Key Takeaways
- Teeth reconstruction is a comprehensive process to rebuild damaged or missing teeth and restore oral function.
- It’s necessary for widespread issues like severe wear, trauma, extensive decay, or bite problems.
- The process involves multiple phases and procedures, often including crowns, bridges, and implants.
- Benefits include restored chewing function, pain relief, improved oral health, and a renewed smile.
- Cost is highly variable, ranging from tens of thousands of dollars, and recovery depends on the procedures involved.
- Finding a prosthodontist or experienced restorative dentist is crucial.
Can Dentists Reconstruct Teeth? Understanding teeth reconstruction
Let’s cut right to the chase, shall we? The question isn’t whether this is some futuristic fantasy plucked from the pages of a sci-fi novel. It’s happening, right now, in dental practices equipped with cutting-edge technology and populated by practitioners possessing a blend of surgical precision and artistic vision. Teeth reconstruction, often bandied about under grander titles like “full mouth reconstruction” or “full mouth restoration,” is not merely a procedure; it’s a comprehensive strategy. Think of it less as a simple repair job and more as overseeing the construction of a new building where the old one crumbled. It necessitates a holistic view of the entire oral system – teeth, gums, bone structure, muscles, and jaw joints – understanding how they interact and where the fundamental breakdown has occurred. It’s the domain of highly skilled dentists, frequently those who’ve pursued advanced training specifically in restorative dentistry or prosthodontics, the specialists dedicated to designing, manufacturing, and fitting artificial replacements for teeth and other parts of the mouth. Their expertise goes far beyond filling cavities or placing single crowns; they are the architects of the mouth, capable of tackling complex cases involving widespread decay, severe wear, trauma, congenital defects, or long-standing bite issues. Their goal? To restore form *and* function. To give you teeth that not only look good but allow you to chew effectively, speak clearly, and live without chronic pain. It’s a testament to the incredible advancements in dental science that what once might have seemed irreversible damage is now routinely addressed with predictable, life-enhancing outcomes. It’s about taking a compromised oral structure and meticulously, painstakingly, rebuilding it, tooth by tooth, arch by arch, until harmony and health are restored. This is the realm of sophisticated diagnostics, detailed planning, and the execution of a sequence of treatments designed specifically for *you*. It’s proof that dental decline isn’t necessarily a one-way street.
Can you reconstruct teeth?
Absolutely, unequivocally, teeth can be reconstructed. This isn’t just a theoretical possibility; it’s a standard, albeit complex, branch of modern dentistry that has transformed the lives of countless individuals whose oral health has been severely compromised. When we talk about reconstruction, we’re not usually referring to a simple filling or even a single crown on an otherwise healthy tooth. We’re talking about a scenario where multiple teeth are damaged, missing, or significantly compromised, impacting not just aesthetics but, crucially, function and overall oral health. The process is akin to a master restorer working on a priceless, damaged antique – it requires intricate knowledge, skilled hands, and a detailed plan to bring it back to its original glory, or often, even better than its original state, correcting underlying flaws that may have led to the damage in the first place. It involves a cascade of potential interventions, a tailored symphony of procedures orchestrated by a qualified dental professional, sometimes even a team of specialists. The beauty of contemporary reconstructive dentistry lies in its customisation; there’s no one-size-fits-all approach. The specific procedures employed, the sequence in which they are performed, and the materials used are all determined by the individual’s unique clinical presentation, their overall health, and their goals. The aim is always multifaceted: to eliminate pain, restore proper chewing function, correct bite imbalances that can lead to further damage or discomfort, protect remaining healthy tooth structure, and, yes, create a smile that the patient feels confident sharing. It’s a journey that demands patience and commitment from the patient, but the ability to confidently eat, speak, and smile again is a profound reward that underscores the powerful reality of modern dental reconstruction. It represents a path forward from what might feel like irreparable damage.
Can I rebuild my teeth?
From the patient’s perspective, the answer is a resounding yes, you *can* undergo the process to rebuild your teeth. However, it’s crucial to understand that this isn’t a DIY project or something you achieve through sheer willpower alone. The ‘rebuilding’ is performed *for* you, and *with* you, by a team of qualified and experienced dental professionals. Your role in this process is fundamental – it begins with recognising the need, seeking consultation, committing to the treatment plan, and diligently following through with appointments and post-treatment care. Think of yourself as the essential client and collaborator in this intricate project. It starts with a detailed, often lengthy, consultation where a comprehensive diagnosis is made. This isn’t just a quick peek inside your mouth; it involves thorough examination, advanced imaging techniques like X-rays and 3D scans, taking impressions to create models of your bite, and assessing the health of your gums and jaw joints. Based on this exhaustive evaluation, the dental team will develop a personalised treatment plan. This plan is your roadmap to a rebuilt smile. It will outline the necessary procedures, the expected timeline, the materials that will be used, and the anticipated costs. Your active participation in understanding and agreeing to this plan is vital. You have the agency to pursue this transformation, to work with experts who possess the knowledge and skills to execute the complex procedures required. It’s a partnership: their expertise, your commitment, culminating in the restoration of your oral health and confidence. So, while you aren’t physically performing the dental work yourself, you absolutely *can* initiate and undergo the treatment necessary to have your teeth rebuilt by those who are highly trained and equipped for this specific kind of sophisticated restoration. It is, truly, a collaborative effort where you are the central figure in your own oral health revival.
What Is a Full Mouth Reconstruction?
At its core, Full Mouth Reconstruction is the apex of complex restorative dentistry. It’s not merely adding or fixing individual teeth in isolation; it’s a sophisticated, all-encompassing undertaking that involves rebuilding or restoring *all* the teeth, or a significant majority of them, within both the upper and lower jaws. The scope is total. It’s the strategic overhaul required when the structural integrity, function, and aesthetics of the entire masticatory system have been compromised by a confluence of problems – extensive decay, severe wear due to grinding (bruxism), acid erosion, trauma that has caused multiple fractures or tooth loss, or long-standing bite discrepancies (malocclusion) that have led to pain and damage. Unlike a “smile makeover,” which focuses primarily on the aesthetic enhancement of visible teeth in a healthy mouth (think veneers or whitening on otherwise sound teeth), full mouth reconstruction is fundamentally rooted in *restoring function and health*. While the aesthetic outcome is invariably a significant and often dramatic benefit, it’s secondary to re-establishing a stable, functional bite, eliminating pain, and ensuring the long-term health and stability of the teeth and supporting structures. It’s a process that often involves multiple phases, potentially spanning months or even years, and frequently requires the coordinated efforts of general dentists, prosthodontists, oral surgeons, periodontists (gum specialists), and orthodontists (bite specialists). It’s a complex, often iterative, process of diagnosis, planning, treatment, and refinement, addressing underlying issues before placing final, definitive restorations. It’s a commitment to comprehensive care, designed to treat the mouth as an integrated system, ensuring that the final result is not just superficially appealing but fundamentally sound, comfortable, and built to last, tackling problems systemically rather than piecemeal.
What Is Full Mouth Restoration Dentistry?
Full Mouth Restoration Dentistry can be understood as the clinical discipline or practice area dedicated to the comprehensive rebuilding of a patient’s bite and smile when significant damage or wear has occurred across the entire mouth. It’s the specialised field that encompasses the principles, techniques, and coordination required for full mouth reconstruction. Think of it as the overarching banner under which these complex, multi-disciplinary treatments fall. Practitioners in this field possess a deep understanding of occlusion (how the upper and lower teeth come together), biomechanics (how forces are distributed throughout the mouth), and the intricate interplay between teeth, gums, bone, muscles, and the jaw joints. They are skilled in diagnosis, complex treatment planning, and the execution or coordination of a wide array of procedures necessary to bring a severely compromised mouth back to optimal health and function. While “reconstruction” often highlights the aspect of *building anew*, particularly after extensive loss or damage, “restoration” tends to emphasise *bringing back* to a previous state of health or function, often involving saving and rebuilding existing teeth alongside replacing missing ones. In the context of a severely damaged mouth, the terms are, frankly, used pretty much interchangeably in everyday practice, both referring to the same comprehensive, complex approach to oral rehabilitation. Full mouth restoration dentistry is about looking at the mouth not as 32 individual units, but as a single, interconnected system that needs to function harmoniously. It requires a level of expertise and strategic thinking that goes beyond routine dental care, bringing together various restorative techniques and potentially multiple specialists to achieve a unified, healthy, and functional outcome. It’s the practice area where dental professionals tackle the most challenging cases, offering hope and tangible results to those with widespread oral health issues.
When Is Dental Reconstruction Necessary? Who Requires It?
Dental reconstruction isn’t a capricious choice or a purely elective cosmetic procedure, at least not in the way a simple tooth whitening might be. It is a necessity born out of significant oral health challenges that compromise function, health, and often, cause chronic pain and discomfort. The need for such extensive work arises when dental problems are widespread, severe, and interconnected, affecting multiple areas of the mouth and impacting the entire masticatory system. We’re talking about situations where addressing individual teeth in isolation simply won’t suffice, because the underlying issues – be it bite collapse, extensive wear, widespread infection, or significant tooth loss – affect the mouth as a whole unit. It’s required when the current state of the mouth threatens not just future dental health but also impacts overall quality of life, making basic functions like eating and speaking difficult or painful. The decision to pursue full mouth reconstruction is typically reached after a thorough and often illuminating diagnostic process that reveals the depth and breadth of the problems at hand. It’s not something recommended lightly; it’s a major undertaking proposed when less comprehensive treatments are simply insufficient to restore the patient to oral health and comfort. It signifies a critical turning point, acknowledging that the dental issues are complex and require a coordinated, multifaceted approach rather than a series of isolated repairs. The patients who embark on this journey are often those who have struggled with deteriorating dental health for years, experiencing escalating problems that have finally culminated in a state requiring this level of intervention to reclaim function and prevent further, potentially irreparable, damage.
Who Requires a Full Mouth Reconstruction?
The cohort of patients who require full mouth reconstruction is diverse, but they share a common thread: their dental issues are extensive, often interconnected, and significantly impairing their oral function and quality of life. Firstly, consider individuals whose teeth have been relentlessly ground down over years, often unconsciously, due to severe bruxism (clenching and grinding). This wear can be so profound that it shortens teeth dramatically, affects the bite, causes pain, and exposes the underlying, sensitive dentin. Then there are those who’ve suffered significant trauma – perhaps an accident, a fall, or a sports injury – resulting in multiple broken, fractured, or knocked-out teeth across different parts of the mouth. Another large group includes individuals with widespread, severe tooth decay, often stemming from years of neglect, poor diet, or medical conditions affecting oral health, leading to multiple cavities, infections, and tooth loss. Patients struggling with persistent jaw pain, muscle spasms, and chronic headaches directly linked to an improper bite (malocclusion) frequently find that correcting their bite through reconstruction is the only way to achieve lasting relief and prevent further damage to their teeth and jaw joints. Furthermore, individuals who have experienced severe acid erosion, whether from dietary habits (consuming large amounts of acidic drinks), medical conditions like GERD (Gastroesophageal Reflux Disease), or eating disorders, can suffer extensive loss of enamel, necessitating comprehensive rebuilding to protect the remaining tooth structure and restore function and appearance. These are not minor issues affecting one or two teeth; they are systemic problems requiring a holistic, extensive solution to restore the entire oral system to health and harmony.
