another major factor is the presence of decay in the wisdom tooth that cannot be properly restored due to its position or partial eruption, or when the wisdom tooth is contributing to decay or damage on the adjacent second molar. The formation of cysts or benign tumors associated with an impacted wisdom tooth is also a critical reason for removal, as these can enlarge and destroy surrounding bone. Less commonly, they may be removed due to their potential to interfere with orthodontic treatment or to address root resorption or bone loss around the second molar caused by the impacted tooth. Finally, in some cases, prophylactic removal is recommended based on strong radiographic evidence of impaction and a high likelihood of future problems, especially in young adults, to avoid more complex procedures or complications later in life.
The Wisdom Tooth Removal Procedure
So, the decision is made – the wisdom teeth need to go. What happens next? This section walks you through the process of wisdom tooth removal, from the initial steps of preparing for the procedure to what actually occurs once you’re in the dental chair. It demystifies the process, explaining who performs the surgery, the different levels of anesthesia involved, and the basic steps the dental professional will take to safely extract these often-stubborn molars. Understanding the procedure can help alleviate anxiety and prepare you for the experience.
Can dentists remove wisdom teeth?
Yes, general dentists are qualified to remove some wisdom teeth, particularly those that have fully erupted into the mouth and can be removed like any other tooth with standard extraction techniques. These are often referred to as “simple” extractions. However, the majority of problematic wisdom teeth, especially those that are impacted (stuck below the gum or bone), require a more involved surgical procedure. In these cases, general dentists will typically refer patients to an oral and maxillofacial surgeon (often simply called an oral surgeon). Oral surgeons have undergone several additional years of specialized training after dental school focusing on surgery of the mouth, jaws, face, and related structures. They are highly skilled in performing complex surgical extractions, including removing bone that may be covering the tooth and sectioning the tooth into smaller pieces for easier removal, and are experienced in administering various types of anesthesia, including sedation and general anesthesia, which are often preferred for wisdom tooth removal.
Preparing for wisdom teeth extractions
Preparing for wisdom tooth extraction surgery involves several important steps to ensure the procedure goes smoothly and recovery is optimized. It begins with a detailed consultation with your dentist or oral surgeon. During this appointment, they will review your medical history, discuss any medications you are taking, examine your mouth, and evaluate recent dental X-rays (often a panoramic X-ray or sometimes a 3D cone beam CT scan) to assess the position, size, and proximity of your wisdom teeth to nerves and other structures. This consultation is your opportunity to ask questions, discuss the procedure, and explore anesthesia options. You will be given specific pre-operative instructions, which typically include fasting (not eating or drinking anything) for a certain number of hours before the surgery if receiving sedation or general anesthesia, arranging for a responsible adult to drive you home and stay with you after the procedure, wearing loose, comfortable clothing, and sometimes starting a course of antibiotics beforehand if an infection is present.
What happens during wisdom tooth removal
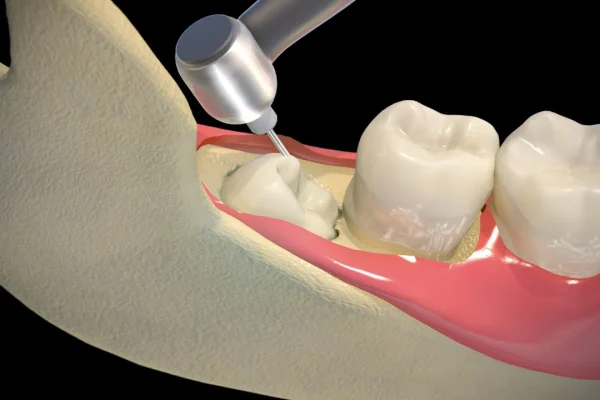
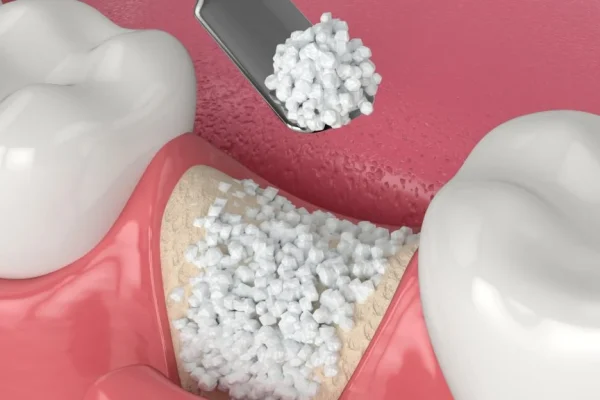
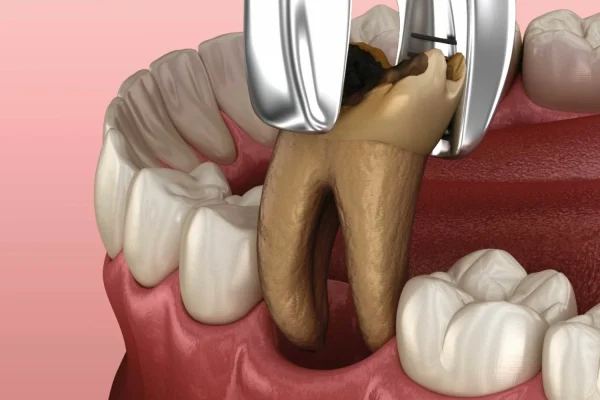
