Key Takeaways
-
- Experiencing *some* pain or discomfort after a root canal is **normal** and common.
-
- This pain is usually due to inflammation in the surrounding tissues, **not** the removed nerve.
-
- Acute pain typically subsides within **1-3 days**, manageable with pain relievers.
-
- Lingering sensitivity or feeling “different” can last for **weeks or even months**.
-
- **Persistent pain**, swelling, fever, or worsening symptoms are **not normal** and require contacting your dentist.
-
- Pain occurring **months or years later** often indicates a new problem or treatment failure, usually due to re-infection.
- Following **post-operative instructions** and getting a **permanent restoration** are crucial for successful healing.
Understanding Root canal and pain after: Is It Normal?
Alright, let’s cut straight to the chase – yes, experiencing some level of discomfort or pain after a root canal procedure is not just normal, it’s incredibly common. Think of it like this: you’ve had a rather significant dental intervention where infected or damaged pulp, the soft tissue containing nerves and blood vessels inside your tooth, is carefully removed. The canals are cleaned, disinfected, shaped, and then sealed. While the original *source* of that searing, often unbearable pre-procedure pain (the infected nerve) is gone, the tissues surrounding the tooth – the ligaments, bone, and gums – have just undergone quite the experience. They’ve been poked, prodded, irrigated, and filled. This manipulation inevitably leads to inflammation, a natural and necessary part of your body’s healing process. So, the initial pain isn’t the old nerve screaming; it’s the neighbourhood around the tooth reacting to the work that’s been done. It’s a temporary protest from the area, a sign that your body is busy repairing itself and settling down after the biological equivalent of a minor renovation project. Reassuringly, this discomfort typically manifests as a mild to moderate ache or a distinct tenderness, especially when you touch the tooth or try to chew on that side. It’s a sensation you’ll likely notice, but it shouldn’t be debilitating. It’s the body’s post-op report, entirely expected and, in many ways, a confirmation that the healing wheels are turning. Don’t let the internet horror stories send you spiraling; a little post-procedure soreness is par for the course.
Is it Normal to Feel Pain After a Root Canal?
Absolutely, unequivocally, *yes*. Feeling some pain, sensitivity, or discomfort after a root canal is not just normal, it’s virtually the standard experience. You’ve had tissue removed from the core of your tooth, canals cleaned and shaped, and then sealed. The procedure, while aimed at saving the tooth and eliminating deep infection, causes inflammation in the delicate periodontal ligament that surrounds the tooth’s root and attaches it to the bone. This ligament is rich in nerve endings, and they’re now reacting to the disruption. Imagine stubbing your toe – the initial pain is sharp, but then you get a dull ache and sensitivity that lasts for a while as the tissues recover. A root canal is a far more controlled process, but the principle of tissue reaction is similar. The body’s immune response kicks in, sending inflammatory cells to the area to clean up debris and start the repair process. This inflammation results in swelling at a microscopic level around the root tip, which can lead to pressure and tenderness. This isn’t a sign of failure; it’s a sign of healing. The pain is usually described as a dull ache, soreness, or tenderness when biting or touching the tooth. It’s a vastly different sensation from the throbbing, constant agony of the pre-root canal infection, which originated from the dying or infected nerve *inside* the tooth. This post-op discomfort is external to the tooth’s core and is part of the natural recovery arc.
How Much Pain after a Root Canal is OK?
Defining “okay” pain is subjective, as individual pain tolerance varies wildly. However, general guidelines suggest that acceptable post-root canal pain is typically mild to moderate. It should be noticeable, perhaps annoying, but manageable with over-the-counter (OTC) pain relievers like ibuprofen (Advil, Motrin) or acetaminophen (Tylenol), or a combination of the two, as recommended by your dentist. Think of it as being comparable to the discomfort you might feel after a minor surgical procedure, like a tooth extraction or even a deep filling. It shouldn’t be excruciating, keeping you up all night despite medication, or so severe that it stops you from performing routine daily activities (aside from eating on the treated side, which you should avoid anyway). If the pain is so intense that even prescription pain medication isn’t touching it, or if it’s getting significantly worse day by day instead of gradually improving, that’s a sign that the pain level might be *beyond* “normal” and warrants a call to your dental office. Normal post-op pain feels like tenderness or a dull ache, especially when pressure is applied, whereas excessive pain, particularly if accompanied by swelling or fever, points towards a potential complication that needs prompt attention. Your dentist can provide a clearer expectation based on the complexity of your specific procedure.
Will I experience pain or discomfort following a root canal?
In all likelihood, yes, you will experience *some* degree of pain, discomfort, or at least a heightened awareness of the tooth after a root canal. It’s simply a physical impossibility to perform such an intricate procedure within the confines of the tooth and the surrounding bone without *any* tissue response. While some lucky individuals report minimal sensation, they are the exception rather than the rule. The vast majority will feel something. The intensity and duration can vary based on several factors: the severity of the original infection (a tooth with a large abscess might have more surrounding inflammation to resolve), the complexity of the tooth’s anatomy and the procedure itself (difficult canals, calcifications), and your individual pain threshold and healing capabilities. Furthermore, just the simple act of keeping your mouth open for an extended period can lead to jaw muscle soreness, adding another layer to the post-procedure feeling. Even if the pain from the nerve inside the tooth is gone (which it should be), the pain receptors in the bone and ligament around the root are still very much active and will signal discomfort as they heal. So, prepare for some sensation, but focus on the fact that this pain is a sign of recovery, not continued infection, in the vast majority of cases. It’s the cost of saving the tooth, and one that is usually temporary and manageable.
How Long Does Pain Last After a Root Canal and What is the Recovery Timeline?
