Key Takeaways
-
- PRF Treatment is a natural, autologous therapy using your body’s own blood to stimulate healing and regeneration.
-
- It works by concentrating platelets, leukocytes, and growth factors within a fibrin matrix, providing a *sustained release* of regenerative signals.
-
- Key benefits include improved skin texture and tone, reduction in fine lines and scars, natural hair growth stimulation, and accelerated healing in medical contexts.
-
- PRF is considered **very safe** due to its autologous nature, with minimal, temporary side effects like swelling and bruising related to the injection process.
-
- The **cost** of PRF treatment varies significantly based on the treatment area and the number of sessions needed, typically ranging from $500 to $2,500+ per session, with a series often recommended.
-
- **Results** are gradual, appearing over weeks and months, and are long-lasting but generally require a series of treatments (commonly 3-4) and periodic maintenance to sustain optimal improvement.
- PRF is particularly effective for rejuvenating delicate areas like the under-eyes and stimulating hair follicles in the scalp.
What is Platelet Rich Fibrin (PRF) Treatment and What Does it Entail?
At its heart, Platelet-Rich Fibrin (PRF) treatment is a revolutionary approach that taps directly into your body’s inherent capacity for repair and regeneration. It begins with the most fundamental component: your own blood. Unlike some synthetic treatments that introduce external agents, PRF therapy is entirely autologous, meaning it uses substances derived directly from you. This fact alone immediately elevates its safety profile, drastically reducing the risk of allergic reactions or rejection, as your body readily recognises and accepts its own biological materials. The procedure itself is elegantly simple, yet profoundly effective in concept. It starts with a small sample of your blood being drawn, much like a standard blood test – typically just a few vials, a volume that is quickly and effortlessly replaced by your system. This blood is then placed into a specialised centrifuge. Now, here’s where the magic of modern science meets natural biology. The centrifuge spins the blood at a specific speed and duration, carefully calculated to separate the different components based on their density. Red blood cells settle at the bottom, the clear plasma rises to the top, and in between lies a crucial layer: the buffy coat, rich in white blood cells and platelets, suspended within a fibrin matrix. This is our gold – the Platelet Rich Fibrin. The key difference between PRF and its predecessor, Platelet-Rich Plasma (PRP), lies precisely in this processing and the resultant composition. PRF is typically prepared using slower centrifugation speeds, which keeps the fibrin network largely intact and allows for the inclusion of beneficial leukocytes (white blood cells) and stem cells that are often filtered out or less concentrated in PRP. The fibrin forms a natural, jelly-like scaffold, trapping the platelets and growth factors and enabling their sustained, slow release over days or even weeks, rather than the rapid burst seen with PRP. This prolonged release is thought to provide a more potent and enduring stimulus for tissue regeneration. Once the PRF is extracted, often in a jelly-like or liquid form depending on the preparation method and intended use, it is ready for application. This is where common terms like PRF injections and Platelet Rich Fibrin therapy come into play, describing the method of delivering this powerful substance directly to the target area. These applications are remarkably diverse, spanning aesthetic concerns like facial rejuvenation, scar revision, and hair loss, to medical uses in wound healing, bone grafting, and musculoskeletal injuries. The PRF treatment procedure is generally straightforward and minimally invasive. After the blood draw and centrifugation (which takes mere minutes), the prepared PRF is applied topically (often alongside treatments like microneedling), or, more commonly, precisely injected into the tissue requiring regeneration. The entire process, from blood draw to application, is typically completed within an hour, making it a convenient option for many patients. This guide is designed to illuminate every facet of this journey, covering all the important things you need to know about The PRF Treatment, from the science underpinning its efficacy to the practical realities of undergoing the procedure and what results you might anticipate. It’s a testament to the body’s incredible ability to heal, amplified and directed with modern clinical technique. While we won’t delve into specific endorsements, it’s worth noting that leading practices across the globe, from reputable dermatology clinics like Pure Dermatology and Deschutes Dermatology to aesthetic centres such as Savalia Plastic Surgery, Beauti Pharm Med Spa, SkinCeuticals SkinLab, Blue Harbor Dermatology, and Care Esthetics, are increasingly offering and refining PRF treatments, a clear indicator of its growing recognition and effectiveness within the professional medical community.
What is Platelet Rich Fibrin (PRF) Therapy?
Platelet Rich Fibrin (PRF) Therapy is essentially a biomedical treatment protocol that harnesses the profound healing and regenerative potential inherently present within a patient’s own circulatory system. The fundamental concept revolves around the isolation and concentrated deployment of specific components of your blood – primarily platelets, but crucially, also including leukocytes (various types of white blood cells) and, in some formulations, circulating stem cells – within a natural fibrin matrix. This matrix is the key differentiator from earlier therapies like Platelet-Rich Plasma (PRP). In essence, you are becoming your own donor, leveraging your body’s sophisticated repair mechanisms to address issues ranging from aesthetic concerns like aging skin or hair thinning to medical needs such as accelerating the healing of wounds or aiding tissue repair following surgical procedures. The process begins with a venipuncture, a standard blood draw performed by a trained medical professional. The volume of blood collected is relatively small, typically anywhere from 10ml to 40ml, depending on the specific treatment area and protocol being followed. This blood is collected in specialized tubes, and critically, these tubes generally do not contain an anticoagulant, or contain very minimal amounts, which is a departure from the PRP preparation method. This absence or minimal use of anticoagulants allows the natural clotting process to be initiated during centrifugation. The collected blood is then immediately placed into a calibrated centrifuge and spun at a relatively low speed compared to PRP preparation, and usually for a shorter duration. This specific centrifugation protocol is designed to keep the various blood components from stratifying too aggressively. Instead of yielding a clear plasma layer and a distinct PRP layer, this method results in a more robust fibrin clot forming at the top of the tube, above the red blood cells. This clot, the Platelet Rich Fibrin, is dense with platelets, which are tiny, disc-shaped cell fragments vital for clotting and packed with potent growth factors – signaling molecules that orchestrate cellular activity, proliferation, and differentiation. However, PRF is more than just concentrated platelets. The slower spin allows for a significant inclusion of leukocytes, particularly neutrophils and lymphocytes, which play critical roles in regulating inflammation, fighting infection, and modulating the immune response, further contributing to tissue regeneration and remodelling. Moreover, the fibrin network itself forms a dynamic scaffold. Unlike the liquid nature of PRP, the PRF clot slowly degrades over several days to weeks in situ (at the injection site), releasing the trapped growth factors and cells gradually. This sustained release is thought to provide a more prolonged and effective stimulus for healing, collagen production, and the formation of new blood vessels (angiogenesis), which is crucial for tissue nourishment and vitality. Thus, PRF Therapy represents an evolution in using autologous blood products, offering a potent, naturally delivered cocktail of regenerative elements encapsulated within a biologically active matrix.
What Are Platelet-Rich Fibrin Injections?
Platelet-Rich Fibrin Injections represent the most common and direct method of delivering the powerful regenerative components isolated through PRF processing into specific target tissues or areas requiring focused rejuvenation or repair. Once the patient’s blood has been drawn and carefully centrifuged according to the precise PRF protocol, the resulting Platelet Rich Fibrin clot, which often presents as a viscous gel or a more liquid form depending on the technique and desired application (sometimes referred to as injectable PRF or Liquid PRF), is extracted from the centrifuge tube. This extracted PRF is then loaded into fine needles or cannulas, specialized thin tubes used for injecting substances into the body. The practitioner then strategically injects the PRF into the treatment area. The key advantage of using injections as the delivery method is the ability to place the regenerative material precisely where it is needed most. For example, in aesthetic treatments, PRF might be injected directly into fine lines and wrinkles on the face, beneath the delicate under-eye skin to address hollowness or dark circles, into areas of volume loss, or directly into the scalp to stimulate dormant hair follicles. In orthopaedic or sports medicine, it might be injected into damaged joints, ligaments, or tendons. The injection process itself is generally well-tolerated. While there might be some mild discomfort associated with needle sticks, practitioners often use topical numbing creams or local anaesthesia, especially in more sensitive areas, to ensure patient comfort. The injections are typically performed with a series of small, precise placements across the treatment zone. The volume injected per area is usually quite small, ensuring even distribution of the PRF’s growth factors and cellular components throughout the target tissue. Once injected, the fibrin matrix begins its work. It acts as a natural scaffold, providing structural support to the surrounding tissues while simultaneously releasing the encapsulated growth factors and cells gradually over time. This slow, sustained release mechanism, inherent to PRF’s fibrin structure, is believed to be more effective at promoting long-term tissue regeneration compared to the more rapid release characteristic of PRP. The injections stimulate the body’s natural healing cascade, encouraging fibroblasts to produce collagen and elastin (the building blocks of healthy skin), promoting angiogenesis (the formation of new blood vessels), and recruiting other regenerative cells to the area. Thus, Platelet-Rich Fibrin Injections are not just a simple delivery system; they are a targeted intervention that directs the body’s own potent repair mechanisms to specific sites, facilitating cellular renewal, tissue remodeling, and ultimately, leading to improvements in texture, tone, volume, and function over time, providing a highly personalised and biologically compatible therapeutic approach.
What is PRF?
PRF stands for Platelet-Rich Fibrin. It is an advanced, second-generation concentrate derived from a patient’s own blood, specifically engineered to stimulate and accelerate tissue healing and regeneration through the concentrated delivery of growth factors and cellular components within a natural fibrin matrix. Think of it as an amplified version of your body’s natural healing response. When you get a cut, your body initiates a complex process involving platelets, white blood cells, and fibrin to stop bleeding and begin repair. PRF takes these key players, concentrates them, and provides them in a format that sustains their activity over a longer period. The process involves drawing a small sample of the patient’s blood and placing it in a centrifuge. However, unlike the preparation of Platelet-Rich Plasma (PRP), which involves a faster spin and often the addition of an anticoagulant, PRF protocols typically use a lower centrifugation speed and no or minimal anticoagulant. This specific, gentler processing is crucial because it allows the formation of a robust, three-dimensional fibrin scaffold or clot. This fibrin matrix is not just passive; it’s biologically active, acting like a natural, biodegradable gel that traps the key cellular components. These key components are, primarily, platelets – the tiny, cell-like fragments (they aren’t technically full cells as they lack a nucleus) that are absolutely packed with alpha granules containing a multitude of growth factors. These growth factors are essentially signaling proteins – the chemical messengers that tell other cells in the body how to behave. We’re talking about potent molecules like Platelet-Derived Growth Factor (PDGF), Transforming Growth Factor Beta (TGF-β), Vascular Endothelial Growth Factor (VEGF), Epidermal Growth Factor (EGF), and Fibroblast Growth Factor (FGF), among others. These growth factors are the architects of tissue repair, promoting cell proliferation, migration, and differentiation; stimulating collagen and elastin synthesis; and driving the formation of new blood vessels. What makes PRF particularly powerful is that, within the fibrin matrix, these growth factors are released slowly over a period of 7 to 14 days or more as the fibrin scaffold gradually degrades. This sustained release provides a prolonged stimulus to the target tissue, which is believed to enhance the overall regenerative outcome compared to the rapid, burst release characteristic of liquid PRP. Furthermore, PRF preparations also include a significant concentration of leukocytes (various types of white blood cells, such as neutrophils, lymphocytes, and monocytes) and circulating stem cells, which are also trapped within the fibrin clot. These additional cellular components contribute significantly to the regenerative process. Leukocytes help modulate the inflammatory response, fight potential infections, and release additional growth factors and cytokines that further support healing and tissue remodelling. Circulating stem cells, though present in smaller numbers, possess the potential to differentiate into various cell types, providing a source of new cells for tissue repair. In summary, PRF is a potent, naturally derived biomaterial comprising concentrated platelets, leukocytes, and stem cells embedded within a slow-resorbing fibrin matrix, all working synergistically to trigger and sustain a powerful regenerative response in the tissue where it is applied.
What is Platelet-Rich Fibrin?
Platelet-Rich Fibrin is best understood as a sophisticated, biocompatible biomaterial derived from a patient’s own blood, uniquely characterized by its three-dimensional fibrin scaffold that encapsulates and provides a sustained release of vital growth factors and cellular components. Unlike Platelet-Rich Plasma (PRP), which is a liquid concentrate of platelets suspended in plasma, PRF leverages the body’s natural clotting process to create a robust fibrin matrix. This matrix is formed when the patient’s blood, collected in tubes without or with minimal anticoagulants, is centrifuged at lower speeds for a shorter duration than typically used for PRP. This specific centrifugation protocol allows the fibrinogen molecules naturally present in the plasma to polymerize and form a complex, spongy, gel-like network – the fibrin clot. This intricate network serves as a natural biological scaffold, providing structural support to the healing tissue where the PRF is placed or injected. More importantly, this fibrin structure acts as a reservoir, physically trapping a significantly higher concentration of platelets, leukocytes (white blood cells), and circulating stem cells compared to what is typically found in PRP. The platelets, as mentioned, are powerhouses of growth factors. Within the protective embrace of the fibrin matrix, these growth factors are not immediately released in a rapid burst, as can happen with liquid PRP. Instead, as the fibrin matrix slowly, gradually degrades over several days or weeks in situ – essentially dissolving naturally within the body’s tissues – it releases the trapped growth factors and signaling molecules in a controlled, sustained manner. This prolonged release profile is considered a key advantage of PRF, providing a more enduring stimulus to the cellular activity required for tissue regeneration, collagen synthesis, angiogenesis (new blood vessel formation), and overall tissue repair. The presence of leukocytes, particularly neutrophils, lymphocytes, and monocytes, is another critical distinction of PRF. These white blood cells are integral to the early inflammatory phase of wound healing, which is a necessary precursor to regeneration. They help clear debris, fight potential infection, and release additional cytokines and growth factors that modulate the regenerative response. The inclusion of these inflammatory and immune cells within the PRF clot contributes to a more holistic and potentially more effective healing environment. Furthermore, the fibrin matrix itself can act as a guide for cellular migration, providing a framework along which cells like fibroblasts and endothelial cells can move and proliferate, facilitating the formation of new tissue and blood vessels. In essence, Platelet-Rich Fibrin is a dynamic, autologous biological dressing or filler, offering a unique combination of mechanical support and sustained delivery of potent regenerative factors, making it a highly effective tool in aesthetic medicine, wound healing, and various other regenerative applications where encouraging the body’s natural repair processes is the primary goal. Its composition, rich in a concentrated blend of platelets, leukocytes, and stem cells held within a natural fibrin matrix, sets it apart and contributes to its increasing popularity as a powerful regenerative treatment.
Platelet-Rich Fibrin (PRF) Treatments
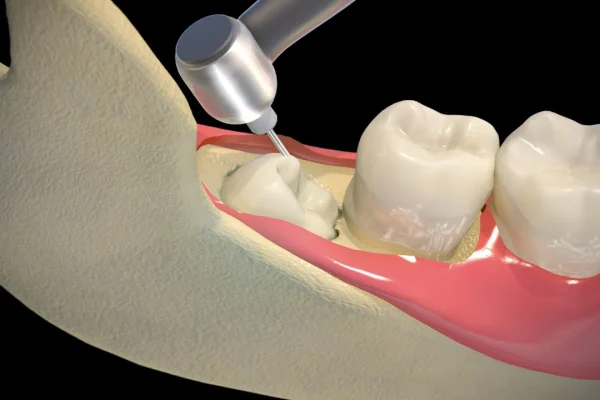
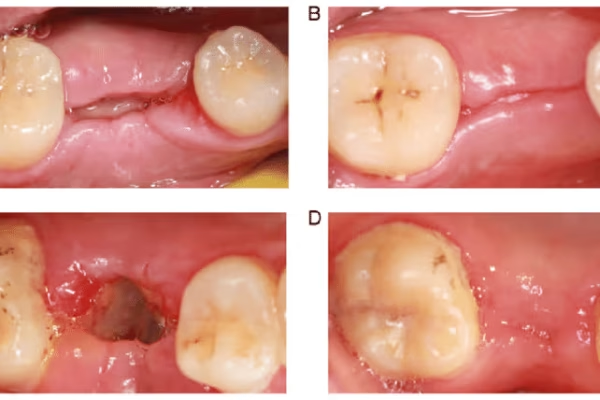
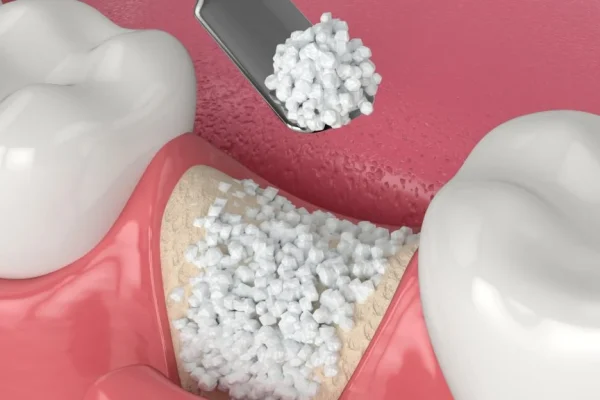
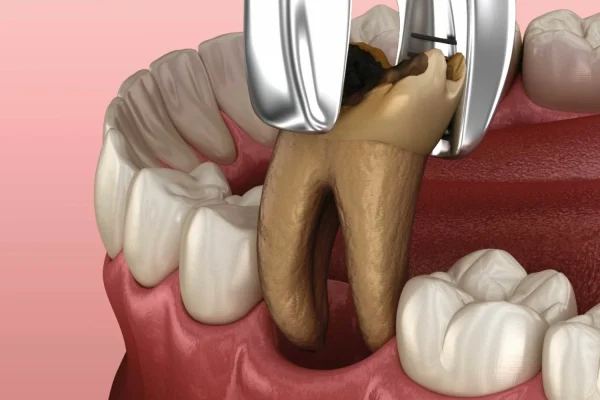
Platelet-Rich Fibrin (PRF) treatments encompass a broad and rapidly expanding spectrum of clinical applications that leverage the regenerative power of this autologous blood concentrate. At its core, any procedure that utilizes PRF to stimulate healing, tissue regeneration, or aesthetic improvement falls under this umbrella. The versatility of PRF stems from its rich composition – concentrated platelets, growth factors, leukocytes, and stem cells embedded within a supportive fibrin scaffold – and its ability to be prepared in various forms, from a viscous liquid to a more gel-like consistency, allowing for different methods of application. In the realm of aesthetic medicine, PRF treatments are particularly popular. They are widely used for facial rejuvenation, addressing concerns such as fine lines and wrinkles (especially around the eyes and mouth), improving skin texture and tone, reducing pore size, and restoring a youthful glow. PRF injections are frequently employed to treat delicate areas like the under-eyes, where the natural, subtle volume restoration and regenerative effects can significantly improve dark circles and hollowness. It’s also used to enhance the results of treatments like microneedling, either applied topically after the procedure or injected simultaneously, boosting collagen production and accelerating healing. Scar revision, including acne scars, is another common aesthetic application, where PRF helps remodel tissue and improve the appearance of depressed or textured scars. Furthermore, PRF has shown significant promise in stimulating hair growth in individuals experiencing hair thinning or loss, with injections delivered directly into the scalp to revitalise dormant or miniaturized hair follicles. Beyond aesthetics, PRF has well-established uses in various medical and surgical fields. In dentistry and oral surgery, it is routinely used to promote bone and tissue regeneration following tooth extractions, dental implant placement, or periodontal procedures. The fibrin scaffold helps stabilise grafts and accelerates healing. In orthopaedics and sports medicine, PRF is employed to aid in the recovery from musculoskeletal injuries, including tendon and ligament tears, joint pain (such as osteoarthritis), and muscle injuries, by injecting it into the affected area to reduce inflammation and stimulate tissue repair. Dermatologists and wound care specialists utilise PRF to accelerate the healing of chronic wounds, ulcers, and burns that are slow to respond to conventional treatments, providing a biological environment conducive to rapid tissue closure and regeneration. The specific preparation method, concentration, and volume of PRF used, as well as the technique of application (injection, topical application, or placement of a solid clot), are tailored to the specific condition being treated and the desired outcome. Whether used independently or in conjunction with other therapies, Platelet-Rich Fibrin treatments represent a powerful tool in the modern medical and aesthetic landscape, capitalising on the body’s intrinsic healing capabilities to achieve natural and lasting results across a diverse range of regenerative applications.
