What Is a Single Tooth Implant and Why Should You Consider One?

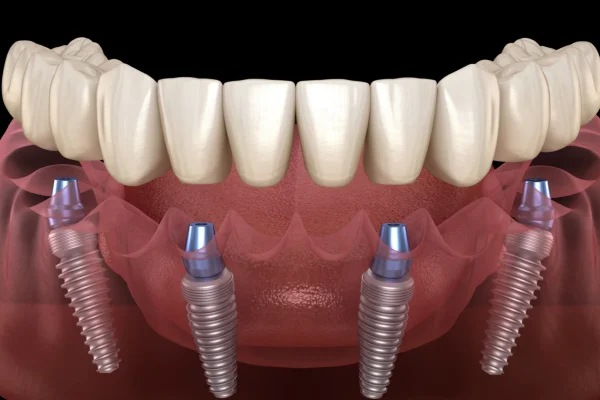
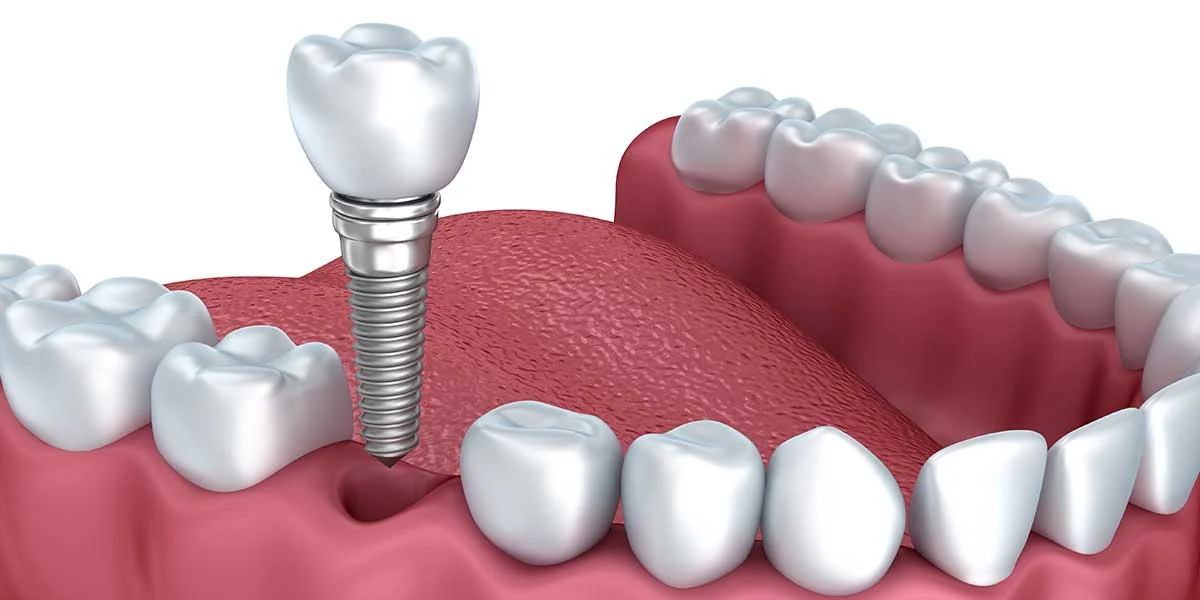
A single tooth dental implant is a modern, reliable solution for replacing a missing tooth — one that closely mimics the look, feel, and function of your natural teeth. It is composed of three main components: a titanium screw that acts as the artificial root, an abutment that connects the screw to the visible part, and a custom-made crown that replicates the appearance of your lost tooth.
This procedure is ideal for patients who have lost a tooth due to trauma, decay, or gum disease but still have healthy surrounding teeth and sufficient bone in the jaw. One of the standout reasons people choose a single tooth implant over other options like bridges or partial dentures is its ability to stand alone without altering neighboring teeth. Traditional bridges often require the adjacent teeth to be filed down to support the restoration, which can compromise their long-term health. Implants, on the other hand, preserve these natural teeth.
There are several compelling reasons to consider this type of implant. First, it delivers aesthetic confidence by filling in unsightly gaps and blending in seamlessly with your remaining teeth. Patients often report significant improvements in self-esteem and social confidence after undergoing the procedure.
Second, a single implant helps maintain oral health by stimulating the jawbone in the same way a natural tooth root would, preventing bone loss and the shifting of adjacent teeth. This helps maintain your facial structure and bite alignment, which can deteriorate over time with untreated tooth loss.
Third, it offers durability and stability unmatched by traditional tooth replacement methods. With proper care, a single tooth implant can last 15–25 years or more, often making it a cost-effective solution in the long run.
Candidates for a single tooth implant typically include healthy adults with good oral hygiene and sufficient bone density. Those with uncontrolled diabetes, heavy smoking habits, or severe gum disease may need to address these conditions before becoming eligible.
Is a Single Tooth Dental Implant Worth It? Key Advantages Explained
When considering whether to invest in a single tooth dental implant, one of the most common questions is: Is it worth it? The short answer is yes — for most patients, the benefits of a single implant far outweigh the initial cost or complexity of the procedure. Let’s break down the key advantages that make this treatment one of the most preferred solutions in modern restorative dentistry.
✅ Long-Term Value Compared to Other Options
- Single tooth implants are designed to last 15 years or more, and often a lifetime with proper care, unlike dental bridges which may need replacement every 7–10 years.
- Implants are made of durable materials like titanium and porcelain, which are resistant to decay and daily wear.
- Over time, their longevity can make them more cost-effective than replacing bridges or dealing with the discomfort of partial dentures.
✅ Improved Lifestyle and Daily Comfort
- Eating, speaking, and smiling all become more natural and effortless compared to removable solutions.
- Since implants are securely fixed in the jaw, there’s no worry of slipping or discomfort while chewing, as may happen with dentures.
- Many patients report a boost in self-confidence, especially when the implant blends perfectly with their natural teeth.
✅ Preserving Jawbone Health and Preventing Teeth Shifting
- Tooth loss can lead to jawbone resorption, where the bone shrinks due to lack of stimulation. Implants solve this by acting like natural tooth roots, keeping the bone active.
- This also prevents adjacent teeth from shifting, which can lead to bite misalignment and increased dental problems.
