Key Takeaways
-
- Wisdom tooth extraction is the surgical removal of the third molars, typically needed when they cause problems like **pain** or **impaction**.
-
- The procedure’s complexity and cost vary based on the number of teeth and whether they are impacted.
-
- Proper preparation, including arranging transport and discussing medical history, is crucial for a smooth experience.
-
- During the procedure, modern anaesthesia ensures you should feel **no sharp pain**, only potentially pressure.
-
- Post-operative pain and swelling are expected, usually peaking around days 2 and 3, and are managed with prescribed medication and care.
-
- While generally safe, risks like dry socket or nerve injury are possible, highlighting the importance of following post-op instructions and knowing when to contact your surgeon.
-
- Recovery involves a few days of significant downtime (3-7 days), with full internal healing taking several months.
- In the **UK NHS**, extraction criteria are based on clinical necessity, not routine removal, and typically require a dentist’s referral.
What is Wisdom Extraction: Understanding the Basics
Stepping into the realm of wisdom tooth extraction often begins with a fundamental question: what exactly are we talking about? At its core, wisdom extraction is the surgical removal of one or more of the third molars, those teeth that emerge (or attempt to emerge) right at the very back of your mouth, usually long after all your other adult teeth have settled in. This late arrival, typically between the ages of 17 and 25 – an age often associated with gaining a little ‘wisdom’ – is precisely how they earned their rather philosophical moniker. The procedure itself goes by many names: wisdom tooth removal, pulling wisdom teeth, getting molars removed (a broader term, but often used in this context), or simply tooth extraction when specified as ‘wisdom’. It’s a common facet of dental practice, often handled by general dentists for simpler cases or, more frequently for complex or impacted teeth, by oral and maxillofacial surgeons, who possess specialized training in surgical procedures of the mouth, jaw, and face. While the term ‘major surgery’ might sound alarming, the classification really depends on the complexity. A simple extraction of a fully erupted wisdom tooth might be considered minor surgery, akin to pulling any other tooth. However, the removal of deeply impacted wisdom teeth, requiring incisions, bone removal, and stitching, certainly falls into the category of more involved, though still routine and safe, oral surgery. Understanding these basics is the first step in demystifying a procedure that can feel daunting simply due to its surgical nature and location in such a sensitive area of the body. It’s a controlled, precise process designed to alleviate pain, prevent future complications, and safeguard your overall oral health.
What are wisdom teeth?
Delving deeper, let’s truly get acquainted with these enigmatic molars. Wisdom teeth, scientifically known as the third molars, are the final set of adult teeth to make their appearance in the human mouth, situated at the posterior-most positions, one in each corner of the upper and lower jaws. Their eruption timeline is famously late, generally materializing sometime between the late teenage years and the mid-twenties, although this window can vary significantly from person to person. It’s worth noting that the presence and number of wisdom teeth are far from uniform across the population. It’s perfectly normal for some individuals to develop fewer than four, or even none at all – a potential evolutionary adaptation in a species with a changing diet and often shrinking jawlines compared to our ancestors. When they do arrive, however, they face a challenge the other teeth rarely encounter: space. By the time the third molars are ready to erupt, the jawbone has often finished growing, and the existing 28 adult teeth have typically claimed all the available real estate. This lack of space is the primary reason wisdom teeth become problematic. They might erupt partially, at an angle, or not at all, becoming what’s known as ‘impacted’. Whether fully erupted or impacted, their location at the back of the mouth also makes them notoriously difficult to clean effectively, leaving them vulnerable to decay and gum disease even if they appear to be coming in straight. They are a fascinating dental anomaly, a relic perhaps from a time when larger jaws were necessary to process a tougher diet, now often causing more trouble than they’re worth in the modern mouth. Understanding their unique characteristics – their late eruption, variable presence, challenging location, and potential for impaction – is key to grasping why ‘wisdom extraction’ is such a prevalent dental procedure.
What is wisdom teeth removal?
Defining wisdom teeth removal isn’t just about stating it’s taking a tooth out; it’s understanding the nuances of a common yet intricate oral surgical procedure. At its core, it’s the process by which one or more third molars are extracted from their socket in the jawbone. While superficially similar to the removal of any other tooth, the context and complexity often elevate it. It’s not merely pulling; it’s a deliberate, planned intervention necessitated by a range of potential issues that these late-blooming teeth can cause. This procedure is one of the most frequently performed oral surgeries worldwide, a testament to how commonly wisdom teeth pose problems in modern mouths. The ‘why’ behind the removal – which we’ll delve into more deeply – is the crucial element defining the procedure. It’s typically performed to address existing pain, swelling, or infection caused by problematic wisdom teeth, or as a preventative measure to avert future issues like impaction-related damage to neighbouring teeth, cysts, or persistent infections. Unlike extracting a front tooth or a pre-molar, wisdom tooth removal, particularly when the tooth is impacted, often requires more than just simple force and forceps. It can involve making incisions in the gum tissue, removing small sections of bone obstructing the tooth’s path, or even sectioning the tooth itself into smaller pieces for easier extraction. This explains why the procedure is often performed by oral surgeons under various forms of anaesthesia, ensuring patient comfort and safety throughout the process. It’s a surgical solution to a common anatomical mismatch – a modern mouth struggling to accommodate ancient hardware – aimed at restoring comfort and maintaining long-term oral health.
Why Are Wisdom Teeth Removed? Necessity and Reasons
The perennial question looms: why do so many people need their wisdom teeth removed? It’s a topic often debated, especially considering that in some individuals, these teeth erupt without incident and cause no problems whatsoever. However, for the vast majority, the space limitations of the modern jaw make the eruption of these final molars a fraught process, leading to a cascade of potential issues that ultimately necessitate their extraction. The most frequent culprit is impaction, a condition where the wisdom tooth is unable to fully emerge through the gum line, either because it’s blocked by another tooth, bone, or gum tissue, or because it’s growing in at an awkward angle (like horizontally or diagonally). Impaction isn’t just an inconvenience; it can be a significant source of pain, swelling, and infection. When a tooth is partially erupted, the flap of gum tissue over it can trap food particles and bacteria, leading to pericoronitis, a painful infection of the surrounding gums. Furthermore, an impacted or misaligned wisdom tooth can exert pressure on the adjacent second molar, potentially causing damage, decay, or contributing to orthodontic issues by pushing other teeth out of alignment. Other reasons for removal include the formation of cysts or tumours around an impacted tooth, or simply the inability to properly clean wisdom teeth due to their far-back location, making them susceptible to decay or gum disease that can then spread. So, while you certainly don’t *have* to get your wisdom teeth removed if they are healthy, fully erupted, properly aligned, and easily cleanable, the reality for most people is that these complications arise, making extraction the recommended, and often necessary, course of action to prevent more significant oral health problems down the line. It’s less about a universal need and more about addressing specific, often painful, issues these unique teeth present.
Why wisdom teeth might need to be removed?
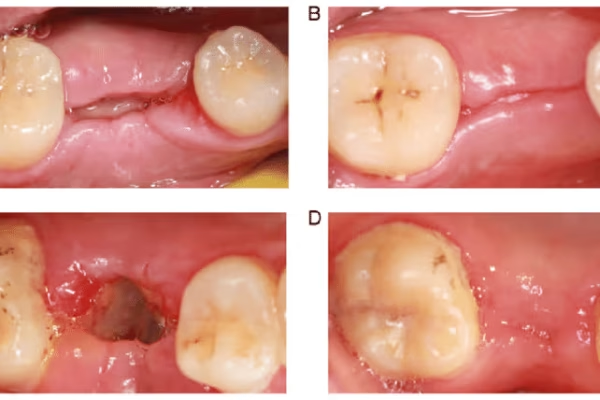
The reasons for needing wisdom teeth extraction are varied, but they overwhelmingly stem from one core problem: inadequate space. When the jaw cannot comfortably accommodate these final molars, they become problematic. The most common reason is **impaction**, which can manifest in several ways: the tooth might be angled towards the front of the mouth (mesial impaction), towards the back (distal impaction), straight down but stuck (vertical impaction), or lying completely on its side (horizontal impaction). Impaction means the tooth cannot fully erupt into a functional position. This often leads to chronic issues. **Recurrent infection**, known as pericoronitis, is a frequent symptom of partially erupted wisdom teeth. The flap of gum covering the tooth creates a perfect breeding ground for bacteria, causing inflammation, pain, swelling, difficulty opening the mouth, and even fever. This can flare up repeatedly, antibiotics offering only temporary relief until the underlying cause (the tooth) is addressed. Furthermore, impacted or poorly positioned wisdom teeth can cause **damage to adjacent teeth**. They can press against the second molar, leading to root resorption (damage to the root structure) or making that molar extremely difficult to clean, resulting in decay on its back surface. Their difficult-to-reach location also makes wisdom teeth highly prone to decay and gum disease **(periodontitis)** even if they are partially or fully erupted but misaligned. Brushing and flossing effectively at the very back is challenging for many people. Beyond infection and damage, **cysts or tumours** can occasionally form around impacted wisdom teeth, requiring surgical intervention. Finally, dentists and surgeons often recommend removal as a **preventative measure**. Even if currently asymptomatic, a deeply impacted tooth or one growing at a clear angle is highly likely to cause problems later in life. Removing them preemptively in younger adulthood, when roots are less developed and bone is less dense, can lead to easier surgery and faster recovery compared to waiting until problems arise in older age. This preventative approach aims to avoid future pain, infection, and damage to surrounding oral structures.