Platelet-Rich Fibrin (PRF) Treatment
A Platelet-Rich Fibrin (PRF) Treatment embodies a therapeutic philosophy deeply rooted in the principles of regenerative medicine, focusing on stimulating the body’s intrinsic healing and rejuvenation processes using its own biological materials. The fundamental idea is elegantly simple yet profoundly effective: instead of introducing synthetic substances or relying solely on external stimuli, PRF therapy concentrates and delivers the very elements your body naturally uses to repair damage and build new tissue. The treatment leverages the potent cocktail of growth factors, cytokines, platelets, white blood cells, and stem cells found in a patient’s blood, packaging them within a biocompatible fibrin matrix that ensures their slow and sustained release at the site of treatment. This autologous nature – meaning derived from the patient themselves – is a cornerstone of PRF treatment, offering an exceptional safety profile by virtually eliminating the risk of allergic reactions, immune rejection, or transmission of diseases. The journey through a PRF treatment typically begins with a detailed consultation with a qualified practitioner. This initial step is crucial for assessing the patient’s specific concerns, medical history, and overall health to determine if they are a suitable candidate for PRF therapy. Once candidacy is established and the treatment plan is agreed upon, the procedure can commence. The core of the treatment involves drawing a small volume of the patient’s blood, which is then immediately processed in a specialised centrifuge. The centrifugation parameters (speed, time, and often temperature) are critical and vary depending on the specific type of PRF being prepared (e.g., Solid PRF, Liquid PRF, Injectable PRF, etc.), each designed to optimise the concentration and retention of key cellular and protein components within the fibrin matrix. The resulting PRF product, whether a solid membrane, a gel, or a liquid, is then carefully collected by the practitioner. The method of application depends entirely on the treatment area and desired outcome. For skin rejuvenation, PRF is often injected directly into the dermis or applied topically after procedures like microneedling. For hair restoration, it’s injected into the scalp. For orthopaedic issues, it’s injected into joints or soft tissues. For wound healing, a PRF membrane or gel might be applied directly to the wound bed. The duration of the procedure itself, from blood draw to final application, is typically quite short, often ranging from 30 to 60 minutes, making it a relatively convenient option. The regenerative process stimulated by PRF is not instantaneous; it unfolds over time as the growth factors and cells signal and orchestrate cellular activity, collagen production, and angiogenesis. Patients are often advised that a series of treatments may be necessary to achieve optimal and sustained results, with the number and frequency tailored to their individual needs and the specific condition being addressed. Ultimately, Platelet-Rich Fibrin Treatment represents a powerful, natural, and versatile approach to regeneration and aesthetic enhancement, harnessing the body’s own healing machinery to promote tissue repair, improve skin quality, stimulate hair growth, and aid recovery across a multitude of applications, offering a compelling option for those seeking biologically compatible solutions.
The PRF Treatment Experience
Stepping into a clinic for a PRF treatment isn’t typically a daunting affair; it’s often framed as a relatively straightforward and comfortable experience, more akin to a specialised medical procedure than a major surgery. The atmosphere in clinics offering PRF, whether it’s a dedicated aesthetic practice or a medical clinic incorporating regenerative therapies, is usually professional, clean, and designed to put patients at ease. The journey invariably begins with a detailed consultation. This isn’t just a formality; it’s a crucial step where your practitioner will delve into your medical history, discuss your specific concerns (whether they’re aesthetic goals like reducing under-eye bags or targeting hair thinning, or medical needs like treating tendonitis), and thoroughly assess your overall health to confirm your suitability for PRF. They will explain the procedure in detail, answer any questions you may have, discuss realistic expectations regarding results and timelines, and outline the proposed treatment plan, including the number of sessions recommended. This consultative phase is vital for ensuring you feel informed, comfortable, and confident moving forward. When it’s time for the treatment itself, the process typically unfolds in a few key stages. It starts with a blood draw. A trained phlebotomist or medical professional will draw a small amount of your blood, usually from a vein in your arm, just like a standard blood test. The amount needed is surprisingly small, typically 1 to 4 vials. This part is usually very quick and causes minimal discomfort, perhaps just a slight pinch or pressure. Immediately after the blood draw, the tubes containing your blood are placed into a specialised centrifuge. This machine spins at precise speeds and durations, separating your blood into its constituent layers. This centrifugation phase takes only a few minutes, during which you can simply relax. Once the centrifugation is complete, the practitioner will carefully retrieve the tubes. You’ll notice the blood has separated, and they will extract the Platelet Rich Fibrin layer – which might look like a golden-yellow gel or a reddish-tinged clot, depending on the preparation method – using a syringe or pipette. This is the potent regenerative material. The final stage is the application or injection of the PRF into the target area. Depending on the area being treated and your sensitivity, a topical numbing cream may be applied beforehand to minimise discomfort. For injections, the practitioner will use a fine needle or cannula to make precise placements. You might feel a slight pressure, a mild stinging, or pinching sensation with each injection, but significant pain is uncommon. If PRF is being applied topically after microneedling, it’s simply massaged into the treated skin. The entire procedure, from blood draw to completion, is often finished within 30 to 60 minutes. Afterward, you’ll receive specific aftercare instructions. While there’s typically minimal downtime, you might experience some temporary redness, swelling, bruising, or tenderness at the treatment sites, which usually subsides within a day or two. Most people can resume their normal activities relatively quickly. The PRF treatment experience is designed to be efficient, safe, and comfortable, harnessing your body’s own healing power in a targeted, clinical setting to initiate a natural process of regeneration.
PRF Procedure
The PRF procedure is a beautifully orchestrated sequence that transforms a small sample of your blood into a potent regenerative tool. It’s a multi-step process, yet surprisingly quick and relatively simple for the patient, typically completed within a single appointment. Let’s break it down:
Step 1: Consultation & Preparation: Before anything clinical happens, a thorough consultation is paramount. This is where the practitioner assesses your candidacy, discusses your goals (e.g., reducing under-eye circles, promoting hair growth, improving skin texture), explains the process in detail, and answers all your questions. Once you’re ready to proceed, you’ll be prepared for the treatment. This might involve cleansing the treatment area and, depending on sensitivity, applying a topical numbing cream to minimise discomfort during the injection phase. Staying well-hydrated in the days leading up to your appointment can also help facilitate an easier blood draw.
Step 2: The Blood Draw: This is the very first physical step. A trained medical professional will perform a standard venipuncture, typically drawing blood from a vein in your arm. The amount of blood required is surprisingly small, usually ranging from 10 ml to 40 ml in total, depending on the scope and area of the treatment. It feels just like having blood taken for a routine lab test – a quick pinch or poke, and then often just a sensation of pressure as the blood is collected into specialised PRF tubes. These tubes are often different from standard blood collection tubes, specifically designed to prevent clotting *too* quickly before centrifugation, or, more commonly in newer protocols, designed *without* anticoagulants to allow natural fibrin formation during processing.
Step 3: Centrifugation: Immediately after the blood is drawn, the tubes are placed into a calibrated centrifuge. This is a laboratory device that spins the tubes at very high speeds. For PRF preparation, unlike PRP, a specific protocol is used: lower speeds for a shorter duration. This is absolutely critical. The gentler spin allows the various components of the blood (red blood cells, white blood cells, platelets, plasma) to separate based on their density, but critically, it permits the fibrinogen in the plasma to polymerize and form a fibrin clot *within* the tube. This centrifuge step typically takes only about 5 to 15 minutes, depending on the specific protocol and equipment used.
Step 4: PRF Extraction: Once the centrifugation cycle is complete, the tubes are removed. You’ll see the blood separated into layers: red blood cells at the bottom, a layer of clear or yellowish plasma at the top, and a concentrated layer of PRF in between, often appearing as a yellowish or reddish clot or gel-like substance just above the red blood cells. The practitioner then carefully collects this valuable PRF layer. Depending on the desired consistency for the treatment (liquid PRF for injection into fine lines, or a more solid gel for under-eye volume), the PRF might be gently aspirated into syringes or manipulated into a membrane.
Step 5: Application or Injection: This is the final step where the prepared PRF is delivered to the target tissue. If treating fine lines, scars, or using it for hair restoration, the liquid PRF or PRF gel is precisely injected into the specific areas using very fine needles. The injection technique will vary depending on the depth and tissue layer being targeted (e.g., intradermal, subcutaneous). If used in conjunction with microneedling, the liquid PRF might be spread topically over the skin after the microneedling device has created micro-channels. For certain medical uses, a more solid PRF membrane might be placed directly onto a wound or surgical site.
The simplicity and relative quickness of the core PRF procedure (blood draw, spin, extraction, application) are significant advantages. It’s an in-office treatment with minimal downtime, allowing patients to integrate this powerful regenerative therapy into their schedules relatively easily, offering a highly accessible path to harnessing their body’s own healing potential.
What does a PRF treatment entail?
Understanding what a PRF treatment *entails* means grasping the complete scope of the experience, from the initial preparatory steps you might take at home to the sensations felt during the procedure itself and the immediate post-treatment period. It’s a holistic picture of the process, ensuring you arrive at your appointment feeling informed and knowing precisely what lies ahead. The journey doesn’t begin the moment you sit in the treatment chair; it often starts a day or two prior. Practitioners typically advise patients on preparatory steps to optimize the treatment’s effectiveness and their comfort. Staying well-hydrated is frequently recommended, as it can make the blood draw easier and quicker. Some clinics might suggest avoiding certain medications, like blood thinners or non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, for a short period before the treatment, as these can potentially increase bruising, although you should always consult your prescribing physician before stopping any prescribed medication. Arriving at the clinic well-rested and having eaten something light is also generally a good idea.
On the day of the treatment, upon arrival, you’ll likely complete any necessary paperwork and perhaps have a final brief consultation to reconfirm the treatment plan and address any last-minute questions. The core of the procedure then begins with the blood draw, as detailed previously. This is a routine step, quick and relatively painless for most people. The blood is immediately processed via centrifugation in a closed system, maintaining sterility and integrity. This step takes only a short time.
While the blood is spinning, the practitioner will prepare the treatment area. This involves cleansing the skin thoroughly to minimise any risk of infection. If injections are planned, especially in sensitive areas like the face or scalp, a topical numbing cream will be applied. This cream needs time to take effect, typically 15-30 minutes, during which you can relax. This is an important step that significantly enhances comfort during the injection phase.
Once the PRF has been extracted from the centrifuge and the numbing cream has done its job, the practitioner proceeds with the application. This is arguably the most precise part of the treatment. Using fine needles or cannulas, the practitioner will inject the liquid or gel-like PRF into the predetermined treatment zones. The technique will vary based on the area – shallow injections for skin texture, deeper for volume loss or scalp treatment. During injections, you might feel slight pressure, a mild pricking sensation, or occasionally a brief stinging, but severe pain is generally not expected, especially with numbing. If PRF is being applied topically after another procedure like microneedling, it is carefully spread over the treated skin.
Immediately following the procedure, the practitioner will provide you with specific aftercare instructions. These instructions are vital for ensuring proper healing and optimising results. They typically include advice on cleansing the treated area, avoiding strenuous exercise, direct sun exposure, swimming pools, and saunas for a short period, and recommendations on applying cool compresses if needed to reduce swelling or bruising. You’ll also be informed about what to expect in terms of immediate post-treatment appearance – redness, swelling, and mild bruising are common and temporary.
In summary, a PRF treatment entails a straightforward, in-office process that combines a simple blood draw and centrifugation with targeted application (most often injection) of the patient’s own concentrated regenerative factors. It involves minimal preparation, a relatively quick procedure time, and a brief recovery period with mild, transient side effects, making it a convenient and natural option for regenerative therapies.
What to Expect from a PRF Treatment
Setting realistic expectations is key when considering any medical or aesthetic procedure, and a PRF treatment is no exception. Understanding what the experience will be like, both during and immediately after, helps ensure comfort and satisfaction. First and foremost, you should expect a highly personalised approach. Your initial consultation will define the treatment areas and the specific type of PRF application best suited to your needs. The experience begins with a simple blood draw, similar to a routine blood test. This part is usually quick, involving just a slight pinch or pressure. If you tend to be nervous about needles, let your practitioner know – they are experienced in making this as comfortable as possible.
Following the blood draw, your blood will be processed in a centrifuge. This takes a short time, typically under 15 minutes. During this waiting period, you can relax. For treatments involving injections, the target area will be thoroughly cleansed, and a topical numbing cream will usually be applied. You should expect to feel some numbness or reduced sensation in the area as the cream takes effect, which greatly minimises discomfort during the injections themselves.
When the PRF is ready and the numbing is effective, the practitioner will perform the injections. You should expect to feel a series of small pricks as the needle enters the skin. You might also feel a sensation of pressure or fullness as the PRF is deposited beneath the surface. While not entirely painless, the discomfort is generally mild and brief, often described as tolerable stinging or pinching. The skill of the practitioner plays a significant role here; an experienced injector will work efficiently and use techniques like cannulas (blunt-tipped tubes) in certain areas to further reduce bruising and discomfort. The total time for the injections varies depending on the treatment area but is usually quick, often just 10-20 minutes.
Immediately after the injections, it’s entirely normal and expected to see some immediate changes in the treated area. You will likely experience redness, particularly in lighter skin tones, and some swelling. This swelling is due to the volume of the injected material and the initiation of the inflammatory phase of healing (which is a necessary and positive part of the PRF process). Mild bruising is also a common possibility at the injection sites. These immediate effects are temporary and typically subside within a few hours to a couple of days.
Regarding results, it’s crucial to manage expectations for timing. PRF stimulates a biological process of regeneration, which takes time. You will *not* see dramatic, immediate results like those you might get from hyaluronic acid fillers (although PRF can provide some subtle, temporary volume). Instead, expect a gradual improvement over weeks and months as collagen is rebuilt, new blood vessels form, and tissues regenerate. The regenerative effects continue long after the initial swelling resolves. Often, a series of treatments is recommended (typically 2-4 sessions spaced several weeks apart) to achieve optimal results, as the effects are cumulative.
A key feature to remember is the autologous nature of PRF – it is derived *entirely* from your own blood. This is why the risk of allergic reactions or rejection is minimal. You are using your body’s own healing power. Expect post-treatment care instructions to follow precisely to ensure the best outcome. In essence, expect a straightforward, relatively comfortable procedure with temporary immediate side effects and gradual, natural improvements over time, rooted in the powerful regenerative capabilities of your own biology.
Why Choose Care Esthetics For PRF Treatment?
When considering a Platelet-Rich Fibrin (PRF) treatment, the clinic and practitioner you choose are paramount to ensuring a safe, effective, and positive experience. While this section names a specific clinic (Care Esthetics, as listed in the prompt), the principles behind selecting a reputable provider apply universally, whether you’re considering Care Esthetics or any other clinic offering PRF therapy. The decision of where to have your PRF treatment should be based on several critical factors that speak to the quality of care, the expertise of the staff, and the overall patient experience.
Firstly, *expertise and experience* are non-negotiable. Look for clinics where the practitioners (doctors, nurses, physician assistants) have extensive training and experience specifically in performing PRF treatments. PRF preparation and injection techniques are nuanced and differ from other injectables. An experienced practitioner understands the precise centrifugation protocols required to yield optimal PRF, the correct techniques for extracting and handling the delicate fibrin matrix, and the anatomical knowledge necessary for safe and effective injection into different tissues (whether it’s the delicate under-eye area, the vascular scalp, or other facial regions). Ask about their training, how long they’ve been performing PRF, and how many treatments they’ve completed.
Secondly, the *quality of the equipment and supplies* is crucial. PRF treatment relies on specialised centrifugation machines and specific sterile collection tubes designed for PRF preparation. Reputable clinics invest in high-quality, medical-grade equipment that is properly maintained and calibrated to ensure consistent and biologically active PRF is produced every time. The use of sterile techniques throughout the blood draw, processing, and injection phases is also vital to prevent complications like infection.
Thirdly, consider the *clinic’s approach to patient care and safety*. A good clinic prioritises patient safety above all else. This means conducting thorough consultations to assess candidacy and potential contraindications, maintaining strict sterile protocols, and providing clear, comprehensive pre- and post-treatment instructions. They should also have protocols in place to manage any potential, albeit rare, side effects or complications. A clinic that offers robust support and is readily available to answer questions or address concerns after your treatment demonstrates a commitment to your well-being beyond the procedure itself.
Furthermore, the *consultation process* itself is a key indicator. A good practitioner will take the time to listen to your goals, explain the science and process of PRF clearly, show you before-and-after photos of their own patients (where available and appropriate), and help you form realistic expectations about the results and the number of sessions needed. They should also discuss the cost transparently. Avoid clinics that promise unrealistic results or heavily pressure you into treatment.
Finally, consider *patient reviews and testimonials*. While not the sole deciding factor, hearing about other patients’ experiences at a particular clinic can provide valuable insight into the level of care, the staff’s demeanor, and the satisfaction with results.
Choosing a provider for PRF treatment is an important decision. By focusing on clinics that demonstrate a commitment to expertise, use high-quality equipment, prioritise safety and patient care, and conduct thorough consultations, you significantly increase your chances of having a successful and positive PRF treatment experience, regardless of the specific name above the door.
How Does PRF Treatment Work to Promote Healing and Rejuvenation?
The science behind how PRF treatment promotes healing and rejuvenation is a fascinating interplay of biology, leveraging the body’s intrinsic repair mechanisms and amplifying them. At the core of this process is the recognition that healing is a cascade of complex events, initiated and guided by a symphony of signaling molecules. Platelets, these small, non-nucleated cell fragments circulating in our blood, are far more than just clotting agents; they are veritable storehouses of growth factors and cytokines, critical signalling proteins that are the master conductors of tissue regeneration. When an injury occurs, platelets are among the first responders. They aggregate at the site of damage, form a plug to stop bleeding, and, crucially, become activated, releasing the contents of their alpha granules. These granules contain a powerful cocktail of growth factors, such as Platelet-Derived Growth Factor (PDGF), which stimulates cell growth and proliferation; Transforming Growth Factor-beta (TGF-β), involved in cell differentiation and matrix formation; Vascular Endothelial Growth Factor (VEGF), a key player in stimulating the formation of new blood vessels (angiogenesis), essential for bringing oxygen and nutrients to the healing tissue; and Epidermal Growth Factor (EGF), which promotes epithelial cell growth and differentiation, vital for skin and tissue surface repair. In a standard injury, this release occurs as a relatively rapid burst. However, with PRF, this natural process is supercharged and sustained. The unique aspect of Platelet Rich Fibrin is the fibrin matrix itself. This naturally occurring protein network forms a stable, three-dimensional scaffold. When PRF is introduced into a treatment area, this fibrin clot integrates with the existing tissue, providing immediate structural support. But its role is far more dynamic. As the fibrin matrix slowly and naturally degrades over several days to weeks, it acts as a controlled-release delivery system. The concentrated platelets and leukocytes (white blood cells) trapped within this scaffold gradually release their payload of growth factors and cytokines into the surrounding tissue. This sustained delivery provides a prolonged stimulus to the local cells – including fibroblasts (responsible for producing collagen and elastin), endothelial cells (which form blood vessels), and resident stem cells – prompting them to proliferate, migrate to the site of need, and differentiate into the cell types required for repair and regeneration. Specifically, the biological mechanisms by which PRF works include stimulating fibroblast activity, leading to increased production of new collagen and elastin fibers, the foundational proteins that provide skin with structure, elasticity, and firmness. This process, known as neocollagenesis and neoelastogenesis, is key to improving skin texture, reducing fine lines and wrinkles, and restoring youthful volume. Furthermore, the rich concentration of VEGF and other angiogenic factors within PRF powerfully stimulates angiogenesis, the formation of new capillaries and blood vessels. This improved vascularity is crucial for delivering oxygen and nutrients to the healing tissue and removing waste products, supporting overall tissue health and vitality, which is particularly important in areas with poor circulation or for stimulating hair follicle activity. The inclusion of leukocytes in PRF also modulates the inflammatory response, ensuring it progresses appropriately from the necessary initial phase to resolution, promoting a healthy healing environment. In essence, PRF doesn’t just provide building blocks; it provides the instructions and fuel, delivered over time via the fibrin scaffold, telling the body’s cells how to repair, rebuild, and rejuvenate tissue in a highly coordinated and sustained manner, harnessing its own inherent biological intelligence for therapeutic gain.