Understanding the recovery timeline after a root canal is key to managing expectations and avoiding unnecessary worry. It’s not an instantaneous fix where all sensation vanishes the moment the procedure is done. Think of it as a phased recovery process. The initial, more noticeable pain is usually short-lived, while a lingering sensitivity or different feeling in the tooth can persist for a longer period as the surrounding tissues completely regenerate and settle. The goal of the root canal is to eliminate the chronic, often excruciating pain of the infected pulp. The pain *after* the procedure is a temporary, acute phase related to healing from the treatment itself. Most patients find that the discomfort peaks within the first 24-48 hours and then begins a steady decline. Complete resolution of all post-procedure symptoms can take anywhere from a few days to a couple of weeks, though the tooth might feel “different” or slightly sensitive to pressure for a bit longer. It’s a process, not a light switch, and patience is definitely required. During this time, the bone around the root tip where the infection was located is also undergoing significant remodelling and healing, which contributes to the overall timeline. The body is essentially cleaning up the remnants of the infection and repairing the damage, and that takes time and can involve some level of discomfort.
How long until a root canal stops hurting?
For the majority of patients, the most bothersome, acute pain or soreness after a root canal typically subsides significantly within 1 to 3 days. This is the period during which the initial inflammation from the procedure is at its peak and then starts to calm down. You should notice a gradual improvement day by day, with the need for pain medication decreasing over this time. While the sharp pain associated with the original infection should be gone immediately (since the nerve is removed), the tenderness from tissue manipulation and inflammation around the root can last for these initial few days. If you are still experiencing significant, disruptive pain beyond this 72-hour window, it’s worth contacting your dentist. Mild discomfort, sensitivity when biting, or a dull ache might linger for up to a week or two, which is also considered within the normal range as the tissues continue to heal. The critical point is that the pain should be *decreasing* over time, not increasing. The swift resolution of acute post-op pain is a good indicator that the initial phase of healing is progressing as expected.
How long does it take for root canal tooth to feel normal?
Ah, the million-dollar question – what constitutes “normal” and how long until you get there? While the acute pain typically disappears within days, the tooth itself might not feel completely “normal” for a longer duration, sometimes weeks to even a few months. The sensation isn’t usually pain, but rather a feeling of difference, sensitivity, or slight awareness of the tooth. Why? Because the supporting structures around the root – the periodontal ligament and the surrounding bone – need time to fully recover and remodel. If there was an infection at the root tip, the bone lesion needs to heal, which is a process that happens gradually over many months and is monitored with follow-up X-rays. The tooth might also feel slightly different because it’s been structurally altered (a filling placed, potentially a crown needed). Sensitivity to pressure or biting might linger simply because the ligament is still recovering its full resilience. Getting the permanent restoration (like a crown) placed is also a crucial step in making the tooth feel normal and restoring its full function and protection. Until then, the temporary filling might feel different or be sensitive to pressure. The key takeaway is that while the pain from the *procedure* resolves relatively quickly, the full integration and complete lack of sensation in the tooth’s vicinity can take longer, representing the deeper level of tissue healing and adaptation occurring.
How Long Does the Pain Last After a Root Canal?
Let’s consolidate the timeline for post-root canal pain. The most intense or acute phase of discomfort, typically described as soreness or a dull ache, usually lasts for 1 to 3 days. During this period, managing the pain with over-the-counter or prescribed medication is most necessary. Following this initial period, the discomfort should gradually subside. You might experience mild sensitivity, particularly when chewing, for up to a week or two. This lingering sensation is still considered normal and indicative of ongoing healing. Factors influencing the duration include the severity of the initial infection (more severe infections often mean more post-op inflammation), whether the tooth was already causing significant pain before the procedure, the complexity of the root anatomy, and how extensive the cleaning and shaping process was. If the tooth was non-vital (nerve was already dead) without significant surrounding infection, the post-op pain might be less severe and shorter-lived than if the tooth had an active, painful abscess. Conversely, sometimes a tricky procedure in a complex tooth can lead to slightly more prolonged discomfort. The crucial point, however, is the *trend*. The pain should consistently improve day by day and week by week. Any pain that persists intensely beyond two weeks, or pain that worsens significantly after the first few days, falls outside the typical recovery window and warrants immediate consultation with your dentist or endodontist.
Why Do You Have A Toothache After A Root Canal? Exploring the Causes
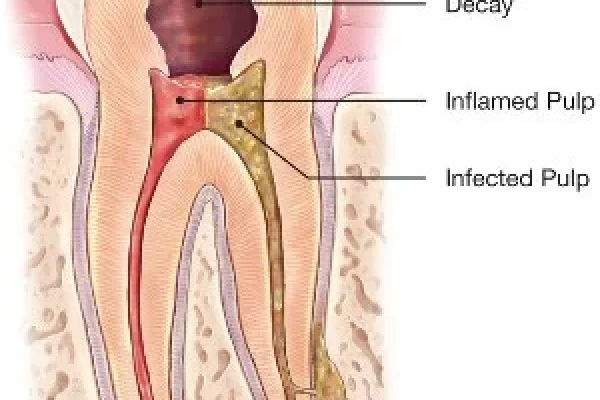
It seems counterintuitive, doesn’t it? The part of the tooth that feels pain (the pulp, containing the nerve) is removed, yet you can still experience a toothache afterwards. This is where understanding the anatomy *around* the tooth becomes critical. A root canal addresses the *inside* of the tooth, but the tooth is anchored within the jawbone by the periodontal ligament, a complex network of fibers, blood vessels, and yes, nerve endings. This ligament and the surrounding bone are highly sensitive to pressure and inflammation. When a root canal is performed, even meticulously, these surrounding tissues are inevitably affected. Instruments extend slightly beyond the root tip, irrigating solutions reach the area, and the tooth is subjected to forces during the procedure. This irritates the periodontal ligament and bone, triggering an inflammatory response. So, the pain isn’t coming from *inside* the tooth anymore; it’s coming from the external support system reacting to the recent activity. It’s a temporary state of protest and repair in the tissues that hold your tooth firmly in place. Understanding this distinction is vital – the cause of post-root canal pain is fundamentally different from the cause of the pain that necessitated the root canal in the first place.