The process of wisdom tooth removal, especially for impacted teeth, is a surgical procedure performed under anesthesia to ensure you are comfortable and feel no pain. The type of anesthesia used will be discussed beforehand and can range from local anesthesia (numbing the area while you remain awake) to sedation (making you drowsy and relaxed) or general anesthesia (putting you completely asleep). Once the anesthesia has taken effect, the surgeon will typically make an incision in the gum tissue to expose the tooth and the underlying bone. If the tooth is covered by bone, a small amount of bone may need to be carefully removed using a dental drill. Often, particularly if the tooth is impacted at an awkward angle or is very large, the surgeon will section (cut) the tooth into smaller pieces for easier removal with less trauma to the surrounding bone and tissue. After the tooth (or pieces) are extracted, the surgeon will clean the surgical site, removing any debris. The gum tissue is often sutured (stitched) closed, and gauze is placed over the site to control bleeding.
How are wisdom teeth removed?
The method used to remove a wisdom tooth depends heavily on whether it has fully erupted or if it is impacted. For a fully erupted wisdom tooth that is accessible, the procedure is similar to a standard tooth extraction. The dentist will use instruments called elevators to gently loosen the tooth from the surrounding bone and ligaments and then forceps to grasp and remove it. This is considered a simple extraction. For impacted wisdom teeth, a surgical extraction is required. This is a more complex procedure typically performed by an oral surgeon. It often involves making an incision in the gums to expose the tooth. If bone is covering the tooth, a small amount of bone may need to be removed. In many cases, the surgeon will need to section (cut) the tooth into two or more pieces using a dental drill. This allows each piece to be removed individually, which is often easier and causes less disruption to the surrounding tissue and bone than trying to remove the tooth whole, especially if it’s angled or deeply impacted. After the tooth fragments are removed, the site is cleaned, and the gums are typically stitched closed.
What Does Removing My Wisdom Teeth Require?
Removing your wisdom teeth involves several distinct requirements and steps. First and foremost, it requires a professional dental assessment, usually involving a clinical exam and diagnostic imaging like X-rays, to determine if removal is necessary and feasible. If extraction is recommended, it requires scheduling the procedure with a qualified dental professional, who might be a general dentist for simple cases or, more commonly, an oral and maxillofacial surgeon for impacted teeth. The procedure itself requires the administration of appropriate anesthesia, which could range from local numbing injections to sedation or general anesthesia, depending on the complexity and your preference, overseen by a trained professional. Post-procedure, it requires diligent adherence to aftercare instructions provided by your surgeon to ensure proper healing and minimize complications. Finally, it requires a period of rest and recovery, during which you will need to manage pain and swelling and modify your diet. In essence, it requires professional expertise for assessment and execution, and patient cooperation for preparation and recovery.
Recovery and Aftercare Following Wisdom Tooth Removal
The procedure is over, but the journey isn’t finished yet. The hours and days immediately following wisdom tooth extraction are crucial for healing and managing post-operative symptoms. This section provides a comprehensive guide to what you can realistically expect during the recovery period, covering everything from initial discomfort and swelling to potential complications like dry socket and how to care for the surgical sites. Proper aftercare is paramount to a smooth recovery, and knowing what to do – and what not to do – can make a significant difference in your healing experience.
What should I expect after a wisdom tooth is taken out?