HOW DO PRF INJECTIONS WORK?
PRF injections represent the direct and powerful application of the Platelet-Rich Fibrin biomaterial precisely where regenerative action is desired, amplifying and directing the body’s inherent healing capabilities to a specific site. When the PRF, typically in a liquid or gel-like consistency, is carefully injected into the target tissue – whether it’s the dermis of the skin, subcutaneous tissue, the scalp, or peri-articular areas – the body immediately recognizes this autologous material. The injected PRF forms a three-dimensional scaffold at the injection site due to its inherent fibrin structure. This scaffold is not just a passive filler (though it can provide some subtle, temporary volume, especially with PRF gel); it’s a biologically active matrix densely packed with concentrated platelets, leukocytes, and circulating stem cells. Upon injection, and as the fibrin begins to integrate with the surrounding tissue, the encapsulated platelets within the matrix become activated. This activation process triggers the release of a vast array of potent growth factors – including Platelet-Derived Growth Factor (PDGF), Transforming Growth Factor Beta (TGF-β), Vascular Endothelial Growth Factor (VEGF), Epidermal Growth Factor (EGF), Insulin-like Growth Factor (IGF), and Fibroblast Growth Factor (FGF). These growth factors are like tiny, powerful messengers. Once released, they bind to specific receptors on the surrounding cells – fibroblasts, keratinocytes, endothelial cells, stem cells, and others – initiating a cascade of biological events crucial for tissue repair and regeneration.
A key mechanism at the injection site is the stimulation of cellular proliferation. Growth factors signal local cells, particularly fibroblasts in the skin, to multiply, increasing the population of cells capable of producing new tissue components. Simultaneously, these factors encourage cellular migration, effectively calling in other regenerative cells from the surrounding tissue or bloodstream to the injection site to assist in the repair process. A primary goal, particularly in aesthetic applications, is stimulating neocollagenesis and neoelastogenesis. The released growth factors strongly encourage fibroblasts to synthesise new collagen and elastin fibers. Collagen provides structural integrity, while elastin provides elasticity and resilience. The formation of this new scaffolding helps to improve skin firmness, reduce laxity, smooth out fine lines and wrinkles, and improve overall skin texture and tone. Furthermore, the presence of VEGF and other angiogenic factors released from the PRF is critical for stimulating angiogenesis – the formation of new blood vessels. Improved vascularity at the injection site ensures that the actively regenerating tissue receives an adequate supply of oxygen, nutrients, and other healing factors, while also facilitating the removal of metabolic waste products. This enhanced blood flow is vital for long-term tissue health and is particularly relevant for applications like wound healing and hair restoration, where circulation is key.
What distinguishes PRF injections, especially compared to PRP, is the sustained release of these growth factors. The fibrin matrix doesn’t break down immediately; it slowly degrades over one to two weeks. This means the growth factors are released gradually over this period, providing a prolonged stimulus to the regenerative processes rather than a single, transient burst. This sustained signalling is thought to lead to more robust and longer-lasting tissue remodeling. Additionally, the leukocytes included in the PRF play a role in modulating inflammation, which is a necessary part of healing but needs to be controlled. They also contribute to the release of other cytokines and growth factors, further enhancing the regenerative environment.
In essence, PRF injections work by creating a micro-environment rich in concentrated regenerative factors and cells, held within a supportive, biodegradable fibrin scaffold, which provides a sustained biological signal that orchestrates local cells to repair, rebuild, and rejuvenate the targeted tissue from within, leading to natural, gradual, and potentially long-lasting improvements in the treated area.
How does PRF work?
The core mechanism by which Platelet Rich Fibrin (PRF) exerts its therapeutic effects lies in its ability to concentrate and deliver the body’s own powerful healing and regenerative components to a specific site, and crucially, to release these components in a slow, sustained manner. It’s a sophisticated biological process initiated by the simple act of preparing and applying or injecting the PRF. When blood is processed into PRF, the key players are isolated and concentrated: platelets, leukocytes (white blood cells), and circulating stem cells, all embedded within a natural fibrin matrix.
Once this PRF preparation is introduced into the desired tissue – whether it’s injected into the skin to address wrinkles, placed into a bone graft site, or applied topically to a wound – the natural biological cascade begins. The fibrin matrix, which forms a natural, three-dimensional scaffold, interacts with the surrounding tissue. This matrix is porous and provides an immediate framework. The platelets trapped within this matrix become activated upon contact with the tissue or as they are released from the slowly degrading fibrin. Upon activation, these platelets degranulate, releasing a concentrated cocktail of growth factors from their alpha granules. These growth factors, which include PDGF, TGF-β, VEGF, EGF, and others, are the primary signaling molecules that initiate and regulate the healing and regenerative response. They bind to receptors on local cells, triggering a cascade of intracellular events.
Specifically, these growth factors stimulate:
1. Cell Proliferation and Migration: They signal cells like fibroblasts (in skin), osteoblasts (in bone), and endothelial cells (in blood vessels) to multiply and move into the PRF-treated area, effectively recruiting the necessary workforce for tissue repair.
2. Matrix Synthesis: Growth factors, particularly TGF-β and PDGF, strongly stimulate fibroblasts to produce extracellular matrix components, most notably collagen and elastin in skin, which are vital for tissue structure, strength, and elasticity. This is a key mechanism for skin rejuvenation, leading to improved texture, tone, and reduced lines.
3. Angiogenesis: VEGF is a potent stimulator of new blood vessel formation. The creation of new capillaries is essential because they supply the regenerating tissue with oxygen and nutrients, which are critical for cellular survival and activity, and also help remove waste products. Improved blood flow is vital for healthy tissue and contributes to vitality and regeneration, such as in hair restoration applications.
4. Modulation of Inflammation: The leukocytes (white blood cells) present in PRF, such as neutrophils and macrophages, play a crucial role in the inflammatory phase of healing. While initial inflammation is necessary to clean up damaged tissue and signal repair, chronic inflammation can be detrimental. The leukocytes in PRF help to modulate this response, ensuring it is effective but controlled, and they also release cytokines that further support the regenerative process.
The most significant distinction of PRF’s mechanism compared to simpler platelet concentrates is the sustained release provided by the fibrin matrix. The fibrin doesn’t break down instantly; it takes 1-2 weeks to resorb. As it degrades, it continuously releases the trapped growth factors and cells. This prolonged exposure to a concentrated supply of regenerative signals provides a more enduring stimulus to the local cells, potentially leading to a more robust and sustained regenerative outcome over time compared to the more rapid, transient burst seen with liquid PRP. In essence, PRF creates a localized, biologically active environment that continuously ‘tells’ the tissue to heal, rebuild, and rejuvenate itself using its own inherent machinery.
What Are the Top Benefits of Platelet Rich Fibrin (PRF) Therapy?
Platelet Rich Fibrin (PRF) Therapy has garnered significant attention across various medical and aesthetic fields due to its numerous compelling advantages, stemming from its natural origin and powerful regenerative capabilities. Unlike treatments that rely on synthetic substances, PRF leverages your body’s own biological power, offering a uniquely biocompatible approach. The benefits experienced can vary depending on the specific application area, but some overarching advantages make PRF a highly attractive treatment option for a wide range of individuals and conditions. One of the most significant overarching benefits is its ability to stimulate genuine tissue regeneration and repair from within. It doesn’t just mask issues; it actively encourages the body to rebuild and rejuvenate damaged or aging tissues. This leads to natural-looking and potentially long-lasting improvements, as the changes are driven by your own cellular activity, creating new collagen, elastin, and blood vessels.
In aesthetic applications, the benefits are particularly striking. For skin rejuvenation, PRF therapy can lead to a noticeable improvement in skin texture and tone, making the skin smoother, more radiant, and healthier-looking. It effectively addresses concerns like fine lines and wrinkles, particularly around the eyes (crow’s feet) and mouth, by stimulating the production of new collagen and elastin, which plumps and firms the skin. PRF is also beneficial for improving the appearance of various types of scars, including acne scars and surgical scars, by promoting tissue remodelling. Furthermore, its ability to stimulate angiogenesis (new blood vessel formation) contributes to improved skin vitality and a youthful glow by enhancing circulation and delivering essential nutrients to the skin cells. Another major benefit in aesthetics is its potential to stimulate hair growth in individuals experiencing hair thinning or loss, offering a natural alternative or adjunct therapy to medical treatments by revitalising dormant hair follicles.
Beyond aesthetics, PRF provides significant benefits in accelerating healing across numerous medical disciplines. In oral surgery and periodontics, it aids in faster and more complete healing after extractions, bone grafting, and implant placement by providing a scaffold and growth factors that support bone and gum tissue regeneration. In orthopaedics, injecting PRF into injured tendons, ligaments, or joints can help reduce pain and inflammation, and importantly, stimulate the repair process of the damaged tissues, potentially accelerating recovery and improving function. For chronic wounds and ulcers that are slow to respond to conventional treatments, the application of PRF can provide the necessary biological signals and scaffold to restart the healing cascade, promoting tissue granulation and closure.
A key inherent benefit of PRF is its exceptional safety profile. Since it is derived entirely from the patient’s own blood, there is virtually no risk of allergic reactions, foreign body rejection, or transmission of infectious diseases. This makes it a very safe option for almost anyone who is a suitable candidate. The procedure is also minimally invasive, typically involving just a simple blood draw and targeted injections or application, resulting in minimal downtime compared to surgical interventions. Finally, the natural and gradual nature of the results is often perceived as a major benefit, avoiding the sometimes artificial look associated with synthetic fillers and instead achieving subtle, yet significant, improvements that appear entirely organic. These collective advantages position PRF therapy as a powerful, safe, and versatile tool for promoting healing and rejuvenation across a wide array of applications.
What Are the 6 Top Benefits of Platelet Rich Fibrin (PRF) Therapy?
Highlighting specific benefits helps clarify the powerful potential of Platelet Rich Fibrin (PRF) Therapy. While its applications are broad, certain key advantages consistently stand out as the most compelling reasons why individuals and practitioners are increasingly choosing this regenerative approach. Here are arguably the six top benefits you can expect from PRF therapy:
-
- Natural Tissue Regeneration & Remodelling: This is perhaps the most profound benefit. PRF doesn’t just add temporary volume or camouflage imperfections; it actively stimulates your body’s own cells – fibroblasts, osteoblasts, stem cells, etc. – to produce new, healthy tissue. This means generating new collagen, elastin, and extracellular matrix components, leading to genuine improvements in skin quality, structural integrity, and tissue health over time. For areas like fine lines or scars, this remodelling effect can lead to significant, lasting improvements in texture and appearance.
-
- Sustained Growth Factor Release: Thanks to its unique fibrin matrix structure, PRF provides a prolonged release of vital growth factors and cytokines over a period of 7-14 days as the clot gradually degrades. This sustained biological signalling offers a more enduring stimulus to the regenerative processes compared to the rapid burst delivery of growth factors seen with liquid PRP. This prolonged cellular ‘communication’ is thought to lead to more robust and potentially longer-lasting regenerative outcomes.
-
- Enhanced Healing & Recovery: Due to the concentrated growth factors, leukocytes, and the scaffolding effect of the fibrin matrix, PRF significantly accelerates the body’s natural healing processes. This benefit is widely utilised in medical fields (dentistry, orthopaedics, wound care) to speed up recovery time, reduce pain, and improve the quality of tissue repair following injury or surgery. In aesthetics, faster healing from associated procedures like microneedling or laser treatments is a welcome bonus.
-
- Improved Skin Texture, Tone, and Radiance: Through the stimulation of collagen and elastin synthesis and enhanced angiogenesis (new blood vessel formation), PRF therapy dramatically improves the overall quality of the skin. Patients often report skin that feels smoother, looks brighter, has a more even tone, and possesses a healthy, youthful radiance. The increased vascularity also contributes to better delivery of nutrients and oxygen to skin cells.
-
- Stimulation of Hair Growth: For individuals experiencing hair thinning or loss, PRF injections into the scalp offer a powerful, natural solution. The growth factors released from the PRF directly stimulate dormant or miniaturised hair follicles, promoting the transition from resting phase (telogen) to growth phase (anagen), increasing hair density, thickness, and vitality. This provides a non-surgical option or complement to other hair restoration methods.
- Exceptional Safety & Biocompatibility: Derived entirely from the patient’s own blood, PRF is 100% autologous. This inherent characteristic means there is virtually no risk of allergic reactions, immune rejection, or transmission of pathogens. This makes PRF an exceptionally safe treatment option suitable for a wide range of patients, including those who may be sensitive to synthetic fillers or other materials.
These six benefits underscore why PRF therapy is becoming a cornerstone in both regenerative medicine and aesthetic practices – offering natural, effective, and safe solutions powered by the body’s own remarkable healing abilities.
Benefits of PRF Injections
Focusing specifically on PRF injections allows us to highlight the unique advantages achieved through this targeted delivery method. While topical application of liquid PRF (often post-microneedling) has its place, the injection technique offers distinct benefits by precisely delivering the concentrated regenerative material into the specific tissue layer or location where it can exert maximum effect. The benefits of PRF injections are numerous and often more pronounced and targeted compared to surface applications because the material bypasses the skin barrier to reach deeper tissues or specific problem areas directly.
Firstly, Targeted Regeneration: Injections allow practitioners to place the PRF exactly where regeneration is needed – whether it’s injecting into a deep wrinkle, a specific area of volume loss (like under the eyes or in the cheeks), directly into scar tissue, or surrounding hair follicles on the scalp. This precision ensures that the high concentration of growth factors and cells is delivered precisely to the site requiring repair and rejuvenation, maximising the potential for results in that specific zone.
Secondly, Stimulation of Subcutaneous and Dermal Tissues: By injecting PRF into the dermis or subcutaneous layer, you directly stimulate the fibroblasts responsible for producing collagen and elastin deeper within the skin structure. This leads to more significant improvements in skin firmness, elasticity, and thickness over time, addressing concerns like skin laxity and fine lines more effectively than surface-level treatments alone.
Thirdly, Volume Improvement (especially with PRF Gel): While PRF is primarily regenerative, it can be processed into a gel-like consistency (often by heating Liquid PRF) which provides a subtle, natural volumizing effect. When injected, particularly in areas like the under-eyes, this PRF Gel can immediately fill hollows and simultaneously work to regenerate the tissue over time. This offers a two-fold benefit: immediate subtle volume correction and long-term regenerative improvements, which is distinct from standard liquid PRF used for general skin quality.
Fourthly, Enhanced Results in Specific Areas: Certain areas, like the delicate under-eyes, significantly benefit from targeted PRF injections. The ability to precisely place the PRF gel or liquid helps to improve dark circles, reduce puffiness, and stimulate new collagen to thicken the thin skin, leading to a brighter, more rested appearance that is often difficult to achieve with topical treatments. Similarly, injecting PRF directly into the scalp can lead to more direct and potent stimulation of hair follicles compared to topical application.
Fifthly, Improved Blood Supply (Angiogenesis): Injections allow for the direct delivery of angiogenic growth factors deep into the tissue, stimulating the formation of new blood vessels (angiogenesis) more effectively. This improved vascularity enhances tissue health, oxygenation, and nutrient supply, which is vital for long-term regeneration and the vitality of tissues like skin and hair follicles.
Finally, Synergy with the Natural Fibrin Scaffold: Once injected, the fibrin matrix within the PRF forms a natural scaffold that integrates with the surrounding tissue. This scaffold supports the cells and guides the regenerative process, while also ensuring the sustained, slow release of growth factors directly at the injection site, prolonging the therapeutic signal compared to systems lacking this matrix.
In summary, PRF injections leverage the power of targeted delivery to maximise the regenerative potential of Platelet Rich Fibrin, offering precise stimulation of specific tissues, facilitating volume improvement where needed, enhancing results in delicate or challenging areas, and promoting robust angiogenesis and tissue remodelling through the natural support and sustained release provided by the fibrin matrix.
Benefits of Platelet-Rich Fibrin (PRF) Injections
Let’s reiterate and expand upon the compelling reasons why Platelet-Rich Fibrin (PRF) injections are increasingly becoming a preferred option for various aesthetic and regenerative concerns. The act of injecting PRF harnesses the natural regenerative power contained within your own blood and directs it with pinpoint accuracy to where it is needed most, leading to a cascade of beneficial biological events. Here are some key benefits, building on our previous points:
-
- Holistic Tissue Rejuvenation: PRF injections initiate a comprehensive rejuvenation process within the treated tissues. Beyond stimulating collagen and elastin, the presence of leukocytes and stem cells within the PRF contributes to a more complete regenerative response, involving tissue remodelling, inflammation modulation, and potentially the recruitment of multi-potent cells to aid in repair. This leads to not just surface-level improvements but a deeper enhancement of tissue health and vitality.
-
- Improved Skin Quality and Elasticity: By directly stimulating fibroblasts in the dermis to produce new collagen and elastin, PRF injections can significantly improve the skin’s structural integrity. This translates into firmer, more supple skin, reduced appearance of fine lines and wrinkles, and improved overall texture and tone. The natural elasticity of the skin is enhanced, giving it a more youthful bounce and resilience.
-
- Reduction in Appearance of Scars and Stretch Marks: PRF injections can be highly effective in improving the appearance of various types of scars (acne scars, surgical scars) and stretch marks. The regenerative factors promote the remodelling of scar tissue, encouraging the production of healthier collagen and smoothing out textural irregularities, leading to a less noticeable and more integrated appearance of the scarred area.
-
- Natural and Gradual Results: One of the appealing aspects of PRF injections is that the results appear gradually and naturally over time. As the body responds to the regenerative signals and builds new tissue, the improvements are subtle initially and become more noticeable in the weeks and months following treatment. This avoids an abrupt or artificial change in appearance, leading to outcomes that look completely organic and refreshed, powered by your own biology.
-
- Longer-Lasting Effects Compared to Some Treatments: While not permanent, the regenerative effects stimulated by PRF injections can be quite long-lasting, often noticeable for 6-12 months or even longer after a series of treatments. Because the treatment encourages the growth of *new* tissue, rather than simply filling space, the improvements persist as long as the new tissue remains healthy. Maintenance treatments can help prolong these results.
-
- Compatibility with Other Treatments: PRF injections can be synergistically combined with other aesthetic procedures to enhance overall outcomes. For example, injecting PRF can boost the results of microneedling, laser treatments, or even complement dermal filler procedures by improving underlying skin quality while fillers provide structural volume. This compatibility allows for comprehensive treatment plans tailored to individual needs.
- Minimally Invasive with Low Downtime: Compared to surgical options for rejuvenation or repair, PRF injections are minimally invasive. The procedure involves only injections, requires no incisions, and typically has very little downtime. Most patients experience only temporary redness, swelling, or bruising that resolves within a day or two, allowing for a quick return to normal activities.
These compounded benefits solidify PRF injections as a powerful and natural choice for those seeking significant, yet natural-looking, improvements in skin quality, addressing scars, stimulating hair growth, and promoting healing across a variety of applications, all while offering an excellent safety profile due to its autologous nature.