How do I know if I need a wisdom tooth extraction?
Pinpointing whether you need a wisdom tooth extraction typically starts with recognizing certain tell-tale signs, although a definitive diagnosis always requires professional assessment. Common symptoms that might suggest your wisdom teeth are causing trouble include **pain** or **soreness** in the back of your jaw, particularly near the eruption site. This pain can range from a dull, persistent ache to sharp, throbbing discomfort, sometimes radiating towards the ear or head. You might also experience **swelling** and **redness** in the gums around the back molars, accompanied by a **bad taste** or **odour** emanating from the area, indicative of infection. Difficulty opening your mouth fully, known as trismus, or pain when chewing towards the back of your mouth are also significant indicators. Sometimes, you might even feel a small, hard lump pushing through the gums at the back. While these symptoms are strong signals to seek dental attention, it’s crucial to understand that wisdom teeth can cause problems even without overt symptoms. This is particularly true for deeply impacted teeth or those causing slow, silent damage to adjacent teeth or bone. Therefore, the definitive answer to whether you need an extraction comes after a thorough dental examination by a dentist or oral surgeon. They will perform a visual inspection and, most importantly, take **dental X-rays**. Panoramic X-rays are especially useful as they show the position of all your teeth, including those still developing or impacted within the jawbone, and their relationship to nerves and sinuses. Based on the clinical examination, your symptoms (or lack thereof), and the X-ray findings, the dental professional can assess the position, health, and potential future impact of your wisdom teeth and provide a recommendation tailored to your specific situation. Trusting their expertise, grounded in diagnostic imaging, is key to making an informed decision about extraction.
Is it OK to leave wisdom teeth?
The question of whether it’s acceptable to leave wisdom teeth in place is entirely valid and depends heavily on individual circumstances. The common narrative often implies that all wisdom teeth must be removed, but this isn’t universally true. It is absolutely **OK to leave wisdom teeth** if they are healthy, functional, and not causing or likely to cause problems. This typically applies to wisdom teeth that have fully erupted into the mouth in a proper position, are correctly aligned with the other teeth in the arch, contribute positively to chewing function (or at least don’t hinder it), and, crucially, can be **easily and effectively cleaned** with regular brushing and flossing. In such cases, they function just like any other set of molars. The key is that they must not be causing impaction, overcrowding, damage to adjacent teeth, or recurrent infections. If a wisdom tooth meets these criteria, extracting it offers no benefit and would be unnecessary surgery. However, even if wisdom teeth are left in place because they appear healthy, **regular monitoring by a dentist is absolutely crucial**. Their late arrival and far-back location still make them somewhat more vulnerable to developing problems later in life compared to other teeth. Routine dental check-ups, including periodic X-rays, allow your dentist to keep an eye on their status, check for signs of decay, gum disease, or subtle shifts in position that could lead to future issues. Think of it like a dormant volcano; it might seem quiet now, but monitoring is wise. So, while surgical removal is a common necessity, it is by no means an automatic sentence for every wisdom tooth. If yours are healthy, aligned, and manageable with daily oral hygiene, they can often remain part of your smile, provided you maintain diligent cleaning and regular professional oversight.
Are there any alternatives to removing a wisdom tooth?
When a wisdom tooth is problematic – impacted, infected, causing pain, or damaging adjacent teeth – the conversation around alternatives to removal becomes quite limited, particularly for symptomatic cases. For wisdom teeth that are genuinely causing issues, **extraction is typically the only definitive solution** to permanently resolve the problem. Managing symptoms, while necessary for temporary relief, does not address the root cause. For instance, if you have an infection (pericoronitis) around a partially erupted wisdom tooth, a dentist might prescribe **antibiotics** to clear the infection and recommend **warm salt water rinses** or antiseptic mouthwashes to help soothe the inflamed gums. **Pain relief medication**, both over-the-counter options like ibuprofen or paracetamol, and sometimes prescription-strength drugs, can help manage the discomfort. However, these measures are just that – managing the symptoms of the underlying issue. They calm the inflammation or mask the pain, but they don’t change the tooth’s position, resolve the impaction, or remove the source of repeated infection or potential damage. Once the effects of the medication wear off, or if the conditions that allowed the problem to develop persist (like trapped food under a gum flap or pressure on another tooth), the symptoms are likely to return. In very rare, specific cases where a wisdom tooth is causing orthodontic issues but isn’t impacted, sometimes minor orthodontic adjustments might be considered, but this is highly unusual and not a standard alternative for typical impaction or infection problems. For the vast majority of cases where wisdom teeth are symptomatic and problematic, extraction remains the gold standard treatment because it physically removes the source of the pain, infection, and damage, thereby preventing recurrence and protecting the rest of your oral health. There’s no magic wand to make a crowded, impacted tooth simply move into a better position or disappear; surgical removal is the direct route to resolution for those situations.
How Much Does Wisdom Teeth Removal Cost?
Discussing the financial aspect of wisdom teeth removal is crucial, as it’s a significant consideration for many individuals and their families. The cost of the procedure isn’t a fixed number; it’s a variable figure influenced by a constellation of factors, meaning you won’t get a one-size-fits-all price tag. Perhaps the most significant determinant is the **complexity of the extraction**. A simple extraction of a fully erupted wisdom tooth, much like pulling any other visible tooth, will naturally cost less than a complex surgical extraction. Complex cases involve impacted teeth – those trapped beneath the gum line or bone – and require incisions, potentially bone removal, and often stitches, making them more time-consuming and surgically involved. The **number of teeth** being removed is another obvious cost factor; extracting all four wisdom teeth in one session will cost more than removing just one or two. The **type of anaesthesia** used also plays a major role. Local anaesthesia, which numbs the immediate area while you remain awake, is the least expensive. Conscious sedation (like nitrous oxide or oral sedatives) or intravenous (IV) sedation, which puts you into a relaxed or semi-asleep state, adds to the cost. General anaesthesia, where you are fully unconscious, is the most expensive and typically requires an anaesthesiologist, significantly increasing the overall fee. The **location** where the procedure takes place also impacts the price – costs can vary geographically, and having the procedure done in a hospital or surgical center will generally be more expensive than in a dental office or specialized oral surgery clinic due to facility fees. Finally, and perhaps most importantly for many, **dental insurance coverage** can drastically alter your out-of-pocket expense. Policies vary widely in what they cover for oral surgery. Some cover a high percentage, while others cover very little, especially if the procedure isn’t deemed strictly ‘necessary’ or if waiting periods apply. Because of these numerous variables, it is absolutely essential to get a detailed, written **cost estimate** from your dental professional *before* scheduling the surgery. This quote should break down the costs for the extraction itself, the anaesthesia, any necessary X-rays or pre-operative appointments, and provide information on what your insurance is expected to cover versus your estimated out-of-pocket responsibility. Navigating these costs requires clarity and direct communication with the provider and your insurance company.
Preparing for Wisdom Teeth Removal and the Procedure
Stepping towards wisdom teeth removal involves more than just booking an appointment; it requires thoughtful preparation to ensure the procedure goes smoothly and sets the stage for a comfortable recovery. The lead-up to the surgery and the events of the day itself are carefully choreographed steps designed with your safety and comfort in mind. Preparing adequately can significantly reduce anxiety and prevent unexpected hiccups. It’s a combination of following specific medical instructions, logistical planning, and getting yourself mentally ready for the experience. You’ll receive detailed instructions from your dentist or oral surgeon’s office, and adhering to them is paramount. On the day of the procedure, you’ll arrive, go through a brief check-in process, meet with the surgical team, and then the extraction itself will take place under the chosen form of anaesthesia. The duration varies, but the actual tooth removal is often quicker than you might imagine, though the overall time spent at the clinic, including preparation and post-op monitoring, will be longer. Understanding each phase – the preparation, the procedure itself, and how long it’s expected to take – helps demystify the process and empowers you to approach the day with greater confidence and less apprehension. It’s a routine medical event for the professionals involved, but for the patient, it’s a personal journey through a necessary step for future oral health, and being well-informed is your best companion on that journey.
How do I prepare for a wisdom tooth extraction?
Proper preparation for wisdom tooth extraction is a multi-faceted process that extends beyond just showing up at the clinic. It begins well before the scheduled date and involves careful planning and adherence to specific instructions provided by your surgical team. First and foremost, if you are undergoing sedation or general anaesthesia, you will receive strict **fasting instructions**. This typically means no food or drink for a certain period (often 6-8 hours) before the surgery to prevent complications related to aspiration during anaesthesia. It is absolutely critical to follow these instructions precisely. Another non-negotiable step is **arranging for transportation home**. You will not be able to drive yourself after receiving any form of sedation or general anaesthesia, and often even after extensive local anaesthesia due to discomfort or residual numbness. You will need a responsible adult to drive you home and ideally stay with you for the initial few hours after the procedure. Before the surgery, you will have a consultation where you must **discuss your full medical history**, including any pre-existing health conditions, allergies, and a complete list of all **medications** you are currently taking, including prescription drugs, over-the-counter medications, vitamins, and herbal supplements. Some medications might need to be adjusted or temporarily stopped before surgery. Your surgeon will also review the anaesthesia options and potential risks. Beyond the medical necessities, practical preparation is key. This includes **gathering necessary supplies for recovery** beforehand: soft foods (yogurt, soup, mashed potatoes), ice packs, gauze pads, over-the-counter pain relievers (ensure they are appropriate and cleared by your surgeon), and any prescribed medications already filled at the pharmacy. Mentally preparing for the procedure is also beneficial. Understanding what will happen, knowing the risks are low but present, and trusting your surgical team can help alleviate anxiety. Don’t hesitate to ask any lingering questions during your consultation – feeling informed is a powerful tool against pre-surgery jitters. A little planning goes a long way in making the entire experience smoother and less stressful.