Immediately after wisdom tooth extraction, you should expect some degree of bleeding from the surgical site, which will be managed by biting down firmly on gauze pads. Swelling of the face and jaw is a very common and normal reaction to oral surgery; it typically peaks 48-72 hours after the procedure. You will also experience pain once the anesthesia wears off, ranging from mild discomfort to moderate or even severe pain, depending on the complexity of the extraction. Numbness or tingling in the lips, tongue, or cheek is possible, usually temporary, especially if local anesthesia was used. You will likely feel tired and drowsy, particularly if you received sedation or general anesthesia. It’s crucial to go straight home and rest, keeping your head elevated. Follow all post-operative instructions diligently, including managing pain with prescribed or over-the-counter medication, applying ice packs to reduce swelling, and adhering to a soft diet. Avoid strenuous activity, smoking, and using straws, as these can hinder healing and potentially lead to complications like dry socket.
Care after surgery for removal of wisdom teeth
Proper care after wisdom tooth removal is vital for preventing complications and promoting faster healing. Here are the key aspects:
-
- Bleeding Control: Bite firmly on the gauze pads placed by your surgeon for 30-60 minutes. Change the gauze as directed. Some oozing is normal for the first 24 hours. Avoid excessive rinsing or spitting.
-
- Swelling Management: Apply ice packs to the outside of your face, over the extraction sites, for 20 minutes on and 20 minutes off during the first 24-48 hours.
-
- Pain Management: Take pain medication as prescribed by your surgeon, or use over-the-counter options like ibuprofen or acetaminophen as recommended. Take medication before the anesthesia completely wears off.
-
- Diet: Stick to soft foods for the first few days (e.g., yogurt, pudding, mashed potatoes, soup). Avoid hot liquids, hard, crunchy, or sticky foods that could irritate the sites or dislodge the blood clot. Gradually return to your normal diet as comfort allows.
-
- Hydration: Drink plenty of fluids, but avoid straws, as the suction can dislodge the blood clot.
-
- Oral Hygiene: Do NOT rinse your mouth for the first 24 hours. After 24 hours, gently rinse with warm salt water several times a day to keep the area clean (a teaspoon of salt in a glass of warm water). You can gently brush your other teeth, but avoid brushing directly over the extraction sites for several days.
-
- Rest: Get plenty of rest, especially in the first 24-48 hours. Keep your head elevated with pillows.
- Avoid: Do not smoke or use tobacco products, as this significantly impairs healing and increases the risk of dry socket. Avoid strenuous physical activity. Avoid alcohol.
What to do following an extraction
Following your wisdom tooth extraction, your immediate priorities should be rest, managing bleeding and swelling, and controlling pain while carefully protecting the surgical site. Here’s a breakdown of key actions:
-
- Rest: Head straight home and recline with your head elevated on pillows. Avoid lying flat. Limit activity for at least the first 24 hours; strenuous activity should be avoided for several days.
-
- Gauze: Keep firm pressure on the gauze pads placed in your mouth as directed by your surgeon. Change them as needed (usually every 30-60 minutes initially) until bleeding subsides.
-
- Ice: Apply ice packs to the outside of your cheek near the extraction sites. Use for 20 minutes on, 20 minutes off, for the first 24-48 hours to minimize swelling.
-
- Medication: Take prescribed pain medication and/or antibiotics exactly as directed. Don’t wait for pain to become severe before taking your pain medication.
-
- Hydration: Drink plenty of water. Avoid hot drinks, carbonated beverages, and using straws.
-
- Diet: Eat only soft foods initially. Avoid chewing on the extraction sites.
-
- Oral Hygiene (after 24 hours): Begin gently rinsing your mouth with warm salt water (half a teaspoon of salt in a cup of warm water) 2-3 times a day, especially after eating, to help keep the area clean. Continue to brush your other teeth carefully, avoiding the surgical sites.
- Avoid: Do not smoke, spit forcefully, rinse vigorously, or use straws for at least the first 48-72 hours, as these actions can dislodge the crucial blood clot and lead to dry socket.
Will I need time off to recover?
Yes, it is highly recommended that you plan to take some time off from work, school, or other strenuous activities to recover after wisdom tooth removal. The amount of time needed varies depending on the complexity of the extraction and how quickly you heal. For most people, particularly after the removal of impacted wisdom teeth, the initial recovery period involving significant swelling, pain, and restricted diet lasts about three to seven days. During the first 24-48 hours, rest is paramount, and you’ll likely feel tired and uncomfortable, making it difficult to concentrate or perform demanding tasks. Even simple extractions may warrant a day or two of rest. Your oral surgeon will give you guidance based on your specific procedure, but planning for at least three days off is generally advisable, and up to a week might be necessary for more complex cases or if your job involves physical labor.