How Much Does PRF Treatment Cost?
The cost of Platelet Rich Fibrin (PRF) treatment is a significant consideration for anyone exploring this option, and it’s important to understand that there isn’t a single, fixed price. The total investment for PRF therapy can vary quite widely depending on a multitude of factors, making it essential to get a personalised quote during your consultation with a practitioner. Several variables contribute to the overall cost, reflecting the complexity of the treatment, the resources involved, and the expertise of the provider.
Firstly, the treatment area is a primary determinant of cost. Treating a smaller, more focused area like the under-eyes or specific scars will generally cost less than treating a larger area like the full face, scalp for hair loss, or multiple joints. Larger treatment areas require more blood draw, more PRF yield, and more extensive application or injection time and technique.
Secondly, the number of sessions recommended in your treatment plan significantly impacts the total expense. PRF therapy is often delivered as a series of treatments to achieve optimal and cumulative results. While a single session might provide some benefit, most practitioners recommend a course of 2 to 4 treatments, spaced several weeks apart (typically 4-8 weeks). The total cost will be the sum of the cost per session, or clinics might offer package pricing for a series, which can sometimes be more cost-effective overall.
Thirdly, the clinic’s location and reputation play a role. Practices located in metropolitan areas or regions with a higher cost of living typically have higher overheads, which can translate to higher treatment prices. Similarly, highly reputable clinics with extensively trained and sought-after practitioners, who may have invested significantly in advanced equipment and staff training, might command higher fees for their expertise and perceived quality of care.
Fourthly, whether PRF is used as a standalone treatment or combined with other procedures will affect the cost. PRF is often used in conjunction with treatments like microneedling, laser therapy, or even dermal fillers. When combined, the total cost will be higher than either treatment individually, reflecting the added complexity, time, and materials used in the combination therapy, although the synergistic results may justify the increased investment.
Finally, the type of PRF preparation might also influence the cost slightly, depending on the kit and processing method used, though this is often bundled into the overall session price. More advanced forms, like injectable PRF gel requiring specific processing protocols, might sometimes be priced differently than basic liquid PRF used topically.
Considering these variables, the cost per PRF session can range from several hundred dollars to upwards of two thousand dollars or more, depending on the factors mentioned. A series of treatments can therefore represent a significant investment, potentially ranging from a couple of thousand dollars to five or six thousand dollars or more in total. It’s crucial to have a detailed discussion about pricing during your consultation, get a clear breakdown of costs, and understand what is included (e.g., consultation fee, numbing cream, follow-up). While cost is important, balancing it with the expertise of the provider and the quality of the materials used is essential for achieving safe and effective results. Don’t hesitate to ask about package deals for multiple sessions, as this is a common practice.
How much does PRF cost?
When you ask, “How much does PRF cost?” you’re looking for the bottom line, the financial investment required for a single treatment session of Platelet Rich Fibrin. As we’ve touched upon, giving a single number is challenging because the price is not uniform across the board. However, we can provide typical ranges and break down the factors that contribute to the final figure you’ll see quoted by clinics. Generally speaking, the cost for a single PRF treatment session in aesthetic or regenerative medicine applications can range significantly, from approximately $500 to $2,500 or even more per session. This wide range underscores the variability based on several key factors.
The primary driver of cost is the treatment area and its size and complexity. A treatment focused solely on rejuvenating the under-eyes, for instance, might fall towards the lower end or middle of this range. This area requires a relatively small amount of blood and PRF, and the injection time is less extensive than treating a larger surface. Conversely, a full-face treatment incorporating multiple injection sites or combining PRF with microneedling over the entire face will require a larger volume of blood to yield sufficient PRF, more time for application or injections across a broader area, and thus commands a higher price, potentially pushing into the upper end of the $1,500 – $2,500+ range per session. Treating the scalp for hair loss, especially if a large area is affected, can also be on the higher end due to the surface area and multiple injection points required to stimulate hair follicles across the entire zone of thinning.
Another factor is the type of PRF preparation being used. While the core process is similar, some techniques yield a more concentrated liquid PRF, while others might process it further into a ‘PRF Gel’ or matrix for volumising effects. The kits required for these different preparations can vary slightly in cost, and the technical skill involved in preparing and injecting these different forms might also influence pricing. For example, creating and injecting PRF Gel for under-eye filler might sometimes be priced differently than simply injecting liquid PRF for skin texture improvement.
The clinic’s overheads are also baked into the cost. This includes the rent for their facility, the cost of utilities, the salaries of their highly trained staff (practitioners, nurses, support staff), marketing expenses, and critically, the significant investment in medical-grade equipment like specialised centrifuges and sterile supplies. Clinics in prime urban locations or those with luxurious facilities will inherently have higher operating costs, which are reflected in their pricing.
Finally, the practitioner’s experience and reputation are valuable. A board-certified dermatologist, plastic surgeon, or other medical specialist with extensive experience and a strong track record in performing PRF treatments safely and effectively will typically charge more for their services than a less experienced provider. You are paying not just for the materials but for their medical expertise, aesthetic eye, and ability to deliver optimal results while minimising risks.
It’s also important to factor in that PRF is often recommended as a series. While a single session cost is what’s being asked here, the *total* cost of a successful treatment *plan* will involve multiple sessions. Always clarify with the clinic whether the quoted price is per session or for a package, and understand what is included in that price. This helps you budget effectively for the entire course of treatment needed to achieve your desired outcomes.
What is PRF cost?
To directly address the question “What is PRF cost?”, we are referring to the financial outlay for a single treatment session utilizing Platelet Rich Fibrin. As previously established, this cost is not a fixed sum but rather a variable figure influenced by a range of factors, primarily centered around the treatment area, the provider’s fees, and geographic location. On average, patients considering PRF treatment for aesthetic or regenerative purposes in the United States, for example, can expect the cost per session to typically fall somewhere in the range of $700 to $1,800. However, it’s crucial to reiterate that this is an average range, and prices can certainly be found both below and above these figures depending on specific circumstances.
Let’s briefly revisit the key elements driving this cost. The area being treated holds significant sway. Treating a small, specific area such as a scar, a single joint, or just the lip lines will naturally require less preparation, less harvested PRF, and less time compared to a large area like the entire face, a substantial portion of the scalp, or using PRF alongside microneedling for full-face rejuvenation. Therefore, costs will scale with the size and complexity of the treatment zone.
The provider’s credentials and the clinic’s standing in the community also play a substantial role in pricing. Clinics run by highly experienced, board-certified physicians with extensive training in regenerative medicine and aesthetics will typically have higher fees reflecting their expertise, safety record, and the quality of care provided. Establishing a reputable practice, investing in ongoing training, and using the most advanced equipment all contribute to the clinic’s operational costs, which are then factored into the treatment price. Think of it as paying for peace of mind and the likelihood of optimal results delivered safely.
Geographic location is a simple but powerful factor. Medical and aesthetic services, like most goods and services, are priced according to the local economy. A PRF treatment in a major metropolitan area like New York City or Los Angeles will almost certainly be more expensive than the same treatment in a smaller town or rural area, simply due to differences in overhead costs, rent, and regional pricing norms.
Furthermore, the specific protocol and kit used by the clinic for PRF preparation can marginally influence the cost. While the core principle is the same, different manufacturers produce different PRF collection and processing kits, and their costs can vary. Some advanced techniques, like preparing injectable PRF gel or manipulating the fibrin matrix for specific applications, might require additional steps or materials that factor into the session price.
It’s also worth noting that the quoted cost for a single session usually includes the necessary steps: the blood draw, the centrifugation process, the extraction of the PRF, and the application/injection itself, along with the use of sterile supplies and potentially topical anaesthetics. It typically *does not* include the cost of multiple sessions if a series is recommended (which is common), nor does it usually include consultation fees if the consultation is billed separately.
Ultimately, while the average cost for a single PRF treatment session hovers around the $700 to $1,800 mark, it is imperative to get a precise quote from the clinic you are considering, as this will be based on your individual treatment plan, chosen area(s), and their specific pricing structure. This ensures you have an accurate understanding of the financial commitment for your unique needs.
How much do PRF injections cost?
Focusing specifically on PRF injections, which is the most common method of delivery in aesthetic applications, the cost structure mirrors the overall PRF treatment cost but specifically pertains to sessions where the prepared Platelet Rich Fibrin is administered via injection. The cost for a session of PRF injections typically ranges from approximately $700 to $2,000 or more, with the exact figure depending significantly on the factors we’ve already explored, namely the area being treated, the volume of PRF required, the complexity of the injection technique, the expertise of the practitioner, and the geographic location of the clinic.
When we talk about PRF *injections*, we are usually referring to targeted treatments for specific concerns. For example, PRF injections are extremely popular for the delicate under-eye area to address dark circles, hollowness, and fine lines. A treatment focused *solely* on the under-eyes might be on the lower to mid-range of the cost spectrum, perhaps starting around $800 and going up to $1,500 or more, depending on the clinic and the extent of the area treated. This is because the volume of PRF needed for this area is relatively small, typically requiring only one or two tubes of blood draw. However, injecting in this sensitive area requires significant skill and precision, which is reflected in the price.
Treating fine lines and wrinkles across other areas of the face, injecting into acne scars, or treating larger areas like the cheeks or jawline for skin rejuvenation would require more PRF and potentially a greater number of injection points or passes. This expands the treatment scope within that session, naturally increasing the cost.
When PRF injections are used for scalp hair restoration, the cost can sometimes be on the higher end, particularly if a larger area of the scalp is being treated. Stimulating hair follicles requires injecting small amounts of PRF across numerous points on the scalp, which is time-consuming and requires a larger yield of PRF, potentially necessitating drawing more blood. A single session of scalp PRF injections might range from $1,000 to $2,500 or more.
The expertise of the injector is particularly relevant when discussing injections. Precisely placing the PRF in the correct tissue layer (intradermal, subcutaneous, periosteal) is critical for achieving optimal results and minimising risks like bruising or unevenness. Highly experienced practitioners, especially those with specific expertise in facial aesthetics or regenerative injections, will typically charge more for their refined technique and skill, which is a valuable investment in the quality and safety of your outcome.
Furthermore, the type of injected PRF matters. If the PRF is processed into a gel-like consistency (often referred to as Injectable PRF or PRF Gel), which can provide more immediate, subtle volume, the preparation process might differ slightly and could influence pricing compared to injecting purely liquid PRF for skin quality.
In summary, while the range for a single session of PRF injections is typically between $700 and $2,000+, expect the final price to be determined by the specific area(s) targeted, the complexity of the treatment plan, the amount of PRF needed (which relates to blood drawn), and the practitioner’s fees and clinic location. It’s always best to get a detailed, itemised quote during your consultation to understand the exact cost for your tailored injection treatment plan.
How Much Does PRF Cost?
Let’s nail down the cost of PRF therapy once more, cutting through the variations to provide a clear perspective on the potential financial commitment. When prospective patients ask, “How much does PRF cost?” they fundamentally want to know the price of undergoing the Platelet Rich Fibrin treatment. As we’ve thoroughly explored, the cost isn’t a uniform price tag found on a shelf; it’s a service fee based on a number of interconnected factors. However, to provide a tangible figure for planning purposes, you should anticipate the cost for a single treatment session to generally fall within the $500 to $2,500 range. This is the typical price bracket for a single visit where blood is drawn, processed into PRF, and then applied or injected into the treatment area.
The primary elements driving where a specific clinic’s price falls within this range are consistent:
1. Treatment Area: Is it a small, focused zone like the under-eyes, or a larger, more extensive area like the full face or scalp?
2. Treatment Scope: Is it a simple injection session, or is it combined with another procedure like microneedling?
3. Provider Expertise: What are the qualifications, training, and experience level of the practitioner performing the treatment?
4. Clinic Location: Where is the clinic geographically located? Costs are higher in major metropolitan areas.
5. Equipment & Materials: The specific type of centrifuge and PRF collection kits used, while standard for reputable clinics, represent an operational cost.
For instance, a basic facial PRF treatment might start around $800-$1,200 per session. A dedicated under-eye PRF treatment using injectable gel might be priced between $1,000-$1,800 due to the precision and type of PRF gel required. Scalp treatments for hair loss, covering a larger area with numerous injections, could easily be $1,200-$2,500+ per session. Treatments for larger musculoskeletal areas might also fall within or exceed this range depending on the joint or tissue involved and the volume of PRF needed.
It’s absolutely essential to understand that while this $500-$2,500 figure is the cost *per session*, PRF is often recommended as a series. Therefore, the *total* investment required to see optimal and lasting results will be the cost per session multiplied by the recommended number of sessions (typically 2-4, spaced several weeks apart). This means the overall cost of a complete PRF treatment plan could range from $1,500 to $10,000 or potentially more, depending on the individual’s needs, the areas treated, and the clinic’s pricing structure for series packages.
Many clinics offer discounted pricing for packages of multiple sessions, recognising that a series is usually necessary for best results. Inquiring about package deals during your consultation is a smart way to potentially reduce the overall cost per session. While the investment can be significant, particularly for a full series, many patients find the natural, long-lasting regenerative benefits and excellent safety profile of PRF to be well worth the cost, especially when compared to the cumulative costs and potential risks of ongoing treatments with temporary synthetic materials or more invasive procedures.
What is the cost of PRF treatment for face?
Zeroing in on facial applications, arguably one of the most popular uses of Platelet Rich Fibrin, the cost of PRF treatment for the face specifically can vary depending on the extent of the treatment. The face is a large canvas, and PRF can be applied to specific areas or across the entire surface. Therefore, the cost will directly correlate with how much of the face is being treated and the specific technique used.
For a targeted area of the face, such as just the under-eyes, just the perioral lines (around the mouth), or specific scars, the cost will be lower than treating the entire face. A single session for a targeted facial area using PRF injections might range from approximately $800 to $1,800. This price reflects the smaller volume of blood needed, less PRF yield, and a more contained treatment zone, although the precision required for delicate areas like the under-eyes can still place it towards the mid-to-upper end of this range for a small area.
If the treatment involves the full face, aiming to improve overall skin texture, tone, elasticity, and fine lines, the cost per session will naturally be higher. This requires drawing more blood to yield enough PRF to cover a larger surface area, whether through multiple injection points across the face or through topical application combined with a full-face microneedling treatment. A single session of full-face PRF treatment (either via injections or paired with microneedling) typically ranges from approximately $1,200 to $2,500 or more. The technique used (e.g., solely injections, topical post-microneedling, or a combination) can also influence the price, as microneedling itself adds to the overall cost.
Factors like the practitioner’s experience, especially their expertise in facial aesthetics and regenerative techniques, and the clinic’s location and overheads continue to play a significant role in determining where the price falls within these ranges. A highly sought-after facial plastic surgeon or dermatologist in a major city will likely charge more for a full-face PRF treatment than a general practitioner in a smaller town, reflecting their specialised skill and the market’s pricing.
As with other PRF applications, a series of treatments is almost always recommended for facial rejuvenation to achieve optimal and cumulative results. Typically, 2 to 4 sessions spaced 4-8 weeks apart are advised. Therefore, the *total* cost of a full facial PRF treatment plan can range significantly, from potentially $2,400-$5,000 for a series focusing on targeted areas to $3,600 to $10,000 or even more for a comprehensive series treating the entire face. Clinics often offer package pricing for a series, which can offer a cost saving compared to paying for each session individually. During your consultation, be specific about the facial areas you wish to treat and ask for a detailed quote for both a single session and a recommended series to understand the full financial commitment for achieving your facial rejuvenation goals with PRF.
Is PRF expensive?
Defining whether PRF treatment is “expensive” is subjective and depends heavily on an individual’s budget, their financial priorities, and how they compare the cost to alternative treatments. However, relative to some other aesthetic and medical procedures, PRF can be considered a moderate to significant investment, especially when considering the need for multiple sessions.
Let’s look at it comparatively. A single syringe of hyaluronic acid dermal filler might cost between $500 and $900 or more, and often multiple syringes are needed for full correction, with results lasting typically 6-18 months. A single session of PRF for a similar area might cost slightly more initially (e.g., $800-$1,800), but when you factor in that a series is usually required (3 sessions perhaps bringing the total to $2,400-$5,400+), the upfront investment for a *complete* course of PRF treatment is often higher than a single filler treatment. However, the benefits of PRF are fundamentally different – they are regenerative, stimulating your body to produce its own tissue, potentially leading to longer-lasting natural improvements compared to fillers which simply occupy space and eventually metabolise.
Compared to surgical procedures like a facelift or hair transplant, PRF is significantly less expensive, less invasive, and has virtually no downtime or surgical risks. These surgical options involve costs ranging from $8,000 to $30,000 or more. In this context, PRF, even as a series, is far more accessible.
Compared to other non-surgical treatments like microneedling (which might cost $300-$800 per session, often recommended in a series) or certain laser treatments (which can vary widely from a few hundred to several thousand dollars per session), PRF’s per-session cost is often higher, especially when combined with these modalities. However, the addition of PRF is intended to *enhance* the regenerative outcome of these treatments by providing growth factors directly.
In medical applications, comparing PRF to the long-term costs of managing chronic conditions or repeated treatments with less regenerative approaches can also factor into perceived expense. If PRF helps significantly improve a musculoskeletal injury or a chronic wound, the upfront cost might be offset by reduced long-term healthcare expenses or improved quality of life.
So, is PRF expensive?
* Yes, it is generally more expensive per session than basic non-invasive treatments like standard microneedling or simple topical therapies.
* Yes, the total cost for a recommended series of PRF treatments represents a notable financial investment, potentially running into several thousand dollars.
* No, it is significantly less expensive than surgical options.
* It depends on how you value natural, regenerative results and compare the cost to the longevity of results from synthetic or less regenerative treatments.
Ultimately, whether PRF feels expensive is a personal assessment based on its cost relative to its benefits, its natural approach, the required number of sessions, and your individual financial situation and priorities. It’s an investment in stimulating your body’s own healing and rejuvenation potential, which many find to be a valuable proposition.
What is the average cost of Microneedeling with PRF?
Microneedling combined with Platelet Rich Fibrin (PRF) is a popular synergistic treatment, particularly for facial rejuvenation, as it pairs the collagen-stimulating effect of controlled micro-injury from microneedling with the powerful growth factor delivery of PRF. This combination leverages two different, yet complementary, mechanisms to enhance skin regeneration. When clinics offer “Microneedling with PRF,” the cost is naturally higher than microneedling alone because it includes the additional steps of drawing blood, processing it into PRF, and applying the PRF during and/or immediately after the microneedling procedure.
The average cost for a single session of Microneedling with PRF on the face typically ranges from approximately $700 to $1,500. As with standalone PRF treatments, this average can fluctuate based on several factors:
-
- Extent of Treatment: Is it full-face microneedling with PRF, or is it focused on a smaller area like the décolletage or specific scars? A full-face treatment will be on the higher end.
-
- Microneedling Device Used: The type of microneedling device (e.g., pen-style vs. roller, depth capabilities, radiofrequency combination) can influence the base cost of the microneedling portion of the treatment.
-
- PRF Application Method: Is the PRF applied topically and massaged into the micro-channels immediately after microneedling (the most common method), or are targeted injections of PRF also performed in specific areas (like under-eyes or deep lines) as part of the combined session? Adding injections would increase the complexity and cost.
- Clinic Location and Practitioner Expertise: As always, location and the experience of the practitioner performing both the microneedling and the PRF processing and application will influence the price.
For instance, a full-face microneedling session that includes topical PRF application might average around $1,000-$1,500 per session. If targeted PRF injections are also performed within the same session on specific problem areas, the cost could go higher, potentially $1,500 to $2,000+. Treating smaller areas like isolated scars with Microneedling + PRF might be closer to the $700-$1,000 range.
