What Is Gum Disease treatment and Why Does It Matter?

- Gum disease, also known as periodontal disease, is an infection of the tissues that support your teeth. It typically starts as gingivitis—a mild inflammation of the gums—and can progress into periodontitis, a more serious condition that can damage the bone that holds your teeth in place.
- Gingivitis is reversible if caught early, often presenting as red, swollen gums that may bleed during brushing or flossing. Periodontitis, however, can cause irreversible damage, leading to gum recession, bone loss, and eventually tooth loss.
- This condition is extremely common: estimates suggest that up to 90% of people will experience some form of gum disease during their lifetime. Yet because it can be painless, many individuals don’t realize they have it until it becomes severe.
- Gum disease is more than just a dental concern. Studies have linked it to several systemic health issues including cardiovascular disease, diabetes complications, osteoporosis, pneumonia, and even adverse pregnancy outcomes. This makes early diagnosis and ongoing prevention vital for overall health.
What Are the Signs and Symptoms of Gum Disease?
- Gum disease often begins silently, with subtle signs that are easy to ignore. One of the earliest and most common indicators is bleeding gums, especially during brushing or flossing. Healthy gums should not bleed.
- Other early warning signs include redness, puffiness, or swelling of the gums, and tenderness when touched. These symptoms typically indicate gingivitis, the mild and reversible form of gum disease.
- As the disease progresses, symptoms become more severe. You might notice gum recession, where the gum tissue pulls back and exposes more of the tooth or even the root.
- Bad breath (halitosis) and a persistent bad taste in your mouth are also common signs, caused by bacterial buildup and infection.
- In advanced stages, gum abscesses (collections of pus) may develop, and teeth can become loose or shift position, making chewing uncomfortable.
- A crucial concern is that gum disease is often painless in its early stages. Many people do not realize they have it until serious damage has occurred. This is why regular dental check-ups are vital.
What Does Periodontitis Look Like Compared to Gingivitis?
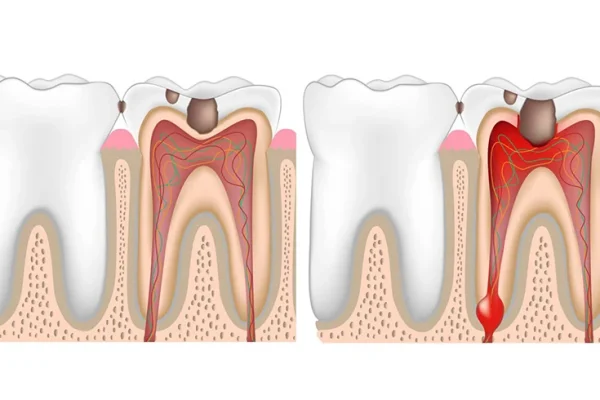
- Gingivitis appears as mildly swollen, red gums that may bleed when brushed. There’s no irreversible damage at this point, and treatment can quickly reverse the condition.
- Periodontitis, however, shows more severe signs. The gums may appear dusky red or purplish, and there may be visible gum recession and deep pockets around the teeth.
- Bleeding on probing during dental exams, increased tooth sensitivity, and loose teeth are red flags indicating advanced gum damage.
What Are the Stages of Gum Disease?
- Gum disease typically progresses through 4–5 clinical stages:
- Stage 1 (Initial Gingivitis): Mild redness and bleeding, reversible with hygiene.
- Stage 2 (Moderate Gingivitis): More pronounced bleeding and swelling.
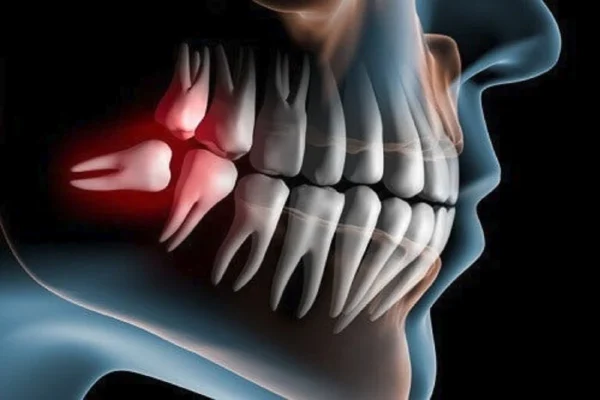
- Stage 3 (Early Periodontitis): Gum detachment begins, slight bone loss.
- Stage 4 (Moderate Periodontitis): Deeper pockets, noticeable bone loss, loose teeth.
- Stage 5 (Advanced Periodontitis): Severe bone loss, abscesses, teeth may fall out.
- Knowing these stages helps patients recognize when to act. Early intervention can prevent the irreversible damage seen in later stages.