What is ‘dry socket’?
Dry socket, clinically known as alveolar osteitis, is a painful complication that can occur after a tooth extraction, most commonly following the removal of lower wisdom teeth. It happens when the blood clot that should form in the empty tooth socket either dissolves prematurely or is dislodged. This blood clot serves as a protective layer and the foundation for new bone and tissue growth. Without the clot, the underlying bone and nerve endings are exposed to air, food, and fluids, leading to intense pain, which is typically worse than the pain experienced immediately after surgery. Symptoms usually develop a few days after the extraction and include severe pain radiating from the socket to the ear or temple, a foul odor, and a bad taste in the mouth. It’s crucial to contact your oral surgeon or dentist if you suspect you have a dry socket. Treatment involves cleaning the socket and packing it with a medicated dressing to protect the exposed bone and promote healing, which provides significant pain relief. Smoking, vigorous rinsing, and using straws after extraction significantly increase the risk of developing dry socket.
Can I talk after wisdom teeth removal?
Yes, you absolutely can talk after wisdom teeth removal, but it might be a bit uncomfortable initially. Your ability to talk normally will depend on the type of anesthesia you received (general anesthesia or sedation might make you feel groggy for a while), the amount of swelling you experience, and any jaw stiffness (trismus) that might occur. Swelling can make it feel awkward to move your mouth fully, and stiffness in the jaw muscles is a common side effect that can restrict opening. While you can talk, it’s generally advisable to limit prolonged conversations, especially in the first 24-48 hours. Excessive talking involves moving your facial and jaw muscles, which could potentially strain the surgical sites, disturb the blood clot, or exacerbate swelling. Rest is key to healing, and that includes resting your jaw. So, while you won’t be completely silent, prepare for some initial difficulty and plan to conserve your energy by talking less.
Will removal affect my brushing?
Yes, wisdom tooth removal will temporarily affect your brushing routine, particularly in the areas where the teeth were extracted. For the first 24 hours after surgery, you should generally avoid rinsing your mouth or brushing the teeth immediately adjacent to the extraction sites to allow the blood clot to form undisturbed. After the initial 24-hour period, you can resume gentle brushing of your other teeth. However, you must exercise extreme caution around the extraction sites themselves. Your surgeon will provide specific instructions, but typically you’ll be advised to avoid brushing directly on the sockets for several days. Instead of forceful brushing, you’ll be instructed to use gentle warm salt water rinses (after the first 24 hours) to help keep the area clean and reduce bacteria. Gradually, as the sites heal and become less tender, you can cautiously begin to clean the surfaces of the teeth next to the extraction sites, slowly working your way back to a normal brushing routine as comfort and healing progress.
Is removing wisdom teeth painful?
Let’s be clear: the wisdom tooth removal procedure itself is not painful because it is performed under anesthesia. You will either have the area numbed with local anesthetic, be in a relaxed or semi-conscious state with sedation, or be completely asleep under general anesthesia, ensuring you don’t feel pain during the extraction. However, it is entirely normal and expected to experience pain and discomfort after the anesthesia wears off, during the recovery period. The level of post-operative pain varies from person to person and depends on factors like how many teeth were removed, whether they were impacted, and your individual pain tolerance. This post-operative pain is managed with prescription pain medication (often opioids for a few days followed by over-the-counter options) and anti-inflammatory drugs like ibuprofen. While it can be uncomfortable for several days, the pain is generally manageable with medication and should gradually decrease as healing progresses.
How painful is wisdom teeth removal?
The pain experienced after wisdom tooth removal is subjective and varies, but it is generally described as moderate to severe, particularly for impacted tooth extractions. It’s typically most intense in the first 24-72 hours following the procedure, coinciding with the peak swelling period. Patients often describe it as a throbbing ache at the extraction sites, sometimes radiating along the jaw. The degree of surgical intervention required (e.g., amount of bone removed, whether the tooth had to be sectioned) directly correlates with the level of post-operative discomfort. While manageable with prescribed pain relievers and anti-inflammatories, it’s definitely a source of significant discomfort that impacts daily activities, eating, and sleeping during the initial recovery phase. The pain should progressively lessen after the first few days, becoming more of a dull ache or soreness before resolving completely, provided there are no complications like dry socket, which causes distinct, severe pain.