What happens during wisdom tooth removal?
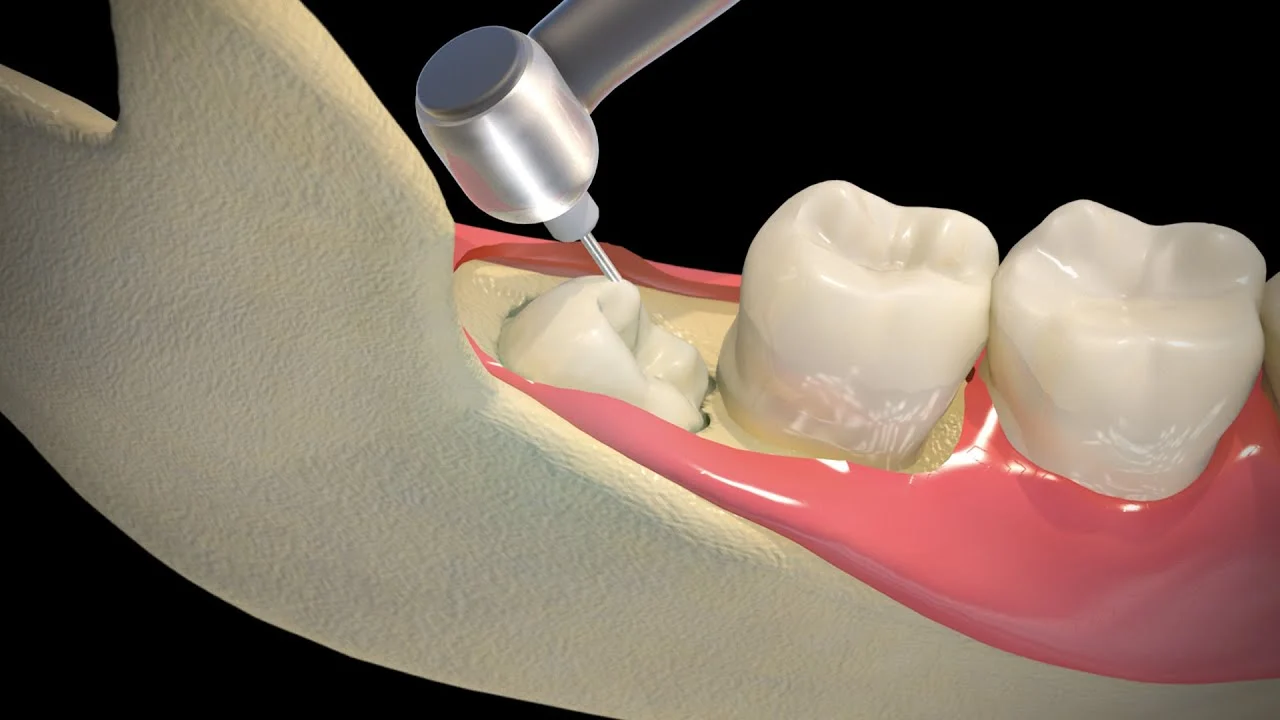
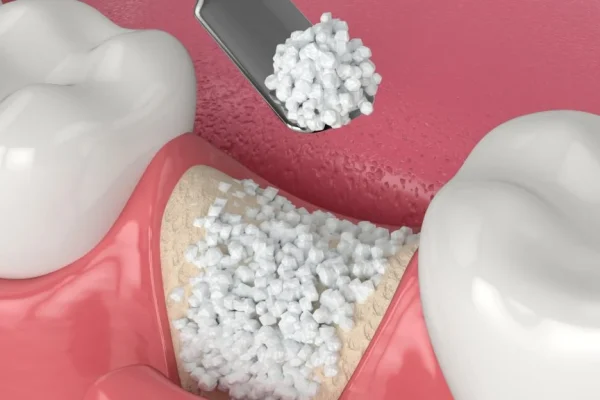
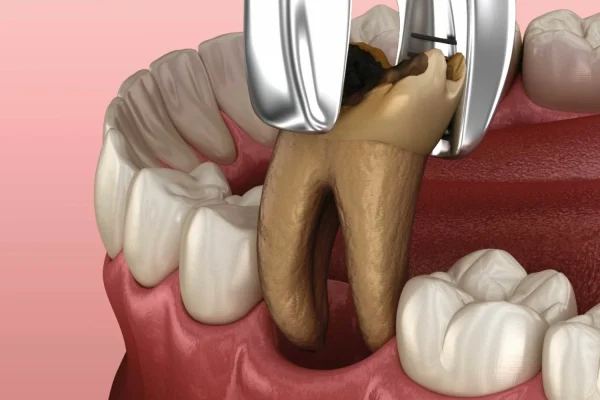
The actual process of wisdom tooth removal is a carefully orchestrated surgical procedure designed to be as comfortable and efficient as possible. It begins with the administration of the chosen **anaesthesia**. For simple extractions of erupted teeth, local anaesthesia, involving injections around the tooth to numb the area, may suffice. For more complex removals or if you have anxiety, conscious sedation (like nitrous oxide or oral pills) or intravenous (IV) sedation will be used to make you relaxed or semi-conscious. General anaesthesia, putting you completely asleep, is reserved for the most complex cases or specific medical needs. Once the anaesthesia has taken effect and the surgical team ensures you are comfortable and profoundly numb (or asleep), the **extraction process** commences. If the tooth has fully erupted, a simple extraction involves using instruments to loosen the tooth gently from its socket before carefully removing it with forceps. However, wisdom teeth, especially impacted ones, rarely cooperate that easily. For impacted teeth, the procedure becomes a **surgical extraction**. This involves making a small **incision** in the gum tissue to expose the tooth and surrounding bone. Often, small amounts of **bone** covering the tooth may need to be carefully and precisely removed using a drill to create a clear path for extraction. If the tooth is particularly large or angled awkwardly, the surgeon may need to **section** it – divide the tooth into two or more pieces – to remove it more easily and with less trauma to the surrounding tissues and bone. After the tooth (or pieces) are removed, the surgeon will **clean the extraction site**, removing any tissue debris or bone fragments. Finally, **stitches (sutures)** may be placed to close the gum incision and help the socket heal. The type of stitches used can vary; some dissolve on their own over time, while others need to be removed by the surgeon at a follow-up appointment. Throughout the procedure, the surgical team monitors your vital signs to ensure your safety and well-being. The focus is on performing the extraction efficiently while minimizing trauma to facilitate a smoother recovery.
How long does it take to remove a wisdom tooth?
Pinpointing the exact duration of wisdom tooth removal is tricky because it’s highly dependent on the individual case, primarily the **number of teeth** being removed and the **complexity** of each extraction. A single, fully erupted wisdom tooth that requires only a simple extraction, much like removing any other non-problematic tooth, can be surprisingly quick. The actual removal part might take just **5 to 15 minutes**. However, this is just the chair time for the extraction itself; the overall appointment will be longer to account for check-in, preparation, administering anaesthesia, post-procedure instructions, and a brief recovery period in the clinic. When the procedure involves multiple teeth, or if they are impacted and require surgical removal, the time frame extends. Removing two impacted wisdom teeth might take anywhere from **20 to 40 minutes** of surgical time. If all four wisdom teeth, particularly if they are all significantly impacted and require complex bone removal or sectioning, are being extracted in one session, the surgical time could range from **45 minutes to 90 minutes or even slightly longer** in exceptionally challenging cases. The anaesthesia method also subtly influences the timing; while the surgery itself might not take longer, the time needed for IV sedation or general anaesthesia to take effect and wear off adds to the overall time you spend at the surgical centre. It’s important not to focus solely on the surgical duration but to factor in the entire appointment time, which can easily be anywhere from one to two hours or more, depending on the clinic’s protocols and the recovery area process. Your surgeon will give you a more precise estimate during your consultation based on the X-rays and their assessment of your specific situation, but understanding that complexity dictates time is key – simple cases are relatively swift, while complex removals require more deliberate and careful surgical work, taking correspondingly longer.
How Painful is Wisdom Tooth Extraction? Managing Discomfort
The question of pain is often the foremost concern for anyone facing wisdom tooth extraction, and it’s understandable why. The mouth is a sensitive area, and the idea of surgical intervention there can provoke significant anxiety. However, it’s crucial to differentiate between the pain you might experience *before* the procedure and the discomfort managed *during* and *after* the extraction. During the surgery itself, advancements in anaesthesia mean that you should feel minimal, if any, sharp pain. The focus then shifts to managing post-operative discomfort effectively. While some level of pain and soreness is an expected part of the recovery process, it is typically manageable with medication and diminishes over time. Understanding the sources of pain – both pre- and post-op – and how they are addressed can help alleviate worry and prepare you for the reality of the experience. Pain is not ignored; it is actively managed throughout the entire process, ensuring that while you will likely feel *some* discomfort, it is kept within a tolerable range as your body begins the healing process. This section aims to provide a realistic picture of the pain aspect, offering insight into what to expect and how to best navigate it.