It’s important to recognise that Microneedling with PRF is almost always recommended as a series of treatments to achieve optimal skin rejuvenation results. A typical course involves 3 to 4 sessions, usually spaced 4 weeks apart. Therefore, the *total* average cost for a complete series of Microneedling with PRF treatments for the face could range from approximately $2,100 to $6,000 or more.
Many clinics offer package pricing for a series of Microneedling with PRF sessions, which often provides a cost saving compared to booking and paying for each session individually. When inquiring, be sure to ask for the cost per session *and* the cost for a package of the recommended number of sessions to get a clear picture of the total investment needed for your skin rejuvenation goals with this powerful combination therapy. This combination therapy is highly valued because the microneedling creates controlled micro-injuries that stimulate a healing response and create pathways for the PRF growth factors to penetrate deeply, leading to enhanced collagen production and overall skin improvement.
What is the price of PRF kit?
The price of a PRF kit itself is not typically something that patients see or purchase directly; it’s a component of the clinic’s operational cost and is bundled into the overall price of the treatment session. However, understanding that these kits are a necessary expense for the clinic helps explain part of the treatment cost. A “PRF kit” refers to the collection of sterile, disposable medical supplies needed for a single patient’s treatment: typically, these include the specialised tubes for drawing blood and processing it in the centrifuge, syringes, needles, and possibly sterile containers or tools for handling the extracted PRF.
The cost of these specialised PRF collection kits for a clinic can vary depending on the manufacturer, the specific type of PRF being prepared (some kits are optimised for different PRF types), and the volume of blood the tubes are designed to hold (which dictates how much PRF can be yielded). Generally, the cost to a clinic for a single patient’s PRF kit can range from approximately $50 to $200 or even more. This cost is incurred *for each and every patient treatment*.
For example, if a clinic uses a kit that costs $100 per patient, and they perform 100 PRF treatments in a month, that’s $10,000 just in disposable kit costs, in addition to staff time, equipment depreciation, rent, utilities, etc. This is why the cost of the kit is an unavoidable component that is factored into the per-session price charged to the patient. Reputable clinics will use high-quality, sterile, single-use kits specifically designed for PRF preparation to ensure safety and consistent yield. Using improper tubes or techniques can compromise the quality and sterility of the PRF product.
As a patient, you won’t purchase the kit separately, but the price you pay for your treatment session covers all the necessary materials, including this specialised kit. Understanding that these specific, sterile supplies are required for safe and effective PRF preparation helps contextualise why the treatment has a certain baseline cost before accounting for the practitioner’s expertise and time. The kit is essentially the vessel that allows your blood to be safely and effectively transformed into the regenerative PRF concentrate, ensuring a sterile process from draw to application.
How Long Do PRF Injections Last and When Can Results Be Seen?
Understanding the timeline for both the appearance and longevity of results is crucial for managing expectations with Platelet Rich Fibrin (PRF) injections. Unlike treatments that provide immediate, albeit temporary, volume or correction, PRF works by stimulating the body’s natural regenerative processes, which unfold over time. Therefore, results are not instantaneous; they are gradual and cumulative, improving over weeks and months after treatment. The duration of these results is also different – rather than the material itself disappearing, the *effects* last as long as the newly generated tissue remains healthy and functional, subject to the natural aging process and individual factors.
Typically, patients do not see dramatic changes immediately after a PRF injection session. There might be some temporary fullness from the injected volume (especially with PRF gel) and transient redness or swelling, but these are not the final results. The regenerative process begins internally as the growth factors are released from the fibrin matrix, signalling cellular activity. This initial biological work happens beneath the surface.
Visible improvements usually begin to appear subtly within 2 to 4 weeks after the first treatment session. During this time, new collagen and elastin production is starting, and improvements in skin texture or a mild increase in firmness might be noticed. However, the most significant and noticeable results typically become apparent around 6 to 12 weeks after the first treatment, and continue to improve with subsequent sessions. This is when the newly formed collagen has built up sufficiently to create visible changes in skin quality, firmness, and the reduction of fine lines or scars. For applications like hair restoration, it might take 3 to 6 months to see noticeable hair regrowth, as hair cycles are slower.
The longevity of the results from PRF injections varies depending on the area treated, the individual’s age and overall health, lifestyle factors, and the number of treatment sessions completed. Because PRF stimulates the growth of *new* tissue (collagen, elastin, blood vessels), the results are potentially much longer-lasting than those achieved with treatments that simply fill space or provide transient stimulation.
For facial rejuvenation and skin quality improvements, the regenerative effects stimulated by a series of PRF treatments can often last for 6 to 12 months or even longer after the final session. Some practitioners report effects lasting up to 18 months. However, it’s important to understand that PRF does not stop the natural aging process. Your skin will continue to age, and external factors like sun exposure, lifestyle, and genetics will influence the long-term maintenance of results. Therefore, many patients opt for periodic maintenance treatments, perhaps once a year after completing an initial series, to help sustain the benefits and continue supporting their skin’s regenerative health.
For hair restoration, the longevity of results can also vary. While PRF can stimulate dormant follicles and promote hair growth, it doesn’t alter the underlying genetic or hormonal factors contributing to hair loss. Therefore, maintenance treatments are often recommended, perhaps every 6 to 12 months, to continue stimulating the follicles and maintain the improved hair density and thickness.
In summary, expect to start seeing subtle results from PRF injections within a few weeks, with more noticeable improvements developing over 2-3 months and continuing to build with subsequent sessions. The duration of these regenerative effects can range from 6 months to over a year, but maintenance treatments are often advised to prolong the benefits as the natural aging process continues. The key is patience, as PRF initiates a biological transformation that unfolds beautifully over time.
How long do PRF injections last?
Delving deeper into the duration of the benefits from PRF injections, it’s important to clarify that we’re discussing the longevity of the *regenerative effects* stimulated by the treatment, not the presence of the injected material itself, which is naturally absorbed by the body. The Platelet Rich Fibrin matrix slowly degrades over a couple of weeks, releasing its growth factors and cellular components. However, the biological processes initiated by these signals – the production of new collagen, elastin, and blood vessels – continue for much longer.
For aesthetic concerns like improving skin texture, elasticity, fine lines, and addressing under-eye concerns, the noticeable results from a course of PRF injections (which typically involves 2-4 sessions) generally endure for 6 to 12 months. Some individuals may experience visible benefits for up to 18 months or occasionally longer, depending on a range of individual factors. These factors include the patient’s age (younger skin with more robust regenerative capacity may respond longer), overall health, lifestyle (smoking, excessive sun exposure, poor diet can diminish longevity), the specific area treated (areas with less movement might hold results longer), and the quality of the PRF prepared and the skill of the injection technique.
The cumulative effect of multiple treatment sessions is also key to longevity. A single PRF session might provide some initial boost, but a series is designed to build upon the regenerative response, leading to more significant and enduring results. The ‘base’ of regenerated tissue becomes stronger and more robust with each treatment.
For hair restoration purposes, the duration of increased hair density and vitality following PRF injections can also vary. While initial stimulation might lead to new growth visible within 3-6 months, maintaining these results often requires ongoing treatment. Without maintenance, the underlying genetic or hormonal factors contributing to hair loss may cause thinning to resume. Many practitioners recommend maintenance sessions for hair loss every 6 to 12 months to sustain the benefits.
It’s crucial to understand that PRF provides a biological stimulus for regeneration, but it does not halt the aging process. New collagen and elastin will be produced, but existing fibers will continue to degrade slowly as part of natural aging, and new damage from environmental factors will occur. This is why maintenance treatments are often recommended, not because the *original* PRF is gone, but because the body continues to age and could benefit from renewed regenerative signals to counteract ongoing decline.
Patients should view PRF injections as stimulating a long-term process rather than providing a temporary filler. The results are natural, subtle, and evolve over time, offering a sustained improvement in tissue health and appearance. The duration of these visible effects is a testament to the power of harnessing the body’s own healing capabilities.
Are PRF results permanent?
The results from Platelet Rich Fibrin (PRF) treatment are generally not considered permanent in the way that, for instance, surgically removed tissue or an implanted non-absorbable foreign body might be. However, the distinction is crucial: while the effects are not permanent, the treatment *does* stimulate the production of *new* tissue – new collagen, new elastin, new blood vessels, and potentially the proliferation of new cells – and this new tissue *is* permanent. What isn’t permanent is the *degree* of improvement relative to the ongoing process of aging and environmental damage.
Think of it like exercising and building muscle. When you exercise, you build new muscle tissue, which is permanent tissue. However, if you stop exercising and continue your normal activities (which are like the aging process), that muscle will gradually atrophy over time. Similarly, PRF stimulates the creation of new, youthful-acting collagen and elastin. This newly generated tissue becomes a part of your body’s structure. However, as your body continues to age, and is exposed to factors like sun damage, pollution, stress, and genetics, the natural degradation of collagen and elastin continues. The newly built tissue will also be subject to these processes over time.
So, while the *material* injected (the PRF clot) is absorbed by the body within a couple of weeks, and the peak regenerative *activity* from a single session might subside after a few months, the *result* of that activity – the new collagen, elastin, and vascularity – persists. The visible *benefit* from a series of treatments might last 6 to 18 months because it takes that long for the effects of natural aging and breakdown to become noticeable enough to diminish the improvement gained from the treatment.
This is why practitioners often recommend maintenance treatments. These aren’t necessary because the previous treatment “wore off” like a temporary filler. Instead, they are recommended to provide renewed stimulation to continue the regenerative process and counteract the ongoing effects of aging and environmental damage, thereby *sustaining* the improved appearance achieved with the initial treatment series.
For hair restoration, the principle is similar. PRF stimulates hair follicles to grow, and the resulting hair is permanent hair. However, if the underlying cause of hair loss (e.g., genetics, hormones) is still active, without continued stimulation (maintenance PRF sessions) or addressing the root cause, those follicles may eventually miniaturise or become dormant again over time.
In essence, PRF treatments stimulate the body to build permanent tissue, but they do not stop the passage of time or protect the skin/tissues from future damage or the ongoing aging process. Therefore, while the tissue created is permanent, the *visual improvement* relative to your baseline will gradually lessen over time, necessitating maintenance sessions to prolong the optimal results. It’s a powerful, natural tool for regeneration, but it requires ongoing support to truly fight the tide of time.
Is PRF permanent?
When the question “Is PRF permanent?” arises, it points to a fundamental misunderstanding of how this regenerative treatment works. Let’s be crystal clear: the Platelet-Rich Fibrin *material itself*, which is injected or applied, is not permanent. It is a biological construct derived from your own blood – the fibrin matrix, platelets, leukocytes, and stem cells – and like any natural tissue or blood product introduced back into the body, it is designed to be metabolised and absorbed by your system over a relatively short period, typically within 1 to 2 weeks. This absorption is necessary for the growth factors to be released and for the fibrin scaffold to play its role in guiding initial tissue organisation before new tissue takes over.
However, the *effects* of PRF are intended to be long-lasting because they stimulate the creation of *new, permanent tissue*. The growth factors released from the PRF trigger cellular processes like neocollagenesis (new collagen formation), neoelastogenesis (new elastin formation), and angiogenesis (new blood vessel formation). The collagen, elastin, and blood vessels that your body produces in response to the PRF stimulation *are* permanent components of your tissue.
The perceived “longevity” of the PRF treatment (often cited as 6-18 months for aesthetic effects) refers to how long the *visible improvement* lasts before the ongoing effects of natural aging and environmental factors diminish that improvement to a point where a touch-up or maintenance treatment is desired. The new tissue is still there, but the surrounding tissue continues to age and degrade.
Think of it like planting a seed (the PRF stimulus) that grows a tree (new collagen/elastin). The seed is gone, but the tree (the new tissue) is permanent. However, the tree will still be affected by weather, pests, and time (the aging process). To keep the forest (your skin/tissue) looking dense and healthy, you might need to plant more seeds periodically (maintenance PRF treatments) to replace trees lost to time or damage, or to thicken areas where the original trees haven’t fully compensated for ongoing loss.
So, to directly answer the question:
* Is the PRF *material* itself permanent? No, it is absorbed.
* Are the *results* (the newly regenerated tissue) permanent tissue? Yes, the tissue is permanent.
* Is the *visual improvement* permanent? No, the visible benefits eventually diminish over time due to natural aging and environmental factors, requiring maintenance to sustain the optimal look.
Therefore, while PRF stimulates permanent tissue growth, the treatment’s perceived duration refers to the period over which the visual benefits are optimally apparent before the ongoing effects of aging necessitate further intervention to maintain those benefits. It’s a distinction worth understanding to set realistic expectations.
What are the results of PRF treatment and how long do they last?
The results of PRF treatment are diverse and depend heavily on the specific area and condition being addressed, but they are fundamentally rooted in stimulating the body’s natural healing and regenerative capabilities. Unlike synthetic fillers that provide immediate structural volume, PRF works by prompting your body to *create* new tissue, leading to improvements that are natural, subtle, and evolve over time.
In aesthetic applications, particularly for facial rejuvenation, the results of PRF treatment include:
* Improved Skin Texture and Tone: Skin becomes smoother, softer, and gains a more even, radiant complexion.
* Reduced Fine Lines and Wrinkles: Collagen and elastin production plumps the skin, smoothing out superficial lines and making deeper wrinkles less noticeable.
* Enhanced Skin Elasticity and Firmness: Increased collagen and elastin restore some of the skin’s youthful bounce and resilience, reducing mild skin laxity.
* Reduction in Appearance of Scars: PRF helps remodel scar tissue, making acne scars, surgical scars, and stretch marks less prominent and blend better with surrounding skin.
* Improvement in Dark Circles and Under-Eye Hollowness: When injected under the eyes, PRF can help thicken the thin skin, improve circulation (reducing dark circles caused by visible vessels), and provide subtle, natural volume to fill hollows, leading to a brighter, more rested look.
* Stimulated Hair Growth: For the scalp, results involve increased hair density, thickness, and growth in areas of thinning, as dormant or miniaturized follicles are stimulated.
In medical applications, results include:
* Accelerated Wound Healing: Faster closure of chronic wounds, ulcers, and burns.
* Improved Bone and Tissue Regeneration: Enhanced healing and integration of grafts in dental and orthopaedic procedures.
* Reduced Pain and Improved Function in Musculoskeletal Injuries: Stimulation of repair in damaged tendons, ligaments, and joints.
When can you see the results?
As the regenerative process takes time, visible results are not immediate.
* Subtle improvements might begin to appear 2-4 weeks after the first session, as initial collagen production starts.
* More noticeable and significant results typically develop over 6-12 weeks following the first treatment.
* Optimal results are usually observed 2-3 months after completing a recommended series of treatments (often 2-4 sessions).
* For hair growth, visible improvement might take 3-6 months.
How long do the results last?
The longevity of the *visible benefits* depends on the area treated, individual factors, and the number of sessions.
* For aesthetic facial rejuvenation, results from a series of PRF treatments commonly last 6 to 12 months, sometimes up to 18 months.
* For hair restoration, results can last 6 to 12 months, but ongoing maintenance is often needed.
* In musculoskeletal or dental applications, the tissue regeneration is permanent, but the *clinical benefit* (like reduced pain or stable graft) lasts as long as the tissue remains healthy and functional, potentially years, but subject to future injury or degradation.
To sustain the aesthetic benefits, periodic maintenance treatments are often recommended, typically once a year, to provide ongoing regenerative support and counteract the effects of aging. While PRF creates permanent tissue, the ongoing process of aging means the *visual improvement* compared to baseline will gradually diminish over time without continued stimulation. Thus, results are long-lasting but require maintenance for sustained optimal appearance.
How long will the results last for?
Addressing the longevity question once more, focusing on the practical duration of the benefits you can *see and feel* after undergoing Platelet Rich Fibrin (PRF) treatment, especially in aesthetic contexts, the typical timeframe for sustained, visible improvement after completing a recommended initial series (usually 2-4 sessions) is consistently cited as 6 to 12 months. It’s important to remember this is not the life span of the injected material (which is absorbed quickly), but the duration over which the newly regenerated tissue continues to provide a noticeable aesthetic enhancement relative to your pre-treatment state and the ongoing effects of aging.
Several factors contribute to this variability within the 6-12 month window, and sometimes extending beyond it to 18 months for some individuals:
-
- Individual Biology: Every person’s regenerative capacity is unique. Younger individuals or those in excellent health with robust healing responses may build collagen and elastin more efficiently and maintain the improvements for a longer duration.
-
- Treatment Area: Different tissues regenerate at different rates and are subjected to varying degrees of movement and stress. For instance, results under the eyes might have a slightly different longevity profile than improvements in cheek texture or scalp hair growth.
-
- Number of Sessions: Completing the full, recommended series of treatments is crucial for maximising longevity. A single session will provide some benefit, but a series builds a stronger foundation of new tissue, leading to more sustained results.
-
- Lifestyle Factors: Post-treatment care and lifestyle choices significantly impact how long your regenerated tissue remains healthy and the visible results persist. Factors that degrade collagen and elastin, such as excessive unprotected sun exposure, smoking, poor nutrition, significant stress, and rapid weight fluctuations, will accelerate the decline of results. Conversely, maintaining a healthy lifestyle, using medical-grade skincare, and protecting your skin from the sun can help prolong the benefits.
- Skin Quality at Baseline: Individuals starting with less severe signs of aging or damage may find their results last longer, as there is less ongoing degeneration to counteract.
Because the results are driven by your body’s natural processes and are subject to the continuous effects of aging and environmental exposure, Platelet Rich Fibrin treatments are often best thought of as an ongoing commitment to regenerative health rather than a one-time fix. To maintain the optimal results achieved with the initial series, periodic maintenance treatments are frequently recommended. These are typically scheduled every 6 to 12 months, depending on the individual’s response and goals. These follow-up sessions provide renewed stimulation to the tissues, helping to support the longevity of the improvements and continue building healthy tissue over time, effectively helping you stay ahead of the aging curve and sustain the benefits of PRF therapy for years to come.
When can I see results from PRF?
Patience is indeed a virtue, especially when it comes to regenerative therapies like PRF, where the visible outcome unfolds over time as your body diligently works to rebuild and rejuvenate tissue from within. You won’t walk out of the clinic with immediate, dramatic changes (beyond some temporary swelling from the injection volume, which quickly subsides). The results are subtle at first, then gradually become more noticeable.
You can typically expect to start seeing the very first subtle signs of improvement from a PRF treatment session within 2 to 4 weeks. During this initial period, the inflammatory phase of healing is active, and fibroblasts begin to be stimulated, starting the process of collagen and elastin production. You might notice a slight improvement in skin texture or a subtle glow, but it’s usually not something others would immediately remark upon.
The more significant and satisfying results generally become apparent around 6 to 12 weeks after your first treatment session. This is when enough new collagen, elastin, and blood vessels have been produced to create visible changes. Skin quality improves more noticeably, fine lines may appear softened, and areas of hollowness or scarring might show initial signs of filling or remodelling. The peak regenerative activity from a single session often occurs around this 2-3 month mark.
However, it’s crucial to understand that PRF treatments are most effective as a series. The regenerative effects are cumulative. While you will see improvement after one session, optimal results are typically achieved only after completing a recommended course of treatments, which is commonly 2 to 4 sessions spaced 4-8 weeks apart. After completing the full series, the results will continue to develop and improve for another 2-3 months *after* the final session. Therefore, the *peak* optimal results might not be fully realised until 3 to 6 months after your very last treatment in a series.
For specific applications like hair restoration, the timeline is a bit different because hair growth cycles are slower. While the PRF is stimulating the follicles from the start, visible hair regrowth typically takes longer to manifest. You might begin to see fine vellus hairs appear around 3 months, with more significant and thicker hair growth becoming apparent 6 to 12 months after starting a treatment series.
In summary, plan to be patient. Expect subtle changes around 2-4 weeks, noticeable improvements around 6-12 weeks, and optimal results after completing a series and allowing a few more months for the full regenerative effects to manifest. It’s a journey of gradual, natural enhancement powered by your own body’s remarkable capabilities.