When Is Dental Reconstruction Necessary?
Dental reconstruction becomes not just an option, but a necessity, when the integrity and function of multiple teeth and their supporting structures are severely compromised, and less comprehensive treatments are insufficient to resolve the issues. It’s necessary when the physical structure of the teeth is significantly degraded across the mouth, whether due to widespread cracks, fractures, or advanced wear, threatening their long-term viability. Crucially, it’s required when the way the upper and lower teeth meet (the occlusion) is fundamentally incorrect, leading to chronic pain in the jaw joints or muscles, causing further damage to teeth, or making proper chewing impossible. Widespread tooth loss, whether from decay, gum disease, or trauma, also often dictates the need for full mouth reconstruction, as simply replacing individual missing teeth isn’t enough when the overall bite has collapsed or the remaining teeth are under excessive strain. Furthermore, significant oral trauma affecting multiple teeth, the jawbone, or the jaw joints almost invariably necessitates a comprehensive reconstruction approach to restore both form and function. Essentially, reconstruction is deemed necessary when the collective dental problems create a cascade of negative effects, impacting not just the appearance of the smile but critically hindering essential functions like eating and speaking, and potentially causing chronic pain. It’s the intervention required when the complexity and scope of the damage exceed the capabilities of standard restorative procedures, demanding a strategic, integrated plan to salvage, restore, and rebuild the entire oral system for long-term health and stability, preventing a downward spiral of dental decline.
Who Are the Types of Patients that Can Experience Advantages from this Treatment?
Beyond the specific conditions necessitating full mouth reconstruction, certain types of patients are uniquely positioned to experience profound advantages from this transformative treatment. Chief among these are individuals suffering from chronic and debilitating jaw joint pain, medically termed Temporomandibular Joint Disorders (TMD) or TMJ disorders, that are directly linked to bite disharmony. Correcting the occlusion through reconstruction can alleviate pressure on the joints and muscles, leading to significant pain relief and improved jaw function. Another group includes individuals with congenital disorders or genetic conditions that have resulted in malformed teeth, missing teeth from birth, or other developmental abnormalities affecting oral structure. For these patients, reconstruction offers the opportunity to build a functional and aesthetic dentition they may never have had otherwise. Survivors of oral cancer who have undergone surgery and radiation, which can severely impact teeth, bone, and soft tissues, often require extensive restorative work to regain the ability to eat and speak comfortably; full mouth reconstruction provides the framework for this complex rehabilitation. Similarly, victims of significant accidents or trauma to the face and mouth, whose injuries have resulted in extensive damage to multiple teeth, supporting bone, and jaw structure, rely on reconstruction to rebuild their oral foundation and restore essential functions. Essentially, anyone facing widespread, complex dental challenges that compromise their quality of life, and for whom piecemeal treatments are insufficient, stands to gain tremendously from the holistic, strategic approach of full mouth reconstruction, moving from a state of chronic problems to one of stability, function, and comfort.
What Functional Challenges Lead to Reconstruction Needs?
The path to full mouth reconstruction is often paved with significant functional challenges that make everyday life increasingly difficult and uncomfortable. A primary driver is severe difficulty in properly chewing food. When multiple teeth are missing, damaged, or severely worn down, the ability to efficiently break down food is compromised. This can lead to digestive issues, nutritional deficiencies, and the forced adoption of soft-food diets, drastically limiting enjoyment and variety in eating. Another significant functional challenge is impaired speech. Missing teeth, particularly front teeth, or a severely misaligned bite can affect the way air flows over the tongue and teeth, leading to lisps or other speech impediments. Chronic pain is perhaps one of the most compelling functional reasons for reconstruction. Bite problems can cause constant strain on the jaw muscles and joints, resulting in persistent headaches, earaches, and pain in the face, neck, and shoulders. This chronic discomfort can be debilitating, impacting sleep, concentration, and overall well-being. Furthermore, a compromised oral structure increases the risk of further, accelerated dental deterioration. An unstable bite places excessive force on remaining teeth, leading to more cracks and fractures. Missing teeth allow adjacent teeth to drift, disrupting the entire arch. Untreated severe wear continues unabated, further destroying tooth structure. Reconstruction addresses these cascading functional failures head-on, aiming to re-establish proper chewing mechanics, improve speech clarity, eliminate pain, and create a stable environment that halts the cycle of deterioration, enabling patients to reclaim essential daily functions they may have lost or severely restricted.
Are Extensive Dental Issues a Reason for Reconstruction?
Without question, extensive dental issues are not merely *a* reason, but often the *primary* and most compelling indicator for full mouth reconstruction. This isn’t a procedure considered for minor cosmetic tweaks or the occasional cavity; it’s the designated pathway when the scale of problems transcends routine dental care. When a patient presents with a constellation of issues such as multiple missing teeth scattered throughout the mouth, widespread decay affecting a significant percentage of their remaining dentition, or severe, generalised wear across both arches (upper and lower), the dentist understands that a tooth-by-tooth approach will likely be insufficient and ultimately less successful in the long run. These extensive problems are rarely isolated; they often stem from underlying systemic issues like unchecked bruxism, acid erosion affecting the entire mouth, or a history of complex medical conditions and treatments. Addressing them requires a strategic, holistic plan that considers how restoring one tooth will impact the others, how the new restorations will interact when biting, and how to create a stable foundation for long-term success. Reconstruction is designed precisely for these scenarios – cases where the complexity and sheer number of problems necessitate a coordinated approach to rebuild the entire oral system from the ground up, rather than chasing individual issues as they arise. It’s the comprehensive solution for extensive damage, offering the opportunity to restore not just individual teeth, but the entire functional unit of the mouth, providing stability and health where previously there was widespread decline and dysfunction.
Do Complex Restorative Needs Indicate Reconstruction?
Absolutely. When a patient’s oral health status presents with complex restorative needs, it’s a clear signal that full mouth reconstruction is likely the appropriate, and often necessary, course of action. Complex restorative needs arise when the required treatments go far beyond simple fillings or even single crowns. They involve situations where multiple teeth need simultaneous intervention, often with overlapping issues like decay, fracture, and bite-related wear. For instance, a patient might need several root canals, followed by crowns on those teeth, alongside the replacement of missing teeth with bridges or implants, while also addressing underlying gum disease or needing minor bone grafting. Trying to tackle these issues with isolated, unrelated procedures would be inefficient, potentially compromise the outcome, and fail to address the fundamental problems affecting the entire bite and oral structure. Complex restorative needs demand a master plan – a sequence of treatments meticulously choreographed to ensure that each step builds upon the last, leading towards a harmonious and functional end result. This level of planning and coordination is the hallmark of full mouth reconstruction. It’s about integrating various restorative techniques – from foundational treatments like gum therapy and extractions to advanced procedures like implant placement and the fabrication of complex multi-unit prosthetics (crowns, bridges) – into a single, cohesive strategy. When the patient’s case involves multiple, interconnected problems requiring a variety of sophisticated interventions executed in a specific order, it undeniably points towards the need for the comprehensive, planned approach that defines full mouth reconstruction, moving beyond simple restoration to true oral rehabilitation.
How Does Teeth Reconstruction Work? What Procedures Are Included?
Embarking on teeth reconstruction is less like booking a standard dental appointment and more like commissioning a significant construction project. The process is anything but boilerplate; it’s a highly individualised journey, meticulously planned and executed in distinct phases. It doesn’t begin with picking up a drill, but with extensive investigation and strategic design. Imagine an architect and structural engineer assessing a building that has suffered significant damage – they wouldn’t start patching holes; they would first conduct a thorough survey to understand the extent of the damage, the structural integrity, and the underlying causes. Similarly, full mouth reconstruction starts with a deep dive into the patient’s oral health status. This involves a comprehensive clinical examination, including a detailed assessment of each tooth, the gums, supporting bone, jaw joints (TMJ), and chewing muscles. Advanced diagnostic records are crucial: a full series of X-rays (including panoramic and potentially 3D cone-beam CT scans), detailed photographs of the teeth and smile from various angles, and accurate impressions or digital scans to create precise models of the teeth and bite. These models are often mounted on an articulator, a device mimicking jaw movements, allowing the dentist to study the patient’s bite dynamics outside the mouth. This diagnostic phase is paramount; it’s where the blueprint for reconstruction is created, identifying the root causes of the problems and formulating a step-by-step plan outlining the necessary procedures and their sequence. The beauty and complexity lie in this tailored approach, recognising that no two mouths, no two sets of problems, are exactly alike, and thus, no two reconstruction plans will be identical, always starting with a thorough understanding before any physical work commences.
How does teeth reconstruction work?
The operational mechanics of teeth reconstruction unfold through a carefully orchestrated series of steps, transforming a state of disrepair into one of renewed function and aesthetics. Following the initial exhaustive diagnostic phase, where the ‘master plan’ is conceived, the actual work begins, typically addressing foundational issues first. This might involve treating any active gum disease (periodontal therapy) to create a healthy base for future restorations, performing necessary tooth extractions for irreparably damaged teeth, or carrying out root canal therapy on infected teeth that can be saved. If significant bone loss has occurred, often a consequence of long-standing tooth loss or gum disease, bone grafting procedures may be required to build up enough stable bone to support future implants or provide a better foundation for dentures or bridges. Only once these preparatory stages are complete and the mouth is healthy and stable are the primary restorative procedures initiated. This phase involves rebuilding the teeth and establishing the correct bite. Procedures might include preparing teeth for crowns or veneers, placing dental implants into the jawbone to replace missing tooth roots, or preparing teeth to support dental bridges. Temporary restorations are frequently placed during this phase to allow the patient to function while the permanent crowns, bridges, or dentures are being fabricated by skilled dental laboratories. These temporaries also serve as a “test drive” for the new bite and aesthetics, allowing for adjustments before the final restorations are made. The process is iterative, sometimes requiring adjustments and refinements as the reconstruction progresses, all guided by the initial comprehensive plan and the goal of achieving optimal function, comfort, and appearance.
What Procedures Are Included in a Full Mouth Reconstruction?