What are the side effects of removing wisdom teeth?
Removing wisdom teeth, being a surgical procedure, comes with several common and expected side effects that are part of the normal healing process. The most prominent side effects are swelling of the cheeks and jaw, which can make your face look puffy and can sometimes cause bruising. Pain and discomfort at the surgical sites are universal side effects, managed with medication. Some degree of bleeding or oozing from the sockets is normal for the first 24 hours. Jaw stiffness (trismus) and difficulty opening your mouth widely are also common due to inflammation and muscle soreness. You might experience temporary numbness or tingling in your lips, tongue, or cheek if the surgery was close to certain nerves, although permanent nerve damage is rare. Other possible, less frequent side effects include bruising on the face or neck, a sore throat, and discomfort from the stitches if they were used. These side effects generally subside gradually over the first week or two.
What are the disadvantages of removing wisdom teeth?
While removing problematic wisdom teeth often prevents more serious issues, the procedure itself does come with potential disadvantages and risks. The most immediate disadvantages are the pain, swelling, bruising, and discomfort experienced during the recovery period, which necessitate time off work or school and restrict normal activities and diet. There are also surgical risks, although generally low, including the possibility of infection at the surgical site, excessive bleeding, and the painful complication of dry socket. A more serious, though rare, risk is temporary or permanent nerve damage, which could lead to numbness, tingling, or altered sensation in the lip, tongue, or cheek. There’s also the financial cost of the procedure and the inconvenience of preparing for and recovering from surgery. For wisdom teeth that are asymptomatic and healthy, the disadvantage is undergoing an unnecessary procedure and exposing oneself to these risks without a clear benefit.
Should I fear wisdom teeth removal?
It’s completely normal to feel apprehensive or anxious about wisdom tooth removal, especially if it’s your first oral surgery or if you’ve heard negative stories. However, you should not approach it with overwhelming fear. Wisdom tooth extraction is one of the most common surgical procedures performed, and oral surgeons are highly trained and experienced in managing it safely and effectively. Modern anesthesia techniques (local anesthesia, sedation, or general anesthesia) ensure that you will be comfortable and pain-free during the procedure itself. While post-operative discomfort, swelling, and the risk of complications like dry socket are real, they are manageable with proper care and follow-up with your surgeon. Discussing your fears and concerns openly with your dentist or oral surgeon can be very helpful; they can explain the process in detail, discuss pain management strategies, and reassure you about the measures taken to ensure your safety and comfort, empowering you with knowledge and reducing anxiety.
Risk factors of inferior alveolar nerve damage
Damage to the inferior alveolar nerve is a potential, though rare, complication specifically associated with the removal of lower wisdom teeth. This nerve runs through the lower jawbone and provides sensation to the lower lip, chin, and some gum tissue and teeth. When a lower wisdom tooth’s roots are very close to or wrapped around this nerve, there is a risk that the nerve can be bruised, stretched, or in very rare cases, severed during the extraction process. This can result in temporary or, even more rarely, permanent numbness, tingling, or altered sensation (paresthesia or dysesthesia) in the lip, chin, or tongue on the affected side. Risk factors for this complication include the anatomical position of the tooth roots in close proximity to the nerve canal as visualized on X-rays (especially panoramic X-rays or 3D CT scans), the depth and complexity of the impaction, the age of the patient (risk might slightly increase with age as bone density increases), and the surgical technique used. Oral surgeons carefully assess the position of the nerve using imaging before surgery and employ techniques to minimize this risk.
Risk factors
Beyond nerve damage, several general factors can increase the overall risk of complications during or after wisdom tooth removal. Smoking is a major risk factor, significantly increasing the likelihood of dry socket and delaying healing. Poor oral hygiene before surgery can increase the risk of infection at the extraction site. Certain medical conditions, such as uncontrolled diabetes or conditions that affect blood clotting or the immune system, can impact healing and increase complication risk, so it’s crucial to provide a complete medical history to your surgeon. The complexity of the extraction itself – for instance, a deeply impacted tooth requiring significant bone removal or sectioning – inherently carries a higher risk of post-operative pain, swelling, and potential complications compared to a simple extraction. Age can also be a factor; while younger patients (late teens/early twenties) often recover faster due to softer bone and less fully formed roots, the risk of nerve injury can slightly increase with age in the lower jaw.
What are common treatments for wisdom teeth complications?