What Causes Pain After A Root Canal?
Several factors contribute to post-root canal pain, primarily related to the body’s response to the procedure and the healing process of the surrounding tissues.
-
- **Inflammation of the Periodontal Ligament:** This is arguably the most common cause. The ligament that attaches the tooth root to the jawbone gets irritated during the cleaning and shaping of the root canals, as well as from the materials used to fill the canals. This causes inflammation and tenderness, especially when chewing or touching the tooth.
-
- **Pressure from the Temporary Filling /Crown:** Sometimes, if the temporary filling or crown sits slightly “high,” meaning it hits before your other teeth when you bite down, it puts excessive pressure on the treated tooth and its sensitive ligament, causing pain. Adjusting the height of the restoration can resolve this quickly.
-
- **Residual Infection in Surrounding Bone/Tissue:** While the main source of infection inside the tooth is removed, sometimes the infection has spread into the bone or tissues around the root tip. Healing these areas takes time, and during this process, there can be lingering tenderness or a dull ache.
-
- **Irritation at the Root Tip:** During cleaning, debris and bacteria can sometimes be pushed slightly past the root tip into the surrounding bone. This exacerbates inflammation and can cause a temporary flare-up of pain.
-
- **Muscle Soreness:** Keeping your mouth wide open for the duration of the procedure can strain the jaw muscles (temporomandibular joint and associated muscles), leading to soreness and aching that might feel like tooth pain but is muscular in origin.
-
- **Reaction to Filling Materials:** Rarely, a patient might have a mild inflammatory reaction to the materials used to fill the root canals or the temporary restoration.
- **Pre-existing Conditions:** If the patient had significant pre-operative pain or a large infection, the post-operative pain might be more pronounced as the body works harder to clear the extensive inflammation. These causes are typically temporary and resolve as healing progresses.
Why is my pain worse after a root canal?
While some initial pain is expected, if your pain is significantly worse *after* the root canal than before, or if it intensifies sharply in the days following the procedure instead of improving, this warrants investigation. Several reasons could explain this:
-
- **Post-Treatment Flare-up:** Sometimes, manipulating the infected tissues during the procedure can irritate the area, leading to a temporary exacerbation of inflammation and pain, especially if there was a significant infection (abscess) present beforehand. It’s like stirring up a hornet’s nest before getting rid of it entirely.
-
- **Procedural Irritation:** While rare with skilled practitioners, excessive manipulation or accidental irritation of the tissues beyond the root tip could cause more significant immediate inflammation.
-
- **Allergic Reaction:** An uncommon but possible cause is an allergic or inflammatory reaction to the materials used within the root canal or the temporary filling.
-
- **High Temporary Filling/Restoration:** As mentioned earlier, if the temporary restoration is too high, the continuous biting pressure can significantly increase pain. This is a simple fix for your dentist.
-
- **Incomplete Debridement or Missed Canal:** In very rare cases, if there were anatomical complexities that led to a missed canal or incomplete removal of infected tissue, this could result in persistent or worsening pain. This would likely require further treatment.
- **Cracked Tooth:** If the tooth had an undetected crack extending into the root structure before or during the procedure, this could become more symptomatic afterwards, leading to pain, especially with biting pressure. Severe or worsening pain isn’t the norm and should always prompt a follow-up call to your dentist.
Does The Tooth Pain Increase Days After Root Canal Treatment?
This is a critical point to understand: **No, typically, tooth pain should *not* significantly increase days after root canal treatment.** While you might experience discomfort that peaks within the first 24-48 hours, the expected trajectory is one of gradual improvement. The pain should be manageable and progressively lessen over the following days. If, after the initial couple of days, your pain suddenly worsens, becomes more intense or throbbing, is accompanied by new or increasing swelling (especially noticeable on your face or gums), or you develop a fever, these are warning signs. A sharp increase in pain after the initial post-op period suggests something is not progressing as expected. It could indicate a flare-up of infection (though the nerve is gone, bacteria can still be present in the surrounding bone), an issue with the temporary restoration, or potentially other complications. While some mild fluctuations in discomfort might occur, a definitive trend towards *more* pain after the first few days is *not* normal healing and requires prompt communication with your dental professional for evaluation. Don’t tough it out if the pain is getting significantly worse; seek advice.
Why Might There Be Pain After a Root Canal Months or Even Years Later?
While the vast majority of root canal treatments are successful and result in a pain-free, functional tooth for many years, they aren’t infallible. Sometimes, pain can emerge or return months or even years after the procedure was completed and the tooth was thought to be fully healed. This is a less common scenario than immediate post-op discomfort, but it’s a possibility patient’s should be aware of. When pain occurs long after treatment, it typically signals that something has gone wrong with the treated tooth or the surrounding area. It’s not a re-emergence of the *original* infection within the canal system (as that should have been thoroughly cleaned and sealed), but rather a new issue or a delayed manifestation of an initial problem that wasn’t fully resolved. The key is that this late-onset pain indicates a problem that requires investigation, usually involving updated X-rays and a clinical examination to determine the cause and necessary steps to resolve it, which might include retreatment, surgery, or in some cases, extraction. Don’t assume old dental work is problem-proof forever; symptoms appearing long after the fact are definitely worth getting checked out.
Why does my tooth still hurt after a root canal? Persistent Pain Explained
“Persistent pain” usually refers to discomfort that lasts significantly longer than the typical 1-2 week recovery period, potentially extending for months. This isn’t the norm and points to an underlying issue that needs to be diagnosed. Several reasons can cause pain to linger for weeks or months after a root canal:
-
- **Re-infection:** This is a common cause of persistent pain. Bacteria can re-enter the tooth if the temporary filling or final restoration (crown) is not placed promptly or properly, leading to leakage. New decay forming around the restoration can also allow bacteria in. Sometimes, even if the initial treatment was perfect, aggressive bacteria from the oral environment can find a way back into the sealed canal system over time if the outer seal is compromised.