The array of procedures that can be included in a full mouth reconstruction is vast and tailored precisely to the individual patient’s unique needs and the complexities of their case. It’s rarely just one or two interventions; it’s typically a combination drawn from the extensive toolkit of restorative and surgical dentistry. Common procedures include the placement of dental crowns on teeth that are severely worn, broken, or decayed to restore their shape, strength, and appearance. Dental bridges are frequently used to replace one or more missing teeth by spanning the gap and attaching to the adjacent teeth (or implants). For replacing missing tooth roots and providing stable support for crowns, bridges, or dentures, dental implants are a cornerstone of modern reconstruction. Veneers, while often seen as purely cosmetic, can also play a role, particularly on front teeth, to restore aesthetics and protect surfaces after bite issues or wear have been corrected. Inlays and onlays are used to restore sections of back teeth that are too damaged for a filling but don’t require a full crown. For patients with extensive tooth loss, partial or complete dentures, sometimes anchored by implants for added stability (implant-supported dentures), may be necessary. Addressing underlying issues is critical, so gum disease treatment (scaling and root planing, or more advanced periodontal surgery) is often a prerequisite. Severely infected or damaged teeth may require root canal therapy or extraction. In very complex cases involving significant jaw misalignment or skeletal discrepancies, orthognathic surgery (jaw surgery) might be part of the treatment sequence, often performed in conjunction with orthodontics to reposition teeth and jaws before final restorations are placed. The specific mix of procedures creates the bespoke nature of each reconstruction.
What are the treatments involved in full mouth reconstruction?
Delving deeper into the specific treatments involved in a full mouth reconstruction reveals the intricate level of detail required to rebuild a compromised oral system. Beyond the broad categories, let’s look at the granular elements. A core component is often the placement of dental crowns. These are caps that cover the entire visible portion of a tooth above the gum line, custom-made from materials like porcelain, ceramic, zirconia, or gold alloys, designed to restore a tooth’s original shape, size, strength, and appearance, crucial for teeth that are severely worn, broken, or heavily filled. When teeth are missing, dental bridges, typically made of porcelain fused to metal or solid zirconia, are used to literally ‘bridge’ the gap, cemented onto adjacent teeth (abutments) or implants. Dental implants themselves involve a surgical procedure to place a titanium or zirconia post into the jawbone, which then fuses with the bone over several months; this stable post then serves as the root for a replacement tooth (a crown), or as an anchor for a bridge or denture, providing unmatched stability. For cases of advanced wear or minor damage on front teeth, dental veneers – thin, custom-made shells, usually of porcelain or composite resin, bonded to the front surface – can be employed to restore shape, size, and colour, often after the underlying bite issues have been corrected. Sometimes, the bite itself needs adjustment, which can involve orthodontics (braces or aligners) to move teeth into a better position or subtle reshaping of the tooth enamel (occlusal adjustment). The treatments are diverse, but the key is their coordination; they are not isolated acts, but carefully sequenced steps in a larger strategic plan aimed at restoring the entire oral complex to optimal health and function, selecting the right tool from the vast dental arsenal for each specific need within the overarching scheme.
What Treatments Does Dental Reconstruction Include?
Dental reconstruction fundamentally includes a comprehensive suite of treatments aimed at restoring the structural integrity, function, and aesthetics of the entire oral system. It’s a multi-disciplinary undertaking that goes beyond addressing individual dental problems in isolation. The scope typically encompasses foundational therapies such as periodontal treatment to ensure healthy gums, which are the necessary support system for any lasting restorations. It often involves endodontic procedures like root canals to save infected teeth or extractions for teeth that are beyond repair. Surgical interventions might be necessary, including bone grafting to augment deficient jawbone volume, sinus lifts, or ridge augmentation to prepare the mouth for dental implants or improve the fit of dentures. The core restorative work involves placing a variety of prosthetic devices: custom-fabricated dental crowns and bridges to restore or replace damaged and missing teeth, veneers to enhance aesthetics and protect tooth surfaces, inlays and onlays for specific types of tooth damage, and various types of dentures (conventional, partial, implant-supported) when extensive tooth loss has occurred. Correction of bite discrepancies is a critical element, potentially involving orthodontics to reposition teeth, or occlusal adjustments to reshape tooth surfaces and ensure proper alignment when biting. The range of treatments reflects the complexity of the problems addressed; reconstruction is not defined by a single procedure, but by the integration of multiple procedures – surgical, restorative, and occasionally orthodontic – into a cohesive plan designed to rehabilitate the entire mouth, ensuring that form and function are restored harmoniously, addressing every facet of the patient’s oral health challenge.
What are the Common Treatments that will Reconstruct Your Teeth?
While the full spectrum of potential procedures in dental reconstruction is vast, there are several workhorse treatments that form the backbone of many full mouth cases, addressing the most frequent issues of damage, wear, and tooth loss. Dental crowns are ubiquitous in reconstruction; they are essential for salvaging severely damaged teeth, providing strength and restoring shape when a tooth is heavily worn, fractured, or extensively filled. Think of them as the definitive cap that gives a compromised tooth a second life and proper function within the new bite. Dental bridges are another staple, offering a reliable way to replace missing teeth by using adjacent natural teeth or implants as anchors, effectively restoring the ability to chew and preventing surrounding teeth from shifting. Perhaps the most transformative common treatment, especially for replacing missing teeth, is the dental implant. These small titanium or zirconia posts surgically placed into the jawbone provide unparalleled stability and longevity, serving as artificial tooth roots upon which crowns, bridges, or dentures can be securely attached. While traditional dentures can also be part of a reconstruction, particularly in cases of extensive tooth loss where implants are not feasible for every missing tooth, implant-supported dentures represent a modern evolution, offering significantly improved stability and comfort compared to their conventional counterparts. Additionally, addressing gum health through scaling, root planing, or other periodontal therapies is a foundational, common first step, as healthy gums are essential for supporting any type of restoration. These common treatments, applied strategically and often in combination, are the core tools used by restorative dentists to rebuild the architecture and function of a severely compromised mouth, proving that extensive damage is frequently addressable with proven, effective techniques.
What Are the Types of Dental Reconstruction?
It’s important to clarify that when discussing “types” of dental reconstruction, we’re not referring to rigid, distinct categories like “Type A” or “Type B” with predefined procedure lists. Full mouth reconstruction is inherently bespoke, a treatment plan uniquely crafted for *each* individual based on their specific diagnosis. However, the concept of “types” can sometimes refer to the *primary focus* or the *extent* of the reconstruction needed. For example, one patient’s reconstruction might be primarily driven by severe tooth wear due to bruxism, requiring significant work to restore the vertical dimension of the bite and rebuild shortened teeth. Another patient’s case might be dominated by widespread tooth loss, necessitating extensive use of dental implants and implant-supported prosthetics. A third might need reconstruction primarily due to trauma that has fractured multiple teeth and damaged supporting bone. While the procedures might overlap across these scenarios (crowns, implants, etc.), the *strategy* and *sequence* will differ based on whether the main challenge is wear, loss, trauma, or a combination. Sometimes, “types” might loosely refer to the *degree* of the problem, implicitly suggesting a more or less complex case, although the term “full mouth” inherently suggests significant complexity across both arches. Ultimately, classifying reconstruction into fixed “types” is less useful than understanding that it is a spectrum of comprehensive treatments, each meticulously designed to address the specific constellation of issues present in a particular patient’s mouth, guided by the goal of restoring total oral health and function through a combination of various restorative and surgical techniques, making each reconstruction a unique and complex undertaking.
What Are the Benefits and Recovery of Full Mouth Reconstruction?
Undergoing full mouth reconstruction is a significant undertaking, demanding time, financial investment, and commitment. However, the benefits that accrue from successfully completing this process are profound and far-reaching, extending well beyond merely fixing teeth. It’s a transformative journey that impacts not just oral health but also overall well-being, confidence, and quality of life. The most immediate and often appreciated benefits relate directly to function: the restoration of proper chewing ability, allowing patients to eat a wider variety of foods comfortably and enjoy meals again, a simple pleasure many with damaged teeth take for granted. Pain relief is another major outcome, particularly for those suffering from chronic headaches and jaw pain linked to bite problems; correcting the occlusion can alleviate years of discomfort. By addressing underlying issues like decay and gum disease, reconstruction significantly improves overall oral health, preventing the cascade of problems that would otherwise continue unchecked. Beyond the functional and health benefits, the aesthetic improvements are often dramatic. Rebuilding damaged or missing teeth, correcting alignment, and restoring the natural shape and color of the dentition can lead to a stunning smile transformation, profoundly impacting self-esteem and confidence. The recovery process, while varying based on the procedures performed, is a manageable period leading to this renewed state. It requires patience and adherence to post-operative instructions, but it is the necessary bridge between the treatment phases and the full realisation of the benefits, culminating in a stable, healthy, functional, and aesthetically pleasing outcome that justifies the investment in time and effort, offering a new lease on oral life.
What Are the Benefits of Full Mouth Reconstruction?
The advantages harvested from a successful full mouth reconstruction are manifold, touching upon fundamental aspects of physical health, emotional well-being, and social interaction. Foremost is the dramatic restoration of masticatory function. For years, patients needing reconstruction might have avoided hard or chewy foods, limited their diet to soft options, and experienced pain or discomfort while eating. Reconstruction enables them to chew efficiently and comfortably, expanding dietary options and improving nutritional intake, a seemingly simple ability that profoundly impacts daily life and enjoyment. Chronic pain relief is another monumental benefit. Malocclusion, severe wear, and damaged teeth often cause persistent headaches, facial pain, and discomfort in the jaw joints and muscles. By correcting the bite and restoring the dental arches, this chronic pain is frequently eliminated or significantly reduced, offering a release from long-term suffering. Oral health is fundamentally improved; underlying issues like gum disease and decay are addressed, halting their progression and creating a stable environment for the remaining and rebuilt teeth. On the aesthetic front, the transformation can be breathtaking. Replacing missing teeth, restoring worn or damaged enamel, correcting proportions and alignment – these elements combine to create a harmonious, natural-looking smile that patients are eager to show off. This aesthetic enhancement directly fuels a surge in self-confidence and quality of life. Patients who previously hid their smiles or felt self-conscious are empowered to interact socially without reservation, laughing freely and speaking clearly. Ultimately, reconstruction is also a preventative measure, creating a stable, balanced bite that protects the remaining teeth and restorations from excessive forces, thus preventing future damage and the recurrence of the initial problems, offering a durable solution for long-term oral health stability.
What to Expect from Full Mouth Reconstruction and Recovery?
Setting expectations accurately is crucial when considering full mouth reconstruction, as it is a significant undertaking that demands patience and commitment over an extended period. Unlike a quick cosmetic procedure, the timeline for a full mouth reconstruction typically stretches over several months, and in complex cases, can even exceed a year or two, particularly if bone grafting, implant integration (which takes months to fuse with bone), or orthodontics are involved. The process unfolds in distinct phases, requiring multiple appointments. Initially, there will be diagnostic appointments, followed by foundational work (gum treatment, extractions, grafts), then surgical phases (implant placement), and finally, the restorative phase where temporary and then permanent prosthetics are fitted. During the treatment period, patients will often wear temporary crowns, bridges, or dentures. While these are functional, they may not be as aesthetically pleasing or as comfortable as the final restorations. Recovery varies depending on the specific procedures performed. Simple crown preparations have minimal recovery, perhaps some temporary sensitivity. Surgical procedures like extractions, bone grafting, or implant placement will involve a more significant recovery period, including potential swelling, bruising, and discomfort managed with prescribed or over-the-counter pain medication. Adhering strictly to post-operative instructions regarding diet (often soft foods initially), oral hygiene, and activity level is essential for proper healing. Follow-up appointments are critical to monitor healing, adjust temporaries, and ensure the treatment plan is progressing as intended. While it’s a marathon, not a sprint, the temporary inconvenience and recovery periods are steps towards a final outcome that is durable, functional, and aesthetically pleasing, representing a significant positive change from the initial state of compromise.