✅ Aesthetic and Functional Superiority
- The crown placed on a single tooth implant is custom-made to match the color, shape, and size of your existing teeth, ensuring a seamless appearance.
- You regain full biting power without compromising nearby teeth, which is often required when placing a bridge.
✅ Independence From Surrounding Teeth
- Unlike a bridge, which uses adjacent teeth as anchors (and may require them to be filed down), a single implant is freestanding — it replaces just the missing tooth without affecting the others.
How Long Does a Single Tooth Implant Last and What Affects Its Durability?
A common concern among patients considering dental implants is: How long does a single tooth implant last? The good news is that single tooth implants are one of the most durable and reliable dental treatments available today. With proper care, they can last decades — and in many cases, a lifetime. However, several factors can influence the actual lifespan of your implant.
✅ Average Lifespan of a Single Tooth Implant
- On average, dental implants last 15 to 25 years, though many last much longer when patients follow recommended dental hygiene routines and attend regular checkups.
- The crown (the visible part of the implant) may need to be replaced sooner, typically every 10–15 years, depending on wear and tear.
✅ Key Factors That Influence Longevity
- Oral hygiene: Daily brushing, flossing, and the use of interdental brushes or water flossers help maintain gum health and prevent infections that can jeopardize the implant.
- Bone health: A healthy jawbone is essential for implant stability. Conditions like osteoporosis or untreated gum disease may reduce implant longevity.
- Smoking: Smokers have a significantly higher risk of implant failure. Smoking affects blood circulation and bone healing, making it harder for the implant to integrate properly.
- Teeth grinding (bruxism): Excessive grinding puts pressure on the implant and may cause the crown or even the implant post to become damaged or loosen over time.
- Diet: While implants allow you to eat most foods comfortably, consistently chewing very hard items (like ice or unpopped popcorn kernels) can cause crown fractures.
✅ Comparison With Bridges and Dentures
- Dental bridges typically last 5 to 15 years, and they rely on the support of neighboring teeth, which may deteriorate over time.
- Removable dentures may need replacement or adjustment every 5 to 8 years, and they do not protect against jawbone loss.
- In contrast, single implants are self-sufficient, preserve jawbone integrity, and require no alteration to surrounding teeth.
✅ Proactive Maintenance for Extended Longevity
- Regular visits to the dentist for professional cleaning and implant inspection are essential.
- Address any early signs of implant issues, like gum irritation or bite discomfort, promptly to prevent complications.
What Is the Procedure for a Single Tooth Implant? Step-by-Step Timeline
Understanding the timeline and steps of a single tooth implant procedure is crucial for patients who want to plan their treatment journey. This process involves multiple phases, from initial consultation to final crown placement, and although it spans several months, each step ensures long-term success and natural aesthetics.
What Happens During the First Consultation?
- Comprehensive oral examination: Your dentist will assess your overall dental health, focusing on the area where the tooth is missing or needs to be replaced.
- Imaging tests: X-rays, panoramic radiographs, and 3D CT scans are taken to evaluate bone density, root placement, and nerve locations to determine if you are a suitable candidate.
- Medical review: The dentist will review your medical history and medications to ensure there are no contraindications for surgery, such as uncontrolled diabetes or immune disorders.
- Treatment planning: Using imaging data, your dentist will create a customized treatment plan, including the size, type, and placement of the implant.
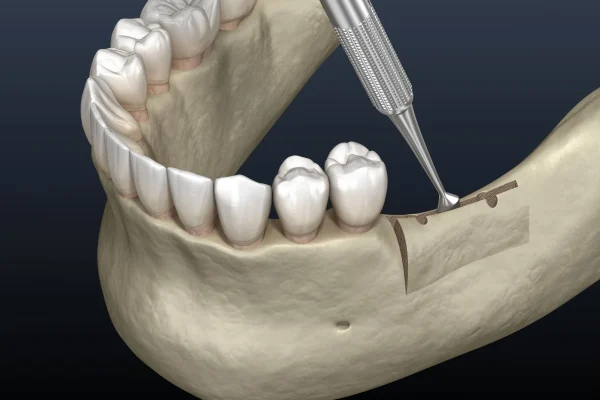
How Is the Implant Surgically Placed?
- Anesthesia and sedation: The procedure is performed under local anesthesia, though some clinics offer IV sedation for anxious patients.
- Placement of the implant: A small incision is made in the gum to expose the jawbone, where a titanium screw (implant post) is inserted precisely into the bone.
- Healing cap and stitches: A healing cap is placed on top of the implant to guide the gum tissue’s growth, and the gum is sutured to promote healing.
How Long Does It Take for the Implant to Heal?
- Osseointegration: This crucial phase lasts between 2 to 6 months, during which the jawbone fuses with the titanium implant. This creates a stable foundation.
- Healing process: Minor swelling or bruising is normal. Patients should avoid smoking, alcohol, and hard foods during this period.
- Temporary options: If the gap affects your smile, a temporary crown or removable partial denture may be used during the healing phase.
What Happens When the Crown Is Attached?
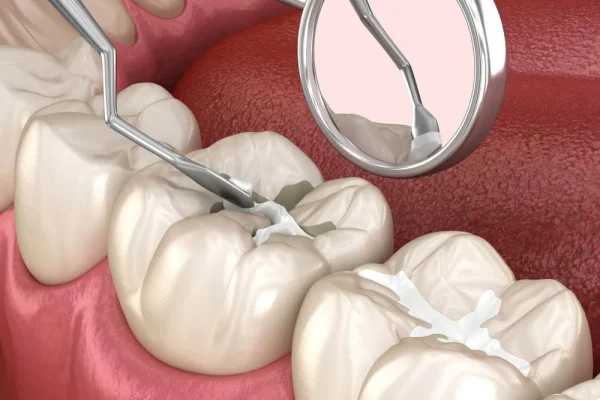
- Abutment placement: Once the implant has fully healed, the healing cap is removed and replaced with an abutment (connector piece).
- Impressions and color matching: Your dentist will take impressions or digital scans and match the color of your new tooth to your natural dentition.
- Crown fitting: The custom-made crown is attached to the abutment, and your bite is adjusted to ensure comfort and function.
Is the Single Tooth Implant Procedure Painful or Uncomfortable?