When does PRF start to work?
PRF starts working the *moment* it is introduced into the tissue, initiating a cascade of biological events at a cellular level, even though these initial processes aren’t immediately visible to the naked eye. The therapeutic action of Platelet Rich Fibrin begins almost instantly through several key mechanisms:
1. Immediate Growth Factor Release (Initial Burst): While PRF is known for its *sustained* release of growth factors from the fibrin matrix, there is an initial, rapid release of a certain percentage of growth factors as the injected PRF interacts with the local tissue environment and platelets become activated. This initial burst provides an immediate signal to the surrounding cells, prompting them to begin their healing and regenerative response. This is the “start” of the work at the molecular level.
2. Inflammatory Response Initiation: The introduction of the PRF, along with the micro-trauma from injections (if applicable) and the presence of leukocytes within the PRF, immediately triggers the necessary inflammatory phase of wound healing. This controlled inflammation is crucial; it involves the recruitment of immune cells that clean up damaged tissue and release further signalling molecules (cytokines and growth factors) that orchestrate the next phases of repair and regeneration. So, from the very beginning, PRF is participating in this foundational stage of healing.
3. Fibrin Scaffold Formation/Integration: The fibrin matrix within the PRF immediately provides a natural, three-dimensional scaffold at the treatment site. This scaffold helps to stabilise the injected material and provides a framework that local cells (like fibroblasts and endothelial cells) can adhere to and migrate along. This integration and structural support begins instantly upon placement.
4. Sustained Growth Factor Release Initiation: Concurrently with the initial burst, the process of slow degradation of the fibrin matrix begins, initiating the sustained release of the remaining trapped growth factors and cells over the following 1-2 weeks. This continuous release provides a prolonged biological signal, ensuring the regenerative message is delivered consistently over time, which is a hallmark of PRF’s mechanism.
So, while you don’t *see* the results immediately, the biological “work” of PRF begins within minutes to hours of treatment, as growth factors are released, inflammatory pathways are activated, the fibrin scaffold integrates, and cells begin receiving signals to initiate proliferation, migration, and matrix synthesis. The body is actively responding and initiating the regenerative process from the moment the PRF is delivered. The visible results are simply the later, tangible manifestation of this ongoing, complex biological activity occurring beneath the surface, which takes weeks to months to become apparent. Therefore, PRF starts to work immediately at a cellular and molecular level, even though the aesthetic or functional improvements are delayed.
How long does PRF Under Eye Treatment last?
PRF treatment for the under-eye area is a particularly popular application due to its ability to naturally rejuvenate this delicate region, addressing concerns like dark circles, hollowness (tear troughs), fine lines, and crepey skin. The longevity of results specifically for PRF Under Eye Treatment tends to fall within the general range for aesthetic PRF applications, typically lasting 6 to 12 months after a recommended series of treatments.
However, several factors are particularly relevant to the under-eye area that can influence how long the benefits are visible:
-
- Delicate Skin: The skin under the eyes is the thinnest on the body, making it particularly susceptible to signs of aging and environmental damage. While PRF stimulates thickening and collagen production, this thinness means changes might be subtle initially and the area is prone to showing age relatively quickly.
-
- Movement and Expression: The under-eye area is constantly in motion due to blinking, squinting, and facial expressions. This dynamic environment can potentially influence the longevity of tissue regeneration compared to less mobile areas.
-
- Underlying Cause of Concern: The duration of improvement can depend on the root cause of the under-eye issue. If dark circles are primarily due to thin skin showing underlying vessels, thickening the skin with PRF can provide long-lasting improvement. If they are related to pigmentation or genetics, PRF’s impact might be less dramatic or require combination therapy. Similarly, if hollowness is due to significant fat loss or bone structure, PRF gel can provide subtle volume and regeneration, but the longevity of volume correction might be less than synthetic fillers designed purely for structural support.
-
- Quality of PRF Gel (if used): For treating hollowness, PRF is often processed into a gel consistency. The specific preparation method and the practitioner’s technique for creating and injecting this gel can influence its initial subtle volumizing effect and potentially the sustained regenerative stimulus.
- Individual Factors: As always, personal healing capacity, age, lifestyle, and genetics play a significant role.
Given the delicate nature of the area and the desire for sustained improvement, a series of 2-3 PRF under-eye treatments spaced about 6-8 weeks apart is commonly recommended. After completing this initial series, the visible benefits of reduced dark circles, improved skin quality, softened lines, and subtle volume enhancement typically last for 6 to 12 months. To maintain these results, many patients choose to have a single maintenance session annually.
It’s crucial to consult with a practitioner experienced in treating the under-eye area with PRF. They can assess your specific concerns, determine if you are a good candidate, explain the expected results and their likely duration based on your individual factors, and outline a tailored treatment and maintenance plan. While not permanent, the 6-12 month longevity makes PRF under-eye treatment a compelling option for those seeking a natural, regenerative approach to rejuvenating tired-looking eyes.
Is PRF for hair permanent?
When considering PRF for hair loss, the question of permanence is similar to other PRF applications but with specific nuances related to hair growth cycles and the underlying causes of hair thinning. Is the *hair* that grows after PRF treatment permanent? Yes, the hair stimulated by PRF injections is your natural hair, and individual hair strands are permanent in the sense that they follow their natural growth cycle until they eventually shed and are replaced by new hairs from the same follicle (in healthy cycles). Is the *effect* of increased hair density or reduced thinning from PRF permanent? Generally, no, the improvement in hair density and thickness achieved through PRF is not considered permanent without maintenance.
Here’s why: Platelet Rich Fibrin works by stimulating dormant or miniaturized hair follicles, prompting them to re-enter the active growth phase (anagen) and produce thicker, healthier hair. This is a powerful regenerative effect. However, the most common cause of hair loss, especially in men and women (androgenetic alopecia), is genetic and hormonal. These underlying factors that caused the follicles to miniaturise in the first place are still present even after PRF treatment.
While PRF provides a robust stimulus, it doesn’t fundamentally alter the genetic blueprint or permanently block the hormonal signals that are causing progressive hair loss. Therefore, without ongoing stimulation, the follicles that responded to PRF may, over time, begin to miniaturise again due to the continued influence of these underlying factors.
Think of PRF for hair loss as fertilising a plant that is struggling in poor soil. The fertiliser (PRF) gives the plant a strong boost and helps it grow healthy and vibrant. But if the soil conditions (underlying cause of hair loss) are not permanently changed, the plant might eventually start to struggle again without continued fertilisation (maintenance treatments) or addressing the soil issue directly.
For this reason, practitioners commonly recommend a series of initial PRF hair restoration treatments (often 3-4 sessions spaced 4-8 weeks apart) to stimulate robust growth, followed by periodic maintenance sessions. These maintenance sessions are typically needed every 6 to 12 months to continue providing the necessary growth factor signals to the follicles and counteract the ongoing progression of hair loss.
While the hair that grows is your own permanent hair, the *state* of the follicle (whether it’s actively growing thick hair or is miniaturising) is influenced by continuous signals. PRF provides a powerful positive signal, but maintaining that positive state often requires repeat treatments to counter the negative signals causing the hair loss. So, PRF helps you regrow your own permanent hair, but sustaining the *density* and *thickness* often requires ongoing treatment.
Is PRF Safe and What Are the Potential Risks or Side Effects?
One of the most compelling aspects of Platelet Rich Fibrin (PRF) treatment is its excellent safety profile. This is primarily attributable to its autologous nature, meaning the material used is derived entirely from the patient’s own blood. Because the body recognizes PRF as its own tissue, the risk of allergic reactions, immune rejection, or transmission of infectious diseases is virtually eliminated. This makes PRF a remarkably safe option for a wide range of individuals, including those who may have sensitivities to synthetic materials used in other aesthetic or medical treatments. The process of obtaining PRF is also minimally invasive, involving only a standard blood draw, centrifugation, and then application or injection using fine needles or cannulas, which inherently carries fewer risks than surgical procedures.
However, like any medical procedure, even minimally invasive ones, PRF treatment is not entirely without potential risks or side effects, although they are generally mild, temporary, and rare. The most common side effects are related to the injection or application process itself. These typically include:
-
- Temporary Swelling: Some degree of swelling at the treatment site is common immediately after injections, due to the volume of the injected material and the body’s natural inflammatory response initiating healing. This swelling is usually mild and resolves within a few hours to 1-2 days.
-
- Bruising: Bruising is possible at any injection site, as a small blood vessel can be nicked by the needle. The likelihood and severity of bruising vary depending on the individual, the treatment area, the practitioner’s technique, and whether certain medications or supplements were taken beforehand that increase bruising risk (e.g., aspirin, NSAIDs, fish oil – always disclose all medications/supplements to your provider). Bruises typically resolve within a week or two.
-
- Redness: The treated area, especially after injections or if combined with microneedling, may appear red. This is part of the normal inflammatory response and usually subsides within a few hours to a day.
- Tenderness or Soreness: The injection sites may feel slightly tender or sore to the touch for a day or two after treatment. This discomfort is generally mild and can be managed with over-the-counter pain relievers if needed (preferably non-NSAIDs).
More severe complications are exceedingly rare but theoretically possible with any injection procedure:
-
- Infection: While rare with proper sterile technique, there is always a minimal risk of infection whenever the skin barrier is breached. Clinics maintain strict sterile protocols during blood draw, processing, and injection to mitigate this risk.
-
- Nerve Injury: Extremely rare, particularly with superficial injections used in aesthetics. This is more of a theoretical risk with injections in areas close to major nerves, but skilled practitioners with extensive anatomical knowledge take precautions to avoid this.
-
- Vascular Compromise: An extremely rare complication where material is inadvertently injected into a blood vessel, potentially blocking blood flow. This is the basis of the rare concern about blindness (discussed below). Experienced practitioners use techniques like aspiration before injecting, using cannulas (blunt-tipped instruments) in high-risk areas, and having thorough anatomical knowledge to minimise this risk.
- Unsatisfactory Results: While not a safety risk, the outcome might not meet expectations. This can be due to various factors, including individual response to treatment, the severity of the condition being treated, or the practitioner’s technique. This highlights the importance of realistic expectations and choosing an experienced provider.
Overall, PRF is considered a very safe treatment option due to its autologous nature and minimally invasive procedure. When performed by a qualified and experienced practitioner adhering to strict sterile protocols, the potential risks and side effects are minimal and transient. Discussing any concerns you have about safety and potential side effects with your practitioner during the consultation is always recommended.
Are PRF injections safe?
To directly address the safety of PRF injections, the overwhelming consensus within the medical community is that they are considered very safe, particularly when performed by qualified and experienced practitioners. The safety profile is a major advantage of PRF therapy compared to treatments involving synthetic substances or more invasive surgical procedures.
The primary reason for this high safety rating is the autologous nature of the injectable material. The Platelet Rich Fibrin is derived entirely from the patient’s own blood. This eliminates the risk of:
* Allergic Reactions: There is virtually no chance of having an allergic reaction to your own blood components.
* Transmission of Infectious Diseases: Since the material comes from *you* and is going back into *you* in a closed, sterile system, there is no risk of transmitting diseases that might occur with blood products sourced from donors.
* Immunological Rejection: Your body recognizes the PRF as its own tissue, so there’s no risk of your immune system rejecting the injected material.
The potential risks associated with PRF injections are predominantly those inherent to any procedure involving needle sticks or injections into the skin:
* Minor and Temporary Side Effects: These are the most common occurrences and include localized redness, swelling, bruising, tenderness, or mild discomfort at the injection sites. These effects are generally mild and subside within a few hours to a couple of days. Bruising can sometimes take longer to resolve (up to a week or two) but is typically minor.
* Risk of Infection: While rare, infection is a theoretical risk whenever the skin barrier is broken. This risk is minimised to an extremely low level by ensuring the procedure is performed in a clean clinical environment using strict sterile techniques throughout the blood draw, processing, and injection phases.
* Risk of Bleeding: Minor bleeding at the injection site is possible but stops quickly. Significant bleeding or hematoma is rare.
Very rare, more serious complications like nerve damage or vascular compromise are theoretical risks with any injection procedure, especially in certain anatomical areas. However, these are exceedingly uncommon in typical aesthetic PRF treatment areas when performed by a practitioner with sound anatomical knowledge and proper injection techniques, such as using cannulas in higher-risk zones and aspirating before injecting to ensure the tip is not within a vessel.
The safety of PRF injections is significantly enhanced by choosing a qualified and experienced provider. A skilled practitioner understands facial anatomy, uses the correct injection techniques and depths for specific areas, maintains sterile protocols, and knows how to manage any potential adverse events.
In conclusion, PRF injections are considered remarkably safe due to the use of your own biological material. The potential side effects are almost always mild and temporary, related to the injection process itself. While extremely rare complications exist, they are minimised when the procedure is performed by a competent professional in a proper clinical setting. For the vast majority of patients, PRF injections offer a safe and well-tolerated path to natural rejuvenation.
Is PRF safe?
Yes, unequivocally, Platelet Rich Fibrin (PRF) is widely regarded as a very safe medical and aesthetic treatment modality. Its safety profile is one of its most significant advantages and a primary reason for its growing popularity. The fundamental principle underpinning PRF’s safety is its autologous nature. This means the therapeutic material used for the treatment is derived directly from the patient’s own blood, without the addition of any foreign substances, chemicals, or anticoagulants (or minimal amounts, depending on the specific protocol).
When you introduce a substance back into the body that originated from that same body, the likelihood of adverse immunological reactions is dramatically reduced. This inherent biocompatibility eliminates the risks commonly associated with synthetic fillers or materials derived from other sources, such as:
-
- Allergic reactions: Eliminated risk as it is your own tissue.
-
- Rejection: Your immune system does not identify PRF as a foreign invader, so there is no risk of rejection.
- Disease transmission: As the blood is drawn from and administered back to the same individual, there is no risk of contracting diseases that could potentially be transmitted through donor blood products.
The process of preparing PRF is also safe and involves standard medical practices: a simple blood draw and centrifugation in a sterile environment. The application, whether topical or via injection, is minimally invasive.
Potential side effects, as discussed, are almost exclusively minor and transient, related to the physical act of injection rather than the PRF material itself. These include temporary swelling, bruising, redness, or soreness at the treatment site. These resolve on their own, typically within a few hours to a couple of days.
While exceedingly rare complications like infection or injury to surrounding structures are theoretically possible with any medical injection, these are not inherent to the PRF material but rather to the technique of administration. These risks are minimised by choosing a qualified and experienced practitioner who adheres to strict sterile protocols and possesses a thorough understanding of anatomy.
Regulatory bodies like the FDA in the United States regulate the *devices* used to process blood for PRF (like centrifuges and collection kits), ensuring they meet safety and quality standards for their intended use (e.g., processing blood components). While PRF itself, as a biologic product used off-label for many aesthetic indications, isn’t given a specific “FDA approval” for these uses in the same way a drug or medical device would be, its safety profile is widely accepted and supported by clinical use and studies.
In conclusion, PRF stands out as a remarkably safe regenerative treatment option due to its 100% natural, autologous composition and minimally invasive application. For the vast majority of suitable candidates, the potential benefits of stimulating natural regeneration far outweigh the minimal, transient risks associated with the procedure itself.
Are there any side effects with PRF treatment?
Yes, while Platelet Rich Fibrin (PRF) treatment is exceptionally safe due to its autologous nature, there are potential side effects, although they are typically mild, temporary, and directly related to the delivery method, primarily injections. These side effects are standard considerations for any procedure involving needle entry into the skin.
The most common side effects patients may experience include:
-
- Swelling (Edema): It’s very common to experience mild to moderate swelling at the injection sites immediately after the procedure. This is partly due to the volume of the injected PRF and partly the body’s natural inflammatory response kicking off the healing process. Swelling is usually most noticeable in areas where more volume was injected or where the tissue is naturally prone to swelling (like the under-eyes). It typically subsides significantly within 24-48 hours.
-
- Bruising (Ecchymosis): Bruising is a potential side effect whenever a needle is used to puncture the skin and tissue. A small blood vessel can be inadvertently nicked, leading to leakage of blood into the surrounding tissue. The extent of bruising varies greatly from person to person and area to area. Some individuals bruise more easily than others. While often minor, bruising can sometimes be noticeable and may take anywhere from a few days to two weeks to fully resolve. Applying cool compresses immediately after treatment can help minimise bruising. Avoiding blood-thinning medications, supplements (like fish oil, Vitamin E, NSAIDs – *if medically cleared by your doctor*), and alcohol before the treatment can also help reduce the risk.
-
- Redness (Erythema): The treated area, especially after injections or if combined with microneedling, may appear red. This is part of the normal inflammatory response and usually subsides within a few hours to a day.
-
- Tenderness or Soreness: The injection sites or the overall treated area might feel slightly tender, sore, or sensitive to touch for 24-48 hours post-treatment. This is typically mild discomfort and can be managed with over-the-counter pain relief (acetaminophen is usually recommended, avoiding NSAIDs if advised by your practitioner).
-
- Minor Bleeding: A tiny amount of bleeding might occur at the exact moment of injection, but this stops almost immediately with slight pressure.
- Itching: Mild itching can occasionally occur during the initial healing phase as tissues regenerate.
Less common, but still possible, side effects can include:
* Small lumps or bumps at the injection site: These are usually temporary and resolve as the injected PRF integrates with the surrounding tissue. Gentle massage (if advised by your practitioner) might help. Persistent or painful nodules should be reported to your practitioner.
* Skin discoloration (Hemosiderin Staining): In rare cases, particularly with bruising under the thin skin of the eyes, iron from broken down red blood cells can be left behind, causing a brownish staining. This is uncommon with PRF (less likely than with traditional fillers that sit for a long time) and often resolves over several months, but can be persistent in very rare instances.
More serious complications like infection, nerve injury, or vascular compromise are exceedingly rare with PRF treatments performed by qualified practitioners adhering to strict sterile protocols and proper injection techniques.
In summary, while serious side effects are rare, it is common to experience mild and temporary side effects like swelling, bruising, redness, and tenderness after PRF treatment, particularly when injections are involved. These are typically manageable and resolve spontaneously within a short timeframe, making the downtime for PRF treatment generally minimal. Always discuss expected side effects and how to manage them with your practitioner before the procedure.
Are there any side-effects?
Absolutely, as with nearly any medical or aesthetic intervention, there are potential side-effects associated with Platelet Rich Fibrin (PRF) treatment, although they are typically minor and transient. It’s important to understand what might occur, even if the treatment is considered very safe overall due to its autologous nature. The side-effects of PRF treatment stem overwhelmingly from the physical action of drawing blood and administering the PRF via injections or topical application, rather than adverse reactions to the biological material itself.
The most frequently encountered side-effects are localized to the treatment area and include:
-
- Temporary Swelling: Mild to moderate puffiness is quite common immediately following PRF injections. This is a combination of the volume of the fluid/gel injected and the initiation of the body’s inflammatory response. It typically resolves within 24-48 hours.
-
- Bruising: Bruising at the injection sites is a possibility. Needles can puncture small blood vessels, leading to leakage of blood into the surrounding tissue. The degree of bruising is highly variable and depends on individual factors, the treatment area (areas with more blood vessels or thinner skin like the under-eyes are more prone), and the practitioner’s technique. Bruises can range from small dots to larger discolored areas and may take up to two weeks to fade completely.
-
- Redness: The skin in the treated area, especially after microneedling combined with PRF or after numerous injections, may appear red and flushed. This is a normal part of the body’s inflammatory healing response and usually diminishes significantly within a few hours or by the next day.
-
- Tenderness or Mild Pain: The injection sites may feel sore, tender, or slightly achy for a day or two after treatment. This is usually mild and manageable and indicates the tissues are responding to the treatment stimulus.
-
- Itching: As the healing process progresses, some patients might experience mild itching in the treated area.