Can Embracing Full Mouth Reconstruction Lead to Renewed Smiles?
The connection between embracing full mouth reconstruction and achieving a truly renewed smile is not just a possibility; it’s one of the most compelling and life-changing outcomes of the process. While the primary drivers for reconstruction are typically functional and health-related, the aesthetic transformation is often profound and deeply impactful on a patient’s self-perception and interaction with the world. Imagine years of hiding a smile due to missing teeth, discoloured restorations, severely worn or chipped surfaces, or a bite that makes teeth look uneven and unattractive. Full mouth reconstruction directly addresses these issues. Missing teeth are replaced, restoring the continuity and fullness of the dental arches. Damaged or worn teeth are rebuilt with high-quality, natural-looking crowns or veneers, restoring their original shape, size, and colour – or even improving upon them. The bite correction often repositions teeth or aligns arches in a way that creates a more harmonious and balanced smile line. The materials used today for crowns, bridges, and veneers are remarkably lifelike, mimicking the translucency and subtle variations of natural enamel, making the rebuilt teeth virtually indistinguishable from healthy natural ones. The result is not just a repaired mouth, but a smile that feels and looks vibrant, healthy, and aesthetically pleasing. This visible transformation has a powerful psychological effect. Patients who were once self-conscious become confident; those who avoided social situations involving eating or close interaction feel liberated. A renewed smile is more than just cosmetic enhancement; it’s a symbol of restored health, function, and self-assurance, a tangible representation of the significant journey undertaken and the positive change achieved, allowing patients to face the world with a beaming, confident expression they might not have felt possible before.
How Much Does It Cost to Rebuild Teeth?
Addressing the financial aspect of rebuilding teeth through full mouth reconstruction is paramount, and it requires a candid acknowledgment upfront: this is a significant investment. Unlike routine dental care, which involves isolated procedures with relatively predictable costs, full mouth reconstruction is a complex, multi-step process involving numerous treatments, specialised materials, extensive laboratory work, and often, the involvement of multiple dental specialists. Consequently, there is no single, fixed price tag. The cost is highly variable and contingent upon a multitude of factors specific to each patient’s needs and the complexity of their case. These variables include the severity and extent of the dental problems (are we rebuilding severely worn teeth, replacing many missing teeth with implants, addressing complex bite issues?), the specific procedures required (does it involve bone grafting, multiple implants, root canals, extensive crown work?), the type and quality of materials used for the restorations (porcelain fused to metal, all-ceramic, zirconia, gold), the fees of the dental professionals involved (specialists often have higher fees than general dentists), the geographic location of the practice (costs can vary significantly between regions or cities), and the complexity of the laboratory work needed to fabricate the custom restorations. Because it’s a bespoke treatment plan, a detailed, accurate cost estimate can only be provided after a comprehensive examination and diagnosis. Any figure quoted without a thorough assessment is merely a rough ballpark, at best. Patients should expect to receive a detailed breakdown of the proposed treatment plan and associated costs during the consultation phase, allowing them to understand the investment required before committing to the process, recognising that this is a major financial undertaking commensurate with the complexity and transformative potential of the treatment.
How much does it cost to rebuild teeth?
Providing a single, definitive cost for rebuilding teeth via full mouth reconstruction is simply impossible, as the figure is highly dynamic and depends entirely on the unique blueprint drafted after a thorough diagnosis. However, to offer some context, it’s essential to understand that full mouth reconstruction is one of the most extensive and consequently, one of the most expensive procedures in dentistry. We are not talking about the cost of a filling or even a single crown. We are discussing the cumulative cost of potentially dozens of individual procedures, surgical interventions, diagnostic records, temporary restorations, extensive laboratory fees for custom-fabricated prosthetics, and numerous appointments spread over a long period. The final figure can range from tens of thousands of dollars to well over $100,000 or more in highly complex cases involving extensive grafting, multiple implants, and full-arch implant-supported bridges. The level of complexity is the primary driver of cost. A case involving moderate wear needing crowns on most teeth will cost significantly less than a case involving widespread tooth loss requiring bone grafting and full-arch implant-supported bridges in both the upper and lower jaws. The materials chosen also play a role; high-quality, aesthetically superior ceramic or zirconia restorations are typically more expensive than metal-based options. Location is another factor, with costs generally being higher in major metropolitan areas compared to smaller towns. Because of this significant financial variance and investment, obtaining a precise, written estimate after a comprehensive examination and detailed treatment planning is absolutely critical. Patients should feel comfortable discussing the estimated cost in detail with their dental provider and exploring all potential payment and financing options before proceeding with treatment.
How much does it cost to rebuild a tooth?
When considering the cost of rebuilding *a single tooth* within the context of a full mouth reconstruction, it’s important to understand that the calculation isn’t as straightforward as simply looking up the price of a single procedure. While individual procedure costs (like a crown, a filling, a veneer, or an implant-supported crown) exist, the cost within a comprehensive reconstruction is part of a larger, integrated plan. The expense of rebuilding a single tooth might involve just the cost of the crown itself, but it could also encompass the cost of the necessary root canal therapy *before* the crown, the cost of the post and core needed to build up the tooth structure *before* the crown preparation, or even the cost of a gum graft if the tooth has recession affecting the restoration’s margin. If the tooth is missing and being replaced by an implant, the cost involves the implant surgery itself, the abutment (connector), and the final crown that goes on top – three distinct components and procedures contributing to the cost of replacing *one* tooth. Furthermore, the lab fee for fabricating a single crown might be higher in a reconstruction case because it needs to be meticulously crafted to fit perfectly within the new, corrected bite scheme of the entire mouth, potentially involving more complex design and communication between the dentist and the lab technician. So, while you *could* ask for the estimated cost of crowning one specific tooth within the plan, the true financial picture emerges only when looking at the total, integrated cost of the entire reconstruction, as the procedures on individual teeth are designed to work in harmony as part of a larger system, making the per-tooth cost less relevant than the overall investment required for the full oral rehabilitation.
What Is the Cost of Full Mouth Reconstruction?
The cost of full mouth reconstruction is the cumulative financial outlay for the entire, multi-phase process of rebuilding and restoring the upper and lower dental arches to optimal function and aesthetics. It is not merely the sum of individual tooth procedures; it encompasses the cost of the extensive diagnostic workup (X-rays, scans, models, bite analysis), the detailed treatment planning process (which can involve hours of the dentist’s and potentially specialists’ time), any necessary preparatory treatments like gum therapy, extractions, or bone grafting, the surgical phases (especially if implants are used), the fabrication of all temporary restorations used throughout the process, the laboratory fees for creating the final, custom-made crowns, bridges, veneers, and dentures (which are significant), the fees for placing all the permanent restorations, and the numerous follow-up appointments required to ensure proper fit and function and monitor healing. Because this process is so comprehensive and variable, providing a fixed figure is impossible without a specific treatment plan. However, patients should prepare for an investment that typically ranges from $20,000 to upwards of $100,000 or more. This wide range reflects the vast difference in complexity between cases. A patient needing crowns on perhaps 10-12 significantly worn teeth might fall lower on the scale than someone requiring extensive bone grafting and 8-12 dental implants supporting full-arch bridges in both jaws. The value lies not just in the materials or procedures but in the expert diagnosis, meticulous planning, and skilled execution required to achieve a functional, comfortable, and long-lasting result that dramatically improves quality of life.
How can I pay for full mouth rehab?
Navigating the financial landscape of full mouth rehabilitation, given its significant cost, requires exploring multiple payment options and strategies. Few people have the liquid funds readily available, so understanding the avenues for financing is crucial. Dental insurance often provides some level of coverage, but it’s essential to be realistic. Most dental insurance plans have annual maximums, often ranging from $1,000 to $2,500 per year, which are quickly exhausted by the cost of complex reconstruction. However, insurance *can* help offset the cost of certain procedures deemed medically necessary, such as extractions, root canals, gum therapy, and sometimes even a portion of crowns or bridges, depending on the specific plan and how the need is documented. Patients should work closely with the dental office’s administrative or treatment coordinator to verify their specific coverage and how it might apply. Beyond insurance, several financing options exist. Many dental practices offer in-house payment plans, allowing patients to pay in installments. Third-party medical and dental financing companies (like CareCredit or Lending Club) specialise in healthcare loans, often offering interest-free periods or extended payment plans based on creditworthiness. Dental savings plans are another option; these are membership programs where participants pay an annual fee and receive discounted rates on dental services from participating providers – they are not insurance but can significantly reduce costs. Finally, some patients may opt for traditional personal loans or even consider phasing their treatment over several years to utilise successive years’ insurance maximums or save up funds, although phasing should always be discussed with the dentist to ensure it doesn’t compromise the overall treatment outcome or stability. Open communication with the dental office about financial concerns and options is paramount to making the process manageable.
Is full mouth rehab covered by insurance?
Whether full mouth rehabilitation is covered by insurance is a nuanced question, and the answer is generally: partially, and it depends heavily on the specific insurance plan and the justification for the treatment. Unlike straightforward procedures, reconstruction often blurs the lines between medical necessity and cosmetic enhancement. Insurance companies typically provide coverage for procedures deemed “medically necessary” to restore basic function and health, such as treating decay, gum disease, infections, and replacing missing teeth for functional reasons. This means components of a full mouth reconstruction like extractions, root canals, gum treatments, bone grafting, and potentially a portion of the cost for crowns, bridges, or dentures might receive *some* insurance coverage. However, procedures considered primarily cosmetic, such as veneers solely for aesthetic reasons or certain types of restorations chosen specifically for their superior appearance over functional need, may not be covered at all. The significant challenge with full mouth reconstruction is its comprehensive nature and high cost. Most standard dental insurance plans have relatively low annual maximum benefits (often $1,000-$2,500). The total cost of a full mouth reconstruction almost always far exceeds this annual maximum. While you can sometimes coordinate benefits between spouses’ plans or utilise two years’ maximums by phasing treatment, insurance coverage will typically only cover a fraction, perhaps 10-20% or in some cases slightly more, of the total cost. Patients should absolutely submit a pre-treatment estimate to their insurance company before beginning, based on the dentist’s detailed treatment plan. This will provide clarity on exactly what the plan *might* cover and the remaining out-of-pocket expense, managing expectations about the extent of insurance support for such a large-scale restorative project.