-
- **Missed Canals:** Some teeth, particularly molars, have complex anatomy with multiple canals. If a very narrow or hidden canal was missed during the initial cleaning and sealing, the tissue within it can become necrotic or infected, leading to chronic pain months down the line.
-
- **Incomplete Cleaning/Disinfection:** In challenging cases, bacteria or infected tissue might not have been completely removed from all parts of the complex canal system during the initial treatment, allowing a low-grade infection to persist and eventually flare up.
-
- **Extracanalic Infection:** Sometimes, infection resides not just *inside* the canal but in the bone and tissues *outside* the root tip. While the root canal addresses the internal source, if the external infection is aggressive or doesn’t heal properly after the internal source is removed, it can cause persistent pain.
-
- **Fractured Root:** A crack in the root of the tooth can be difficult to detect. If a root fracture occurs, it can allow bacteria from the mouth to track down the crack and infect the surrounding bone, causing pain. Root fractures often have a poor prognosis.
-
- **Non-healing Periapical Lesion:** The area of infection at the root tip (periapical lesion) should heal after the root canal. In some cases, this healing doesn’t occur, leading to chronic inflammation and pain.
- **Pain from Neighboring Structures:** Sometimes, the pain isn’t actually coming from the treated tooth but from an adjacent tooth, the jaw joint, or a nerve issue in the face, which can be mistaken for pain from the tooth. Diagnosing the exact cause of persistent pain requires a thorough examination, often including new X-rays (standard and possibly 3D cone-beam CT) and clinical tests.
Why does my root canal hurt after months?
When pain surfaces several months after a root canal procedure, it almost always indicates a problem that has developed *after* the initial treatment or was not fully resolved by it. It’s not the initial healing discomfort we discussed earlier. Common culprits for pain appearing months down the line include:
-
- **Re-infection due to coronal leakage:** The most frequent reason. The outer seal of the tooth (either the temporary filling, the final filling, or the crown) is compromised. This allows oral bacteria and saliva to seep into the root canal system, leading to a new infection inside the tooth and subsequent inflammation/infection in the bone around the root tip. This is why getting the final restoration placed promptly after a root canal is crucial – the temporary filling is just that, temporary, and not designed to provide a long-term, bacteria-proof seal.
-
- **Fracture of the tooth or root:** Teeth that have had root canals are more brittle because the pulp is removed (which provides some moisture and resilience) and they often have large fillings or have lost significant structure. A crack or fracture can develop months or years later from biting forces, allowing infection in.
-
- **New decay:** Developing new cavities on the tooth surface or beneath the restoration can lead to leakage and re-infection of the root canal system.
-
- **Failure of the periapical lesion to heal:** In some cases, despite a technically perfect root canal, the chronic infection site at the root tip (the periapical lesion) doesn’t resolve. This can be due to very resistant bacteria, a cyst formation, or other factors preventing healing, leading to lingering or returning symptoms.
- **Missed anatomy:** Sometimes, very complex or extra canals were not located and treated during the initial procedure. Over time, tissue breakdown and infection in these untreated areas can cause pain. Pain emerging months after treatment is a clear signal that the tooth needs to be re-evaluated by an endodontist or general dentist experienced in root canal treatment.
Experiencing root canal tooth pain months or years after treatment? Why does this happen?
Okay, let’s talk about the long game. Pain emerging not just months, but even *years* after a root canal treatment is a more significant concern, as it typically points to a failure of the initial treatment or a new problem entirely. While root canals boast a high success rate (often above 95% in studies), failure is a possibility, and symptoms can take a long time to manifest. The primary reasons for pain occurring years after a root canal mirror those causing pain after months, but with a longer timeline for the issue to develop or become symptomatic:
-
- **Coronal Leakage (Delayed):** The most common culprit. Over years, the filling or crown can wear down, chip, or develop microscopic gaps. This allows oral bacteria to slowly migrate into the root canal system, eventually leading to re-infection. Think of it like a slow leak that eventually causes a flood. The process can take a considerable amount of time to cause noticeable symptoms.
-
- **Root Fracture:** As mentioned, root-canal-treated teeth can be more susceptible to fracture over time, especially if they weren’t protected by a crown or if they were subjected to heavy biting forces or bruxism (teeth grinding). A fracture can develop gradually over years, allowing infection to set in.
-
- **New Decay:** Cavities can form on any tooth, and a tooth with a root canal is no exception. If decay reaches the internal tooth structure below the restoration, it can lead to re-infection of the root canal system.
-
- **Recurrence of Periapical Lesion:** In some cases, the bone lesion around the root tip might appear to heal initially but then recur years later. This could be due to persistent bacteria that were dormant, or other factors preventing long-term healing.
-
- **Procedural Complications (Delayed Manifestation):** Very occasionally, issues from the original procedure (like a separated instrument within the canal or a perforation) might not cause immediate symptoms but can lead to chronic inflammation or infection that flares up years later.
- **Re-treatment Failure:** If the tooth was previously retreated, the prognosis might be slightly lower than the initial treatment, making it more susceptible to late-onset issues. Pain occurring years after treatment warrants a thorough investigation by a dental professional. Often, re-treatment (cleaning and sealing the canals again) or periapical surgery is necessary to attempt to save the tooth.