What Causes Gum Disease to Develop?
- The primary cause of gum disease is the accumulation of dental plaque, a sticky film composed of bacteria, food particles, and saliva. When plaque is not removed regularly by brushing and flossing, it hardens into tartar (also called calculus), which cannot be removed with home care and requires professional cleaning.
- As plaque and tartar build up along and under the gumline, they trigger an immune response in the body. This leads to inflammation, which initially results in gingivitis—the earliest stage of gum disease.
- If left untreated, this inflammation allows bacteria to penetrate deeper into the gum tissue, forming pockets between the teeth and gums. These periodontal pockets become reservoirs for bacteria and toxins, leading to destruction of gum tissue and supporting bone—hallmarks of periodontitis.
- Importantly, poor oral hygiene is not the only contributing factor. Several other risk factors can accelerate the development of gum disease, even in individuals who brush and floss regularly.
Can Smoking and Diabetes Increase the Risk of Gum Disease?
- Yes, both smoking and diabetes are major risk factors for developing gum disease.
- Smoking is one of the most significant contributors. It weakens the immune system, making it harder for the body to fight infections, including those in the gums. Smokers are more likely to accumulate plaque and tartar, and their symptoms may be masked, such as less obvious bleeding, which can delay diagnosis.
- Smoking also reduces oxygen in the bloodstream, slowing healing in gum tissues and making treatments less effective.
- Diabetes impacts the body’s ability to process sugar, but it also reduces circulation, which impairs wound healing and increases the risk of infection. People with poorly controlled diabetes are more susceptible to infections, including those affecting the gums.
- The relationship between gum disease and diabetes is bidirectional—not only can diabetes worsen gum health, but gum disease can make it more difficult to control blood sugar levels.
- Other systemic health conditions that can influence gum disease include autoimmune disorders, stress, hormonal changes (such as during pregnancy or menopause), and nutritional deficiencies, especially in vitamins C and D.
How Is Gum Disease Diagnosed by Dentists?
- Detecting gum disease early is essential to prevent its progression from mild gingivitis to advanced periodontitis. Dentists use a combination of clinical assessments, measurements, and imaging to make a diagnosis.
- One of the first steps is a comprehensive oral examination, where the dentist checks for visible signs such as redness, swelling, bleeding, gum recession, and plaque or tartar buildup.
- During this exam, your dentist will likely perform periodontal probing using a special instrument called a periodontal probe. This tool measures the depth of the pockets between your gums and teeth. In a healthy mouth, the pockets are usually 1–3 mm deep. Depths of 4 mm or more indicate the presence of gum disease.
- Pocket depths of 5 mm or deeper can signal advanced periodontitis. These deeper pockets are more difficult to clean with regular brushing and flossing, making them more prone to bacterial buildup and progression of the disease.
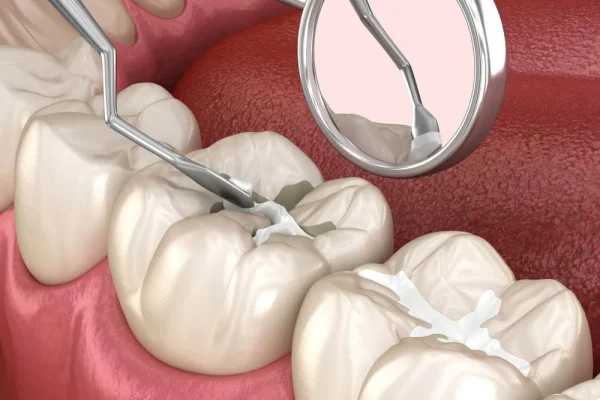
What Is Scaling and Root Planing and How Does It Work?
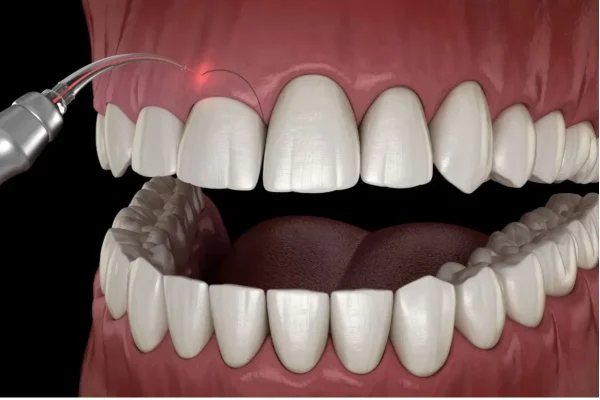
- If the probing measurements confirm gum disease, your dentist may recommend a deep cleaning procedure called scaling and root planing. This is often the first step in treating gum disease non-surgically.