How Long Does Teeth Reconstruction Take and Last?
Understanding the timeline for both the process of teeth reconstruction and the expected lifespan of the restorations is vital for managing expectations and planning. These are two distinct concepts: the duration of the *treatment itself* versus the *longevity* of the finished product. The treatment phase is a journey, not a quick fix. It’s a multi-stage process requiring significant time commitment spread over many months or even years, depending on the complexity of the individual case, the specific procedures involved (especially those requiring healing time like surgery), and the patient’s scheduling flexibility. This isn’t about rushing; it’s about allowing adequate time for healing, for meticulous work to be performed, for custom restorations to be fabricated in the lab, and for the patient to adapt to changes in their bite. Conversely, the longevity of the reconstruction refers to how long the final crowns, bridges, implants, and other restorations are expected to function and look good before needing repair or replacement. This isn’t a lifetime guarantee without maintenance, but with proper care, these restorations are designed for significant durability. Managing expectations around both the duration of the treatment and the need for ongoing maintenance to ensure the longevity of the investment is a key part of the consultation process, ensuring patients understand that this is a long-term commitment yielding long-term benefits, but requiring patience during the process and diligence afterward.
How long does teeth reconstruction last?
The question of how long teeth reconstruction *lasts* pivots not on the duration of the treatment itself, but on the lifespan of the materials and procedures used in the final restorations. It’s critical to understand that full mouth reconstruction, while durable and designed for longevity, is not necessarily a “forever” solution in the sense that no part of it will ever need attention again. However, with diligent home care, regular maintenance appointments with your dentist, and avoidance of habits that can damage dental work (like chewing ice or using teeth as tools), the components of a reconstruction can provide many years, often decades, of reliable function and aesthetics. For instance, high-quality dental crowns and bridges, common components of reconstruction, are typically expected to last between 10 to 15 years, or even longer, depending on the material, the forces placed upon them, and the patient’s oral hygiene. Dental implants, which replace tooth roots, have a remarkably high success rate and, with proper care, can potentially last a lifetime. The crowns or prosthetics attached to implants may need periodic replacement, but the implant post itself is designed to be permanent. Veneers might last 7-15 years. Dentures, whether traditional or implant-supported, may require relining, rebasing, or eventual replacement as the underlying bone and tissue change over time, although implant-supported dentures offer much greater long-term stability. The ultimate longevity is a function of several factors: the quality of the materials and lab work, the precision of the planning and execution, the patient’s oral hygiene habits, their diet, whether they use a nightguard if they grind their teeth, and attendance at regular dental check-ups for professional cleaning and assessment. It’s a long-term investment requiring ongoing vigilance for maximum return.
How long does a tooth reconstruction take?
The query “How long does a tooth reconstruction take?” carries a potential ambiguity: does it refer to the time spent working on *one* specific tooth within the larger full mouth plan, or the duration of the *entire process* involving that tooth’s role in the reconstruction? If focusing on a single tooth *procedure* within the grand scheme, the duration varies widely. Placing a filling might take minutes. Preparing a tooth for a crown typically takes 1-2 hours. A root canal can take 1-2 hours or more, sometimes requiring multiple visits. Surgically placing a single dental implant takes perhaps 1-2 hours, but the tooth reconstruction on that implant (placing the abutment and crown) occurs months later after healing. However, within the context of a full mouth reconstruction, focusing on the time spent on an individual tooth during one appointment misses the larger picture. That single tooth appointment is merely one step in a complex, carefully sequenced process. The overall time it takes for a *specific tooth* to be fully reconstructed, from initial diagnosis to the placement of its final restoration, depends entirely on its condition and the procedures needed for it and the surrounding teeth, all within the flow of the larger plan. A tooth needing a root canal and crown might take several weeks or months from start to finish if other procedures are happening simultaneously or need to precede it. A tooth being replaced by an implant takes several months for healing before the crown is placed. So, while the chair time for work on one tooth might be relatively short, the total time that tooth is *involved* in the overall reconstruction journey can be extensive, dictated by the pace and phases of the comprehensive treatment plan for the entire mouth.
How long will a full mouth reconstruction take?
The total duration of a full mouth reconstruction is a significant commitment of time, typically ranging from several months to upwards of two years, and in some very complex cases requiring orthodontics or multiple surgical stages, it could potentially extend even longer. This is not a procedure completed in a single appointment or even a few weeks; it’s a phased process designed for optimal results and healing. The exact timeline is dictated by the complexity of the patient’s case, the number and type of procedures required, and the necessary healing time between stages. For instance, cases requiring significant bone grafting or dental implants need several months of healing after surgery before the next phase of placing restorations can begin, allowing the bone to integrate properly with the graft material or the implant posts. If orthodontics are needed to reposition teeth before the final restorations, this phase alone can take a year or more. Even without major surgery, the process of preparing multiple teeth, taking impressions, fabricating custom restorations in the dental lab, fitting temporaries, and then finally fitting and adjusting the permanent crowns, bridges, or dentures across both arches involves numerous appointments spaced out over time. The scheduling availability of the patient and the dental team can also influence the pace. While it requires patience, this extended timeline allows for meticulous planning, precise execution, adequate healing, and the opportunity for adjustments along the way, ensuring the final result is stable, comfortable, and aesthetically pleasing. It’s a long-term investment of time and effort, but one with the potential for life-changing outcomes.
Does Tooth Reconstruction Hurt?
It’s a common, and entirely understandable, concern when facing extensive dental work: will it be painful? The short answer regarding pain *during* tooth reconstruction procedures is generally no, thanks to the effective use of local anesthesia and sedation options. Modern pain management techniques in dentistry are highly advanced, ensuring that the areas being worked on are completely numb. Patients may feel pressure or vibration, but sharp pain during the procedure itself is not expected. However, it’s equally important to address the discomfort and soreness that *can* occur *after* procedures, particularly surgical ones or those involving extensive preparation. Recovery from certain stages of full mouth reconstruction, such as tooth extractions, bone grafting, or implant placement, will involve post-operative discomfort, swelling, and bruising, much like recovery from any minor surgery. The level of discomfort varies depending on the invasiveness of the procedure and the individual’s pain tolerance. Dentists manage this post-operative pain effectively through prescription pain medication, antibiotics (to prevent infection), and anti-inflammatory drugs. Even non-surgical procedures involving significant tooth preparation for multiple crowns might result in temporary sensitivity or soreness of the gums. Patients are provided with detailed post-operative instructions on how to manage discomfort, including recommendations for pain medication, diet modifications (initially soft foods), and oral hygiene during the healing phase. While the *process* of reconstruction isn’t entirely without periods of recovery and manageable discomfort, especially after surgical interventions, the actual procedures are performed with measures in place to prevent pain, making the journey as comfortable as possible for the patient, ensuring that the fear of pain doesn’t become a barrier to achieving a healthy, functional mouth.
What Materials, Alternatives, and Additional Procedures Are Used in Full Mouth Reconstruction?
Full mouth reconstruction is a multifaceted undertaking that draws upon a wide range of materials and can incorporate various additional procedures beyond the most common restorative steps. The success and longevity of the reconstruction are heavily dependent on the quality and appropriateness of the materials chosen for the final restorations. Dentists select materials based on factors like strength requirements (e.g., using stronger materials for back teeth that bear heavy chewing forces), aesthetic considerations (e.g., using highly translucent materials for front teeth), potential for allergic reactions, and cost. Furthermore, the complexity of reconstruction often necessitates addressing underlying issues or incorporating adjunctive procedures that aren’t strictly restorative but are critical for creating a stable foundation for the final work. These might include periodontal surgery to address gum recession or disease, orthodontic treatment to realign teeth, or surgical procedures like bone grafting, sinus lifts, or ridge augmentation to prepare the jawbone for implants or other prosthetics. While full reconstruction is often the ideal solution for widespread damage, it’s also relevant to briefly touch upon potential alternatives, acknowledging that not every patient is a candidate for or desires such an extensive undertaking, although comprehensive rehabilitation of this nature is typically recommended when the problems are severe and widespread. Understanding the palette of materials and the scope of potential complementary procedures reveals the depth of planning and execution required for successful full mouth reconstruction, showcasing the blend of engineering, biology, and artistry involved in rebuilding a smile and bite from the ground up, utilising the best tools available in modern dentistry to achieve durable, functional, and aesthetic results tailored to the specific needs of the individual patient, ensuring that every aspect of the oral system is considered and addressed within the comprehensive plan.
What materials are used for full mouth reconstruction?
The selection of materials for full mouth reconstruction is a critical aspect of treatment planning, influencing the durability, aesthetics, and cost of the final restorations. Modern dentistry offers a sophisticated palette of materials, each with specific properties making them suitable for different applications within the mouth. For crowns, bridges, inlays, and onlays, common choices include porcelain fused to metal (PFM), which offers strength from the metal substructure and aesthetics from the porcelain overlay, although the metal can sometimes show as a grey line at the gumline. All-ceramic materials like lithium disilicate (e.g., E.max) offer excellent aesthetics, mimicking the translucency of natural enamel, and good strength, making them popular for front teeth and certain back teeth. Zirconia is another increasingly popular material, renowned for its exceptional strength and durability, making it ideal for back teeth, long dental bridges, and frameworks for implant-supported prosthetics, while newer generations of translucent zirconia also offer improved aesthetics. Gold alloys remain an option, particularly for back teeth, prized for their durability, biocompatibility, and gentle wear on opposing teeth, although less commonly chosen for aesthetic reasons. For veneers, porcelain is the standard, offering superior aesthetics and stain resistance compared to composite resin, which is sometimes used for direct bonding or less durable veneers. Dental implants are typically made from titanium, a biocompatible metal that integrates well with bone, or increasingly, zirconia, an aesthetic alternative that also integrates with bone. Dentures can be made from acrylic resin, sometimes reinforced with metal frameworks for partial dentures, with prosthetic teeth made of acrylic or porcelain. The choice of material is a careful decision made by the dentist, considering the specific location of the restoration in the mouth, the forces it will endure, the patient’s aesthetic goals, budget, and any potential material sensitivities, ensuring the chosen materials contribute to the longevity and success of the overall reconstruction.
When Are Dental Implants Used for Restoration?
Dental implants represent a cornerstone of modern restorative dentistry, revolutionising the approach to replacing missing teeth and playing a pivotal role in many full mouth reconstructions, particularly when tooth loss is a significant component of the patient’s issues. Implants are essentially artificial tooth roots, typically made of biocompatible titanium or zirconia, surgically placed into the jawbone. They are used for restoration when there are missing teeth, as they provide a stable, independent anchor for replacement teeth, unlike bridges which rely on adjacent natural teeth for support or traditional dentures which rest on the gums. In the context of full mouth reconstruction, implants are invaluable for several reasons: they prevent bone loss in the jaw, which naturally occurs after tooth extraction and can compromise the stability of other restorations; they offer superior stability and chewing power compared to traditional dentures or bridges that are not implant-supported; and they do not require modifying adjacent healthy teeth, as bridges do. Implants can support individual crowns to replace single missing teeth, serve as anchors for multi-unit bridges when several teeth in a row are missing, or provide crucial support and retention for implant-supported dentures or full-arch fixed prosthetics (like All-on-4 or similar techniques) in cases of complete tooth loss in an arch. Their use is indicated when the patient has sufficient bone volume (or undergoes grafting to create it) and good general health suitable for minor surgery. While they are an investment, their long-term success rates and ability to restore near-natural function make them the preferred method for tooth replacement in many reconstruction scenarios, offering a robust and durable foundation for the final dental work and contributing significantly to the overall stability and longevity of the rehabilitated bite.