Managing and Reducing Pain After a Root Canal Procedure
Dealing with any kind of pain is unpleasant, even if you know it’s temporary and expected. The good news is that the pain and discomfort following a root canal are typically very manageable with simple, accessible strategies. The goal here is to alleviate the immediate post-operative soreness, make the healing period as comfortable as possible, and prevent the pain from becoming a major disruption to your life. Your dentist will likely provide specific instructions tailored to your situation, but there are general guidelines that apply broadly to most patients undergoing a root canal. The focus is on controlling inflammation and providing comfort while your body does the crucial work of healing the tissues surrounding the treated tooth. You don’t have to just “suffer through it”; there are effective ways to dial down the discomfort and help you get back to feeling like yourself relatively quickly after the procedure.
What is the best pain relief after a root canal?
The “best” pain relief after a root canal often involves a multi-modal approach, frequently starting with over-the-counter (OTC) options. Non-steroidal anti-inflammatory drugs (NSAIDs) like **ibuprofen** (brand names include Advil, Motrin) are typically the first line of defense and highly recommended. NSAIDs work by reducing inflammation, which is a primary cause of post-procedure pain. Taking ibuprofen as directed by your dentist (often a higher initial dose followed by regular dosing for a few days) can significantly reduce swelling and pain. **Acetaminophen** (brand names include Tylenol) is another effective option, particularly if you cannot take NSAIDs due to medical conditions or allergies. Acetaminophen works differently, primarily by blocking pain signals to the brain, rather than reducing inflammation. Often, dentists recommend alternating between ibuprofen and acetaminophen or even taking them together (at different times, following specific dosing instructions) for enhanced pain relief, as they work synergistically. For more severe pain, your dentist might prescribe a stronger pain reliever, possibly a combination product containing an opioid (like hydrocodone with acetaminophen, e.g., Vicodin or Norco) for a short period (usually only 1-3 days). However, due to concerns about opioid dependence, dentists are increasingly prioritizing NSAIDs and acetaminophen first. Always follow your dentist’s specific dosage and timing instructions for any pain medication, whether OTC or prescription.
How to get rid of root canal pain?
While you might not be able to achieve *complete* elimination of pain instantly (healing takes time!), you can effectively manage and significantly reduce post-root canal discomfort. Here’s a comprehensive strategy:
-
- **Follow Medication Instructions:** This is paramount. Take the pain medication your dentist recommended or prescribed, exactly as directed, and start taking it before the local anesthetic completely wears off if advised. Stay on schedule for the first 24-48 hours, even if you start feeling better, to keep the inflammation under control.
-
- **Use Cold Compresses:** Applying an ice pack wrapped in a cloth to the outside of your cheek near the treated tooth can help reduce swelling and numb the area. Apply for 15-20 minutes at a time, with breaks in between, for the first day or two.
-
- **Avoid Chewing on the Treated Side:** Stick to eating soft foods and chew on the opposite side of your mouth, especially until the tooth receives its final restoration (filling or crown). Putting pressure on the tooth with the temporary filling will likely cause pain and could potentially dislodge the temporary seal.
-
- **Eat Soft Foods:** For the first few days, choose foods that require minimal chewing, like soup, yogurt, smoothies, mashed potatoes, scrambled eggs, and pasta. Avoid hard, crunchy, sticky, or very hot or cold foods that could irritate the area or damage the temporary filling.
-
- **Maintain Good Oral Hygiene:** Gently brush and floss around the treated tooth to keep the area clean and prevent infection, but be careful not to disturb the temporary filling. Your dentist might recommend a saltwater rinse.
-
- **Elevate Your Head:** When sleeping, keep your head slightly elevated to help reduce swelling.
-
- **Rest:** Allow your body time to heal. Avoid strenuous activities immediately after the procedure.
-
- **Contact Your Dentist if Needed:** Don’t hesitate to call your dental office if you experience severe pain, uncontrolled swelling, fever, a bad taste/discharge, or if your temporary filling comes out completely.
- **Attend Follow-Up Appointments:** It is absolutely critical to return to your dentist to have the permanent filling or crown placed on the tooth as soon as recommended. The temporary filling is not designed to provide a long-term, bacteria-proof seal, and delaying the permanent restoration significantly increases the risk of re-infection and failure.
How can I get instant relief from root canal pain?
Achieving truly “instant” relief from post-root canal pain is often an unrealistic expectation, as healing is a biological process that takes time. However, you can take steps to get *rapid* relief and make yourself more comfortable quickly. The fastest way to start alleviating the pain is by taking your prescribed or recommended pain medication as soon as possible, ideally *before* the local anesthetic completely wears off, if your dentist advises this. NSAIDs like ibuprofen, when taken promptly and at the correct dosage, can start reducing inflammation and pain signals relatively quickly, often within 30-60 minutes. Combining ibuprofen with acetaminophen (following dentist’s instructions) can also provide faster and more potent relief than either medication alone. Applying a cold compress to the outside of your cheek near the treated area can also offer relatively immediate, though temporary, numbing and swelling reduction. While you won’t likely feel zero pain the moment you swallow a pill, these methods are the quickest ways to initiate pain relief and start the process of becoming comfortable. Remember, consistency with medication and following post-op instructions are key to sustained comfort, not just instant fixes. If you’re experiencing severe, uncontrolled pain, contact your dentist immediately, as this could indicate a complication needing urgent attention.
Identifying Abnormal Pain After Root Canal Treatment: When to Worry
While some degree of discomfort after a root canal is normal, there are specific signs and symptoms that fall outside the realm of typical healing and should raise a red flag. Recognizing these warning signs is crucial because they could indicate a potential complication, such as a developing infection, a failure of the treatment, or an issue with the restoration. Ignoring these signs could lead to more significant problems and potentially jeopardize the treated tooth. Your dental team should provide you with clear post-operative instructions and inform you about what to expect and when to call them. However, empowering yourself with the knowledge of *abnormal* symptoms means you can be proactive about your health. This section is designed to highlight those less-than-normal signs that signal it’s time to pick up the phone and consult with your dentist or endodontist without delay. It’s about knowing the difference between the expected temporary ache and something more serious that requires professional evaluation.