- Scaling involves removing plaque and tartar from the tooth surfaces, especially below the gum line, using ultrasonic devices or manual tools.
- Root planing smooths the surfaces of the tooth roots to make it more difficult for bacteria to attach and to promote reattachment of the gum tissue to the tooth surface.
- These procedures can be performed over multiple visits and may involve local anesthesia to minimize discomfort.
- Scaling and root planing not only reduce inflammation and pocket depth but also halt further damage to the gums and bones if followed up with consistent oral hygiene and professional maintenance.
How Do Dentists Use Dental X-rays to Detect Gum Disease?
- Dentists also rely on dental X-rays to assess damage beneath the surface, especially bone loss that isn’t visible during a clinical exam.
- These X-rays can show horizontal or vertical bone loss, helping the dentist determine the stage of periodontitis and whether surgical intervention may be needed.
- In moderate to severe cases, your dentist may refer you to a periodontist, a gum disease specialist who can evaluate your condition further and propose a treatment plan involving advanced therapies or surgery.
How Can You Treat Gum Disease Effectively?
- Treating gum disease effectively requires a combination of professional dental care and consistent oral hygiene practices at home. The earlier gum disease is diagnosed, the more straightforward the treatment and the better the chances of full recovery—especially during the gingivitis stage.
- Treatment begins with the removal of plaque and tartar, which are the root causes of infection. For early cases, this often means a professional cleaning by a dentist or dental hygienist. However, moderate to severe cases require more intensive procedures.
What Are the Best Treatments for Periodontitis?
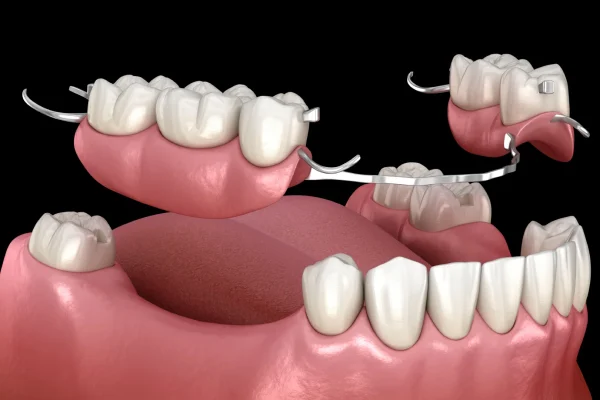
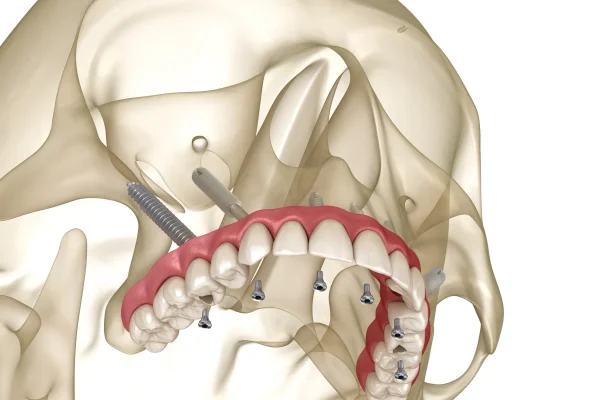
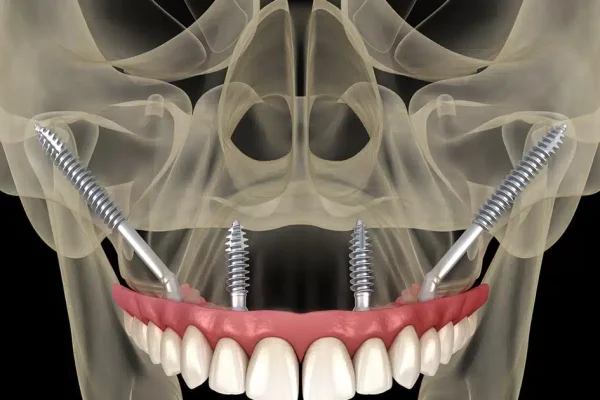
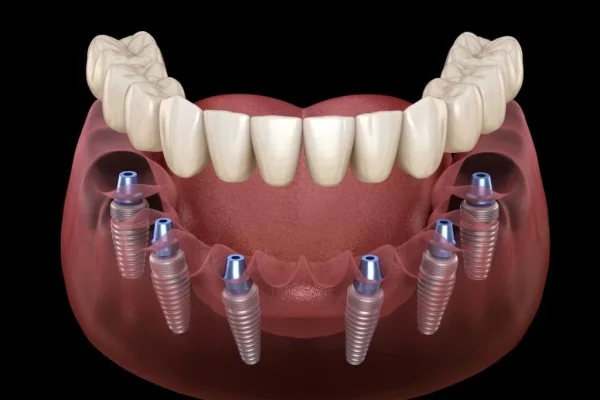
- When gum disease has progressed to periodontitis, treatment typically includes scaling and root planing, as already discussed, but may also involve surgical options if pockets remain deep after non-surgical therapy.