Treatments for complications arising from wisdom teeth depend entirely on the specific issue encountered. For pericoronitis (infection around a partially erupted tooth), initial treatment often involves irrigation and cleaning of the area, warm salt water rinses, and a course of antibiotics to clear the infection, sometimes followed by pain management before the tooth is ultimately removed. If dry socket occurs after extraction, the treatment involves gently irrigating the socket to remove any debris and placing a medicated dressing or paste into the socket, which provides significant pain relief and protects the exposed bone while the area heals. This dressing may need to be changed every few days. Infections that spread (cellulitis, abscesses) require prompt and often stronger antibiotic therapy, potentially drainage of pus, and urgent removal of the source tooth. Cysts or tumors associated with impacted teeth necessitate surgical removal of the lesion along with the tooth, and sometimes require further treatment depending on the pathology found. Damage to adjacent teeth due to wisdom tooth pressure might require restoration (like a filling for decay) or more complex treatment if the damage is severe.
Keeping and Caring for Your Wisdom Teeth
As we’ve established, not all wisdom teeth are destined for extraction. For those fortunate enough to have them erupt properly and behave themselves, the goal shifts from removal to maintenance. This section outlines the responsibilities that come with keeping your wisdom teeth, emphasizing the ongoing importance of vigilant oral hygiene in those hard-to-reach areas and the necessity of regular professional check-ups to ensure they remain healthy and problem-free over time.
Keeping Your Wisdom Teeth?
If your wisdom teeth have fully erupted, are in a good position without crowding other teeth, and can be easily cleaned, congratulations – you might be one of the lucky ones who gets to keep them! In this scenario, where the teeth are functional and healthy, there is no medical reason to remove them. Keeping them means treating them just like any other tooth: brushing, flossing, and getting regular dental check-ups. However, even healthy wisdom teeth require diligent care precisely because of their location at the very back of the mouth, which makes them more challenging to keep clean. Your dentist will continue to monitor them during your routine appointments, often with periodic X-rays, to ensure they remain healthy, free of decay, and aren’t causing any subtle problems you might not be aware of. Keeping them is a valid option when they aren’t causing or likely to cause pathology, but it requires a commitment to excellent oral hygiene in that specific area.
How to clean wisdom teeth?
Cleaning wisdom teeth effectively presents a unique challenge simply due to their position at the very back of the mouth. When they are fully erupted and properly aligned, they need to be brushed and flossed just like your other molars, but reaching them can be awkward. Using a toothbrush with a small head specifically designed for accessing tight spaces can help. Focus on angling the brush head to reach all surfaces, including the chewing surface and the side facing your cheek and tongue. Pay particular attention to the back surface, behind the tooth, where plaque and food debris can easily accumulate. For flossing, this area can be particularly difficult. Consider using aids like floss holders, interdental brushes, or a water flosser (oral irrigator) to help remove plaque and debris from between the wisdom tooth and the adjacent second molar, and around the wisdom tooth itself. If a wisdom tooth is only partially erupted, cleaning around the gum flap covering it is even harder and is often a source of infection; your dentist might recommend specific techniques or rinses for these areas.
How can I care for my wisdom teeth?
Caring for wisdom teeth that you plan to keep involves consistent, thorough oral hygiene and regular professional dental monitoring. Firstly, commit to brushing them diligently twice a day. Given their tricky location at the back, spend extra time angling your toothbrush to ensure you reach all surfaces, including the distal (back) surface. Flossing is equally crucial; use dental floss or interdental cleaners daily to clean between the wisdom tooth and the second molar. If you struggle with manual flossing in this area, consider investing in a water flosser, which can be very effective at removing debris and bacteria from around the wisdom teeth and under any gum flaps. Regular use of an antimicrobial mouthwash might also be beneficial as an adjunct to brushing and flossing. Secondly, and just as importantly, maintain a schedule of regular dental check-ups and professional cleanings. Your dentist needs to examine your wisdom teeth regularly and take periodic X-rays to check for any signs of decay, gum disease, impaction issues, or other problems that might develop over time, even if you aren’t experiencing symptoms.
Other Specific Questions About Wisdom Teeth
Beyond the common inquiries about pain, removal, and eruption, wisdom teeth sometimes spark more unique or philosophical questions. This section tackles some of those specific curiosities, exploring the origins of their name, addressing unusual symptoms, and touching on topics like genetics, potential long-term impacts on other teeth, and even the feasibility of dental procedures during pregnancy.
Why is it called wisdom teeth?