One of the most common concerns for patients considering dental implants is the level of pain or discomfort they might experience during and after the procedure. The good news is that advancements in dental implant techniques, anesthesia, and aftercare have significantly minimized pain, making the process more manageable and predictable than ever.
Pain Levels During and After Surgery
- During the procedure: Thanks to local anesthesia, patients typically feel little to no pain while the implant is being placed. The area is numbed completely, and many clinics also offer sedation dentistry options for those with dental anxiety.
- After the surgery: Mild to moderate discomfort is normal and usually peaks within the first 24 to 48 hours. Pain can be managed effectively with over-the-counter painkillers such as ibuprofen or acetaminophen.
- Swelling and bruising: Some swelling in the gums and cheeks and minor bruising around the implant site are common, especially within the first few days post-surgery.
Use of Anesthesia and Post-Operative Pain Management
- Types of anesthesia: Most procedures use local anesthesia, but options such as IV sedation or oral sedatives are available for patients who require additional comfort.
- Pain control: Dentists often prescribe pain medications and may recommend using a cold compress to reduce swelling and discomfort.
- Diet and rest: A soft food diet, avoiding hot beverages, and resting for the first 24–48 hours are all essential parts of the post-operative protocol to ease discomfort.
Normal Discomfort vs. Signs of Complications
- What’s normal: Slight pain when chewing, minor bleeding, and gum tenderness for a few days are all part of the normal healing process.
- When to worry: Intense pain that does not subside, persistent swelling, pus discharge, or fever could indicate an infection or other complication.
- What to do: If you experience unusual symptoms, it’s important to contact your implant dentist immediately to prevent implant failure or additional health risks.
In summary, while a single tooth implant procedure is a form of oral surgery, the discomfort is typically short-lived and manageable. With the right pain management plan and proper post-operative care, most patients report only mild discomfort and are able to return to normal activities within a few days.
What Are the Common Side Effects and Risks of Dental Implants?
While single tooth dental implants are considered a safe and effective solution for missing teeth, like any surgical procedure, they come with potential side effects and risks. Being informed about what to expect can help patients manage healing properly and identify when professional attention is needed.
Swelling, Bruising, and Gum Sensitivity
- Post-operative swelling: It is normal to experience swelling around the gums and face within the first few days after the implant surgery. This is the body’s natural response to the surgical procedure and usually resolves within 3–5 days.
- Bruising: Minor bruising may appear on the cheek or gum tissue near the implant site. This is also common and temporary.
- Gum sensitivity: The surgical site will likely be tender to the touch, especially when eating or brushing. This typically subsides as healing progresses.
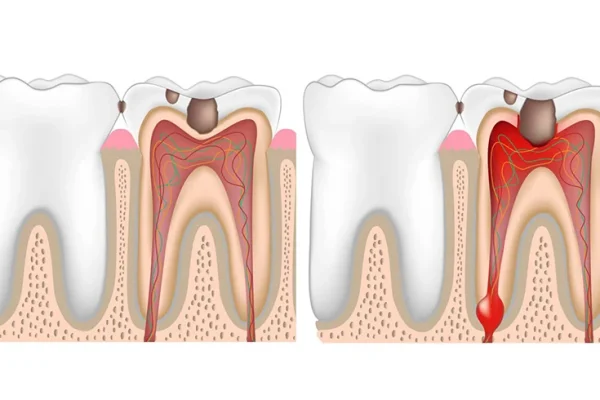
Potential for Infection or Implant Rejection
- Infection risks: One of the most common complications is infection at the implant site. This can occur if bacteria enter the surgical area during or after the procedure.
- Signs of infection: Symptoms include persistent pain, swelling, pus, fever, or foul odor from the implant site. These should be evaluated promptly.
- Implant failure or rejection: Although rare, an implant may not properly integrate with the jawbone, especially in patients who smoke, have poor oral hygiene, or suffer from uncontrolled diabetes.
- Preventive measures: Following strict hygiene protocols, attending follow-up appointments, and quitting smoking can drastically reduce these risks.
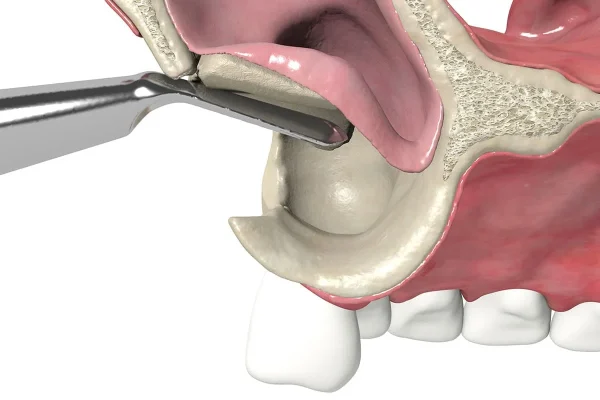
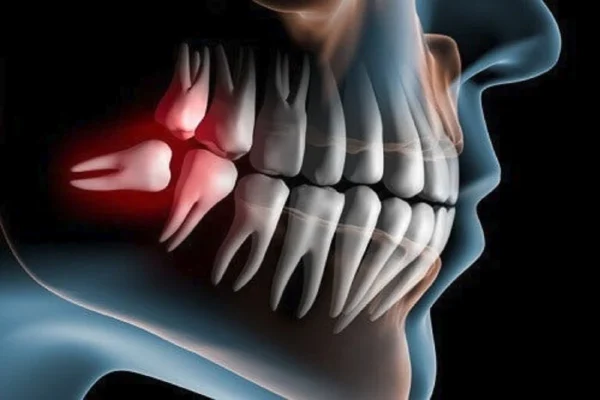
Nerve and Sinus Complications (Rare)
- Nerve damage: Improper placement of the implant can, in very rare cases, impinge on surrounding nerves, leading to numbness, tingling, or pain in the chin, lips, or tongue.
- Sinus issues: For implants placed in the upper jaw, especially the molar region, there is a small risk of the implant protruding into the sinus cavity if not placed correctly.
- Avoidance through precision planning: Thorough diagnostic imaging (such as CBCT scans) and planning by experienced implantologists minimizes these risks.
How to Minimize Risks Through Professional Care
- Choose a qualified specialist: Ensure your dental implant is placed by a trained and experienced implantologist, oral surgeon, or periodontist.