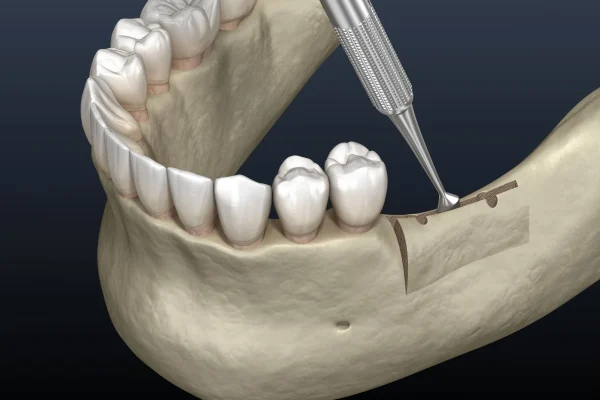
- Flap surgery (pocket reduction surgery): The periodontist lifts the gums to clean the tooth roots more thoroughly and may reshape the bone before suturing the gums back in place. This reduces pocket depth and makes daily cleaning easier.
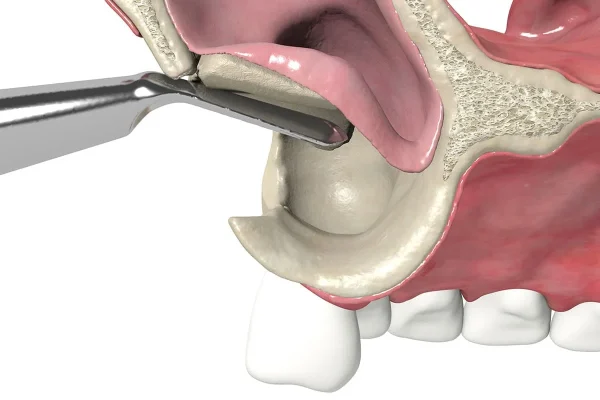
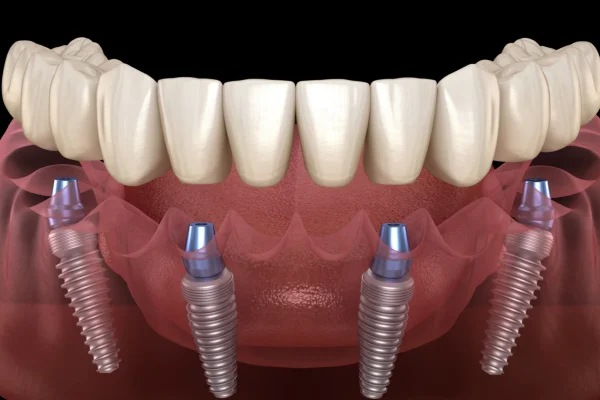
- Bone grafts: If significant bone loss has occurred, grafting procedures use either synthetic, autogenous (your own), or donor bone to help rebuild the lost structure.
- Guided tissue regeneration: This involves placing a membrane between the gum and bone to allow bone to regrow while keeping the gum tissue out.
- Tissue-stimulating proteins: Gels containing proteins that encourage regrowth of bone and gum tissue can be applied directly to the affected area.
- These treatments aim not only to eliminate the infection but also to restore the structural support of teeth and improve gum aesthetics.
What Are the Best Antibiotics or Gels for Gum Infections?
- In cases of severe infection, dentists may prescribe antibiotics to help control bacterial growth in conjunction with mechanical cleaning.
- Common antibiotics include metronidazole, doxycycline, and minocycline. These may be taken orally or applied directly into gum pockets using gels or slow-release microspheres.
- Topical antiseptics, like chlorhexidine gels or mouth rinses, may be recommended for continued use at home, especially following deep cleanings.
- These medications help reduce inflammation, lower bacterial load, and promote healing of gum tissues when used correctly.
Can You Treat Gum Disease at Home Naturally?

- While professional dental treatment is the cornerstone of gum disease management, many people seek ways to complement these efforts with home remedies. It’s important to understand that natural treatments cannot replace dental intervention, especially once gum disease has advanced to periodontitis.
- However, for mild gingivitis, consistent and careful home care can help reverse symptoms and restore gum health.
- Natural remedies may reduce inflammation, ease bleeding, and support tissue healing, but they should be used alongside—not instead of—professional cleaning and guidance.
What Home Remedies Help Heal Gums Faster?