What pain can wisdom teeth cause?
The pain inflicted by problematic wisdom teeth *before* they are removed can be quite severe and disruptive, far exceeding the discomfort of the extraction itself in some cases. This pre-extraction pain is usually a signal that something is going wrong with the wisdom tooth’s development or position. One of the most common culprits is **impaction**. As an impacted tooth attempts to erupt but is blocked, it can press against the roots of the adjacent second molar or against the surrounding bone, creating a deep, persistent ache or pressure sensation in the back of the jaw. This can sometimes radiate upwards towards the ear or cause headaches. If the tooth is partially erupted and covered by a flap of gum (an operculum), **pericoronitis**, an infection of the gum tissue, is highly likely. This causes acute, throbbing pain, often described as intense, localized soreness, accompanied by swelling, redness, and sometimes pus. The pain from infection can make chewing, swallowing, and even talking difficult, and can be constant and debilitating until the infection is treated, and often, the tooth is removed. Misaligned wisdom teeth can also cause pain by pushing against other teeth, leading to generalized soreness or shifting. In rare cases, cysts or tumours forming around an impacted tooth can cause pressure and pain, though these are less common symptoms. The key takeaway is that the pain *caused by* problematic wisdom teeth is often due to ongoing pressure, inflammation, or active infection. This pre-existing pain is often the driving force behind the decision to seek extraction in the first place, seeking relief from the chronic or acute discomfort these misbehaving molars can inflict. It’s a different beast entirely from the surgical discomfort managed after the procedure.
Is it painful to remove wisdom teeth?
Addressing the fear directly: during the *actual process* of wisdom tooth removal, you should not experience sharp or significant pain. This is thanks to the effectiveness of modern **anaesthesia**. Whether you receive local anaesthesia, sedation, or general anaesthesia, the primary goal is to ensure that the surgical site is completely numb or that you are in a state where you don’t perceive pain. With local anaesthesia, the injections might sting briefly, but after they take effect, you will lose sensation in the area where the teeth are being removed. You will likely still be **aware of pressure and movement** during the procedure, especially during the wiggling and loosening stages, but this should not feel like pain. It’s a sensation of force being applied. If you are under sedation, you will be relaxed and potentially drowsy or in a dreamlike state, making you less aware of the sensations, though you might still dimly perceive pressure. Under general anaesthesia, you are completely unconscious and will have no awareness or memory of the procedure itself. Therefore, the surgical act of removal is designed to be painless from the patient’s perspective at that moment. The pain and discomfort occur *after* the anaesthesia wears off, which marks the beginning of the recovery phase. This post-operative pain is due to the surgical trauma to the gums, bone, and surrounding tissues as they begin to heal. But during the procedure itself? No, the objective is a pain-free experience thanks to effective numbing and anaesthetic techniques, allowing the surgeon to work efficiently and the patient to remain comfortable.
What day is wisdom tooth pain the worst?
Understanding the typical timeline of post-operative discomfort is crucial for setting realistic expectations during recovery. While everyone heals slightly differently, the pain and swelling following wisdom tooth extraction tend to follow a predictable pattern, peaking a couple of days after the surgery. The initial hours after the procedure, while the local anaesthesia is still wearing off, might bring mild discomfort. However, as the full effect of the anaesthesia dissipates, usually within a few hours, the pain will start to become more noticeable. Taking your prescribed or recommended pain medication *before* the anaesthesia completely wears off is often advised to manage this transition effectively. The **pain and swelling are generally the worst on days 2 and 3 following the surgery**. This is the period when the body’s inflammatory response to the surgical trauma is typically at its peak. You might experience significant discomfort, soreness, swelling (leading to the characteristic chipmunk cheeks), bruising, and stiffness in the jaw. This peak discomfort can make talking, eating, and opening your mouth difficult. After this peak around day 2-3, you should notice a gradual improvement each day. Pain levels should start to decrease, swelling will begin to subside, and jaw stiffness should lessen. By day 5-7, most of the acute pain should be significantly reduced, though some soreness and tenderness might linger for a week or two, particularly at the extraction site. Understanding that days 2 and 3 are likely to be the most challenging in terms of discomfort can help you prepare mentally and ensure you have adequate pain medication and support during this peak recovery period.
What kind of medication is given after extraction?
Managing pain and preventing infection are key components of post-wisdom tooth extraction care, and medication plays a central role in this. The type of medication prescribed or recommended will depend on the complexity of the extraction and your individual pain tolerance and medical history. For simple extractions, **over-the-counter (OTC) pain relievers** are often sufficient. Non-steroidal anti-inflammatory drugs (NSAIDs) like **ibuprofen (Advil, Motrin)** are commonly recommended because they not only alleviate pain but also help reduce swelling. Acetaminophen (Tylenol) is another option, particularly if you cannot take NSAIDs, though it primarily helps with pain relief without the significant anti-inflammatory effect. For more complex surgical extractions, especially involving impacted teeth, your surgeon will likely prescribe stronger **prescription pain medication**. This could include opioids (like codeine, hydrocodone, or oxycodone), often combined with acetaminophen, or stronger NSAIDs like prescription-strength ibuprofen. These are intended for short-term use during the initial peak of post-operative pain. It’s crucial to take these medications exactly as prescribed, understanding their potential side effects (like drowsiness or constipation) and avoiding activities like driving or operating heavy machinery while on them. In cases where there was an existing infection before the surgery, or if there is a high risk of post-operative infection (for instance, due to compromised immunity or a complex surgical site), your surgeon may also prescribe a course of **antibiotics**. It’s vital to take the full course of antibiotics as directed, even if your symptoms improve, to ensure the infection is fully cleared. Additionally, sometimes a prescription-strength **antiseptic mouthwash** like chlorhexidine is recommended to help keep the surgical sites clean, especially in the days before you can brush normally near the area. Your surgeon will provide clear instructions on which medications to take, how often, and for how long, tailoring the regimen to your specific needs.
Risks and Complications of Wisdom Teeth Removal
While wisdom tooth removal is widely considered a safe and routine oral surgical procedure performed millions of times each year, it is still surgery, and like any surgical intervention, it carries a degree of inherent risk and the potential for complications. Being informed about these possibilities is not meant to alarm you, but rather to provide a realistic understanding of what could potentially happen and how rarely serious issues occur. The vast majority of people undergo the procedure without significant complications, experiencing only the expected post-operative swelling and discomfort. However, being aware of potential risks allows you to recognize the signs if something isn’t progressing as it should and know when to seek professional advice. Common, less serious complications include predictable side effects like bruising or jaw stiffness, while rarer issues can include things like nerve injury or dry socket. Understanding these potential outcomes and, critically, knowing when to contact your dentist or oral surgeon if concerns arise, is an essential part of being a prepared and empowered patient throughout the process. This section aims to outline these possibilities clearly and concisely, placing them in the context of overall procedural safety.
Is wisdom teeth removal safe?
Yes, broadly speaking, **wisdom teeth removal is considered a safe and routine surgical procedure** when performed by qualified and experienced dental professionals, such as oral and maxillofacial surgeons or general dentists trained in surgical extractions. Millions of these procedures are carried out annually worldwide with a very high success rate and minimal incidence of serious, long-term complications. The risks associated with the surgery are well-documented and understood, and surgeons take numerous precautions to minimize them, including thorough pre-operative assessments (like reviewing medical history and X-rays), maintaining sterile surgical environments, and using appropriate anaesthesia and techniques. While there are potential risks, as there are with any surgery, they are generally uncommon, and severe, life-threatening complications are exceedingly rare. The benefits of removing problematic wisdom teeth – preventing pain, infection, damage to adjacent teeth, and other issues – far outweigh the risks for most individuals who require the procedure. The safety profile of wisdom teeth removal is well-established within the medical and dental communities. You can significantly enhance the safety of your procedure by choosing a qualified and reputable surgeon, openly discussing your full medical history and any concerns you have, and diligently following all pre- and post-operative instructions provided by their office. These steps help ensure that potential risks are identified and mitigated, making the procedure as safe as possible for you.
What are the risks of a wisdom tooth extraction?
While generally safe, wisdom tooth extraction, particularly when teeth are impacted, does carry potential risks and complications. Understanding these helps you monitor your recovery. The most common issues include:
-
- **Bleeding:** Some oozing or light bleeding is normal for the first 24 hours. However, persistent, heavy bleeding that doesn’t stop with pressure is a risk, though uncommon.
-
- **Swelling and Bruising:** Significant facial swelling and bruising around the jaw and cheek are very common responses to surgical trauma and are temporary, usually peaking around day 2-3.
-
- **Infection:** While antibiotics may be prescribed, infection at the extraction site can occur. Signs include increasing pain after a few days, swelling, redness, warmth, fever, and pus.
-
- **Dry Socket (Alveolar Osteitis):** This is one of the most painful complications, occurring when the blood clot in the extraction socket dislodges or dissolves prematurely (usually 3-5 days post-op), leaving the bone exposed. It’s significantly more likely with lower tooth extractions and certain risk factors like smoking.
-
- **Nerve Injury (Paresthesia):** The inferior alveolar nerve (running through the lower jaw, controlling sensation in the lower lip, chin, and tongue) and the lingual nerve (controlling sensation and taste in the tongue) are located near lower wisdom teeth roots. There is a small risk of temporary or, very rarely, permanent damage during extraction, leading to numbness, tingling, or altered sensation in the lip, chin, or tongue. The risk varies depending on the nerve’s proximity to the tooth roots as seen on X-rays.