- Pre-operative evaluation: Comprehensive assessment of bone density, medical history, and gum health is critical.
- Post-op instructions: Carefully follow all aftercare guidelines, including dietary restrictions and oral hygiene routines.
- Regular follow-ups: Continued monitoring ensures the implant is healing correctly and allows early detection of complications.
How Much Does a Single Tooth Implant Cost and What Factors Affect It?
Understanding the cost of a single tooth implant is essential for anyone considering this long-term solution. While dental implants are more expensive upfront compared to bridges or dentures, they offer unmatched durability, aesthetics, and function. Several factors influence the total cost, and knowing these can help patients budget more effectively and explore financing options.
Average Price Ranges in Various Regions
- United States: On average, a single dental implant costs between $3,000 and $5,000, including the implant post, abutment, and crown.
- United Kingdom: Prices typically range from £2,000 to £2,800 depending on the clinic’s location and the materials used.
- Australia: Expect to pay around AUD $3,000 to $6,500 per implant, often higher in metropolitan areas.
- Albania: The average price for a single tooth dental implant in Albania ranges between €400 and €700, depending on the clinic, implant brand, and the complexity of the procedure.
- Thailand and Turkey: Popular dental tourism destinations, with prices ranging from $1,000 to $2,000, including consultation, surgery, and prosthetics.
Prices vary widely due to differences in clinic overheads, specialist fees, technology used, and cost of living in each country or city.
Cost Components: Consultation, Surgery, Abutment, Crown
- Consultation: Includes clinical exams, x-rays, 3D scans, and treatment planning. This can cost $100–$500, sometimes included in package deals.
- Implant surgery: The placement of the titanium post is the core procedure, ranging from $1,000 to $2,500.
- Abutment: This connector, often custom-made, adds $300–$600 to the bill.
- Crown: Typically porcelain or zirconia, the crown may cost $1,000–$2,000, depending on aesthetics and lab quality.
Many clinics offer all-inclusive packages that bundle these components at a slight discount.
Factors That Impact Price (Materials, Clinic, Location)
- Material quality: Titanium implants are standard, but zirconia or high-end ceramic options can increase cost.
- Clinic reputation: Premium dental centers with advanced equipment and digital labs charge more but offer enhanced precision and outcomes.
- Practitioner’s experience: Highly qualified implantologists or specialists may command higher fees but also reduce the risk of complications.
- Additional procedures: Bone grafting, sinus lifts, or extractions will add to the cost.
Discuss Insurance and Financing Options
- Insurance coverage: Many dental insurance plans do not fully cover implants, classifying them as cosmetic. However, some may partially cover the crown or surgery.
- Payment plans: Clinics often provide 0% APR financing over 12–24 months, making the investment more manageable.
- Dental tourism: Traveling abroad for dental implants can reduce costs significantly, though it requires careful vetting of the clinic.
Can One Implant Replace More Than One Tooth?
Many patients wonder if a single dental implant can replace more than one missing tooth—especially when facing gaps that involve adjacent or multiple teeth. While single tooth implants are designed for one-to-one tooth replacement, there are certain scenarios where one implant can support more than one tooth. Understanding the biomechanics, risks, and alternatives is key to making the right treatment choice.
Situations Where a Single Implant Supports Two Crowns
- Cantilever bridges: A single implant may support a two-unit cantilever bridge, where the second crown is “suspended” from the implant-supported crown.
- Condition for success: This approach is only considered when the missing teeth are adjacent and in low-stress areas (like lateral incisors) to avoid overload on the implant.
- Clinical risk: While cost-effective, cantilever bridges can introduce uneven force distribution, increasing the risk of implant failure if not carefully planned.
Difference Between Single Implants and Implant Bridges
- Single implants: One implant for one tooth. Offers independent support and avoids stress on adjacent teeth.
- Implant bridges: Two or more implants placed to support a larger span of multiple missing teeth (usually three or more).
- Comparison:
- Stability: Bridges offer better long-term stability when replacing several teeth.
- Cost: Fewer implants = lower cost, but long spans may still require multiple posts.
- Hygiene: Cleaning is easier with single implants than with connected bridgework.
Structural Limitations and Risks
- Bone support: A single implant bearing two crowns requires excellent bone density and volume to prevent overload and loosening.
- Stress concentration: Uneven biting forces on multiple teeth supported by one implant can cause micromovement, bone loss, or even fracture of the restoration.
- Patient selection: Not suitable for bruxism (teeth grinding) patients or in high-chewing-pressure areas like molars.
Alternatives for Multi-Tooth Gaps
- Two separate implants: If budget allows, placing one implant per missing tooth remains the gold standard.
- Implant-supported bridge: Ideal when three or more adjacent teeth are missing—usually requiring two implants to anchor the span.
How Many Teeth Can Be Supported by One Dental Implant?
While dental implants are most commonly used in a one-to-one tooth replacement approach, advancements in implantology have enabled single implants to support multiple teeth under the right conditions. However, this depends on various clinical factors, and the design must be carefully engineered for long-term success.
Standard Use of Implants for One-to-One Replacement
- Default practice: The standard protocol in implant dentistry is one implant per tooth, especially for front teeth or single gaps. This ensures optimal load distribution and natural esthetics.
- Superior strength: A single implant provides a solid root replacement and allows for precise control over the crown’s alignment, angulation, and appearance.
- Preserves surrounding teeth: Unlike traditional bridges, single implants don’t require adjacent teeth to be reshaped or involved in the support process.