- Salt Water Rinse: One of the oldest and most effective remedies, rinsing with warm salt water can reduce inflammation, soothe sore gums, and help flush out bacteria. Mix ½ teaspoon of salt into a cup of warm water and swish it around your mouth for 30 seconds, twice daily.
- Turmeric Paste: This anti-inflammatory and antimicrobial spice can be mixed with water or coconut oil and applied to the gums to help soothe irritation and reduce bacterial activity.
- Aloe Vera Gel: Known for its healing properties, pure aloe vera gel can be applied directly to inflamed gum tissue to support healing and reduce discomfort.
- Vitamin C and Vitamin D: These nutrients support gum repair and reduce bleeding. Eat foods rich in these vitamins—such as citrus fruits, leafy greens, and fatty fish—or consider a supplement if your intake is low.
- Oil Pulling: Swishing coconut or sesame oil for 10–15 minutes may reduce plaque and bacterial buildup, though scientific evidence is still developing.
Can You Reverse Gum Disease Without a Dentist?
- For early-stage gingivitis, it’s possible to reverse the condition through dedicated oral hygiene: brushing twice daily, flossing, and using antibacterial mouthwash.
- However, periodontitis cannot be reversed at home. Once gum disease causes tissue or bone loss, professional intervention is necessary to prevent further damage.
- Many people mistake reduced bleeding or pain for healing, but gum disease often progresses silently. Routine dental checkups are vital for monitoring and managing the condition.
- In short, you can’t cure moderate to severe gum disease naturally, but you can improve symptoms and slow its progression with consistent, supportive home care.
How Do You Know If You Have Gum Disease?
- Many people don’t realize they have gum disease until it becomes advanced. This is because the early signs of gum problems—like gingivitis—are often painless and subtle. However, knowing what to watch for can help you catch gum disease early and prevent progression to periodontitis.
- This section explains how to recognize gum disease at home and when to seek professional help.
Common Signs People May Notice at Home
- Bleeding when brushing or flossing: If your gums bleed easily during oral hygiene routines, it’s a sign of inflammation—often the first indicator of gingivitis.
- Red or swollen gums: Healthy gums are firm and pink. Infected gums may appear puffy, tender, or red in color.
- Persistent bad breath (halitosis): Bacteria trapped under the gumline can release foul-smelling compounds that lead to chronic bad breath.
- Gum recession: If your teeth appear longer than usual or you feel sensitivity along the gumline, it could mean your gums are pulling away from the teeth.
- Tooth sensitivity or pain: Especially when eating hot or cold foods, sensitivity may occur due to exposed roots from gum recession.
- Loose or shifting teeth: A later-stage sign, this happens when the structures supporting the teeth (gums and bone) weaken.
- Pus or abscesses: A buildup of pus around the gumline is a sign of a serious infection requiring immediate treatment.
Self-Assessment Questions and When to Call a Dentist
- Ask yourself the following:
- Do your gums bleed regularly?
- Have you noticed any gum recession?
- Are your teeth shifting position?
- Does brushing or flossing hurt your gums?
- Do you have constant bad breath?
- If you answer yes to one or more of these, especially if symptoms are persistent or worsening, it’s time to see a dentist.
- A professional exam can confirm whether it’s gingivitis or periodontitis, and guide you toward the right treatment plan.
- Remember: Gum disease can be present without pain, and it often gets worse quietly. Proactive care is the best way to protect your oral health.
How Can You Prevent Gum Disease from Returning?
- Preventing gum disease recurrence is entirely possible with consistent habits and awareness. Once treated, especially in the early stages like gingivitis, the condition can stabilize. However, gum disease, especially periodontitis, is often chronic. That’s why long-term prevention focuses on daily oral care, lifestyle choices, and regular dental monitoring.
- In this section, we explain how to maintain healthy gums for the long haul—even after treatment.
Emphasizing the Importance of Daily Oral Hygiene
- Brush twice a day with fluoride toothpaste: Choose a soft-bristled brush and gently clean all tooth surfaces. Aggressive brushing can damage gums and worsen recession.
- Use proper brushing technique: Tilt the brush at a 45-degree angle toward the gumline and use short, circular motions.
- Floss daily: Flossing is essential to remove plaque between teeth where a brush can’t reach. You can also use water flossers or interdental brushes for more convenience.
- Antimicrobial mouthwash: Using a dentist-recommended mouthwash can help control bacteria and reduce inflammation. Chlorhexidine is often prescribed for short-term use, while over-the-counter rinses with essential oils or cetylpyridinium chloride may be suitable for everyday use.
Can You Prevent Gum Disease If It Runs in Your Family?