-
- **Damage to Adjacent Teeth:** During removal, there’s a slight risk of inadvertently damaging nearby fillings, crowns, or the second molar itself.
-
- **Sinus Issues:** For upper wisdom teeth, especially those close to the maxillary sinus, there’s a small risk of creating an opening between the mouth and the sinus (oro-antral communication) or displacing a tooth fragment into the sinus. This often heals on its own or may require additional treatment.
-
- **Jaw Stiffness (Trismus):** Difficulty opening the mouth widely due to muscle spasms and swelling is common and usually resolves within a week or two.
- **Fractured Jaw:** This is an extremely rare complication, typically only associated with extremely difficult extractions in patients with underlying bone conditions.
While this list might seem extensive, it’s crucial to remember that these are *potential* complications, and most patients experience only the expected, temporary discomfort of swelling and mild-to-moderate pain managed with medication. Your surgeon will discuss specific risks relevant to your case based on your X-rays.
When to call your dentist or surgeon?
Knowing when to contact your dentist or oral surgeon after wisdom tooth removal is crucial for ensuring your recovery stays on track and addressing potential complications promptly. While some post-operative discomfort, swelling, and light bleeding are normal, certain signs indicate you should seek professional advice. You should **call your dentist or surgeon immediately** if you experience any of the following:
-
- **Excessive or uncontrollable bleeding:** If you are applying firm, constant pressure with gauze pads as instructed, but the bleeding does not slow down or stop after several hours, or if it seems significantly heavier than just oozing.
-
- **Severe pain that is not controlled by prescribed medication:** While some pain is expected, if the medication isn’t providing relief, or if the pain worsens dramatically after the initial few days instead of improving.
-
- **Signs of infection:** This includes fever (temperature over 38°C or 100.4°F), increasing swelling (especially after the first 2-3 days), spreading redness from the extraction site, warmth around the area, or the presence of pus.
-
- **Symptoms of dry socket:** This is characterized by sudden, intense, throbbing pain, often starting 3-5 days after the extraction, sometimes radiating to the ear, accompanied by a bad taste or odour from the socket and the visible loss of the blood clot.
-
- **Persistent numbness:** While numbness from local anaesthesia can last several hours, and nerve-related numbness might persist for days, if you experience complete numbness in your lip, chin, or tongue that does not show any signs of improving after several days (as discussed during your consultation).
-
- **Difficulty breathing or swallowing:** This is an urgent sign and could indicate significant swelling or another serious issue. Go to an emergency room if you cannot reach your surgeon immediately.
- **Medication side effects:** If you experience severe or unexpected reactions to the pain medication or antibiotics.
It’s always better to err on the side of caution. If something feels significantly wrong or different from what your surgeon described as normal recovery, a quick call to their office can provide reassurance or prompt necessary follow-up care. Don’t hesitate; they are there to help manage your post-operative well-being.
Dry socket after wisdom teeth removal
Dry socket, medically known as alveolar osteitis, is arguably one of the most common and certainly the most painful complications that can occur after wisdom tooth extraction, particularly following the removal of lower molars. It’s not an infection, but rather a failure of the blood clot to properly form or remain in the empty tooth socket. After a tooth is extracted, a blood clot naturally forms in the socket, serving as a protective layer for the underlying bone and nerves and initiating the healing process. If this clot gets dislodged, dissolves prematurely, or fails to form adequately, the bone and nerve endings in the socket become exposed to air, food, and fluids. This exposure leads to intense pain, which is often described as severe, throbbing, and radiating pain that can shoot up into the ear or down the neck. Unlike typical post-operative pain which improves over a few days, dry socket pain usually begins 2 to 5 days after the extraction and worsens progressively. Other signs include a foul odour or taste coming from the empty socket, and upon inspection, you might see visible bone instead of a dark blood clot. Risk factors for developing dry socket include smoking (which significantly increases the risk), vigorous rinsing or spitting, using straws (the suction can dislodge the clot), poor oral hygiene, and having a history of dry socket with previous extractions. Treatment involves cleaning out the socket by the dentist or surgeon and packing it with a medicated dressing to protect the exposed bone and nerves. This packing is usually changed every day or two until the pain subsides and the socket begins to heal properly, which can take a week or more. While painful, dry socket doesn’t typically lead to more serious complications like infection, but it definitely prolongs the recovery period and requires professional management to alleviate the intense discomfort. Preventing it involves following your surgeon’s post-operative instructions diligently, particularly avoiding smoking and suction activities.
Wisdom Tooth Removal Recovery: What to Expect
Embarking on the road to recovery after wisdom tooth removal is a key phase that demands patience, care, and strict adherence to post-operative instructions. While the procedure itself is relatively quick, the healing process takes time, varying in duration depending on the complexity of the extraction and individual factors. The immediate period after the surgery will involve managing expected symptoms like swelling, discomfort, and limited jaw movement. The focus then shifts to promoting proper healing of the extraction sites, preventing complications like dry socket or infection, and gradually returning to your normal routine. Understanding the typical recovery timeline and knowing what steps to take (and avoid) is essential for a smooth and efficient healing journey. From managing initial bleeding to gradually reintroducing solid foods and resuming physical activity, each day brings you closer to full recovery. This section provides a detailed roadmap of what to expect during this crucial phase, arming you with the knowledge to navigate it successfully and comfortably, ensuring that the benefits of the extraction are fully realized without undue setbacks.
How long is recovery from wisdom teeth removal?
Defining the duration of wisdom tooth removal recovery involves distinguishing between the initial recovery period and the complete healing of the surgical site. The **initial recovery**, where the most significant symptoms like pain, swelling, and stiffness are present, typically lasts for **3 to 7 days**. During this first week, you will likely be managing discomfort with medication, sticking to a soft diet, experiencing some difficulty opening your mouth, and potentially noticing swelling and bruising. Most people feel significantly better and are able to return to work, school, or light activities within **3 to 5 days**, especially after simple extractions or if they only had one or two teeth removed. However, if you had multiple impacted teeth removed under general anaesthesia, the initial recovery period before you feel ready to resume normal daily life might extend closer to a full week or slightly longer. Beyond this initial phase, the **full healing of the extraction socket** takes much longer. The blood clot needs to be replaced by granulation tissue, which then gets filled in by new bone and covered by gum tissue. This process can take **several weeks, often 6 to 8 weeks, or even up to a few months** for the bone to fully remodel and the socket to completely fill in. While you’ll feel functional and comfortable long before this full healing is complete, activities that could potentially disturb the socket, like vigorous rinsing or poking the area, should be avoided for a longer duration. So, while you’ll likely be back on your feet and feeling relatively normal within a week, the internal healing is a marathon, not a sprint, requiring mindful care during the initial critical period to ensure everything heals as it should.
How long does a wisdom tooth extraction take to heal?
Focusing specifically on the biological process within the empty socket, the healing journey after a wisdom tooth extraction unfolds in stages and is a longer process than just the initial symptomatic recovery period. Immediately after the tooth is removed, the socket fills with blood, forming a crucial **blood clot**. This clot is the foundation of healing, protecting the underlying bone and nerves and serving as a scaffold for new tissue growth. Within the first few days, the body starts to replace this blood clot with **granulation tissue**, a delicate network of blood vessels and connective tissue. This tissue is highly vascular and vital for bringing in the cells needed for repair. Over the following weeks (typically 2-4 weeks), this granulation tissue matures, and the gum tissue around the edges of the socket begins to close in, gradually covering the opening. Simultaneously, the process of **bone remodelling** begins. Specialized cells start laying down new bone within the socket, slowly filling the void where the tooth root used to be. This bony fill-in is a much slower process and can take **several months** (often 4-6 months or even up to a year) for the socket to be fully filled with mature bone and the surrounding bone structure to fully remodel and strengthen. While you won’t feel this internal healing happening after the first few weeks, it’s the reason why dentists might still recommend caution with very hard or sharp foods directly on the extraction site for a longer period, and why the jawbone might appear slightly different on X-rays for some time. So, while you’re generally back to normal activities and pain-free within a week or two, the physical reconstruction of the jawbone at the site takes months to complete, marking the full, complete healing timeline of the extraction socket itself.
Do and don’ts after wisdom teeth removal?
Navigating the post-operative period is critical for preventing complications and ensuring a smooth recovery. Adhering to specific dos and don’ts is paramount.
-
- **DO:**
-
- **Apply ice packs:** Use ice packs or a cold compress on your cheeks, 20 minutes on and 20 minutes off, for the first 24-48 hours to help reduce swelling and bruising.
-
- **Take prescribed medication:** Follow your pain medication and antibiotic regimen exactly as directed. Don’t wait for pain to become severe before taking medication.
-
- **Rest:** Get plenty of rest, especially on the first day. Keep your head elevated with pillows while resting or sleeping to help minimize swelling.
-
- **Eat soft foods:** Stick to a diet of soft, cool foods like yogurt, smoothies, applesauce, soup (lukewarm, not hot), mashed potatoes, and scrambled eggs for the first few days.
-
- **Stay hydrated:** Drink plenty of fluids, but avoid using a straw. Water is best.
-
- **Keep the extraction site clean (gently):** After the first 24 hours, you can start gently rinsing your mouth with warm salt water (1/2 teaspoon salt in a glass of warm water) several times a day, especially after eating, to help keep the area clean. Do not rinse vigorously.