Cases Involving Implant-Supported Bridges or Dentures
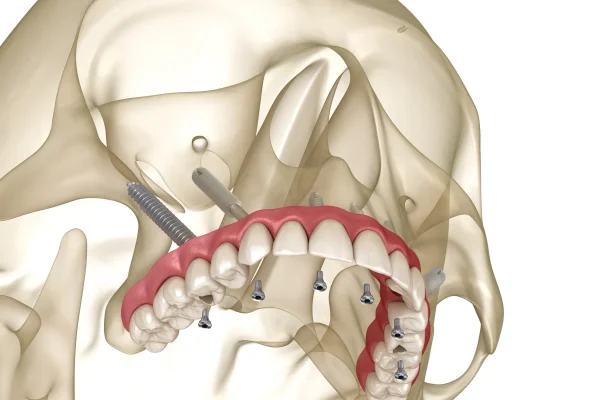
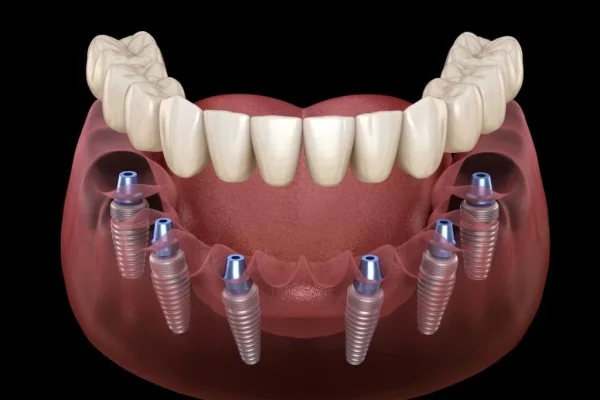
- Implant-supported bridges: When replacing multiple missing teeth (typically three or more), two implants can anchor a bridge that spans the gap. For example, two implants might support three or four crowns joined together.
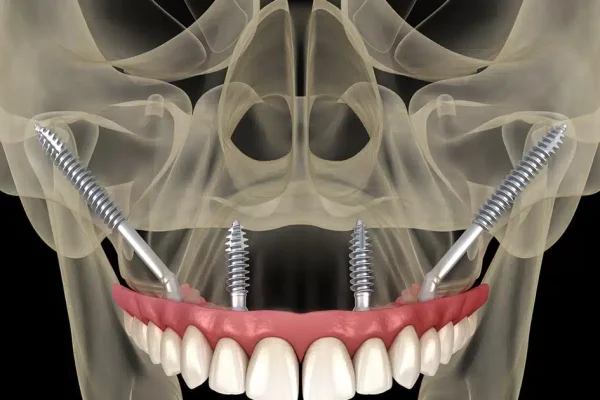
- Full-arch solutions: In cases of full mouth restoration, four to eight implants may support an entire arch of 10 to 14 teeth. Systems like All-on-4 or All-on-6 leverage strategic implant placement to restore full function and esthetics.
- Overdentures: In patients with extensive tooth loss, two to four implants can support removable dentures, significantly enhancing stability compared to traditional dentures.
Clarify Misconceptions About Multi-Tooth Support Per Implant
- Not always viable: Although it’s technically feasible, placing multiple crowns on a single implant (especially in high-stress chewing areas) is generally avoided due to biomechanical limitations.
- Force distribution: Each tooth in the mouth plays a role in absorbing bite forces. Asking one implant to carry the load of several teeth increases the risk of mechanical failure or bone resorption.
- Individual assessment required: Your dentist must evaluate jawbone health, bite alignment, and aesthetic goals before deciding if one implant can support more than one tooth.
What Are the Alternatives to a Single Tooth Implant?
While single tooth dental implants are often considered the gold standard for tooth replacement, they are not the only solution available. Patients may have different needs, budgets, or medical conditions that make alternative treatments more suitable. Understanding these options can help you make an informed decision in collaboration with your dentist.
Dental Bridges: Pros and Cons
- What they are: A dental bridge involves creating a false tooth (pontic) held in place by crowns affixed to the adjacent healthy teeth.
- Pros:
- Faster procedure: Unlike implants, which require healing time, bridges can often be completed in two visits.
- Lower upfront cost: Bridges generally cost less than implants, making them attractive to patients on a budget.
- Non-surgical: No surgical intervention is required, which is beneficial for medically compromised patients.
- Cons:
- Affects adjacent teeth: To place the bridge, your dentist must file down neighboring teeth—even if they are healthy.
- Bone loss continues: Bridges don’t stimulate the jawbone, potentially leading to bone resorption over time.
- Shorter lifespan: Dental bridges may need replacement every 10–15 years, while implants can last much longer.
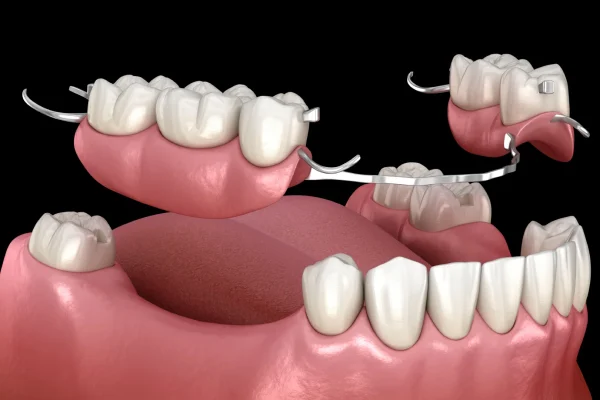
Removable Partial Dentures
- What they are: These are custom-made, removable appliances that replace one or more missing teeth.
- Pros:
- Affordable: This is the least expensive option for replacing missing teeth.
- Non-invasive: Ideal for those who cannot undergo surgery due to health issues.
- Quick turnaround: They can be fabricated quickly compared to implant procedures.
- Cons:
- Stability issues: They may shift or move during eating and speaking.
- Aesthetics: Often bulkier and less natural-looking than fixed options.
- Maintenance: Require daily removal and cleaning, which some patients find inconvenient.
Resin-Bonded Bridges (Maryland Bridges)
- What they are: A conservative type of bridge that uses metal or porcelain wings bonded to the back of adjacent teeth.
- Pros:
- Minimally invasive: No need to reshape neighboring teeth significantly.
- Aesthetic: Often used for front teeth due to their natural appearance.
- Cons:
- Limited durability: Not suitable for areas with high biting force.
- Risk of debonding: The bonded wings can become loose over time.
When Each Is Preferred Over Implants
- Budget constraints: Partial dentures or bridges are often recommended for patients unable to afford implants.
- Health limitations: Patients with conditions like uncontrolled diabetes or severe bone loss may not be suitable for implants.
- Temporary solutions: Young patients who are still growing may use bridges or dentures until they are eligible for implants.
Can You Get a Single Tooth Implant at Any Age?
Single tooth dental implants are a versatile solution, but age can play a critical role in determining whether or not someone is an ideal candidate. While implants are widely used in adults of all ages, there are some considerations—especially at the extremes of the age spectrum—that both patients and dentists should understand.