Can Full Mouth Rehab Be Done With Dentures?
Yes, absolutely, full mouth rehabilitation can certainly be accomplished using dentures, particularly in cases of significant or complete tooth loss where other options like extensive bridging or numerous implants may not be feasible or desired by the patient. While modern dentistry often leans towards fixed solutions like implants and crowns, dentures remain a viable and important part of the restorative toolkit, focused on restoring function, phonetics, and aesthetics to the greatest extent possible. In scenarios where all teeth in an arch are missing, a complete denture replaces the entire arch. If only some teeth are missing, a partial denture can be used, which attaches to the remaining natural teeth or implants. Traditional dentures, both complete and partial, are removable and rest on the gum tissues. While they restore appearance and some chewing function, they can sometimes be less stable, especially lower complete dentures, and may require adhesives. However, within a full mouth rehabilitation plan, even traditional dentures are designed with careful consideration of the bite relationship with the opposing arch (whether that arch has natural teeth, crowns, or another denture) to ensure the best possible function and comfort. A significant advancement that integrates dentures into more stable rehabilitation is the use of dental implants to support or retain the dentures. Implant-supported dentures snap onto a few strategically placed implants, offering vastly improved stability, retention, and chewing efficiency compared to traditional dentures. They still typically remain removable for cleaning, but provide a level of confidence and function much closer to natural teeth. Thus, dentures, especially when combined with implant support, can be a very effective method for achieving full mouth rehabilitation, providing a functional and aesthetic solution for patients with extensive tooth loss, aligning with the core goals of restoring oral health and quality of life, proving that rehabilitation isn’t limited to fixed restorations.
When is Jawbone Grafting Required in Reconstruction?
Jawbone grafting is a frequently necessary adjunctive procedure in full mouth reconstruction, particularly in cases involving tooth loss or advanced gum disease, because a sufficient volume and density of healthy jawbone are critical prerequisites for many restorative treatments, especially dental implants. When a tooth is lost and not immediately replaced, the jawbone that previously supported it naturally begins to resorb, or shrink, over time because it is no longer receiving the stimulation from chewing forces transmitted through the tooth root. Advanced periodontal (gum) disease https://dentale-albania.com/general-dentistry/gum-disease-treatment/ also causes destruction of the bone supporting the teeth. If a patient needing reconstruction has areas where teeth have been missing for a while, or has suffered significant bone loss due to disease or trauma, there might not be enough bone height, width, or density to securely place dental implants, which require stable bone for osseointegration (fusion with bone). Insufficient bone can also compromise the support for bridges or the fit and stability of dentures. In these situations, jawbone grafting is required to rebuild the deficient bone. This involves surgically placing bone grafting material (which can be sourced from the patient’s own body, a donor, animal sources, or synthetic materials) into the area of bone deficiency. The graft material acts as a scaffold, stimulating the body to grow new bone tissue. This process takes several months to heal and for the new bone to mature sufficiently to support implants or other restorations. Therefore, bone grafting is a crucial step in reconstruction when the existing bone structure is inadequate, creating the necessary stable foundation for successful and long-lasting restorative work, ensuring that the planned rebuild has a solid structural base.
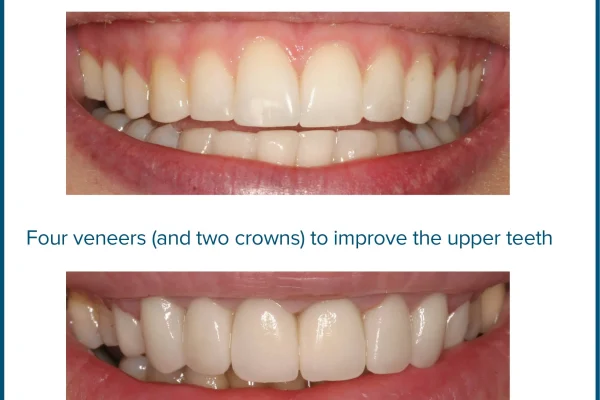
Can Veneers Be Used in Full Mouth Reconstruction?
Yes, veneers can be a valuable component in full mouth reconstruction, though they are typically used strategically and often in the later phases, primarily to enhance the aesthetics of the front teeth *after* the underlying functional and structural issues have been addressed. Unlike a simple “smile makeover” where veneers might be applied to otherwise healthy teeth purely for cosmetic reasons like changing colour or minor shape adjustments, in a full mouth reconstruction, veneers are usually incorporated as part of the overall plan to restore harmony and aesthetics to the anterior (front) teeth once the bite has been corrected, missing teeth replaced, and severely damaged teeth restored with crowns or other means. For instance, if the reconstruction involved correcting severe wear that shortened all the teeth, crowns might be used on the back teeth for strength, while veneers could be placed on the front teeth after the bite height has been re-established. This allows for a highly aesthetic result on the visible front teeth, while using stronger, full-coverage restorations (crowns) on the posterior teeth where chewing forces are higher. Veneers can also be used to protect the front surfaces of teeth that have been weakened by acid erosion, after the bite relationship has been corrected and any necessary restorative work on back teeth is complete. It’s crucial to understand that veneers alone are insufficient for a full mouth *reconstruction* if significant functional issues like bite collapse, severe wear across multiple teeth, or widespread missing teeth are present. They serve as a finishing touch or a targeted solution for specific aesthetic or protective needs on the front teeth *within* the larger, function-first framework of a comprehensive reconstruction plan, playing an important role in achieving the final aesthetic outcome after the foundational work is complete.
How Is Full Mouth Reconstruction Planned and Maintained?
Full mouth reconstruction is less a spontaneous event and more a meticulously planned campaign. Its success hinges on a detailed, strategic blueprint developed well before the first restorative procedure takes takes place. This planning phase is arguably the most critical part of the entire process, laying the groundwork for predictable outcomes and ensuring all aspects of the patient’s oral health and functional needs are addressed in the correct sequence. It involves a deep dive into diagnostics, collaborative consultation between the dental team and the patient, and careful consideration of every step required to move from the current compromised state to a stable, functional, and aesthetic result. But the journey doesn’t end when the final restoration is cemented into place. Maintaining the results of a full mouth reconstruction is just as crucial as the planning and execution phases. This extensive investment in oral health requires ongoing care and vigilance to ensure the longevity of the restorations and prevent the recurrence of the problems that necessitated the reconstruction in the first place. It’s a commitment to lifelong maintenance, understanding that even the most durable materials and expertly placed restorations require regular check-ups, professional cleanings, and diligent home care to stand the test of time and continue providing the intended functional and aesthetic benefits. Planning creates the outcome; maintenance preserves it, making both integral parts of the reconstruction narrative.
How Do We Plan Full Mouth Reconstruction?
The planning phase of full mouth reconstruction is a sophisticated process that involves gathering comprehensive information and using it to develop a detailed, sequential treatment strategy. It begins with the thorough diagnostic assessment mentioned earlier, including detailed clinical examination, full-mouth X-rays (sometimes including cone-beam CT scans for 3D imaging), high-quality intraoral and extraoral photographs, and accurate impressions or digital scans of the teeth to create models of the patient’s arches. These models are typically mounted on an articulator to simulate the patient’s jaw movements and analyse their bite (occlusion) in detail, identifying discrepancies and determining the optimal functional position for the new bite. This bite analysis is critical, as restoring a stable, balanced bite is a primary goal of reconstruction. The dentist will then meticulously evaluate all the gathered information – the health of each tooth, the condition of the gums and bone, the state of the jaw joints, the patient’s aesthetic concerns, and their functional limitations. Based on this comprehensive analysis, a proposed treatment plan is formulated. This plan outlines the necessary procedures, the recommended sequence (e.g., treating gum disease first, then extractions, then grafting, then implants, then temporaries, then final crowns), the timeline, and the estimated costs. Often, wax models (“wax-ups”) or digital mock-ups are created based on the treatment plan, allowing the dentist and patient to visualise the planned changes to the teeth and bite and predict the aesthetic outcome before any work begins in the mouth. This detailed planning phase often involves collaboration between a general dentist, prosthodontist, and potentially other specialists, ensuring a cohesive and effective approach to the complex case. Patient involvement in understanding and approving the plan is paramount, as they are integral partners in this extensive process.
What to expect during a full mouth reconstruction?
Embarking on a full mouth reconstruction is a journey that unfolds over time and involves a series of distinct phases and numerous appointments, rather than a single, swift intervention. Patients should expect the process to be lengthy, typically spanning from several months to a year or more, depending on the complexity and the need for healing periods between procedures. The initial phase involves extensive diagnostics and planning appointments. Following this, treatment proceeds in stages, often starting with addressing underlying issues like gum disease, tooth decay, or infections through periodontal therapy, fillings, root canals, or extractions. If surgical procedures like bone grafting or dental implant placement are necessary, these will constitute separate phases, each requiring several months of healing time before restorative work can continue. Throughout the process, particularly during the restorative phases, patients will likely wear temporary restorations (crowns, bridges, or dentures). These temporaries are crucial for allowing the patient to function, protecting prepared teeth, and serving as a blueprint or “test drive” for the final bite and aesthetics, allowing the dentist to make adjustments before the permanent restorations are fabricated. Expect multiple appointments for tooth preparation, taking impressions or scans for temporary and permanent restorations, fitting temporaries, trying in permanent restorations, and finally, cementing them in place. Some appointments, especially surgical ones, might be longer, while others for adjustments or impressions could be shorter. Communication with the dental team is key; ask questions, understand the purpose of each appointment, and report any discomfort or issues with temporaries promptly. While it’s a significant commitment of time and involves periods of healing and adjustment, knowing what to expect helps manage the process and focus on the ultimate goal of a healthy, functional, and beautiful smile.
What Are the Various Phases Involved in Full Mouth Reconstruction?