-
- **Resume gentle oral hygiene:** You can usually start gently brushing your teeth the day after surgery, being very careful to avoid the extraction sites initially. Gradually progress to brushing the surrounding areas as comfort allows.
-
- **DON’T:**
-
- **Don’t smoke or use tobacco products:** This is one of the biggest risk factors for dry socket and significantly impairs healing. Avoid it completely during recovery.
-
- **Don’t drink alcohol:** Alcohol can interfere with pain medications and the healing process.
-
- **Don’t use straws:** The suction created by drinking through a straw can easily dislodge the protective blood clot, leading to dry socket.
-
- **Don’t rinse vigorously or spit forcefully:** This can also dislodge the blood clot. Use gentle rinsing and let the water passively flow out of your mouth.
-
- **Don’t eat hard, crunchy, chewy, or hot foods:** These can irritate the surgical site, dislodge the clot, or get stuck in the socket. Avoid popcorn, nuts, chips, steak, etc., for at least a week or two.
-
- **Don’t exercise strenuously:** Avoid heavy lifting or strenuous physical activity for the first few days, as this can increase bleeding and swelling. Gradually reintroduce exercise as you feel able.
- **Don’t constantly poke the extraction site** with your tongue or fingers. Leave the clot undisturbed.
Following these guidelines diligently will significantly improve your comfort and reduce the risk of complications, paving the way for a smoother recovery.
How soon can you eat after wisdom teeth removal?
You can typically begin eating relatively soon after wisdom teeth removal, but the key is to start with **soft foods** and be mindful of the surgical sites. You should wait until the local anaesthesia has completely worn off before attempting to eat anything. This is crucial to avoid accidentally biting your numb lips, cheeks, or tongue. Once feeling has returned to normal, which usually takes a few hours, you can safely start consuming liquids and very soft, cool foods. Think **smoothies (without a straw!), yogurt, applesauce, pudding, lukewarm soup (avoiding anything hot as heat can increase swelling and bleeding), and ice cream (plain, without solid bits or cones)**. The coolness can also be soothing. Over the next few days, as your comfort level improves and swelling begins to subside, you can gradually progress to slightly more substantial soft foods. This might include mashed potatoes, scrambled eggs, soft pasta, well-cooked vegetables, or soft fish. Avoid any foods that require significant chewing, are hard, crunchy, sticky, or have small particles that could get lodged in the sockets (like seeds, nuts, rice, popcorn, chips, or toast) for at least a week, or as long as your surgeon advises. Chewing near the extraction sites should also be minimized initially, opting to chew on the opposite side of your mouth if only one side was worked on. Listen to your body; if eating a certain food causes pain or discomfort, stick to softer options for a little longer. The general rule is to start very soft and cool, and slowly transition back to your normal diet over the course of about a week, depending on how your individual healing progresses. Hydration is also vital, so make sure you are drinking plenty of water throughout the day.
How to sleep with wisdom teeth removal?
Sleeping comfortably and safely after wisdom tooth removal requires a few simple adjustments to your usual routine to minimize swelling and promote healing. The most important recommendation is to **sleep with your head elevated**. Use several pillows to prop up your head and upper body. Keeping your head higher than the rest of your body helps reduce blood flow to the surgical sites, which in turn helps to control swelling and reduce bleeding. This elevated position should be maintained for the first few nights, or as long as you notice significant swelling. Secondly, try to **avoid sleeping directly on the side of your face** where the teeth were extracted, especially if you had more extractions or more complex surgery on one side. Sleeping on your back is generally the preferred position as it maintains the elevation and prevents pressure on the cheeks. If you must sleep on your side, try sleeping on the side *opposite* to the extractions, if possible. If teeth were removed on both sides, sleeping on your back with elevated pillows is the best strategy. Be prepared for some discomfort, which might make falling asleep challenging initially. Taking your pain medication as prescribed before bedtime can help manage this. You might find yourself waking up more frequently during the night due to soreness or the need to adjust your position. Creating a comfortable sleep environment – dark, quiet, and cool – can also help. Remember that good rest is crucial for healing, so prioritize getting as much sleep as possible, even if it’s broken sleep initially. Maintaining head elevation is the most impactful step you can take while sleeping to support your recovery.
How long will it bleed after wisdom tooth extraction?
Some amount of bleeding or oozing is entirely normal and expected after wisdom tooth removal, and it can persist for up to **24 hours** following the procedure. Immediately after the teeth are extracted, the surgeon will place thick gauze pads over the extraction sites and instruct you to bite down firmly. This pressure helps to control bleeding and encourages the formation of a stable blood clot in the socket. You will likely need to change these gauze pads periodically in the hours following surgery. When you change the gauze, some light bleeding might still be present; this is not necessarily cause for alarm. The bleeding should gradually lessen over the first 24 hours. It might change from bright red blood to a more pinkish or reddish-brown colour mixed with saliva as the hours pass. It’s important to distinguish between active bleeding (where the gauze is quickly saturated with bright red blood) and light oozing (where the gauze or your saliva is just tinged with pink or red). Light oozing can continue for several days. If you experience significant bleeding that doesn’t seem to slow down after applying fresh, firm pressure with gauze for 30-60 minutes, you should contact your oral surgeon’s office. Avoid rinsing your mouth or spitting frequently during the first 24 hours, as this can dislodge the developing blood clot and prolong bleeding. Gently biting on a moistened tea bag (the tannic acid can help with clotting) is an old remedy sometimes suggested for persistent oozing, but consult your surgeon first. The primary goal for the first 24 hours is to maintain gentle pressure and allow the blood clot to form undisturbed; this is your body’s natural way of stopping the bleeding and starting the healing process.
Are there stitches in wisdom teeth?
Yes, it is common for **stitches (sutures)** to be placed in the gums after wisdom tooth extraction, particularly following surgical removal of impacted teeth or when incisions were made to access the tooth. The primary purposes of these stitches are to help **close the gum incision** that was made to reach the tooth, to **hold the gum tissue in place** around the extraction socket, and to help **keep the blood clot stable** within the socket. By bringing the edges of the gum tissue together, stitches protect the extraction site from food particles and bacteria, promote faster initial healing of the soft tissue, and reduce the risk of the blood clot becoming dislodged, which helps prevent dry socket. Not all wisdom tooth extractions require stitches. If a tooth was fully erupted and removed simply without needing an incision, stitches might not be necessary. The type of stitches used can vary. Most commonly, oral surgeons use **dissolvable stitches**. These are made from materials that the body gradually breaks down and absorbs over the course of about a week to 10 days, meaning they do not need to be manually removed. As they dissolve, they might start to loosen and fall out on their own, which is a normal part of the healing process. Less commonly, non-dissolvable stitches might be used, which would require a follow-up appointment with your surgeon typically about a week after the surgery to have them removed. Your surgeon will inform you during your post-operative instructions whether stitches were used and if they are dissolvable or require removal. You might feel the stitches with your tongue, and they can sometimes feel a bit irritating, but it’s important not to pick at them.
What happens after wisdom teeth removal?
Immediately following your wisdom tooth removal procedure, you will be taken to a recovery area, especially if you received sedation or general anaesthesia. The surgical team will monitor you as you recover from the anaesthetic effects. You will have gauze pads in your mouth over the extraction sites, and you’ll be instructed to bite down on them firmly to control bleeding. Once you are fully awake, alert, and stable, the surgical team will provide you with crucial **post-operative instructions**. These instructions cover everything you need to know for the next few days and weeks: how to manage pain (timing and dosage of medication), instructions regarding swelling (using ice), dietary restrictions (what to eat and avoid), oral hygiene guidelines (when and how to gently clean), activity restrictions (avoiding strenuous exercise), and when and how to change the gauze pads. They will also provide contact information and explain signs of potential complications that warrant calling the office. Before you are discharged, your ride (the responsible adult who brought you) will need to be present and will also receive instructions. You will then be sent home to rest and begin the recovery process. The first 24-48 hours at home are typically when you’ll experience the most significant swelling, some bruising, and discomfort. You will need to stick to liquids and soft foods, take your pain medication regularly, apply ice packs, and rest with your head elevated. Over the following days, the swelling and pain should gradually start to decrease. Follow-up appointments are sometimes scheduled within a week or two to check on healing, remove stitches if necessary, and address any concerns. It’s a period of rest, careful management of symptoms, and allowing your body to heal from the surgical procedure.
How many days should I take off for wisdom teeth recovery?
The number of days you should plan to take off from work, school, or strenuous activities for wisdom teeth recovery is variable and depends significantly on the **complexity of your extraction** and your body’s individual healing response. For **simple extractions** of fully erupted wisdom teeth, many people feel well enough to return to normal, non-strenuous activities within **1 to 2 days**. You might still experience some mild discomfort and swelling, but it’s usually manageable. However, if you had **more complex surgical extractions**, involving impacted teeth, bone removal, and multiple stitches, the recovery period is typically longer. For these cases, it’s highly recommended to plan to take off at least **3 to 5 days**, and sometimes up to a full week. This allows ample time for the initial swelling and pain to subside significantly, for you to maintain a soft diet, and to avoid dislodging the blood clot. Factors like the type of anaesthesia used can also play a role; recovering from general anaesthesia or deep IV sedation usually requires a full day of rest alone. Furthermore, consider the nature of your work or activities. If your job involves heavy lifting, physical exertion, or significant talking, you might need more time off than someone with a sedentary desk job. Strenuous activity too soon can increase bleeding, swelling, and pain. Discuss your specific procedure and job/lifestyle requirements with your oral surgeon during your consultation. They can provide a personalized recommendation based on their assessment of your case, helping you plan accurately for the necessary downtime to ensure a smooth and effective recovery period without rushing it. It’s generally better to err on the side of taking slightly more time off than you think you’ll need, rather than rushing back and potentially delaying your healing or causing complications.