Age Considerations for Implant Candidates
- Minimum age: Implants are typically not recommended for individuals under the age of 18. This is because the jawbone must be fully developed to ensure the implant integrates correctly and remains stable.
- Bone maturity: In younger patients, premature implant placement can result in alignment issues as the jaw continues to grow, causing the implant to shift or appear misaligned.
- Custom treatment planning: In cases of trauma or congenital absence of a tooth, dentists may consider temporary solutions like resin-bonded bridges or partial dentures until the jaw is fully matured.
Differences Between Young Adults and Older Adults
- Young adults (20s–40s): Generally healthy and with good bone density, younger patients are typically ideal candidates for single tooth implants. Healing tends to be quicker, and long-term success rates are high.
- Middle-aged adults (40s–60s): Many patients in this range choose implants as a long-term investment after tooth loss from trauma, decay, or failed root canals. The success of implants in this group is also very high, especially when paired with good oral hygiene.
- Older adults (60s and beyond): Contrary to common belief, there is no upper age limit for implants. In fact, many older patients benefit from implants as a stable, functional, and aesthetic alternative to dentures. As long as the individual has good general and oral health, age itself is not a limiting factor.
Bone Health and Growth Plate Closure in Teens
- Bone growth evaluation: Before placing an implant in a teenager, dentists use X-rays or 3D imaging to determine if the growth plates in the jaw have closed. This step is crucial to ensure proper long-term positioning of the implant.
- Alternative approaches: In growing teens, space maintainers or temporary crowns can be used until implant placement becomes viable.
Medical and Lifestyle Considerations Regardless of Age
- Bone density and volume: At any age, the success of an implant depends largely on having sufficient bone in the jaw. Bone grafting may be required in cases of resorption.
- Overall health: Chronic conditions like diabetes, osteoporosis, or habits like smoking can influence candidacy and healing outcomes more than age alone.
- Commitment to oral care: Long-term success also requires proper hygiene and regular dental check-ups, which are lifestyle-dependent rather than age-specific.
How Long Does a Single Tooth Implant Take from Start to Finish?
When planning for a single tooth dental implant, one of the most common questions patients ask is, “How long will the entire process take?” The answer varies depending on several factors including the patient’s oral health, need for preparatory procedures like bone grafting, and the clinic’s specific approach. However, understanding the general timeline can help set realistic expectations and allow for better planning.
General Treatment Timeline: Consultation to Final Crown
- Initial consultation: The first step is a detailed examination, which includes X-rays or a CT scan, oral health assessment, and discussion of the treatment plan. This appointment typically lasts 30 to 90 minutes.
- Pre-surgical preparations: If tooth extraction or bone grafting is necessary, additional appointments may be scheduled, and healing time will be required before the implant can be placed.
- Implant surgery: The procedure for placing the titanium implant typically takes about 30 minutes to 1 hour for a single tooth and is usually done under local anesthesia.
- Healing period: After the implant is placed, it takes time for the bone to integrate with the implant in a process known as osseointegration. This can take anywhere from 2 to 6 months, depending on the individual’s bone density and healing response.
- Abutment and crown placement: Once healing is complete, the dentist places an abutment (connector) and takes impressions or digital scans for the custom-made crown. The final crown is then attached within 1–2 weeks.
Healing Times and Appointments Needed
- Multiple phases: Implant treatment consists of at least 3 visits—initial consultation, surgery, and crown placement. Additional visits may be needed for post-operative check-ups and impressions.
- Recovery time: Most patients can return to normal activities within 1–2 days after surgery, though complete healing of the implant site takes several months.
- Temporary tooth options: During healing, patients may be given a temporary crown or removable partial denture to preserve aesthetics and function.
Timeline Variability Based on Bone Grafts or Complications
- Bone graft delays: If a bone graft is required, healing can take 3–6 months before the implant can be placed. This adds to the total treatment time.
- Infection or implant rejection: Though rare, complications can extend the process further. Careful planning and hygiene help minimize risks.
- Immediate implants: In some cases, especially with excellent bone density, an implant and temporary crown may be placed on the same day. However, this is not suitable for every patient and involves a higher risk profile.
What Specialist Should You Choose for a Dental Implant?

Choosing the right professional for your single tooth dental implant is crucial for both the success of the procedure and your long-term oral health. While general dentists can place implants, it’s often advisable to consult with a specialist—especially for complex cases or when bone grafting or anatomical risks are involved.
Roles of Implantologists, Oral Surgeons, Periodontists, and Prosthodontists
- Implantologists: These are dentists who specialize specifically in the placement of dental implants. They typically have additional training and experience focused on implant techniques, surgical protocols, and implant systems. They’re often the go-to professionals for routine to moderately complex cases.
- Oral Surgeons: Also known as oral and maxillofacial surgeons, these specialists are trained to handle more complicated implant procedures, such as cases involving bone grafts, sinus lifts, or nerve proximity. They’re highly skilled in surgical aspects of the implant process.
- Periodontists: These specialists focus on gum health and the supporting structures of the teeth. They are an excellent choice for patients with periodontal disease or concerns related to gum recession and tissue management around the implant site.
- Prosthodontists: These experts are specialists in restorative dentistry, including crowns, bridges, and dentures. They often work in collaboration with other specialists to design and place the final crown on the implant for optimal function and aesthetics.
Criteria for Choosing the Right Expert
- Training and credentials: Look for specialists who have completed advanced training in implantology, oral surgery, or periodontics. Credentials from recognized institutions or professional organizations like the ICOI (International Congress of Oral Implantologists) can offer added assurance.
- Experience with single tooth implants: Ask how many implants the provider places per year and whether they routinely perform single tooth procedures, especially in the area you need treated.