- Genetics plays a role, but it’s not destiny: Studies show that some individuals are more genetically predisposed to periodontal issues due to immune response differences.
- Family history means you should be more vigilant: If your parents lost teeth early or had severe gum disease, you might inherit similar vulnerabilities.
- Daily care and lifestyle matter more: Smoking, diet, diabetes, and oral hygiene have a more direct impact. Good habits can often override genetic predisposition.
- Regular checkups are key: High-risk individuals should schedule more frequent cleanings (every 3–4 months instead of every 6). Periodontal monitoring may include probing depth measurements and bone loss evaluations.
Lifestyle Tips to Prevent Recurrence
- Avoid smoking: Tobacco is one of the leading preventable risk factors for gum disease. It reduces oxygen supply to the gums and suppresses healing.
- Limit sugary and starchy foods: These feed harmful bacteria and increase plaque formation.
- Eat nutrient-rich foods: Vitamins C and D are especially important for gum repair and bone health.
- Manage systemic conditions: Conditions like diabetes need to be controlled, as they compromise immune function and healing ability.
What Are the Complications of Untreated Gum Disease?
Untreated gum disease, particularly periodontitis, can cause far more damage than many realize. Beyond bleeding gums or bad breath, it can have serious long-term consequences for both oral and systemic health. This section explores the critical risks associated with ignoring periodontal issues and why early diagnosis and intervention are essential.
How Can Gum Disease Lead to Tooth Loss?
- Destruction of supporting tissues: As periodontitis progresses, it breaks down the ligaments and bone structures that anchor teeth.
- Deep periodontal pockets: These spaces between teeth and gums harbor harmful bacteria, making it increasingly difficult to clean effectively—even with professional help.
- Teeth become loose: Over time, teeth can shift position, become mobile, and eventually fall out or require extraction.
- Loss of bite and function: Missing teeth can impact chewing, nutrition, speech, and even self-confidence.
What Are the Systemic Effects of Periodontal Disease?
- Increased cardiovascular risk: Research has found a strong link between gum disease and heart problems, such as atherosclerosis (hardening of the arteries), due to chronic inflammation.
- Diabetes complications: Gum disease can make it more difficult to control blood sugar levels, while high blood glucose can worsen gum inflammation—creating a vicious cycle.
- Adverse pregnancy outcomes: Pregnant individuals with gum disease may have a higher risk of preterm birth and low birth weight.
- Potential respiratory issues: Bacteria from the mouth can be aspirated into the lungs, increasing the risk of pneumonia in vulnerable populations.
- Links to cognitive decline: Emerging studies have suggested an association between periodontal pathogens and diseases like Alzheimer’s, although more research is needed.
Other Common Complications of Gum Disease
- Gum abscesses: These painful infections can form around the roots of teeth when bacteria become trapped in deep pockets.
- Chronic halitosis: Ongoing bad breath, often caused by decaying food and bacteria under the gums, can be socially and psychologically distressing.
- Jawbone deterioration: Untreated periodontitis leads to bone loss in the jaw, which may affect future options for implants or dentures.
- Receding gums: As tissue pulls back, it exposes the tooth roots, leading to sensitivity and increased risk of decay.
By understanding the full scope of risks, patients are more likely to take gum disease seriously. Prevention and early treatment remain the best strategy to avoid these life-altering complications.
What Are the Best Products to Use for Gum Disease?

Choosing the right products for managing gum disease is an essential part of both treatment and prevention. While professional intervention is often necessary—especially for moderate to severe cases—the tools and products used at home play a pivotal role in controlling plaque and reducing inflammation.
What Toothpaste and Mouthwash Help With Gum Disease?
- Toothpastes formulated for gum health: Products like Parodontax and Colgate Total contain antibacterial ingredients such as stannous fluoride and triclosan, which help fight plaque and reduce gum bleeding.
- Prescription-strength pastes: In more advanced cases, dentists may recommend toothpaste containing higher fluoride concentrations or antibacterial agents.
- Mouthwashes with antimicrobial ingredients: Chlorhexidine gluconate is a gold standard for short-term use to reduce bacterial loads, often prescribed after scaling or surgery.
- Over-the-counter options: Brands like LISTERINE® offer alcohol-free mouthwashes containing essential oils like thymol, menthol, and eucalyptol which target harmful bacteria and promote fresh breath.
- Important note on usage: Chlorhexidine should not be used for extended periods without dentist supervision due to side effects such as staining and altered taste.
What Are the Best Antibiotics or Gels for Gum Infections?
- Topical antibiotic gels: Gels like metronidazole or doxycycline can be inserted into periodontal pockets to fight infection locally. These are especially useful for isolated pockets that don’t respond to cleaning alone.