The common name “wisdom teeth” is purely colloquial and stems from the relatively late age at which these third molars typically make their appearance compared to all your other adult teeth. While most of your permanent teeth erupt between the ages of 6 and 12, the wisdom teeth usually begin to emerge much later, generally between the ages of 17 and 25. This period in life is traditionally associated with reaching adulthood, maturing, and supposedly gaining more life experience, hence the informal link to acquiring “wisdom.” It’s a linguistic tradition rather than a medical or functional description, highlighting the timing of their eruption during late adolescence or early adulthood, a phase perceived as a transition towards greater maturity.
Why does my wisdom tooth smell?
A foul odor emanating from the area around your wisdom tooth is often a strong indicator of trapped food particles, bacteria, or infection. Because wisdom teeth are located so far back in the mouth, they are difficult to reach and clean effectively. If a wisdom tooth is partially erupted, a flap of gum tissue (operculum) often covers part of the crown, creating a perfect pocket where food debris, plaque, and bacteria can become trapped. This trapped matter decomposes, producing volatile sulfur compounds that cause a foul smell and bad taste. Furthermore, this trapped bacteria can lead to an infection of the gum tissue (pericoronitis), which often involves the formation of pus; pus is a collection of white blood cells, dead tissue, and bacteria and has a distinct, unpleasant odor and taste. If you notice a persistent bad smell from your wisdom tooth area, it’s a sign that hygiene is insufficient or that an infection might be brewing, and you should see a dentist.
Can wisdom teeth cause crooked teeth?
This is a widely debated topic, and the direct link between erupting wisdom teeth and the crowding or misalignment of front teeth is often overstated. While it was once commonly believed that the pressure from wisdom teeth pushing forward as they erupt could cause the front teeth to shift and become crooked, most modern orthodontic and dental research suggests that wisdom teeth are not a primary cause of significant anterior tooth crowding or malocclusion. Crowding of front teeth, especially in late adolescence or early adulthood, is more frequently attributed to natural developmental changes in the jaw, genetic factors influencing tooth size versus jaw size, and the tendency for teeth to naturally drift forward over time. Orthodontic relapse (teeth shifting back after braces) is also a common cause of late-onset crowding. While a severely impacted wisdom tooth might theoretically exert some pressure, it’s generally not considered powerful enough to move an entire arch of established teeth significantly. However, your dentist or orthodontist will evaluate your specific case to determine if your wisdom teeth might be a contributing factor to crowding or require removal for orthodontic treatment.
Are x-rays needed for wisdom teeth?
Yes, dental X-rays are absolutely essential for properly evaluating wisdom teeth and are considered a standard part of assessing their presence, position, and potential issues. A clinical examination alone cannot fully reveal the status of wisdom teeth, especially if they are still embedded in the bone or only partially erupted. Panoramic X-rays are particularly valuable as they provide a single image showing the entire upper and lower jaws, all the teeth (including those still developing or impacted), and important surrounding structures like the jawbone, sinuses, and nerve canals (specifically the inferior alveolar nerve in the lower jaw). This allows the dentist or oral surgeon to visualize the number of wisdom teeth present, their stage of development, their exact position and angle (e.g., impacted, horizontal, angled), the amount of space available for them to erupt, and their proximity to nerves or the roots of adjacent teeth. This information is crucial for diagnosing impaction, predicting potential problems, planning for surgical removal if necessary, and assessing the risks involved.
Why don’t some people have wisdom teeth?
The absence of one or more wisdom teeth in some individuals is a fascinating aspect of human genetic variation and evolution. It’s believed to be primarily due to genetic factors; some people simply inherit genes that result in the failure of one or more third molars to develop at all (a condition called congenital anodontia of third molars). This trait is thought to be increasing in prevalence within human populations over time and is considered by some evolutionary biologists as an ongoing evolutionary trend. As our diets have become softer and our use of tools for food preparation has reduced the need for heavy chewing, the functional requirement for wisdom teeth has diminished. Concurrently, evolutionary changes have led to smaller jaw sizes. The genetic programming for tooth development is complex, and the absence of wisdom teeth in some individuals might be a manifestation of genetic adaptation reflecting the reduced need and limited space for these teeth in modern humans. It’s a perfectly normal variation and often means those individuals avoid the common problems associated with wisdom teeth.
Can wisdom teeth grow back?