Breaking down full mouth reconstruction into its constituent phases helps illuminate the structured and logical progression of the treatment process. While the specific steps can vary slightly based on the patient’s unique needs, a typical full mouth reconstruction often follows a sequence like this: Phase 1: Diagnosis and Planning. This initial phase is all about gathering information through comprehensive examination, X-rays, scans, models, and bite analysis. Based on this data, the detailed, multi-step treatment plan is developed, often including discussions with specialists and the patient. Phase 2: Addressing Foundational Issues. This phase focuses on creating a healthy base for the restorative work. It includes treating any active gum disease, performing necessary tooth extractions, completing root canal therapy on savable teeth, and undertaking surgical procedures like bone grafting or sinus lifts if needed. This phase can be lengthy, requiring sufficient healing time after surgical interventions. Phase 3: Restorative Procedures (Preparation & Temporary). Once the foundation is healthy and stable, the restorative work begins. This involves preparing the teeth for crowns or veneers, surgically placing dental implants (if not done in Phase 2), taking impressions or digital scans, and fitting high-quality temporary restorations across the arches. These temporaries are crucial for function and aesthetics while the permanent restorations are being custom fabricated by a dental laboratory, and they allow the dentist and patient to evaluate and refine the planned bite and appearance. Phase 4: Placement of Permanent Restorations. This is where the final crowns, bridges, veneers, or dentures are fitted, adjusted for perfect bite and comfort, and permanently cemented or attached. This phase often involves multiple appointments to ensure precise fit and aesthetics across the entire mouth. Phase 5: Maintenance and Follow-up. The treatment is complete, but the care continues. This phase involves regular recall appointments for professional cleanings, check-ups, and monitoring the long-term health of the restorations and remaining natural tissues. This structured, phased approach ensures that each step builds correctly upon the last, leading to a stable and successful final outcome.
How is a full mouth reconstruction maintained?
Maintaining the results of a full mouth reconstruction is absolutely critical to ensuring the longevity of the significant investment made and preventing future problems. Reconstruction is not a one-time fix that negates the need for ongoing dental care; rather, it creates a restored structure that requires diligent maintenance. The cornerstone of maintenance is rigorous oral hygiene at home. This means brushing at least twice a day, paying careful attention to cleaning around crowns, bridges, and implants, and daily flossing or using interdental brushes to clean between teeth and under bridge work. Patients might be instructed on specific cleaning techniques or tools tailored to their new restorations. Regular professional dental check-ups and cleanings are equally essential. These appointments, typically scheduled every three to six months depending on the individual’s needs, allow the dental hygienist to thoroughly clean areas that are difficult to reach at home and enable the dentist to meticulously examine the condition of all the restorations, the health of the gums and bone, and the stability of the bite. Early detection of any potential issues with the restorations (like chipping or wear) or underlying tissues (like gum recession or inflammation around implants) allows for timely intervention, preventing minor problems from escalating into major ones. For patients with a history of bruxism (teeth grinding), wearing a custom-fitted nightguard is often a vital part of maintenance to protect the new restorations from excessive forces. Finally, avoiding habits like chewing on hard objects (ice, pens, fingernails), using teeth to open packages, or consuming excessive amounts of staining or acidic foods and drinks will also contribute significantly to the lifespan and appearance of the reconstruction. Maintenance is an active partnership between the patient and the dental team, crucial for preserving the restored function and aesthetics for years to come.
Where Can You Find Full Mouth Reconstruction Services?
Locating a qualified dental professional or clinic capable of performing comprehensive full mouth reconstruction requires seeking out practitioners with specific expertise and experience in complex restorative cases. This isn’t typically the domain of every general dental practice. While a general dentist with extensive continuing education in restorative dentistry might perform moderately complex reconstructions, the most challenging cases often necessitate the skills of a specialist. Prosthodontists are the gold standard specialists in this field; they are dentists who have completed an additional three years of advanced training specifically in the restoration and replacement of teeth and the comprehensive management of complex oral health issues. Their expertise in occlusion, materials science, and treatment planning for extensive reconstruction is unparalleled. Therefore, searching for a board-certified prosthodontist or a practice with a prosthodontist on staff is an excellent starting point. Additionally, some larger multi-specialty dental clinics or dental centres associated with university dental schools often have teams of specialists (including prosthodontists, oral surgeons, and periodontists) who collaborate on complex full mouth reconstruction cases, offering a coordinated approach under one roof. When researching potential providers, look for dentists or practices that explicitly list “full mouth reconstruction,” “full mouth restoration,” “complex restorative dentistry,” or “prosthodontics” among their services. Reviewing before-and-after photos of similar cases in their portfolio can also provide insight into their capabilities. Ultimately, finding the right provider begins with acknowledging the complexity of the treatment and seeking out professionals who have demonstrated the specific training, experience, and collaborative capabilities required for successful comprehensive oral rehabilitation.
Can You Find Full Mouth Reconstruction at PureSmile?
Regarding finding full mouth reconstruction services at a specific provider like PureSmile, the availability depends entirely on the range of services offered by that particular clinic or dental group and the expertise of their dentists. Many larger, multi-location dental groups like PureSmile aim to provide a comprehensive suite of services to cater to a wide range of patient needs. It is quite possible that a dental group of this size and scope employs dentists with advanced training in restorative dentistry or has prosthodontists on staff who are qualified to perform full mouth reconstruction. However, it is not a guarantee. Full mouth reconstruction requires specific diagnostic tools, treatment planning protocols, laboratory relationships for complex prosthetics, and clinical skills that go beyond basic general dentistry. Therefore, the definitive answer lies in directly contacting the PureSmile clinic you are interested in visiting. You should inquire specifically about their full mouth reconstruction or full mouth restoration services, ask about the qualifications and experience of the dentists who perform these procedures, and request a consultation to have your specific needs evaluated. Looking at their website’s list of services and dentist biographies might also provide clues regarding their capabilities in complex restorative dentistry. Assuming they are a reputable, larger practice, there is a good chance they can either provide the service or refer you to a qualified specialist within their network or community, as comprehensive care is often a goal of larger dental organisations.
Do American College of Prosthodontists Members Provide Full Mouth Reconstruction?
Yes, unequivocally, members of the American College of Prosthodontists (ACP) are precisely the specialists who are specifically trained and highly qualified to provide full mouth reconstruction. Prosthodontics is one of the nine dental specialties recognized by the American Dental Association, and it focuses on the diagnosis, treatment planning, rehabilitation, and maintenance of the oral function, comfort, appearance, and health of patients with clinical conditions associated with missing or deficient teeth and/or oral and maxillofacial tissues. Completing the requirements for becoming a prosthodontist involves three additional years of rigorous post-dental school training in an accredited program, focusing heavily on complex restorative dentistry, dental implants, dentures, and managing bite problems. Full mouth reconstruction is considered a core competency and a significant part of a prosthodontist’s practice. They are specifically trained to handle the most complex cases of tooth wear, trauma, genetic defects, and widespread tooth loss requiring integrated treatment plans involving multiple procedures and specialists. Their expertise lies in comprehensively planning and overseeing the entire reconstruction process, often acting as the lead clinician who coordinates care with other specialists like oral surgeons (for implant placement or grafting) and periodontists (for gum health). Therefore, if you are seeking a provider for full mouth reconstruction, finding a member of the American College of Prosthodontists is an excellent strategy, as you are seeking out a specialist whose training and practice are centred around these types of complex restorative challenges, offering a high level of expertise and experience in rebuilding compromised mouths.
Is Full Mouth Reconstruction Available at London Dental Implant Clinics?
Yes, full mouth reconstruction is very commonly available at dental implant clinics, particularly those located in major cities like London. Clinics that specialise in dental implants are inherently involved in one of the most significant components of many full mouth reconstruction cases: the replacement of missing teeth with stable, long-lasting implant-supported restorations. A clinic focused on dental implants is likely to employ dentists with expertise in implantology (the surgical placement of implants) and the subsequent prosthetic restoration of those implants. Many implant clinics also have strong relationships with or employ prosthodontists, who, as mentioned, are specialists in reconstruction and frequently utilise implants as a key tool in their comprehensive treatment plans. Furthermore, implant placement often requires adjunctive procedures like bone grafting or sinus lifts, skills that are standard within a dedicated implant clinic. While an implant clinic’s primary focus might be missing teeth, the complexity of placing multiple implants or restoring an entire arch with implant-supported prosthetics (like full-arch bridges or dentures) falls squarely within the realm of full mouth rehabilitation. Such clinics are typically equipped to handle complex restorative cases that involve implants as a central element. If your need for reconstruction stems significantly from missing teeth or requires substantial implant work, a reputable dental implant clinic in a city like London is an excellent place to inquire about full mouth reconstruction services, as they possess the necessary expertise and resources for a crucial part of the process, and often manage the entire case or collaborate with other specialists as needed.
Can Our Dentists Perform Full Mouth Reconstruction?
Whether “our dentists” – meaning the dentists at your current or local general dental practice – can perform full mouth reconstruction is a question that requires direct inquiry. General dentists are highly skilled practitioners who perform a wide range of essential dental services. However, full mouth reconstruction represents a level of complexity that goes significantly beyond routine procedures like fillings, single crowns, or basic cleanings. It demands advanced training, specific experience, and the ability to plan and execute a multi-disciplinary treatment strategy involving potentially complex surgical and restorative steps. Some general dentists do pursue extensive continuing education in advanced restorative dentistry and comprehensive care, equipping them to handle moderately complex reconstruction cases. Others may not have this specific focus or training. The best way to determine if your current dentist or the dentists at a particular practice can perform full mouth reconstruction is to simply ask them directly. Explain your situation and inquire about their experience and capabilities in treating such comprehensive cases. A responsible general dentist, even if they don’t personally perform full mouth reconstruction, will be able to accurately assess your needs and, if necessary, refer you to a qualified specialist, such as a local prosthodontist, or an oral surgeon/restorative team that specialises in these complex cases. They can often serve as your initial point of contact and guide you toward the appropriate specialist if your case requires expertise beyond the scope of their practice, ensuring you receive care from a provider with the necessary skills for the specific challenges of full mouth reconstruction.
Is Full Mouth Dental Restoration Available in Sydney?
Yes, full mouth dental restoration services are definitely available in a major metropolitan city like Sydney, Australia. Sydney boasts a large number of highly qualified dental professionals, including general dentists with advanced training in restorative dentistry, as well as specialists like prosthodontists, oral surgeons, and periodontists, who are equipped to plan and perform complex full mouth reconstruction cases. As a major global city, Sydney’s dental community often has access to the latest technologies, materials, and techniques in comprehensive restorative dentistry. You can find practitioners offering these services in various settings, from individual specialist practices (particularly prosthodontists’ offices) to larger multi-disciplinary dental clinics that house various specialists under one roof, facilitating the collaborative care often needed for full mouth reconstruction. To find a suitable provider in Sydney, you could search specifically for “Prosthodontist Sydney,” “Full Mouth Reconstruction Sydney,” or “Complex Restorative Dentistry Sydney.” Websites of dental professional associations in Australia might also offer directories of specialists. As always, the best approach is to research potential clinics, read reviews if available, and schedule a consultation to discuss your specific needs and the dentist’s experience and approach to full mouth restoration. The availability of skilled practitioners and advanced dental facilities in Sydney means that comprehensive oral rehabilitation is certainly within reach for residents in that area, offering solutions for even the most complex dental challenges.