- Small bumps or irregularities: Occasionally, tiny bumps might be palpable or visible at injection points. These are usually temporary and related to the injected material settling or minor swelling. They should resolve within a few days or weeks. If they persist or are painful, you should contact your practitioner.
More serious adverse effects are exceedingly rare but are worth mentioning as theoretical possibilities with any injection:
-
- Infection: Although rare with sterile technique, any break in the skin barrier carries a minimal risk of bacterial infection.
-
- Nerve damage: Extremely rare, particularly in aesthetic procedures when performed by an experienced practitioner with good anatomical knowledge.
- Vascular complications: An incredibly rare event where injected material obstructs a blood vessel. This is the basis of the extremely rare concern about blindness with certain facial injections. Experienced injectors use techniques to mitigate this risk.
In summary, while PRF itself is inherently safe as it comes from your own body, the process of administering it via injection can lead to common, mild, and temporary side effects such as swelling, bruising, redness, and tenderness. These are expected parts of the post-treatment experience and indicate the body is beginning its healing process. Severe side effects are exceptionally uncommon when treatments are performed by qualified professionals.
What are the risks of PRF?
When discussing the risks of Platelet Rich Fibrin (PRF) treatment, it’s important to differentiate between common, transient side effects and rare, potential complications. While the treatment is generally very safe due to its autologous nature, understanding the full spectrum of potential outcomes is part of informed consent.
The most common “risks” are actually the expected, temporary side effects already discussed:
* Bruising
* Swelling
* Redness
* Tenderness/Soreness
* Minor bleeding at injection site
* Temporary bumps/irregularities
These are risks in the sense that they are undesirable outcomes, but they are typically mild, temporary, and resolve on their own within a short period, representing the body’s normal response to injection and the initiation of healing.
The truly potential risks, which are rare to extremely rare, are associated with the medical procedure of blood draw, processing, and injection:
1. Infection: Any time a needle penetrates the skin, there is a theoretical risk of introducing bacteria and causing an infection. This risk is extremely low in a clinical setting with strict adherence to sterile protocols (using disinfected skin, sterile needles, tubes, and syringes, and performing the procedure in a clean environment).
2. Nerve Injury: Injecting material near a nerve could potentially cause temporary or, in extremely rare cases, permanent nerve damage, leading to numbness, tingling, or weakness in the affected area. This risk is minimised by the practitioner’s detailed knowledge of anatomy and careful injection technique, particularly in areas where nerves are more superficial.
3. Vascular Compromise / Intravascular Injection: This is a very rare but potentially serious risk with any facial injection. It occurs when the injected material inadvertently enters a blood vessel and blocks it, potentially leading to tissue death (necrosis) or, in exceptionally rare cases near the eyes or nose, vision loss or blindness if the vessel connects to the retinal artery. While PRF is a natural substance, it is still a material that could block a vessel. Experienced practitioners use specific techniques to avoid this, such as aspirating before injecting to check if they are in a vessel, injecting slowly, using cannulas (blunt-tipped instruments) in certain areas, and having a thorough understanding of vascular anatomy.
4. Unsatisfactory Results: While not a medical safety risk, the outcome of the treatment might not meet the patient’s expectations. This could be due to factors like the patient’s individual response, the severity of the condition treated (some issues may require more intensive treatment), or suboptimal technique. Realistic expectations, thorough consultation, and choosing a skilled provider help mitigate this risk.
5. Formation of Scar Tissue or Fibrosis: While PRF is used to *improve* scarring, improper technique or excessive treatment could theoretically lead to unwanted fibrous tissue formation, though this is not a common complication of PRF itself.
6. Hair Shedding (Telogen Effluvium): When treating the scalp for hair loss, there is a rare possibility of experiencing a temporary increase in hair shedding in the initial weeks or months after treatment before regrowth begins. This is usually temporary and indicates follicles are transitioning cycles.
To mitigate these risks, it is absolutely paramount to seek treatment from a qualified medical professional (such as a dermatologist, plastic surgeon, physician assistant, or nurse practitioner supervised by a physician) who has specific training and extensive experience in performing PRF treatments and facial injections. They are equipped to handle the procedure safely, recognise potential issues, and manage them appropriately.
What are the disadvantages of PRF?
While Platelet Rich Fibrin (PRF) treatment offers numerous benefits and boasts an excellent safety profile, it’s important to consider potential disadvantages or limitations to have a balanced perspective and determine if it’s the right treatment for your specific needs and expectations.
Here are some potential disadvantages of PRF:
-
- Requires Multiple Sessions: Unlike some treatments that might offer noticeable results in a single session (like a temporary filler), PRF is fundamentally a regenerative therapy. Its effects build gradually over time. Consequently, a single PRF session is often insufficient to achieve optimal results for most conditions. A series of treatments (typically 2-4 sessions spaced weeks apart) is usually recommended. This means a longer commitment in terms of time and, importantly, financial investment compared to a one-off treatment.
-
- Results Are Gradual, Not Immediate: If you’re looking for instant gratification or a dramatic, immediate change, PRF is likely not the best choice as a standalone treatment. The regenerative process it stimulates takes time, and visible improvements unfold over weeks and months as new collagen, elastin, and blood vessels are formed. While some subtle temporary volume might be seen with PRF gel, it does not provide the immediate structural correction or volume of synthetic fillers.
-
- Results Vary Individually: The effectiveness of PRF treatment can vary from person to person. Because it relies on stimulating your body’s own biological processes, the outcome is influenced by your individual healing capacity, age, overall health, genetics, and lifestyle. While most people see positive results, the degree of improvement can differ, and there’s no guaranteed outcome.
-
- Not a Solution for Severe Volume Loss or Skin Laxity: While PRF can improve skin quality and provide subtle volume and firmness, it is not a substitute for procedures designed to address significant volume depletion (like robust dermal fillers) or severe skin laxity (like surgical lifts). It works best for mild to moderate concerns or as an adjunct to other treatments for more severe issues.
-
- Potential for Minor Side Effects: While not severe, the potential for temporary side effects like bruising, swelling, and redness can be inconvenient for some individuals, requiring a few days of social downtime depending on the severity.
-
- Cost: As discussed, a full series of PRF treatments represents a notable financial investment, potentially costing several thousand dollars. While less expensive than surgery, it is generally more costly than basic non-invasive treatments.
-
- Requires Blood Draw: While a simple and safe procedure, some individuals have an aversion to blood draws or needles. PRF therapy requires drawing blood at the start of every session.
- Availability and Practitioner Expertise: While growing in popularity, PRF treatment, particularly using advanced protocols, may not be available in all clinics. Finding a practitioner with extensive experience and specific training in PRF preparation and application techniques is crucial for safety and optimal results, and such practitioners may not be readily accessible in all areas, or their services may be more costly.
Considering these potential disadvantages alongside the significant benefits is essential for making an informed decision about whether PRF treatment aligns with your expectations, timeline, and budget, and whether it’s the most appropriate solution for your specific concerns.
Can PRF go wrong?
While Platelet Rich Fibrin (PRF) treatment is widely regarded as very safe, particularly due to its autologous nature, like any medical procedure, there are instances where things might not go exactly as hoped, or rare complications could occur. So, yes, theoretically, PRF *can* “go wrong,” though serious adverse events are uncommon when the procedure is performed correctly by a qualified professional.
When people ask if PRF can “go wrong,” they are typically concerned about:
1. Lack of Expected Results (Unsatisfactory Outcome): This is perhaps the most common way a treatment might feel like it “went wrong” from a patient’s perspective. The results achieved might be less significant than anticipated or hoped for. This could happen for several reasons:
* Individual Response: Some people’s bodies may not respond as strongly to the regenerative stimulus as others, perhaps due to age, underlying health conditions, or genetics.
* Severity of Condition: PRF might not be powerful enough as a standalone treatment for very severe issues (e.g., deep wrinkles, significant volume loss, advanced hair loss).
* Incorrect Treatment Plan: The number or frequency of sessions might have been insufficient for the desired outcome.
* Suboptimal PRF Preparation: If the blood draw, handling, or centrifugation protocol is not followed precisely, the resulting PRF might not contain the optimal concentration of platelets, leukocytes, and growth factors, reducing its effectiveness.
* Improper Application/Injection Technique: Injecting PRF into the wrong tissue layer or distributing it unevenly can compromise the results.
2. Exacerbation of Problem (Very Rare): While extremely rare, in the context of hair loss, some individuals might experience temporary increased shedding (telogen effluvium) before regrowth begins, which can feel like the problem is worsening initially. This is usually a temporary phase.
3. Complications Related to the Procedure: Although rare, the potential risks discussed previously could be considered things “going wrong”:
* Infection: If sterile technique is compromised, infection at the treatment site is a serious complication.
* Significant Bruising or Swelling: While minor effects are common, severe or prolonged bruising/swelling could occur in rare instances, potentially leading to discomfort and longer downtime.
* Lumps or Nodules: Persistent or painful lumps can sometimes occur, though usually temporary.
* Nerve or Vascular Injury: As mentioned, extremely rare but serious risks, particularly intravascular injection, which is a significant concern in areas like the face.
4. Allergic Reaction (Extremely, Extremely Rare): While PRF is autologous, some protocols *might* involve the addition of minimal substances (though most modern protocols avoid this). Even theoretically, a reaction to a component in the processing tube or a topical product used could occur, though reactions to the PRF itself are virtually non-existent.
To minimise the chances of things “going wrong,” especially regarding safety and achieving satisfactory results, the most critical step is selecting a highly qualified, experienced, and reputable practitioner who uses proper protocols and maintains strict sterile standards. They can accurately assess your needs, create a realistic treatment plan, perform the procedure safely, and manage any potential issues that may arise. A thorough consultation is also essential to ensure your expectations align with what PRF can realistically achieve.
PRF Treatment Safety – What to Expect
When undergoing Platelet Rich Fibrin (PRF) treatment, you should expect a strong emphasis on safety protocols from the moment you step into a reputable clinic. Your safety is paramount, and understanding the measures taken, as well as what to expect in terms of post-treatment sensations, is key to a comfortable experience. While PRF is exceptionally safe due to its autologous nature, the procedure involves medical steps that require adherence to strict standards.
Safety Measures You Can Expect:
-
- Thorough Consultation: Expect a detailed medical history review to identify any potential contraindications (though contraindications for PRF itself are minimal, related mostly to blood disorders or active infections). Your practitioner will discuss your health status to ensure PRF is suitable.
-
- Sterile Environment: The procedure will be performed in a clean, clinical setting designed for medical procedures.
-
- Strict Aseptic Technique: Expect the practitioner and assisting staff to adhere to strict sterile protocols throughout the entire process. This includes cleaning the blood draw site and the treatment area meticulously with antiseptic solutions, using sterile, single-use needles, syringes, tubes, and gloves. The PRF processing in the centrifuge is done in a way that maintains the sterility of the final product.
-
- Qualified Personnel: Blood will be drawn by a trained professional (phlebotomist, nurse, or physician). The PRF processing and application/injection will be performed by a licensed medical practitioner (physician, physician assistant, nurse practitioner) with specific training and experience in PRF therapy and the relevant anatomical area being treated.
- Anatomical Knowledge & Safe Injection Techniques: If injections are involved, expect the practitioner to have a detailed understanding of the underlying anatomy of the treatment area. They will use techniques designed to minimise risks, such as choosing appropriate needle or cannula types, injecting at correct depths, and potentially aspirating before injecting in certain areas to avoid blood vessels.
What to Expect Post-Treatment (Normal & Expected Side Effects):
After the treatment, you should expect and be prepared for the following, which are considered normal side effects and indicate the treatment is initiating a healing response:
-
- Temporary Swelling: Mild puffiness at the injection or treatment site. This usually resolves within 1-2 days.
-
- Temporary Redness: The treated area may look flushed for a few hours to a day.
-
- Temporary Bruising: Some bruising is common. It can range from mild spots to more noticeable discolouration and may take up to two weeks to resolve.
-
- Temporary Tenderness/Soreness: Mild discomfort upon touching the treated area for a day or two.
- Temporary Bumps or Irregularities: Small, palpable bumps at injection sites that usually flatten out within days or a couple of weeks as the PRF integrates.
These expected side effects are generally manageable with simple aftercare like cool compresses and over-the-counter pain relief (if necessary) and typically require minimal downtime. Severe side effects are rare. You should receive clear instructions on post-treatment care and know who to contact if you have any concerns or experience unexpected symptoms. In essence, expect a safe, well-controlled procedure with predictable, temporary minor side effects, allowing for a relatively quick return to normal activities.
Can PRF cause blindness?
The concern about blindness in relation to aesthetic injections, while extremely rare, is a serious one that primarily pertains to injections performed in certain areas of the face, particularly around the eyes, nose, and forehead. This rare complication occurs if injectable material is inadvertently injected into a blood vessel (intravascular injection) that is connected to the arterial supply of the eye (specifically, branches of the ophthalmic artery). If the material blocks blood flow through this vessel, it can lead to a lack of oxygen supply to the retina or optic nerve, potentially causing vision loss or, in the most severe cases, blindness.
So, *theoretically*, could PRF cause blindness if injected into a vessel supplying the eye? Yes, because PRF is a material that, if injected intravascularly into a critical vessel, could potentially block blood flow. The risk is not due to the *nature* of PRF itself (it’s not toxic or inflammatory in a way that directly damages the eye), but due to its *physical presence* potentially causing a vascular occlusion (blockage).
However, it is absolutely crucial to emphasize that **blindness as a complication of facial injections, including PRF, is exceedingly rare.** The risk is minimal when the procedure is performed by a highly trained, experienced practitioner who has a thorough understanding of facial anatomy, particularly the complex vascular network in areas like the periorbital (around the eye) and nasal regions.
Experienced practitioners take significant precautions to mitigate this risk, especially when injecting near the eyes:
* Expert Anatomical Knowledge: Understanding the location and path of key blood vessels.
* Aspiration: Before injecting, the practitioner may pull back on the syringe plunger (aspirate) to see if blood enters the syringe, which would indicate the needle tip is inside a blood vessel. While not foolproof, this is a safety measure.
* Using Cannulas: In higher-risk areas, many practitioners prefer to use blunt-tipped cannulas instead of sharp needles. Cannulas are less likely to pierce blood vessels and tend to push them aside instead, significantly reducing the risk of intravascular injection.
* Slow Injection Speed & Low Pressure: Injecting slowly and using minimal pressure.
* Injecting in Correct Tissue Plane: Ensuring the material is injected into the appropriate layer (e.g., subcutaneous or supraperiosteal, depending on the treatment goal and area) and not into vessels.
While the theoretical risk exists with *any* injectable material (fillers, fat, PRP, PRF) in certain high-risk areas, it is not a common or expected outcome of PRF treatment. The risk is minimised to an almost negligible level when the procedure is performed by a highly skilled, experienced, and reputable practitioner who prioritises patient safety and employs best practices for injection techniques in anatomically sensitive areas. Always choose your provider wisely.
Is PRF injection under the eye safe?
PRF injection under the eye is considered safe and is a very popular and effective application for rejuvenating this delicate area, provided it is performed by a qualified, experienced practitioner with specific expertise in treating the periorbital region. While the under-eye area is anatomically sensitive and requires careful technique, PRF is particularly well-suited for this zone due to its natural composition and regenerative properties.
Here’s why it’s considered safe for this area:
-
- Autologous Material: As with all PRF treatments, using the patient’s own blood product dramatically reduces the risks of allergic reactions, rejection, or inflammatory responses often seen with synthetic fillers in this thin-skinned area. This is a significant advantage for the under-eyes, which can be prone to sensitivity and chronic swelling or reactions from foreign substances.
-
- Regenerative Properties: PRF stimulates the production of new collagen, elastin, and blood vessels. This helps to thicken the thin skin under the eyes, improve circulation (which can reduce dark circles caused by visible blood vessels), and improve overall skin quality and firmness. This regenerative effect addresses the underlying issues causing concerns like hollowness and lines, rather than just physically filling space.
-
- Subtle, Natural Results: PRF provides subtle, natural volume and regeneration, which is ideal for the delicate under-eye area where an overfilled or unnatural look is highly undesirable.
- Use of PRF Gel: For under-eye hollowness, PRF is often processed into a gel-like consistency (injectable PRF gel). This gel provides a softer, more integrated type of fill compared to some denser fillers, which can look unnatural or cause bluish discoloration (Tyndall effect) under thin skin.
However, the safety is highly dependent on the skill and experience of the injector. The under-eye area has complex anatomy with delicate blood vessels and nerves. A practitioner must:
-
- Have a detailed understanding of the vascular and neural anatomy of the periorbital region.
-
- Use appropriate injection techniques, such as injecting slowly, using small volumes per injection point, and injecting in the correct tissue plane (often deep, near the bone, or intradermally depending on the specific concern).
-
- Consider using a blunt-tipped cannula instead of a sharp needle. Cannulas are generally safer in areas with numerous blood vessels as they are less likely to pierce them, significantly reducing the risk of bruising, swelling, and the extremely rare but serious complication of vascular occlusion that could lead to blindness.
- Adhere strictly to sterile protocols.
The rare concern about blindness associated with facial injections is theoretically possible in this area if material is injected into a vessel connected to the eye’s blood supply. However, with proper technique and precautions taken by an experienced professional, the risk is minimal.
In conclusion, PRF injection under the eye is a safe and effective regenerative treatment when performed by a highly skilled practitioner. The natural material minimises risks compared to synthetic alternatives, and the technique focuses on stimulating natural rejuvenation. Choosing your provider carefully is the most important factor in ensuring safety for this delicate treatment area.
Is PRF filler safe?
When discussing “PRF filler,” it’s important to clarify what is meant. Standard Platelet Rich Fibrin (PRF) is not a filler in the traditional sense like hyaluronic acid (HA) or calcium hydroxylapatite fillers, which are designed primarily to provide immediate, structural volume. However, PRF can be processed in a way that creates a more gel-like consistency, often referred to as Injectable PRF Gel or sometimes colloquially as “PRF filler,” particularly when it’s used to add subtle volume, for example, under the eyes or in other areas of mild volume loss. This PRF Gel is created by gently heating liquid PRF after centrifugation, causing the fibrin matrix to solidify into a mouldable gel.
Considering this injectable PRF Gel used for subtle volume and regeneration, is it safe? Yes, injectable PRF Gel is considered very safe, benefiting from the same excellent safety profile as standard liquid PRF due to its autologous nature.
Here’s why Injectable PRF Gel is safe:
-
- 100% Autologous: Like regular PRF, the gel is made solely from the patient’s own blood components (platelets, leukocytes, fibrin). No synthetic additives, cross-linking agents (like those in HA fillers), or foreign materials are used to create the gel structure. This eliminates the risk of allergic reactions, foreign body responses, or rejection that can sometimes occur with synthetic fillers.
-
- Biocompatible and Biodegradable: The fibrin gel matrix is a natural component of the body and is fully biocompatible. Once injected, it is naturally, slowly, and completely absorbed by the body over time as it releases its encapsulated growth factors and cells. It doesn’t remain as a foreign substance long-term.
-
- Regenerative Function: While providing subtle volume, the PRF Gel simultaneously releases growth factors that stimulate the surrounding tissues to produce new collagen, elastin, and blood vessels. This means it not only provides a temporary fill but also works to improve the underlying tissue quality.
- Minimised Risk of Lumps/Irregularities (Compared to some fillers): Due to its natural composition and integration with tissue, PRF Gel tends to provide a very smooth, natural feel and appearance. While temporary bumps can occur at injection sites, the risk of forming persistent, noticeable lumps or irregularities can be lower compared to some denser synthetic fillers, especially when injected superficially.
The potential risks associated with injecting PRF Gel are the same general risks associated with any injection procedure, as discussed earlier: temporary swelling, bruising, redness, tenderness, and the extremely rare risks of infection, nerve injury, or vascular compromise.
The *technique* of injecting PRF Gel is also critical for safety and optimal results, particularly in delicate areas like the under-eyes. An experienced practitioner knows how to handle and inject the gel properly to ensure smooth, even placement and avoid complications.