What is not normal after a root canal?
Distinguishing normal post-operative discomfort from concerning symptoms is vital. Here’s a list of things that are *not* typically considered normal after a root canal and should prompt you to contact your dentist:
-
- **Severe, Uncontrolled Pain:** Pain that is excruciating and not adequately managed by the pain medication prescribed or recommended by your dentist. If the pain is getting worse despite following medication instructions, this is a red flag.
-
- **Significant Swelling:** Swelling that is noticeable on the outside of your face or jaw, or significant, increasing swelling of the gums around the treated tooth. Minor gum tenderness is okay, but visible facial swelling is not.
-
- **Fever:** Developing a fever after a root canal can be a sign of spreading infection.
-
- **Pus or Discharge:** Seeing pus or experiencing a foul taste from drainage near the treated tooth or on the gums is a strong indicator of infection.
-
- **Pain That Significantly Worsens After the First Few Days:** As mentioned before, pain should improve over time, not get worse after the initial 1-3 day peak.
-
- **Allergic Reaction:** Symptoms like rash, itching, or difficulty breathing (which are rare but serious) are not related to the tooth itself but could be a reaction to medication and require immediate medical attention.
-
- **Numbness or Unusual Sensations:** Prolonged numbness (beyond the initial effect of the anesthetic), tingling, or altered sensation that lasts for days or weeks in the lip, chin, or tongue is rare but could indicate nerve injury and should be reported.
- **Difficulty Opening Your Mouth:** While some jaw soreness is normal, severe limitation in opening your mouth could indicate muscle spasm or spreading infection.
If you experience any of these symptoms, don’t wait for your next scheduled appointment. Contact your dentist’s office right away to describe what you’re experiencing.
How to tell if you have an infection after a root canal?
While the root canal *removes* the main source of infection from inside the tooth, sometimes bacteria persist in the surrounding bone or re-enter the tooth, leading to a new or lingering infection. Signs that you might have an infection after a root canal treatment include:
-
- **Persistent or Worsening Pain:** Pain that doesn’t improve or gets significantly worse after the initial healing period (beyond a few days). Throbbing pain is a common sign of infection.
-
- **Swelling:** Swelling around the gum of the treated tooth or noticeable swelling on the face or jaw near the tooth. Swelling indicates inflammation, often due to bacterial presence.
-
- **Tenderness to Touch:** The gum tissue around the treated tooth or the jawbone near the root tip feels very sore or tender when you touch it.
-
- **Pus or Drainage:** Observing pus coming from the gum near the tooth, or a persistent bad taste in your mouth due to drainage from a small pimple-like bump on the gum (called a fistula or sinus tract).
-
- **Fever:** A raised body temperature can indicate a systemic response to infection.
- **Feeling Unwell:** General malaise, fatigue, or feeling run down in conjunction with dental symptoms.
It’s important to note that sometimes, infections after root canals can be “silent” and show no symptoms for a long time, only appearing on an X-ray. However, if you experience any of the above clinical signs, it’s crucial to contact your dentist promptly. Infection needs to be addressed, often with antibiotics and potentially further dental treatment (like retreatment or surgery) to eliminate the source.
How to tell if a root canal failed?
A root canal is considered “failed” if it doesn’t successfully eliminate the infection or if the tooth later becomes re-infected or develops another complication that renders the treatment ineffective. Signs that a root canal might have failed or is failing often include:
-
- **Return of Original Symptoms:** The same type of pain, swelling, or sensitivity that you experienced *before* the root canal procedure returns after a period of being symptom-free.
-
- **New Pain or Swelling:** Developing new, significant pain or swelling in the tooth or surrounding area months or years after the treatment. This pain might be different from the original pain.
-
- **Persistent Tenderness or Pain to Biting:** If the tooth remains chronically sensitive to pressure or biting months after the expected healing period.
-
- **Development of a Pimple on the Gum:** A fistula or sinus tract (a small bump that may release pus) appearing on the gums near the treated tooth is a classic sign of ongoing infection and treatment failure.
-
- **Radiographic Evidence:** Often, the first sign of failure is visible on an X-ray taken during a routine check-up. The X-ray might show the infection at the root tip (the periapical lesion) has not healed or has reappeared or grown.
- **Tooth Discoloration:** While not always indicative of failure, significant discoloration years later could sometimes point to issues within the tooth structure.
It’s important to distinguish between initial healing discomfort (which is normal and temporary) and true failure, which manifests later or involves symptoms that don’t resolve. If you suspect your root canal has failed based on these symptoms, your dentist will conduct an examination, take X-rays, and discuss potential options, which could include retreatment of the tooth, periapical surgery (apicoectomy), or ultimately, extraction of the tooth. Root canal failure is not uncommon, but often the tooth can still be saved with further intervention.
Experiencing Specific Types of Pain After a Root Canal: Pressure, Biting, and Nerve Pain
Sometimes, the pain after a root canal isn’t just a general ache; it’s a very specific sensation, often triggered by certain actions like biting down or touching the tooth. These specific types of pain have particular causes and can be more concerning depending on their timing and severity. Understanding *why* you might feel pain when you bite down or whether that lingering “nerve” sensation is normal is key to accurately assessing your post-procedure experience. While the main nerve *inside* the tooth is removed, your mouth is a complex network of nerves, and the tissues surrounding the treated tooth are still very much innervated. This section delves into these specific pain types to clarify their origins and implications after a root canal, helping you differentiate between expected sensitivity and signals of potential trouble.
Why Does a Tooth with Root Canal Hurt with Pressure or When Biting?