- Minocycline microspheres: Marketed under brands like Arestin, these are placed into pockets and slowly release antibiotics over several days.
- Oral antibiotics: In severe or spreading infections, systemic antibiotics like amoxicillin, clindamycin, or metronidazole may be prescribed.
- Enzyme suppressants: Low-dose doxycycline can be used long-term to suppress collagenase—an enzyme responsible for tissue destruction in periodontitis.
- Benefits of localized treatment: These products minimize side effects compared to systemic antibiotics and deliver medication precisely where it’s needed.
Recommended Dental Tools and Accessories
- Soft-bristled toothbrushes: These are gentle on inflamed gums and effective at removing plaque without causing further irritation.
- Electric toothbrushes: Models with oscillating-rotating technology (like Oral-B) are particularly effective at plaque removal in hard-to-reach areas.
- Interdental brushes and floss: Essential for removing plaque between teeth where toothbrush bristles can’t reach. TePe and GUM® brand brushes are widely recommended.
- Water flossers: Devices like Waterpik help flush out food particles and bacteria from periodontal pockets with pulsating streams of water.
- Tongue scrapers: Reducing bacteria on the tongue can also help manage halitosis and maintain overall oral hygiene.
By using these dentist-recommended products consistently, patients can significantly improve their gum health and support the effectiveness of clinical treatments.
Can Children Get Gum Disease and How Is It Treated?
Gum disease is often associated with adults, but it’s important to recognize that children and adolescents can also be affected. While advanced periodontal disease is rare in younger populations, early forms like gingivitis are common and should not be ignored. Timely intervention and good oral hygiene education can prevent long-term damage.
Why Are Children at Risk of Gum Disease?
- Poor brushing habits: One of the most frequent causes of gingivitis in children is inconsistent or improper brushing and flossing. Plaque builds up around the gumline, leading to inflammation.
- Puberty gingivitis: Hormonal changes during puberty can increase blood flow to the gums, making them more sensitive and reactive to even small amounts of plaque. This condition is temporary but requires careful oral hygiene.
- Orthodontic appliances: Braces and retainers make it harder to clean all tooth surfaces, increasing the risk of plaque accumulation and gum irritation.
- Dietary habits: Frequent consumption of sugary snacks and drinks fuels bacterial growth and acid production, contributing to plaque buildup.
- Mouth breathing: Children who breathe through their mouths often develop dry gums, which can become inflamed and irritated.
What Are the Signs of Gum Disease in Children?
- Bleeding when brushing or flossing
- Red or swollen gum tissue
- Persistent bad breath despite brushing
- Gum recession or “longer-looking” teeth
- Sensitivity when eating or drinking
Early signs are often dismissed as “normal” or “temporary” by parents, which is why regular dental check-ups are essential.
How Is Gum Disease Treated in Children?
- Professional cleaning: The first step in treating gingivitis in children is a gentle but thorough cleaning performed by a dentist or hygienist. This removes plaque and tartar that home care may miss.
- Oral hygiene education: Children are taught how to brush properly using circular motions and to floss daily. Using kid-friendly electric toothbrushes can increase engagement and improve results.
- Antibacterial mouth rinses: Mild antimicrobial rinses may be prescribed in older children to reduce bacterial levels and inflammation, especially during orthodontic treatment.
- Dietary guidance: Reducing sugary snacks and increasing water intake helps lower bacterial activity in the mouth.
- Parental involvement: Parents play a crucial role in overseeing daily brushing and flossing, especially for younger children who may lack the manual dexterity to clean thoroughly.
When Should a Specialist Be Consulted?
- Aggressive periodontitis: Although rare, some children develop more severe forms of periodontal disease that progress rapidly. These may require referral to a pediatric periodontist.
- Systemic links: Gum disease in children can be associated with systemic conditions like diabetes or immune deficiencies. A multidisciplinary approach may be needed for proper diagnosis and management.
Proactive care in childhood sets the foundation for lifelong oral health. With early detection, proper treatment, and preventive habits, gum disease in children is manageable and often reversible.
How Do You Recover After Gum Disease Treatment?
Recovering from gum disease treatment is a critical phase in achieving long-term oral health. Whether you’ve undergone non-surgical procedures like scaling and root planing or more advanced surgical interventions, the recovery process requires specific care and attention to ensure proper healing and to prevent a recurrence of infection.
What Should You Expect After a Deep Cleaning or Surgery?
- Mild discomfort and sensitivity: After scaling and root planing, it’s common to experience some soreness, sensitivity to temperature, or even slight bleeding. These effects usually subside within a few days.
- Swelling or inflammation: Some patients may notice mild gum swelling, especially if the treatment involved deeper cleaning or flap surgery.