Can I Get Full Mouth Restoration or Dental Reconstruction in New York City?
Absolutely. New York City is a global hub for advanced medical and dental care, and it offers abundant options for obtaining full mouth restoration or dental reconstruction. As a major metropolitan area, NYC is home to a vast number of highly skilled dental professionals, including numerous board-certified prosthodontists – the specialists primarily focused on complex restorative cases like full mouth reconstruction. You can find practitioners offering these services throughout the five boroughs, from private practices catering to complex restorative and cosmetic needs to large dental centres and university dental schools that often have dedicated departments or clinics for prosthodontics and comprehensive care. Many practices in NYC are equipped with state-of-the-art technology for diagnostics and treatment, and they often work with elite dental laboratories to fabricate high-quality custom restorations. Given the competitive landscape, you’ll find dentists in NYC who are at the forefront of advanced restorative techniques. To find a provider, you can search for “Prosthodontist NYC,” “Full Mouth Reconstruction New York,” “Comprehensive Restorative Dentistry NYC,” or look for multi-specialty dental practices in specific neighbourhoods. Referrals from your general dentist are also a good starting point. Be prepared to research different practices, review their credentials and experience, and schedule consultations to determine the best fit for your specific needs and to discuss treatment plans and costs in detail. The density of dental professionals and facilities in New York City ensures that patients seeking complex full mouth restoration have access to a wide range of highly qualified providers.
Does Mullane Dental Offer Full Mouth Reconstruction?
Regarding a specific practice like Mullane Dental, whether they offer full mouth reconstruction depends entirely on the scope of services provided by their practice and the specific training and experience of the dentists on their team. Mullane Dental appears to be a general dental practice (based on a quick search, assuming a specific practice is being referenced). While some general dental practices may offer a broad range of services, including some restorative procedures, full mouth reconstruction is a highly complex specialty area. To determine if Mullane Dental provides full mouth reconstruction, you would need to directly contact their office. Ask specifically about their services in full mouth reconstruction or full mouth restoration. Inquire about the experience of the dentists there in handling complex, comprehensive cases involving multiple missing or damaged teeth and bite issues. It is possible that one or more dentists at Mullane Dental have pursued significant continuing education in advanced restorative techniques that enable them to undertake such cases. However, if they do not, or if your case is particularly complex, a reputable practice like Mullane Dental should be able to refer you to a qualified specialist, such as a local prosthodontist, who is specifically trained for this type of work. The best and only way to get a definitive answer about their specific service offerings for full mouth reconstruction is to reach out to Mullane Dental directly and schedule a consultation to discuss your oral health needs and their capabilities.
Frequently Asked Questions About teeth reconstruction
Navigating the prospect of comprehensive dental work like teeth reconstruction often brings a host of questions to mind. It’s a complex topic, covering everything from the fundamental possibility of rebuilding teeth to the intricate details of cost, duration, and pain management. Patients considering this path naturally seek clarity on what is involved, who it’s for, and what the outcomes are likely to be. These frequently asked questions touch upon the core concerns people have when facing the possibility of rebuilding their smile and bite. Understanding the answers to these questions is crucial for making informed decisions and feeling confident about embarking on the reconstruction journey. They get right to the heart of the matter, addressing the practicality, necessity, process, and implications of undertaking such a significant dental transformation, providing a solid foundation of knowledge for anyone exploring this vital option for restoring their oral health and quality of life. Let’s dive into some of the most common queries that arise when the topic of teeth reconstruction comes to the fore, aiming to provide clear, comprehensive answers that illuminate the path forward for those in need of extensive dental restoration.
Can you reconstruct teeth?
Yes, let’s reiterate this foundational truth with absolute certainty: teeth can indeed be reconstructed. This isn’t wishful thinking or a futuristic concept; it’s a tangible reality achieved through the skilled application of modern dentistry, specifically within the realm of restorative dentistry and prosthodontics. The ability to reconstruct teeth has evolved dramatically over the past few decades thanks to advancements in materials, techniques, diagnostic technology, and interdisciplinary collaboration among dental specialists. When we say “reconstruct,” we mean far more than just superficial repairs. We mean the ability to rebuild teeth that are severely worn down, broken, decayed beyond standard repair, or missing entirely, while simultaneously addressing complex issues like bite alignment problems, jaw joint pain, and underlying gum or bone deficiencies. This comprehensive approach to rebuilding teeth involves using a variety of procedures tailored to the individual’s specific constellation of problems. It might include placing durable, custom-made crowns on damaged teeth to restore their form, function, and strength; using dental implants surgically placed into the jawbone to replace missing tooth roots and provide a stable foundation for new teeth; fabricating bridges or dentures to fill gaps where teeth are missing; and employing techniques to correct bite discrepancies that contribute to damage. The possibility of teeth reconstruction offers immense hope to individuals who have suffered extensive damage or tooth loss, providing a pathway to regain not just a functional bite and improved oral health but also the aesthetic confidence that comes with a complete, healthy-looking smile. It is a powerful testament to what modern dentistry can achieve, offering life-changing solutions for even the most challenging dental conditions.
How does teeth reconstruction work?
The process of teeth reconstruction operates through a highly structured, multi-phase approach that prioritizes diagnosis, planning, foundational treatment, and then the precise placement of restorative components. It doesn’t begin with fixing teeth directly but with a deep, investigative dive into the patient’s entire oral system. This initial phase involves comprehensive diagnostics: detailed clinical examination, extensive X-rays and 3D scans to assess bone structure and tooth roots, precise models of the teeth and bite, and evaluation of the jaw joints and muscles. This information is meticulously analysed by the dental team, often led by a prosthodontist, to determine the root causes of the problems (e.g., is it wear, trauma, decay, bite issues?) and assess the extent of the damage. Based on this thorough understanding, a detailed, step-by-step treatment plan is formulated, outlining every necessary procedure and its optimal sequence. The actual work begins with addressing any underlying diseases, such as periodontal (gum) disease https://dentale-albania.com/general-dentistry/gum-disease-treatment/ or active decay, creating a healthy foundation. This might involve scaling and root planing, extractions of unsavable teeth, or root canal therapy. Surgical phases, such as bone grafting to rebuild deficient bone or dental implant placement to replace missing roots, are then performed, requiring crucial healing periods. Only after these preparatory steps and healing are complete does the primary restorative phase commence. This involves preparing the teeth for crowns or veneers, placing abutments on implants, taking impressions for final restorations, fitting temporary prosthetics, and finally, seating and adjusting the custom-fabricated permanent crowns, bridges, or dentures across both arches. The process is collaborative, involving the patient’s input, and often requires coordination among different specialists, ensuring that each stage is completed precisely and contributes to the overall goal of a stable, functional, and aesthetically pleasing rebuilt bite.
Who Requires a Full Mouth Reconstruction?
Full mouth reconstruction is typically required by individuals who have suffered extensive damage or loss to multiple teeth, leading to significant impairment of their oral function, health, and often, causing chronic pain. This is not a procedure for minor dental issues. The primary candidates are those with mouths where widespread problems exist across both the upper and lower arches, impacting the entire bite system. This includes patients whose teeth have been severely worn down by years of grinding (bruxism) or acid erosion, leading to shortened teeth, bite collapse, and pain. Individuals who have experienced significant dental trauma, such as from an accident, resulting in multiple broken, fractured, or missing teeth, often need full reconstruction to restore structure and function. Those with widespread, severe tooth decay that has compromised the integrity of numerous teeth, leading to cavities, infections, and tooth loss, are also prime candidates. Furthermore, patients suffering from chronic jaw pain, headaches, or muscle soreness related to a severely misaligned bite (malocclusion) that is causing damage to their teeth or jaw joints frequently require reconstruction to correct the bite and alleviate symptoms. People with congenital conditions affecting tooth development or those who have undergone treatments for serious diseases like oral cancer, which have compromised oral tissues, may also need extensive rehabilitation. Essentially, anyone whose dental issues are so extensive, complex, and interconnected that they cannot be effectively treated with isolated procedures, and where the problems significantly impact their ability to eat, speak, or live without pain, is a likely candidate for full mouth reconstruction, seeking a comprehensive solution to reclaim oral health and quality of life.
How much does it cost to rebuild teeth?
The cost to rebuild teeth through full mouth reconstruction is a significant financial investment, and it varies dramatically from patient to patient due to the highly individualized nature of the treatment. There is no single price tag; it is determined by the complexity and extent of the dental problems, the specific procedures required, the materials used for the restorations, the number of teeth involved, whether surgical procedures like bone grafting or implant placement are necessary, the fees of the dental professionals involved (specialists typically have higher fees), the geographic location of the clinic, and the complexity of the laboratory work needed for the custom prosthetics. Because it’s a comprehensive plan addressing the entire mouth, the cost is cumulative, reflecting the sum of all diagnostic records, planning time, preparatory treatments (like gum therapy or extractions), surgical phases, temporary restorations, laboratory fees, permanent restorations (crowns, bridges, implants, dentures, veneers), and numerous appointments. While specific estimates can only be provided after a thorough examination and detailed treatment plan are created, patients should anticipate costs ranging from approximately $20,000 to $100,000 or more. Mild to moderate cases focusing primarily on wear might fall on the lower end, while complex cases involving extensive tooth loss, multiple implants with grafting, and full-arch fixed prosthetics will be significantly higher. Dental insurance typically provides only limited coverage, often capped by annual maximums that are quickly met. Therefore, patients often explore financing options such as dental payment plans, third-party medical financing companies, or personal loans. Understanding that this is a major investment in long-term oral health and quality of life, and obtaining a detailed written estimate upfront, is crucial for financial planning.
How long does teeth reconstruction last?
The longevity of teeth reconstruction, meaning how long the final restorations are expected to last before needing repair or replacement, is not a fixed duration but rather an expected lifespan influenced by several key factors. While the process of reconstruction itself might take months or years, the materials and techniques used are designed for significant durability, often providing many years, frequently decades, of reliable service. The lifespan varies depending on the specific type of restoration and the materials used. For instance, high-quality dental crowns and bridges, common components of reconstruction, are typically expected to last between 10 to 15 years, or even longer, depending on the material, the forces placed upon them, and the patient’s oral hygiene. Dental implants, which replace tooth roots, have a remarkably high success rate and, with proper care, can potentially last a lifetime. The crowns or prosthetics attached to implants may need periodic replacement, but the implant post itself is designed to be permanent. Veneers usually last 7-15 years. Dentures, whether traditional or implant-supported, may require relining, rebasing, or eventual replacement as the underlying bone and tissue change over time, although implant-supported dentures offer much greater long-term stability. The ultimate longevity is a function of several factors: the quality of the materials and lab work, the precision of the planning and execution, the patient’s oral hygiene habits, their diet, whether they use a nightguard if they grind their teeth, and attendance at regular dental check-ups for professional cleaning and assessment. It’s a long-term investment requiring ongoing vigilance for maximum return.