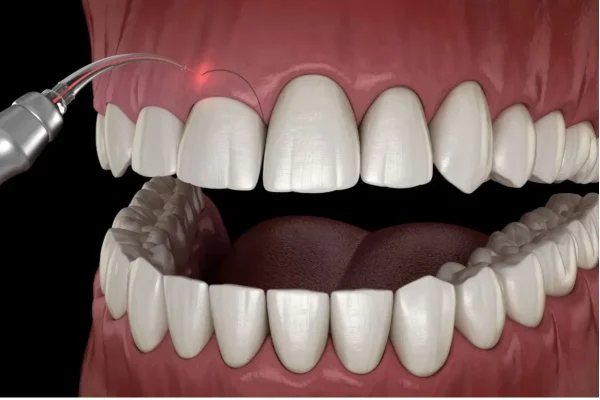
- Access to technology: Choose clinics that use 3D imaging, digital scanning, and guided implant surgery. These tools improve accuracy and outcomes.
- Patient reviews and results: Real patient testimonials and before-and-after photos can help you assess the provider’s track record and patient satisfaction.
Importance of Experience and Credentials
- Reduced complications: Experienced implant dentists are more likely to foresee potential issues such as bone deficiencies or sinus interference and address them proactively.
- Improved aesthetics: Specialists are better equipped to deliver a natural-looking result, especially for front-tooth implants where cosmetic detail matters.
- Efficient treatment planning: A skilled professional will tailor a plan to your anatomy and health profile, streamlining the process and minimizing unnecessary delays or costs.
In summary, while many dental professionals are qualified to place single tooth implants, selecting a specialist with extensive training, hands-on experience, and access to advanced tools can significantly improve your results. It’s worth investing in a qualified provider to ensure both functional success and a beautiful smile.
Is a Bridge or Implant Better for Replacing One Tooth?
When deciding between a dental bridge and a single tooth implant to replace a missing tooth, it’s important to weigh the pros and cons of each solution. While both options aim to restore function and aesthetics, they differ significantly in procedure, durability, maintenance, and impact on surrounding teeth.
Compare Longevity, Invasiveness, and Maintenance
- Longevity: Single tooth implants generally last longer than dental bridges. A well-placed implant with proper care can last 20+ years or even a lifetime, while bridges may need replacement every 7–15 years depending on materials and wear.
- Invasiveness: Although an implant requires surgical placement into the jawbone, it preserves the integrity of adjacent teeth. A bridge, by contrast, involves grinding down healthy neighboring teeth to support the prosthetic, making it more invasive to natural enamel.
- Maintenance: Implants are easier to care for because they mimic natural teeth. You can brush and floss them like your other teeth. Bridges require special flossing tools or interdental brushes to clean underneath the pontic (false tooth), adding complexity to oral hygiene routines.
Pros and Cons of Each
- Dental Bridge – Pros:
- Faster restoration: Often completed in two visits.
- No surgery required.
- Lower initial cost than implants.
- Dental Bridge – Cons:
- Requires removal of enamel from adjacent healthy teeth.
- Increased risk of decay and failure in supporting teeth.
- Shorter lifespan than implants.
- Dental Implant – Pros:
- Preserves jawbone health by stimulating bone growth.
- Doesn’t impact neighboring teeth.
- Offers superior durability and aesthetics.
- Dental Implant – Cons:
- Higher upfront cost.
- Longer treatment time due to healing.
- Surgical procedure with associated risks (though minimal in healthy patients).
Patient Cases Where One Is Preferred Over the Other
- When implants are preferred:
- Patients with sufficient bone density and healthy gums.
- Individuals wanting a long-term, low-maintenance solution.
- Situations where adjacent teeth are healthy and should remain untouched.
- When bridges are preferred:
- Patients with insufficient bone who cannot undergo bone grafting.
- Those looking for a faster, non-surgical option.
- Cases where adjacent teeth already need crowns or restorations.
Ultimately, both options can effectively restore a missing tooth, but single tooth implants tend to offer better long-term outcomes and less damage to natural teeth. However, a dentist’s personalized recommendation based on your oral health, preferences, and budget will guide the best decision for your case.
Why Are Single Tooth Implants So Expensive?
The cost of a single tooth implant can come as a surprise to many patients. Understanding what drives the price helps explain why dental implants are more expensive than other tooth replacement options like bridges or dentures. From the technology used to the expertise involved, every aspect of the process contributes to the final price.
Detailed Breakdown of Costs: Surgery, Lab, Materials
- Surgical Procedure: Implant placement is a surgical procedure that requires specialized equipment, sterile conditions, and experienced dental professionals. The surgical fee covers the planning, anesthesia, implant insertion, and any necessary aftercare visits.
- High-Quality Materials: The titanium post that integrates with your jawbone is a biocompatible, medical-grade material. This ensures longevity and minimizes risk of rejection. The abutment and crown, often made from porcelain or zirconia, are custom-designed to match your natural teeth.
- Laboratory Work: The dental crown that caps the implant is fabricated in a high-tech dental lab using digital scans, milling machines, and skilled technicians. Customization ensures that the new tooth fits perfectly in your bite and looks indistinguishable from your natural teeth.
- Multiple Appointments: The process includes several visits—initial consultation, imaging, surgery, follow-up checkups, and final crown placement—each contributing to the overall cost.
Discussion on Quality vs. Price
- Long-Term Value: Though the upfront cost is higher, implants often last significantly longer than bridges or dentures. Over time, this reduces the need for replacement and repeated dental visits, making implants a cost-effective choice in the long run.
- Expertise Matters: Implantology is a specialized field. Dentists who perform implants have additional training and certifications. Their expertise ensures precise placement, reducing the likelihood of complications or failure—another factor that influences cost.
- Technology Investment: Clinics offering implants often invest in advanced equipment such as 3D CT scanners, digital impression systems, and CAD/CAM software to provide accurate diagnostics and better outcomes.
Long-Term Value Comparison With Cheaper Options
- Bridges: May cost less initially but often need replacement within a decade, especially if adjacent teeth develop issues.
- Dentures: Lower cost but less stable, can affect eating and speaking, and may require relining or replacement over time.
- Implants: Higher initial cost, but they preserve jawbone health, maintain facial structure, and can last a lifetime with proper care.
In conclusion, the higher cost of a single tooth implant reflects its durability, functionality, aesthetics, and the advanced care required. It’s an investment in long-term oral health and quality of life.
Can a Single Tooth Implant Be Done in One Day?
With the rise of advanced dental technologies, patients often wonder whether they can get a new tooth in a single visit. This question leads to the concept of “same-day implants” or “immediate load implants,” a technique that allows the placement of a dental implant and temporary crown in just one appointment. However, not everyone qualifies for this fast-track treatment.