Pain when biting or applying pressure to a root-canal-treated tooth is one of the most common complaints during the initial recovery period. This specific type of pain is usually **not** coming from the nerve *inside* the tooth (which has been removed), but from the **periodontal ligament** that surrounds the root and anchors the tooth to the jawbone. Here’s why this happens:
-
- **Inflammation of the Periodontal Ligament:** The process of cleaning, shaping, and filling the root canals inevitably irritates the periodontal ligament at the root tip. This causes inflammation, and the ligament becomes sensitive to pressure. When you bite down, you put force on the tooth, which transfers stress to this inflamed ligament, resulting in pain or tenderness. This is a very common and normal part of the healing process for the first few days or even a couple of weeks.
-
- **High Temporary Filling or Restoration:** If the temporary filling or the final crown is slightly “high” (meaning it touches the opposing tooth with more force than your other teeth when you bite down), it creates excessive, constant pressure on the treated tooth. This overloads the healing periodontal ligament, causing pain every time you bite. This is a simple fix – your dentist can adjust the height of the filling or crown.
-
- **Periapical Inflammation/Infection:** If there was a significant infection at the root tip before the root canal, the bone and tissues in that area are inflamed or infected. Even after the root canal removes the source inside the tooth, the surrounding area needs to heal. Biting pressure can irritate this healing (or still infected) periapical region, causing pain. While initial tenderness is normal, severe or persistent pain on biting could indicate that the periapical area isn’t healing properly or that there’s residual bacteria.
- **Cracked Tooth or Root:** Less commonly, pain on biting, especially sharp pain, could be a sign of a crack in the tooth structure that extends into the root. Biting forces open and close the crack, stimulating nerve fibers in the ligament or allowing bacteria to enter, causing pain. If biting pain is severe, sudden, or feels like a sharp jolt, especially long after the procedure, it warrants immediate investigation for a possible fracture.
Will nerve pain go away after root canal?
This question requires a nuanced answer because the term “nerve pain” can be interpreted in different ways.
If by “nerve pain” you mean the kind of severe, often throbbing, spontaneous pain that originated from the infected or dying **pulp nerve inside the tooth** before the root canal – then **yes, that type of nerve pain should go away** immediately after the root canal procedure, because that nerve tissue has been removed. The primary goal of the root canal is to eliminate that specific pain source.
However, if by “nerve pain” you mean any sensation felt by **nerve endings** in the area, including those in the surrounding tissues like the periodontal ligament and bone – then **no, you might still feel sensation or discomfort** (which is transmitted by nerves) from these *external* structures as they heal. These tissues contain nerve endings that sense pressure, temperature (though the tooth itself shouldn’t be sensitive to cold/hot after the nerve is removed), and pain. The post-operative pain you feel (especially when biting or touching the tooth) is transmitted by these surrounding nerves, not the nerve that was inside the tooth. So, while the specific “pulp nerve pain” is gone, you can still experience pain or sensitivity transmitted by other nerves in your mouth during the healing process. Furthermore, very rarely, the inferior alveolar nerve (which runs through the jawbone and provides sensation to the lower lip and chin) can be irritated during procedures on lower back teeth, causing temporary numbness or altered sensation, which is a different type of nerve issue altogether and should be reported to your dentist.
Is jaw pain normal after a root canal?
Yes, experiencing some degree of jaw pain or soreness after a root canal is quite common and usually nothing to be overly concerned about. Root canal procedures, especially on back teeth, can take a significant amount of time, sometimes an hour or two (or even longer for complex cases). During this time, you have to keep your mouth open wide, often with the help of a bite block to keep it stable. Maintaining your jaw in this position for an extended period can strain the muscles and joint involved in opening and closing your mouth (the temporomandibular joint or TMJ and surrounding muscles). This can lead to muscle fatigue, soreness, stiffness, or aching in the jaw area, which might extend towards your ear or temple. This type of pain is muscular or joint-related, not directly from the treated tooth itself, although it can sometimes feel like it’s related. The discomfort usually resolves within a day or two as the strained muscles recover. Gentle jaw exercises (like slowly opening and closing your mouth) and warm compresses applied externally to the jaw area can help alleviate this type of soreness. While mild jaw discomfort is normal, severe jaw pain, difficulty opening your mouth widely, or clicking/locking noises in the jaw joint might warrant mentioning to your dentist, particularly if they persist or worsen significantly.
What to Do and What Not to Do After Root Canal Treatment
Successfully navigating the period immediately following a root canal procedure isn’t just about managing pain; it’s also about taking proactive steps to promote healing and avoid complications that could jeopardize the tooth or lead to further issues. Your actions in the first few days and weeks are crucial. Following your dentist’s specific post-operative instructions is paramount, as they are tailored to your individual procedure and overall health. However, there are general guidelines – important do’s and don’ts – that apply broadly to most patients undergoing a root canal. Adhering to these simple rules can significantly improve your comfort level during recovery, help ensure the tooth heals properly, and protect the temporary restoration until the final crown or filling is placed. Think of this as the essential roadmap for the immediate aftermath, designed to smooth your path back to full function and comfort.
What are the do’s and don’ts after a root canal?
To ensure a smooth recovery and protect your newly treated tooth, keep these essential do’s and don’ts in mind:
**DO:**
-
- **Take Medication as Directed:** Absolutely follow your dentist’s instructions for pain relievers and any prescribed antibiotics. Take pain medication *before* the local anesthetic wears off if advised.
-
- **Use Cold Compress:** Apply ice packs wrapped in cloth to the outside of your cheek intermittently for the first 24-48 hours to help reduce swelling.
-
- **Eat Soft Foods:** Stick to a soft diet for the first few days. This minimizes chewing pressure on the treated tooth. Examples include soups, yogurt, smoothies, mashed potatoes, pasta, scrambled eggs.
-
- **Chew on the Opposite Side:** Whenever possible, chew your food on the side of your mouth opposite the treated tooth, especially until the permanent restoration is placed.
-
- **Maintain Good Oral Hygiene:** Gently brush and floss around the treated tooth to keep the area clean. Be careful not to dislodge the temporary filling. Rinsing with warm salt water (a teaspoon of salt in a glass of warm water) several times a day can also help keep the area clean and promote gum healing.