This question comes up sometimes, perhaps fuelled by discomfort or the feeling that the problem tooth has returned, but the answer is a definitive no. Teeth, including wisdom teeth, are formed during specific developmental stages of life. Once a wisdom tooth has fully formed (whether it erupts or remains impacted) and is subsequently extracted from the jawbone, it is gone permanently. The human body does not have the biological mechanism to regenerate an entirely new tooth in the same socket after extraction. Any sensation of a tooth growing back is likely either a misunderstanding, a new problem developing in the area (like bone spur healing, swelling, or issues with the adjacent tooth), or perhaps another wisdom tooth from a different quadrant attempting to erupt. But the extracted tooth itself cannot regrow.
Can I have wisdom teeth removed whilst pregnant?
While routine, non-urgent dental procedures, including elective wisdom tooth removal, are often postponed until after pregnancy, necessary dental treatment, including extractions, can be performed safely during pregnancy when indicated. The primary concern during pregnancy is the well-being of both the mother and the developing fetus. However, untreated dental infections can pose a risk to pregnancy, so managing acute pain or infection associated with a wisdom tooth is crucial. If removal is necessary due to severe pain, infection, or other urgent issues, it is typically recommended to perform the procedure during the second trimester, as this is generally considered the safest period for dental treatment. Any dental treatment during pregnancy requires close consultation and coordination between your dentist or oral surgeon and your obstetrician or midwife. They will carefully weigh the risks and benefits, select appropriate local anesthesia and pain management options that are safe during pregnancy, and time the procedure optimally to ensure the best possible outcome for both mother and baby.
How Much Does Wisdom Teeth Removal Cost?
Let’s talk brass tacks. The financial aspect of dealing with wisdom teeth, particularly extraction, is often a significant concern for patients. This section aims to provide a realistic overview of the costs involved, acknowledging that there’s no single fixed price tag. We’ll discuss the factors that cause costs to vary and touch upon how dental insurance typically fits into the picture, giving you a better sense of what to expect when budgeting for this potential procedure.
How much does wisdom teeth removal cost?
Pinning down an exact price for wisdom tooth removal is tricky because the cost varies considerably based on several factors. Generally, you can expect the cost per tooth to range anywhere from a couple of hundred dollars for a simple, fully erupted tooth extraction performed by a general dentist, to upwards of $500-$1,000 or even more per tooth for complex surgical extractions of impacted teeth performed by an oral surgeon, especially if IV sedation or general anesthesia is used. The total cost for removing all four impacted wisdom teeth with sedation can easily range from $2,000 to $4,000 or even higher in some areas. Key factors influencing the cost include: the complexity of the extraction (simple vs. surgical/impacted), the type of anesthesia used (local vs. sedation vs. general), the location and fees of the dental professional (general dentist vs. oral surgeon; geographical variations), and importantly, your dental insurance coverage. Dental insurance often covers a portion of the cost, but there will likely be deductibles, co-pays, and annual maximums that affect your out-of-pocket expense. Getting a detailed estimate from your dentist or oral surgeon before the procedure is essential, and check with your insurance provider to understand your coverage.
Frequently Asked Questions About wisdom of teeth
To wrap things up and provide quick answers to the most common queries, here’s a concise FAQ section summarizing the key points we’ve covered throughout this comprehensive guide to wisdom teeth.
A wisdom tooth, also known as a third molar, is the final set of molars located at the very back of your mouth, typically one in each corner (upper left, upper right, lower left, lower right). They are the last teeth to develop and attempt to erupt.
Wisdom teeth most commonly begin to emerge between the ages of 17 and 25, a period traditionally associated with gaining “wisdom,” which gives them their common name. However, eruption timing can vary, and issues with impacted teeth can arise later in life.
They frequently do, particularly when erupting into insufficient space, becoming impacted, or if infection (pericoronitis) develops around them. The pain level varies, but severe pain, swelling, and signs of infection are not normal and require dental attention.
What is the purpose of wisdom teeth?
In early humans with larger jaws and rougher diets, wisdom teeth provided extra chewing power and acted as replacements for worn or lost teeth. In modern humans with smaller jaws and softer diets, they often serve no essential function and are more likely to cause problems.
Is it necessary to remove wisdom teeth?
Removal is not necessary if wisdom teeth are healthy, fully erupted, properly positioned, and can be easily cleaned. However, removal is recommended and often necessary if they are causing current problems (pain, infection, decay, damage to adjacent teeth, cysts) or if imaging shows they are impacted in a way that presents a high risk of future complications.