Specific Issues and Considerations
Beyond the general process of extraction and recovery, there are certain specific issues, scenarios, and common questions related to wisdom teeth that warrant focused discussion. These touch upon the nuances of impaction, potential nerve involvement with lower teeth, common misconceptions (like effects on jawline), and the typical age window for the procedure. While the core principles of wisdom tooth extraction apply broadly, understanding these specific considerations can provide a more complete picture and address particular concerns individuals might have based on their unique situation. Delving into these areas adds depth to our comprehensive guide, moving from the general ‘what and why’ to the ‘how it affects me’ aspects, including issues tied to tooth position, anatomical proximity, and timing.
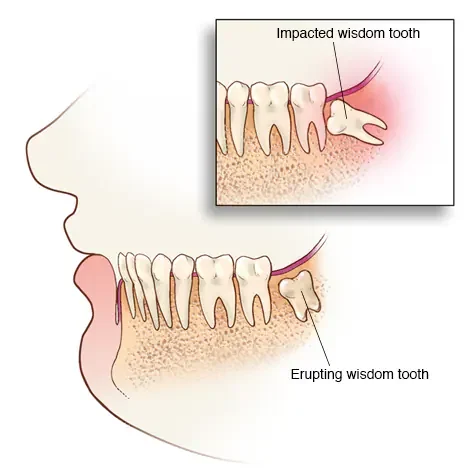
Impacted wisdom teeth
The concept of **impacted wisdom teeth** is central to understanding why so many extractions are necessary and often more complex than removing other teeth. An impacted tooth is one that is partially or completely trapped within the jawbone or under the gum tissue and is unable to erupt into its normal position due to a physical obstruction. This obstruction is typically another tooth, bone, or dense gum tissue. Impacted wisdom teeth come in various types based on their orientation and depth within the jawbone:
-
- **Mesial Impaction:** The most common type, where the tooth is angled forward, towards the front of the mouth.
-
- **Distal Impaction:** The tooth is angled backward, towards the back of the mouth.
-
- **Vertical Impaction:** The tooth is upright but cannot erupt because it’s stuck against the tooth in front or covered by too much bone.
- **Horizontal Impaction:** The tooth is lying completely on its side, usually pushing directly into the root of the adjacent second molar.
Impacted teeth are problematic because they can exert pressure on neighbouring teeth, leading to crowding or damage; they are difficult or impossible to clean properly, increasing the risk of decay and gum disease; and they can create pockets under the gum tissue that trap bacteria, causing recurrent infections (pericoronitis). Deeply impacted teeth can also be associated with the formation of cysts or tumours, although this is less common. The presence of impaction almost always necessitates surgical removal rather than a simple extraction, as it involves accessing the tooth through gum incisions, potentially removing bone, and often sectioning the tooth for easier removal. The depth and angle of impaction directly correlate with the complexity and potential risks (like nerve involvement) of the extraction procedure. Identifying the type and degree of impaction through X-rays is a critical step in planning the surgical approach and informing the patient about what to expect during and after the procedure.
Issues with lower wisdom teeth
While both upper and lower wisdom teeth can become problematic and require extraction, lower wisdom teeth often present unique challenges and considerations due to their anatomy and location within the mandible (lower jawbone). One of the primary concerns specific to lower wisdom teeth, especially those that are deeply impacted or positioned horizontally, is their close proximity to the **inferior alveolar nerve**. This sensory nerve runs through a canal within the lower jawbone and provides sensation to the lower lip, chin, and some of the gums. In some individuals, the roots of the lower wisdom tooth can be very close to or even wrapped around this nerve canal, a relationship clearly visible on detailed X-rays or 3D scans. Extracting such teeth carries a small, but potential, risk of injuring this nerve, which can result in **temporary or permanent numbness (paresthesia)** in the lower lip and chin. While permanent nerve damage is rare, temporary numbness or altered sensation is a recognized risk that surgeons carefully assess and discuss with patients. Another issue is the **density of the lower jawbone** compared to the upper jaw. The mandible is denser bone, making the surgical removal of impacted teeth, especially those covered by a significant amount of bone (bony impactions), potentially more complex and requiring more bone removal than with upper teeth. Lower extractions are also more commonly associated with **dry socket** compared to upper extractions, although the exact reasons aren’t fully understood, likely related to blood supply and the size of the socket. Finally, lower wisdom teeth infections (pericoronitis) tend to be more acutely painful and can sometimes lead to swelling that affects the ability to open the mouth widely (trismus) more severely than upper tooth infections. These factors contribute to lower wisdom tooth extractions often being considered slightly more complex and carrying a higher potential for certain post-operative complications than their upper counterparts, necessitating careful surgical planning and patient education.
Does removing wisdom teeth affect the jawline?
A common concern or myth circulating is whether getting wisdom teeth removed will somehow change the shape or definition of your jawline. Let’s address this directly: **removing wisdom teeth does not typically affect the appearance or structure of your jawline or facial shape.** This misconception might arise because wisdom teeth are the last to emerge and are located at the back of the jaw, leading some to believe they contribute significantly to the jaw’s structure or size. However, the jawbone’s size and shape are determined by genetics and growth processes that occur much earlier in life, long before wisdom teeth typically emerge. By the time you’re in your late teens or early twenties, your jawbone has largely completed its growth. While the teeth sit within the jawbone, their presence or absence, especially at the very back, does not alter the underlying bone structure that defines the jawline contour. Think of it this way: removing a house from a plot of land doesn’t change the fundamental shape of the land itself. Similarly, removing the teeth from the jawbone doesn’t remodel the bone that gives your jaw its visible shape. Any minor changes in facial appearance immediately after surgery are temporary and due solely to post-operative swelling and bruising, which resolve within a week or two. There might be a very subtle change in the bone density immediately surrounding the extraction site as it heals, but this is internal and does not impact the external appearance of the jawline. So, rest assured, electing to have your wisdom teeth removed for health reasons will not fundamentally change the aesthetic contour of your jaw.
What’s the average wisdom teeth removal age?
The typical age range for wisdom teeth removal aligns closely with when these teeth are most likely to emerge and potentially cause problems. The **average age for wisdom teeth removal falls predominantly between the late teenage years (around 17 or 18) and the mid-twenties (around 25)**. This timeframe is significant for several reasons. Firstly, it’s when the third molars usually attempt to erupt. Secondly, during this period, the roots of the wisdom teeth are often still developing and may not be fully formed. This can make extraction surgically easier, as the tooth might be less firmly anchored in the bone, and the risk of nerve injury can sometimes be lower if the root formation is incomplete and further from the nerve canal. Additionally, the bone surrounding the teeth in younger adults is generally less dense and more elastic than in older adults, which can also facilitate easier removal and potentially faster healing. Dentists and oral surgeons often recommend evaluating wisdom teeth in this age group, even if they are not yet symptomatic, to assess their position and predict whether they are likely to cause future problems. Removing them preemptively in this age window can be beneficial for these surgical and recovery reasons. However, it’s important to note that wisdom teeth can be removed at *any* age if they are causing pain, infection, or other issues. While the surgery and recovery might be slightly more involved in older adults due to denser bone and fully formed roots, age itself is not a barrier to necessary extraction if the teeth are problematic. The “average age” simply reflects the window when problems most commonly manifest and preventative removal is often considered most advantageous.
Wisdom Teeth Removal NHS and UK Specific Information
For individuals in the United Kingdom considering wisdom tooth removal, understanding the process within the National Health Service (NHS) framework is vital, as it differs significantly from seeking private dental care. The availability and criteria for NHS treatment are governed by specific guidelines focused on clinical necessity, which impacts who qualifies for the procedure and how they access care. Navigating the system requires awareness of these criteria and the typical referral pathway. Costs on the NHS are also structured differently, falling under set dental charge bands rather than variable private fees. This section aims to clarify these UK-specific points, providing essential information for those navigating the NHS system for wisdom tooth extraction.
wisdom tooth removal nhs
Within the NHS in the UK, wisdom tooth removal is not automatically performed simply because the teeth are present or even impacted. The criteria for extraction are based on clinical need, primarily guided by the **National Institute for Health and Care Excellence (NICE) guidelines**. These guidelines, last updated in 2000, recommend against the routine removal of symptomless impacted wisdom teeth. NHS extraction is generally advised only when problematic wisdom teeth are causing or contributing to active pathology. This pathology includes situations like recurrent episodes of infection (pericoronitis), non-restorable decay in the wisdom tooth or the adjacent tooth due to the wisdom tooth’s position, the formation of cysts or tumours, or internal or external resorption of the tooth or adjacent tooth root caused by the wisdom tooth. Essentially, the NHS will typically only fund the removal if the wisdom teeth are causing demonstrably harmful issues or are clearly diseased. Asymptomatic impacted wisdom teeth, even if they might theoretically cause problems in the future, are usually not grounds for extraction under current NHS policy unless there are specific, extenuating clinical circumstances justifying the procedure. This is a key distinction from some private practices where preventative removal of asymptomatic but clearly impacted teeth might be more commonly offered. Understanding these NHS criteria is essential for managing expectations about whether your wisdom tooth removal will be covered by the public healthcare system. Your general dentist will assess whether your situation meets the NICE guidelines for referral and potential treatment on the NHS.