-
- **Contact Your Dentist if Needed:** Don’t hesitate to call your dental office if you experience severe pain, uncontrolled swelling, fever, a bad taste/discharge, or if your temporary filling comes out completely.
-
- **Attend Follow-Up Appointments:** It is absolutely critical to return to your dentist to have the permanent filling or crown placed on the tooth as soon as recommended. The temporary filling is not designed to provide a long-term, bacteria-proof seal, and delaying the permanent restoration significantly increases the risk of re-infection and failure.
- **Rest:** Give your body time to recover.
**DON’T:**
-
- **Chew or bite heavily on the treated tooth:** Especially until the permanent restoration is in place. Temporary fillings are not strong enough for normal chewing forces and can break or dislodge, leading to leakage and re-infection.
-
- **Eat Hard, Crunchy, or Sticky Foods:** These can break the temporary filling or get stuck around the tooth, causing irritation or damage. Avoid nuts, popcorn, hard candy, chewing gum, caramels.
-
- **Smoke:** Smoking impairs blood flow and significantly delays healing. Avoid smoking during the recovery period.
-
- **Consume Hot Beverages Immediately:** Allow the anesthetic to wear off completely before consuming hot drinks to avoid accidental burns.
-
- **Ignore Worsening Symptoms:** If pain increases significantly after the first few days, or if swelling, fever, or discharge appear, do not assume it will get better on its own. These are signs that require professional attention.
- **Skip Your Permanent Restoration Appointment:** This is arguably one of the biggest “don’ts.” Leaving a temporary filling in place for too long is a primary cause of root canal failure due to leakage and re-infection.
How do I know if my root canal is healing?
Monitoring your symptoms and sensations can give you a good indication of whether the healing process is progressing as expected after a root canal. While healing happens internally (within the bone and ligament), the outward signs of successful recovery are often noticeable. Here’s what to look for as positive indicators that your root canal is healing well:
-
- **Gradual Decrease in Pain and Sensitivity:** The most obvious sign. The discomfort you felt immediately after the procedure should steadily lessen each day. You should need less and less pain medication over the first few days and weeks. Sensitivity to pressure or biting should also decrease over time.
-
- **Return to Normal Function:** As the tooth heals and is eventually restored with a permanent crown or filling, you should gradually be able to return to using the tooth for normal chewing without pain or significant discomfort. This return to function is a strong sign of healing.
-
- **Lack of Swelling or Other Concerning Symptoms:** The absence of red flags like increasing swelling, fever, pus, or worsening pain is a positive indicator. If these symptoms were present before the root canal (due to infection), their complete resolution confirms that the infection has been successfully addressed and healing is underway.
-
- **Improved Feeling in the Area:** While the tooth itself may feel slightly different, the general sensation in your jaw and surrounding tissues should return to normal. Any initial muscle soreness from keeping your mouth open should also resolve.
- **Radiographic Evidence (Later):** The ultimate confirmation of healing, especially if there was an infection at the root tip (periapical lesion), comes from follow-up X-rays taken by your dentist months later (e.g., at 6 months or a year). These X-rays will show evidence of bone regeneration and healing around the root tip. You won’t be able to see this yourself, but your dentist will monitor it.
Essentially, healing means a progressive reduction in symptoms and a return towards a pain-free, functional state for the tooth. If your symptoms are consistently improving and you don’t develop any of the “not normal” signs, you are likely healing well.
Frequently Asked Questions About ‘root canal and pain after’
Navigating the aftermath of a root canal can bring up a cascade of questions, fueled by personal experience, online searches, and maybe a touch of dental anxiety. It’s natural to wonder if what you’re feeling is “right” or if something is amiss. To wrap things up and provide quick clarity on the most common concerns, let’s address the key questions that frequently pop up when people are dealing with pain and recovery after a root canal. These are the headlines of uncertainty, and we’ll provide concise answers to put your mind at ease – or prompt you to call your dentist if necessary.
Is it Normal to Feel Pain After a Root Canal?
Yes, it is very normal and expected to feel some degree of pain, discomfort, or tenderness after a root canal. This is primarily due to the inflammation of the surrounding tissues (periodontal ligament and bone) as they heal from the procedure itself, not the original nerve pain inside the tooth. The pain is typically mild to moderate and manageable with over-the-counter pain relief.
How long does pain last after a root canal?
Acute pain or significant discomfort usually lasts for 1 to 3 days, peaking within the first 24-48 hours and then gradually improving. Mild sensitivity, especially when biting or touching the tooth, might linger for up to a week or two as the surrounding tissues continue to settle down. The tooth might feel “different” for a longer period, but sharp or severe pain should resolve relatively quickly.
What Causes Pain After A Root Canal?
Pain after a root canal is primarily caused by inflammation in the tissues surrounding the tooth root (the periodontal ligament and jawbone) due to the manipulation during the procedure. Other causes can include pressure from a high temporary filling, residual bacteria in the surrounding bone, or muscle soreness from keeping your mouth open. It is *not* caused by the nerve inside the tooth, as that is removed.
What is the best pain relief after a root canal?
Often, a combination of over-the-counter NSAIDs (like ibuprofen) and acetaminophen is recommended and highly effective for managing post-root canal pain by reducing inflammation and blocking pain signals. Your dentist may prescribe stronger medication for severe pain. Always follow your dentist’s specific dosage and timing instructions. Using cold compresses externally can also provide relief.
What is not normal after a root canal?
Signs that are *not* normal after a root canal and require contacting your dentist immediately include severe pain that isn’t controlled by medication, significant or increasing swelling (especially on the face), fever, pus or discharge from the gum near the tooth, or pain that significantly worsens after the first few days instead of improving. These symptoms could indicate a complication or infection needing prompt attention.