- Tightness in the gums: As the inflamed tissue heals and adheres back to the tooth surface, your gums may feel tighter than before, especially in areas where pockets have been reduced.
How Can You Care for Your Gums Post-Treatment?
- Follow your dentist’s instructions carefully: These may include prescribed mouth rinses like chlorhexidine or instructions on when to resume brushing and flossing.
- Use a soft-bristled toothbrush: It’s crucial to avoid aggressive brushing. A soft-bristled or electric toothbrush with gentle pressure is recommended to prevent irritating healing tissue.
- Avoid hot, spicy, or crunchy foods: These can aggravate sensitive gums during the first few days of recovery.
- Stick to a bland, soft diet: Foods like mashed potatoes, soup, scrambled eggs, and smoothies are soothing and reduce mechanical irritation on the gums.
- Apply cold compresses (if advised): This helps to minimize swelling and ease discomfort after surgical procedures.
Are There Medications or Products That Help Healing?
- Over-the-counter pain relievers: Ibuprofen or paracetamol can reduce post-treatment discomfort and inflammation.
- Antibacterial mouthwashes: Your periodontist may recommend chlorhexidine or hydrogen peroxide-based rinses to help control bacteria during healing.
- Healing gels: Some dentists apply tissue-regenerating gels with growth factors after surgery to enhance healing and minimize discomfort.
- Antibiotics: In more severe or high-risk cases, oral antibiotics may be prescribed to prevent infection during recovery.
What Should You Monitor During Healing?
- Watch for signs of infection: Persistent swelling, pus, or severe pain beyond the first few days may indicate complications. Always notify your dental professional if these arise.
- Track gum reattachment: Your dentist may remeasure pocket depths in a follow-up visit to assess how well the gums are healing and reattaching to the teeth.
- Expect some gum recession: As inflammation reduces, the gums may shrink slightly. This is a normal part of the healing process, though it may expose more tooth surface.
How Can You Support Long-Term Recovery?
- Keep up with professional cleanings: Your dentist will likely recommend maintenance cleanings every 3–4 months instead of every 6.
- Practice daily oral hygiene: Proper brushing, flossing, and rinsing are essential to prevent reinfection and maintain the results of treatment.
- Stay hydrated and nourished: A healthy diet and adequate water intake can support tissue regeneration and immune response.
- Avoid smoking and alcohol: These hinder healing and dramatically increase the risk of recurring periodontal disease.
Frequently Asked Questions About Gum Disease

In this section, we answer the most commonly asked questions about gum disease, including misconceptions, treatment outcomes, and what patients can realistically expect when managing or attempting to cure this condition.
What Is the Best Treatment for Gum Disease?
- The best treatment depends on the stage of the disease: Gingivitis, the early stage of gum disease, is best treated through improved oral hygiene and professional cleanings. Periodontitis requires more advanced interventions like scaling and root planing, antibiotics, or even surgery.
- Non-surgical methods are ideal for early cases: If caught early, deep cleaning (scaling and root planing) and good home care may be enough to reverse symptoms and stabilize the condition.
- Advanced cases may need surgical solutions: When deep pockets persist or bone loss is significant, treatments such as flap surgery, bone grafts, soft tissue grafts, or guided tissue regeneration become necessary.
- Laser therapy is emerging as a minimally invasive alternative: In selected cases, lasers can help remove infected tissue and promote healing with less discomfort than traditional surgery.
- Ongoing maintenance is part of the treatment: Gum disease is chronic, meaning regular periodontal maintenance every 3 to 4 months is critical to prevent relapse.
- Customized plans offer the best results: Dentists or periodontists tailor treatment based on pocket depth, bone level, patient health, and lifestyle factors like smoking or diabetes.
Can You Cure Gum Disease Without a Dentist?
- Early gingivitis can be reversed at home: Improving brushing and flossing, using antibacterial mouthwash, and adopting better dietary habits can reduce mild gum inflammation and bleeding.
- Periodontitis cannot be cured at home: Once the disease progresses to bone loss and gum detachment, only professional care can clean below the gumline and halt the disease.
- Home remedies help support healing—not replace treatment: Rinses like saltwater or hydrogen peroxide, and natural agents like turmeric or aloe vera, may reduce inflammation but won’t eliminate harmful bacteria under the gums.
- Skipping the dentist may lead to irreversible damage: Avoiding dental care risks worsening the infection, leading to abscesses, tooth loss, and jawbone destruction.
- Dentist involvement ensures correct diagnosis: Many signs of gum disease are subtle and easily missed. A dentist uses probing and X-rays to detect issues that aren’t visible or painful yet.
Ongoing monitoring is key: Even if symptoms improve at home, regular check-ups help catch flare-ups before they lead to permanent damage.