Do I need to be referred for wisdom teeth removal?
Yes, in the UK, if you are seeking wisdom tooth removal through the NHS, you will almost certainly **need to be referred** by a general dental practitioner (your regular dentist). You cannot typically self-refer directly to an oral surgeon or hospital service for wisdom tooth extraction on the NHS. The process usually begins with you visiting your general dentist because you are experiencing symptoms or during a routine check-up where they identify a problematic wisdom tooth. Your dentist will examine your mouth, take X-rays (if necessary), and assess whether your wisdom teeth meet the criteria for removal under the NHS NICE guidelines (i.e., if they are causing current pathology). If your dentist determines that extraction is clinically necessary according to these guidelines, they will then **write a referral letter** to the appropriate secondary care service. This referral is typically made to an oral and maxillofacial surgery department in a hospital or sometimes to a community dental service that handles more complex extractions. You will then be placed on a waiting list to be seen by a specialist or surgeon who will further assess your case and potentially schedule the extraction. This referral pathway ensures that patients accessing NHS services for wisdom tooth removal are assessed based on clinical need by experienced practitioners and directed to the appropriate level of care. While the referral is necessary for NHS treatment, if you choose to pursue private wisdom tooth removal, you can often contact an oral surgeon’s clinic directly, though some may still prefer a referral from your general dentist for comprehensive patient information.
wisdom teeth removal cost uk nhs
Understanding the cost of wisdom teeth removal in the UK depends entirely on whether the procedure is carried out through the **NHS** or **privately**. If your wisdom tooth removal is deemed clinically necessary by a dentist and meets the NHS NICE guidelines, and is subsequently performed within the NHS system (either in a general dental practice capable of performing the extraction or, more likely, in a hospital setting following a referral), the cost will fall under the standard NHS dental charge bands. As of the current charging structure in England, a typical wisdom tooth extraction would fall under **Band 2** (£76.00 as of April 2024). This band covers a range of treatments, including extractions, fillings, and root canal treatment. If the extraction is more complex and requires additional procedures like X-rays or examinations as part of the course of treatment leading up to the extraction, the overall treatment might fall into **Band 3** (£333.70 as of April 2024), which covers complex treatments like dentures, bridges, and crowns, or multiple extractions requiring laboratory work or extensive planning. However, for a single extraction, Band 2 is more common. It’s crucial to note that this NHS charge is a flat fee for the *entire course of treatment* within that band, not per tooth. So, if you have multiple wisdom teeth removed in the same course of treatment, you would still typically only pay the Band 2 or Band 3 charge once. This is significantly different from **private costs**, which can vary widely based on the factors mentioned earlier (number of teeth, complexity, anaesthesia type, surgeon’s fee, clinic location) and can range from a few hundred pounds per tooth for simple cases under local anaesthesia to several thousand pounds for multiple complex extractions under general anaesthesia in a private hospital. The NHS provides a substantially more affordable option, but eligibility is strictly based on clinical necessity according to national guidelines.
Frequently Asked Questions About wisdom extraction
It’s natural to have a barrage of questions when facing something like wisdom tooth removal. The process, recovery, potential discomfort, and costs can all be sources of uncertainty. To help consolidate key information and address the most common queries head-on, this section compiles some frequently asked questions about wisdom extraction. Think of it as a quick recap and clarification of the points we’ve covered, offering concise answers to the questions most people ask when contemplating or preparing for this common oral surgery. From defining the procedure to setting expectations for recovery, these FAQs aim to provide quick, accessible answers to your lingering questions, empowering you with confidence as you navigate the experience.
What is wisdom teeth removal?
Wisdom teeth removal, also known as wisdom tooth extraction or wisdom extraction, is a common oral surgical procedure performed to remove one or more of the four adult teeth located at the very back of your mouth. These teeth, medically referred to as the third molars, typically emerge (or attempt to emerge) between the ages of 17 and 25. The procedure is undertaken when wisdom teeth cause current problems, such as pain, infection, swelling, impaction (being trapped beneath the gums or bone), overcrowding of other teeth, damage to adjacent teeth, or the formation of cysts. It can also be recommended preventatively if examination and X-rays indicate a high likelihood of future problems due to the tooth’s position or impaction status. The complexity of the removal varies depending on whether the tooth is fully erupted or impacted, and the surgery can range from a relatively simple extraction (similar to removing any other visible tooth) to a more complex surgical procedure involving incisions, bone removal, and stitches for impacted teeth. The procedure is usually performed by a general dentist or, more commonly for complex cases, by an oral and maxillofacial surgeon, using local anaesthesia, sedation, or general anaesthesia to ensure patient comfort throughout the extraction process. The primary goal is to alleviate existing symptoms and prevent future oral health complications caused by problematic wisdom teeth.
Is wisdom teeth removal a major surgery?
Classifying wisdom teeth removal as “major surgery” depends on how one defines “major.” Compared to highly invasive procedures like open-heart surgery or complex abdominal surgery, wisdom teeth removal is generally **not considered a major surgery** in that sense. It is typically performed as an outpatient procedure (meaning you go home the same day), often in a dental office or specialized oral surgery clinic rather than a hospital operating room (unless general anaesthesia is required or for medically complex patients). However, it is undeniably a **surgical procedure** that involves cutting into tissues (gums), potentially removing bone, and requires anaesthesia. For simple extractions of fully erupted teeth, it might be considered a minor surgical procedure. But for impacted wisdom teeth, which are trapped within the bone and require a more involved surgical approach, it is certainly a more significant intervention than a routine dental filling or simple tooth cleaning. Therefore, while not “major” in the context of life-threatening or system-altering operations, it is definitely more than a trivial dental procedure and should be treated with appropriate respect for the recovery process it entails. It carries risks inherent to any surgery, requires specific post-operative care, and can lead to temporary but significant discomfort. So, while not “major” in the highest medical sense, it is a proper surgical procedure requiring careful consideration and recovery time.
How long is recovery from wisdom teeth removal?
The length of recovery from wisdom teeth removal can be viewed in two phases: the initial recovery from the most acute symptoms and the complete healing of the extraction socket. The **initial recovery period**, during which most people experience swelling, pain, and stiffness, typically lasts for **3 to 7 days**. During this first week, discomfort is managed with medication, and diet is restricted to soft foods. Most individuals feel well enough to return to their normal daily routines, such as work or school (avoiding strenuous activity), within **3 to 5 days** for most cases, although more complex extractions might require a full week off. Beyond this initial phase, the **complete healing of the extraction socket**, where the bone remodels and fills in the void left by the tooth root, is a much longer process. This internal healing can take **several weeks, often 6 to 8 weeks, and potentially up to several months (4-6 months)** for the bone to fully mature and the site to regain its full strength. While you won’t feel this internal healing day-to-day after the first couple of weeks, it means the area is still somewhat vulnerable during this extended period. Therefore, while you’ll likely feel functional and comfortable much sooner, the complete biological restoration of the surgical site is a process that unfolds over a longer timeframe, though it doesn’t typically interfere with your ability to resume normal eating and activities after the initial symptomatic recovery period.
How painful is wisdom tooth extraction?
During the actual wisdom tooth extraction procedure itself, you should not experience significant pain thanks to effective **anaesthesia**. Whether you receive local anaesthesia, sedation, or general anaesthesia, the surgical site will be numbed, or you will be in a state where you do not consciously perceive pain. You might feel pressure or movement, especially during the loosening of the tooth, but this should not feel like sharp pain. The pain associated with wisdom teeth removal primarily occurs **after the anaesthesia wears off**, as part of the normal post-operative healing process. This post-operative discomfort is due to the trauma to the gums, bone, and surrounding tissues during the surgery. The intensity and duration of this pain vary depending on the complexity of the extraction; removing impacted teeth typically results in more post-operative pain than removing erupted ones. Pain and swelling often **peak around days 2 and 3** following the surgery before gradually subsiding. This discomfort is managed effectively with pain medication, which can range from over-the-counter options like ibuprofen to prescription-strength pain relievers, depending on the severity. While there will be pain during recovery, it is generally manageable with medication and time, and certainly less debilitating than the chronic pain that problematic impacted or infected wisdom teeth can cause before removal.
Is wisdom teeth removal safe?
Yes, in the vast majority of cases, wisdom teeth removal is considered a **safe and routine oral surgical procedure**. It is one of the most common surgeries performed worldwide by qualified general dentists and oral and maxillofacial surgeons, with a very high success rate. Like any surgical procedure, it does carry potential risks and complications, such as bleeding, swelling, bruising, infection (including dry socket), nerve injury (usually temporary numbness), damage to adjacent teeth, or sinus issues (for upper teeth). However, serious, long-term complications are rare. The risks are well-understood by dental professionals, and numerous precautions are taken during the pre-operative assessment and the procedure itself to minimize them. For most individuals who require the procedure due to problematic or potentially problematic wisdom teeth, the long-term benefits of preventing pain, infection, damage, and other issues far outweigh the relatively low risks associated with the surgery. Choosing an experienced and qualified surgeon, providing a complete medical history, and strictly following all pre- and post-operative instructions are key factors in ensuring the procedure is as safe as possible for you.