Explanation of Same-Day Implants (Immediate Load)
- What Are Same-Day Implants?: This technique involves placing the implant post and a temporary crown on the same day. Instead of waiting for the jawbone to heal over months, a provisional crown is attached immediately after surgery.
- Purpose of the Temporary Crown: The crown placed on the same day is usually temporary and not for chewing hard food. It maintains aesthetics and helps the patient avoid the inconvenience of a visible gap.
- Permanent Crown Comes Later: After the healing phase (osseointegration), which still takes several months, a permanent crown replaces the temporary one.
Who Qualifies for This Option
- Strong Bone Structure: Patients with sufficient bone density and volume are more likely to qualify for immediate implants. A healthy jawbone ensures better initial stability of the implant.
- Good Oral Health: Ideal candidates have healthy gums and no signs of periodontal disease, which could compromise implant success.
- Non-Smokers Preferred: Smoking can delay healing and increase the risk of implant failure. Non-smokers or those willing to quit during healing are better candidates.
- No Clenching or Grinding: Patients who suffer from bruxism (teeth grinding) may put excessive pressure on the new implant, increasing failure risk.
Risks and Success Rates vs. Traditional Method
- Risk of Failure: Although appealing, immediate implants carry a higher risk of failure if the implant doesn’t integrate well due to premature loading (putting pressure on it too soon).
- Comparable Success Rates—When Conditions Are Ideal: Studies have shown success rates similar to traditional implants in patients who meet the right criteria and follow post-op care instructions.
- Strict Aftercare is Key: Patients must adhere strictly to dietary restrictions (soft food only), avoid biting on the implant site, and maintain excellent oral hygiene.
While same-day implants offer convenience and instant results, traditional implant procedures remain the gold standard for most patients due to their proven long-term success. An in-depth consultation with an implant specialist is essential to determine whether this accelerated option is appropriate.
Can You Eat Normally After a Single Tooth Implant?
One of the top concerns for patients considering a single tooth implant is whether they’ll be able to return to eating normally. The good news is, with proper healing and aftercare, a dental implant can fully restore your chewing function—often better than before. However, it’s crucial to understand the timeline and dietary stages that follow the implant procedure.
Eating After Surgery: Immediate and Long-Term
- Immediately Post-Surgery: In the first 24–48 hours after implant placement, the surgical site is highly sensitive. Dentists recommend sticking to a liquid or very soft food diet during this period. Think smoothies, broths, yogurt, and mashed potatoes.
- Avoid Hot and Spicy Foods: Heat and spices can irritate the surgical site and delay healing. It’s also wise to avoid acidic foods and beverages like citrus juice, vinegar, or carbonated drinks early on.
- Gradual Progression: As the implant begins to integrate with the bone and your discomfort diminishes (typically after 1–2 weeks), you can slowly reintroduce soft solid foods. Pasta, soft-cooked vegetables, scrambled eggs, and fish are good transitional choices.
Foods to Avoid and Recommended Diet
- Hard or Crunchy Foods: Avoid nuts, chips, apples, crusty bread, and any food that could place pressure on the implant site during the healing phase. These can interfere with osseointegration or even damage the healing implant.
- Sticky Foods: Chewing gum, toffee, and sticky candies can pull on the temporary crown or irritate stitches, increasing the risk of complications.
- Recommended Options:
- Protein-rich foods like eggs, tofu, and tender meats (once healing permits).
- Hydrating fruits like bananas and watermelon.
- Calcium-rich dairy to support bone health and healing.
Long-Term Chewing Function with Implants
- Comparable to Natural Teeth: Once fully healed and restored with a permanent crown, your implant will function nearly identically to a natural tooth. You’ll be able to chew tough foods like steak or raw vegetables with confidence.
- No Movement or Loosening: Unlike removable dentures, a single tooth implant is fixed in place. There’s no risk of slippage, which significantly improves the eating experience.
- Protective Measures: Although you can eat normally, it’s wise to avoid habits like biting ice or using your teeth to open packaging—whether you have implants or not.
In summary, a single tooth implant not only restores your smile but also your ability to enjoy food without restriction—after a brief healing period and guided dietary progression.
Frequently Asked Questions About Single Tooth Dental Implant

As dental implants become more popular for replacing missing teeth, patients often have recurring questions about safety, success, and healing. Below we answer two of the most frequently asked questions specifically related to single tooth implants.
How Long Does It Take for a Single Tooth Implant to Heal?
- Typical Healing Timeline: The healing process after implant placement usually takes between 3 to 6 months. This period allows for osseointegration, where the titanium post fuses securely with the jawbone.
- Healing Phase Breakdown:
- Week 1: Swelling, slight bruising, and tenderness. Sutures are usually removed after 7–10 days.
- Week 2–4: Soft tissue around the implant begins to heal. Patients can begin eating soft solids.
- Month 2–4: Bone starts to integrate with the implant. Most patients feel almost normal.
- Factors Affecting Healing:
- Bone quality and density at the implant site.
- Overall health and immune response.
- Whether additional procedures (e.g., bone grafts or sinus lifts) were required.
- How to Support Healing:
- Avoid smoking and alcohol.
- Maintain good oral hygiene without disturbing the surgical site.
- Follow dietary instructions and attend scheduled follow-up visits.
What Is the Success Rate of Single Tooth Implants?
- Success Rate Statistics: Single tooth implants boast a high success rate—between 95% to 98%—when placed by experienced specialists and maintained properly by patients.
- Why They Succeed:
- Use of biocompatible titanium that integrates naturally with bone.
- Thorough preoperative assessment (bone scans, medical history).
- Adherence to aftercare guidelines, such as avoiding undue pressure on the implant during healing.
- When Complications Arise:
- Implants can fail due to peri-implantitis (a form of gum disease), poor osseointegration, or mechanical overload.
- Medical conditions like uncontrolled diabetes or autoimmune disorders may also increase risks.
- Maintaining Long-Term Success:
- Brush and floss daily, including interdental care around the implant.
- Visit your dentist regularly for professional cleanings and monitoring.
- Wear night guards if you grind your teeth, which can put excess force on the implant.
By understanding these key FAQs, patients can make more informed decisions and feel confident about the long-term benefits of their single tooth implant investment.