In summary, yes, injectable PRF Gel is a safe option for providing subtle volume and stimulating regeneration, particularly appealing for areas like the under-eyes or for addressing mild volume loss where a very natural result is desired. Its safety stems directly from its autologous origin, making it highly biocompatible and well-tolerated by the body, with risks primarily limited to the injection process itself when performed by a qualified professional.
Who Is a Good Candidate for PRF Treatment?
Identifying who is a good candidate for Platelet Rich Fibrin (PRF) treatment involves assessing an individual’s overall health, their specific concerns, and their expectations for the outcome. Because PRF therapy relies on the body’s natural healing and regenerative capacity, the ideal candidate is generally someone in good overall health with a functional immune system and healthy blood. This is crucial because the success of the treatment depends on the ability of the patient’s body to produce sufficient quantities of healthy platelets, leukocytes, and fibrin and to respond effectively to the regenerative signals released from the PRF.
Individuals who have specific aesthetic or regenerative concerns that PRF is known to effectively address are prime candidates. This includes people looking to:
-
- Improve skin texture, tone, and elasticity, particularly addressing fine lines and wrinkles.
-
- Reduce the appearance of mild to moderate skin laxity.
-
- Improve the appearance of scars, such as acne scars or certain surgical scars.
-
- Address dark circles and mild to moderate hollowness under the eyes.
-
- Stimulate hair growth in areas of thinning or hair loss (often due to androgenetic alopecia or other non-scarring alopecias).
- Accelerate healing and regeneration in specific medical contexts, such as after dental procedures, for chronic wounds, or certain musculoskeletal injuries.
A good candidate should also have realistic expectations about the results and the timeline. PRF treatment delivers gradual, natural improvements and often requires a series of sessions to achieve optimal outcomes. It’s not a magical cure or an overnight transformation, and it doesn’t provide the dramatic structural change of surgery or the immediate, significant volume of certain synthetic fillers. Candidates who understand and are comfortable with this process are typically more satisfied with their results.
Furthermore, individuals who prefer a natural, minimally invasive approach to rejuvenation and healing are excellent candidates for PRF. The autologous nature of the treatment appeals greatly to those who wish to avoid introducing synthetic substances into their bodies.
Ideal candidates should also be able to adhere to pre- and post-treatment instructions, such as staying hydrated before the blood draw and following aftercare guidelines regarding activity levels, sun exposure, and skincare.
In summary, a good candidate for PRF treatment is a healthy individual seeking natural, gradual improvement for specific aesthetic or regenerative concerns that fall within PRF’s scope of effectiveness, who has realistic expectations about the process and results, and is comfortable with a minimally invasive procedure utilizing their own blood. A thorough consultation with a qualified practitioner is the best way to confirm if you are a suitable candidate based on your unique circumstances and goals.
Who is a candidate for PRF?
Broadly speaking, a candidate for Platelet Rich Fibrin (PRF) treatment is any individual who can benefit from the stimulation of their body’s natural healing and regenerative processes, provided they meet certain baseline health requirements. The candidacy extends across various age groups and genders, focusing more on the specific issue being addressed and the patient’s physiological ability to respond to treatment.
Key characteristics that define a potential candidate include:
-
- Adequate Platelet Count and Healthy Blood: Since the treatment relies on concentrating platelets and other blood components, individuals must have a healthy blood profile without significant blood disorders, active infections, or conditions that affect platelet function or count (e.g., certain types of anaemia, platelet dysfunction syndromes). A practitioner will assess your medical history to ensure your blood is suitable for processing.
-
- Specific Aesthetic Concerns: Individuals seeking improvement in skin quality (texture, tone, elasticity), reduction of fine lines and wrinkles, treatment of mild to moderate scars (like acne scars), or management of under-eye issues (dark circles, hollowness, crepey skin) are common aesthetic candidates.
-
- Hair Loss Concerns: Individuals experiencing early to moderate stages of non-scarring hair loss, such as androgenetic alopecia (male or female pattern baldness), are often good candidates for scalp PRF injections aimed at stimulating follicular activity.
-
- Medical Needs: Patients requiring enhanced healing in specific areas, such as post-dental surgery (extractions, implants, bone grafts), for chronic non-healing wounds, or for certain musculoskeletal injuries (tendinopathy, osteoarthritis) can be medical candidates.
-
- Good General Health: While not requiring perfect health, candidates should generally be well and free from acute illnesses or severe chronic diseases that could impair their healing capacity or make the procedure unsafe.
-
- Non-Smokers or Willing to Reduce Smoking: Smoking impairs circulation and healing, which can negatively impact the results of PRF treatment. Non-smokers or those willing to significantly reduce or quit smoking will generally see better outcomes.
- Not Pregnant or Breastfeeding: As with many aesthetic procedures, PRF is generally avoided during pregnancy and breastfeeding due to a lack of safety data in these populations.
It’s also important for candidates to understand that PRF works synergistically with the body. Conditions or medications that suppress the immune system or interfere with clotting/healing may affect the outcome.
Ultimately, the best way to determine candidacy is through a thorough consultation with a qualified practitioner who can review your full medical history, perform a physical assessment of the area to be treated, and discuss whether PRF is the most appropriate and likely effective treatment option for your specific situation. They will ensure you meet the necessary health criteria for undergoing the procedure safely and effectively.
Who’s a Good Candidate for PRF Injections?
Focusing specifically on PRF injections, the criteria for a good candidate align closely with the general criteria for PRF treatment, but with particular emphasis on the suitability for an injectable procedure and the specific concerns injections are best poised to address. A good candidate for PRF injections is someone looking for targeted regeneration and improvement in specific tissues or areas, delivered via needle or cannula.
Key characteristics of a good candidate for PRF injections include:
-
- Suitability for Injection Procedures: While minimally invasive, injections involve needles. A good candidate should be comfortable with the idea of injections, although measures like topical numbing creams are used to minimise discomfort. They should not have a severe needle phobia.
-
- Specific, Localized Concerns: PRF injections are ideal for targeting defined areas. This includes:
* Fine lines and wrinkles (e.g., crow’s feet, smile lines, perioral lines).
* Under-eye issues (dark circles, mild hollowness, crepey skin).
* Acne scars or other depressed scars.
* Areas of mild volume loss where a natural, subtle fill is desired alongside regeneration (e.g., using PRF gel).
* Specific joints, tendons, or ligaments with injury or degeneration (in medical applications).
* Specific areas of the scalp for hair thinning.
- Specific, Localized Concerns: PRF injections are ideal for targeting defined areas. This includes:
-
- Desire for Natural, Gradual Improvement: Candidates who appreciate and prefer results that develop subtly over time, powered by their body’s own biology, are well-suited for PRF injections. They are not seeking immediate, dramatic structural changes.
-
- Patience and Commitment to a Series: Optimal results from PRF injections typically require a series of treatments. Good candidates are prepared for the commitment of multiple sessions and understand that patience is required to see the full benefits unfold over several months.
-
- Good Skin Quality (Relative to Age): While PRF improves skin quality, candidates with overly thin, severely damaged skin (e.g., severe sun damage) or extremely poor healing capacity due to systemic issues might have a less pronounced response. PRF often works best on skin that still has some inherent regenerative capacity.
-
- Free from Active Skin Infections in the Treatment Area: Any active infection (bacterial, viral like herpes simplex) in or near the planned injection site would be a contraindication until resolved, to prevent spreading the infection.
- Not on Certain Medications: Individuals on high doses of systemic corticosteroids or certain immunosuppressants might have impaired healing responses. Those on strong anticoagulants may be at higher risk of significant bruising or bleeding (though this needs careful medical assessment).
In essence, a good candidate for PRF injections is someone seeking targeted, natural regeneration for specific aesthetic or medical issues that are responsive to local growth factor delivery, who is in reasonably good health, has realistic expectations, and is prepared for a course of treatment. A consultation remains the definitive step to assess individual suitability and tailor a treatment plan.
Am I a candidate for treatment with PRF?
To determine definitively if *you* are a candidate for treatment with Platelet Rich Fibrin (PRF), the most crucial step is to schedule a consultation with a qualified medical or aesthetic practitioner who offers the treatment. While the general criteria provide a framework, a personalized assessment is necessary to evaluate your specific situation.
During a consultation, the practitioner will:
1. Review Your Medical History: They will ask about your past and current health conditions, medications (prescription and over-the-counter), allergies, and any previous cosmetic procedures. This is to identify any potential contraindications or factors that could affect the safety or outcome of the treatment, such as blood disorders, active infections, certain autoimmune conditions, or medications that impact blood clotting or healing.
2. Discuss Your Concerns and Goals: You’ll have the opportunity to explain exactly what aesthetic issue (e.g., under-eye circles, hair thinning, wrinkles) or medical condition (e.g., joint pain, slow-healing wound) you want to address. The practitioner will assess whether PRF is a suitable treatment option for your specific concern and discuss what results can realistically be achieved.
3. Examine the Treatment Area: The practitioner will physically examine the area you wish to treat. For example, they might assess your skin quality, the type and severity of your wrinkles or scars, the pattern and extent of your hair loss, or the condition of your joint. This helps them determine if PRF is appropriate and to plan the optimal treatment approach (e.g., injection depth, volume needed).
4. Evaluate Your Overall Health: A general assessment of your health status helps ensure you are fit for the procedure, including the blood draw and healing process.
5. Manage Expectations: The practitioner will provide you with realistic information about the expected results, the number of sessions likely needed, the timeline for seeing results, the longevity of the benefits, and potential side effects. They will ensure you understand that PRF provides natural, gradual improvements.
Based on this comprehensive assessment – your health, your specific concerns, and the practitioner’s expertise – they will be able to tell you whether you are a good candidate for PRF treatment and if it is the most appropriate option to help you achieve your goals. They can also explain the specific type of PRF preparation and application technique that would be best suited for your needs. Don’t hesitate to ask questions during this consultation; it’s your opportunity to gather all the information you need to make an informed decision about your treatment journey.
Ideal Candidates for PRF Treatment
The concept of an “ideal” candidate for PRF treatment narrows down the broader pool of potential candidates to those who are most likely to experience significant benefits and be highly satisfied with their outcomes. These individuals typically possess a combination of specific characteristics that make PRF a particularly well-suited and effective choice for them.
Ideal candidates for PRF treatment often are:
1. Individuals in Good Health with Robust Healing Capacity: The most ideal candidate has a healthy immune system, no significant blood disorders, and no underlying medical conditions (like uncontrolled diabetes or severe autoimmune disease) that could significantly impair their body’s ability to heal and regenerate tissues effectively. Their body is primed to respond optimally to the regenerative signals.
2. Seeking Natural, Subtle, and Gradual Improvements: Someone who values a very natural look and prefers treatments that work *with* their body to stimulate regeneration, rather than relying on synthetic materials for immediate, dramatic changes, is an ideal fit for PRF’s mechanism of action and timeline of results.
3. Addressing Mild to Moderate Concerns: PRF is typically most effective for addressing mild to moderate signs of aging (fine lines, mild laxity), early to moderate stages of hair thinning, mild to moderate scarring, or localized areas needing enhanced healing. While it can provide some benefit for more severe issues, the results may be less pronounced as a standalone treatment, and the ideal candidate’s concerns fall squarely within PRF’s sweet spot.
4. Prepared for a Series of Treatments: Ideal candidates understand that PRF is usually a process requiring multiple sessions to build cumulative results. They are patient and committed to completing the recommended treatment course.
5. Willing to Follow Pre and Post-Treatment Instructions: Adhering to guidelines regarding hydration, avoiding certain substances, and following aftercare instructions (like sun protection and avoiding strenuous activity) helps optimise results and minimise side effects. An ideal candidate is compliant with these recommendations.
6. Non-Smokers: While smokers can technically receive PRF, smoking severely compromises circulation and healing, significantly reducing the potential effectiveness and longevity of the results. A non-smoker is therefore an ideal candidate for maximizing treatment benefits.
7. Seeking Long-Term Tissue Health: Ideal candidates are interested in not just temporary cosmetic fixes but in improving the fundamental health and regenerative capacity of their tissues for more enduring benefits.
In essence, the ideal candidate is a healthy, compliant individual with realistic expectations, whose specific concerns are well-matched to PRF’s regenerative capabilities, and who values a natural, gradual approach to rejuvenation and healing, committing to the process required for optimal results. A consultation will confirm if you align with these characteristics.
Who is not a candidate for PRF?
While PRF treatment is remarkably safe and suitable for many people, there are specific conditions and circumstances that would make an individual *not* a candidate for the therapy, either for safety reasons or because the treatment is unlikely to be effective. It’s crucial for practitioners to screen potential candidates thoroughly to identify these contraindications.
Individuals who are generally *not* candidates for PRF treatment include:
1. Individuals with Platelet Dysfunction Syndromes: Since PRF relies on healthy, functional platelets, any disorder that affects the number or function of platelets (e.g., thrombocytopenia, qualitative platelet defects) would make someone unsuitable, as their blood would not yield effective PRF.
2. Individuals with Blood Clotting Disorders: While PRF promotes clotting *in situ* via fibrin, individuals with significant systemic clotting disorders, especially those on strong anticoagulant medications (blood thinners, although temporary cessation *might* be possible under strict medical supervision for some), may not be ideal candidates due to potential risks of bleeding or compromised PRF formation.
3. Individuals with Active Infections: Any active infection, whether localized in the treatment area (e.g., active acne breakouts, cold sores, skin infections) or systemic (e.g., fever, flu), is a contraindication. Introducing needles into an infected area can spread the infection, and systemic infection can compromise the body’s healing response. Treatment should be postponed until the infection is fully cleared.
4. Individuals with Chronic Liver Disease: Severe liver disease can affect clotting factors and overall health, potentially impacting the body’s ability to heal and produce necessary blood components for PRF.
5. Individuals with Certain Cancers or Undergoing Chemotherapy/Radiation: Active cancer, particularly blood cancers, or undergoing aggressive chemotherapy or radiation therapy can significantly impair the body’s healing capacity, blood cell production, and immune function, making PRF treatment unsuitable. A history of certain cancers might also be a contraindication; this requires careful medical assessment.
6. Individuals with Severe Systemic Diseases: Uncontrolled diabetes, severe autoimmune diseases, or other significant systemic health issues that compromise the immune system or healing response may make someone a poor candidate or require careful management and assessment before treatment.
7. Individuals Taking Certain Medications: While some medications are minor concerns (like NSAIDs slightly increasing bruising risk), high doses of chronic systemic corticosteroids can significantly suppress the immune system and impair healing, often making someone unsuitable for regenerative therapies like PRF.
8. Pregnant or Breastfeeding Women: For safety reasons and due to a lack of specific studies in these populations, PRF is generally contraindicated during pregnancy and breastfeeding.
9. Individuals with Unrealistic Expectations: While not a medical contraindication, individuals who expect immediate, dramatic results or believe PRF is a permanent cure-all may not be satisfied and are often considered unsuitable unless expectations can be appropriately managed during consultation.
Any of these conditions or circumstances would typically rule out PRF treatment. A thorough medical history taken by a qualified practitioner is essential to identify individuals who are not suitable candidates and ensure treatment is safe and appropriate.
Who is not a candidate for PRF injections?
Beyond the general contraindications for PRF treatment itself (as discussed above, related to blood health, active infection, severe systemic disease, etc.), there are a few additional considerations that might make someone unsuitable specifically for PRF *injections*, even if they might otherwise be a candidate for PRF applied via other methods (like topical application after microneedling, though injection is the most common aesthetic use).
Reasons someone might not be a candidate for PRF injections include:
1. Severe Needle Phobia: For individuals with an extreme, debilitating fear of needles or injections, the stress and anxiety associated with the procedure might outweigh the potential benefits, even with topical numbing and a skilled practitioner. While counselling or alternative delivery methods might be explored, severe phobia is a practical contraindication for injections.
2. Skin Conditions at the Injection Site: Active inflammatory skin conditions (like eczema, psoriasis), open wounds, rashes, or severe active acne breakouts directly in the planned injection area would make injection unsafe due to the risk of exacerbating the condition or introducing infection. Treatment must be postponed until the skin is clear and healthy in the treatment zone.
3. History of Certain Scars: While PRF can improve some scars, individuals prone to hypertrophic scarring or keloid formation in the treatment area might require extra caution or may be less ideal candidates, as injections themselves could potentially trigger abnormal scar tissue formation in predisposed individuals, although this risk is generally low with fine needles.
4. Certain Anatomical Considerations (Area-Specific): While rare, some individuals might have unusual anatomical variations or previously injected materials (like permanent fillers) in the target area that could make injecting PRF more challenging, risky, or less predictable. This requires careful assessment by an experienced practitioner.
5. Recent Use of Certain Aesthetic Treatments: Depending on the area and the specific treatment, having certain procedures immediately prior to planned PRF injections might be a temporary contraindication. For example, recent use of temporary dermal fillers or certain laser treatments in the exact same area might require a waiting period, although PRF is often *combined* with treatments like microneedling or lasers for synergy, requiring careful timing.
It’s important to distinguish between general PRF contraindications (which would rule out any form of PRF) and reasons specific to the injection method. If the issue is solely related to the injection site or the patient’s comfort with needles, alternative delivery methods might be considered if available and appropriate for the condition, or another treatment modality altogether might be recommended. Again, a thorough consultation is essential to review all factors and determine the safest and most effective approach.
What Age Range Is PRF Treatment Best Suited For?
PRF treatment doesn’t have a strict age limit, and its suitability is less about hitting a specific age milestone and more about the individual’s specific needs, overall health, and the quality of their tissues and regenerative capacity. However, we can discuss the age ranges where PRF tends to be most commonly used and where individuals might see the most significant benefits.
PRF treatment is often very effective for adults generally from their late 20s or early 30s through their 70s or even older, depending on the specific application and individual health.
-
- Younger Adults (Late 20s – 40s): In this age range, PRF is often used preventatively or to address early signs of aging, improve skin quality, treat acne scars, or address early hair thinning. Younger individuals typically have more robust regenerative capabilities and higher concentrations of growth factors in their blood, meaning their tissues are often highly responsive to PRF stimulation. They might see results appear more quickly and potentially last longer (within the typical range) than older individuals. PRF can help maintain youthful skin texture and prevent the progression of early signs of aging.
-
- Middle-Aged Adults (40s – 60s): This is perhaps the most common age range for aesthetic PRF treatments. As collagen and elastin production naturally declines, fine lines, wrinkles, and mild skin laxity become more apparent. PRF is well-suited to stimulate regeneration, improve skin quality, address under-eye concerns, and treat hair loss which often becomes noticeable in these decades. Results are typically very good in this age group, helping to visibly rejuvenate the skin and slow down the aging process naturally.
- Older Adults (60s+): PRF can still be beneficial for older individuals, particularly for improving skin texture, tone, and thin, crepey skin, and aiding in medical healing applications (wound care, post-surgical). While their regenerative capacity may be somewhat diminished compared to younger individuals, PRF can still provide a valuable stimulus. The degree of aesthetic improvement in terms of significant lifting or volume correction may be less pronounced compared to younger adults or treatments specifically designed for volume, but improvements in skin quality and overall health are still achievable and often appreciated for achieving a more refreshed and revitalized look. In medical applications, PRF’s ability to accelerate healing is valuable regardless of age.
The key is not a person’s chronological age, but their biological age and health. A very healthy 70-year-old with good skin quality might respond better than a less healthy 50-year-old with extensive sun damage or underlying conditions.
In summary, while PRF can offer benefits across a wide adult age spectrum, it is perhaps best suited for individuals in their late 20s through 60s for aesthetic rejuvenation purposes, where the natural decline in regenerative capacity makes PRF’s stimulating effect particularly impactful, and where addressing mild to moderate concerns is the primary goal. However, candidacy is always determined on an individual basis through consultation, considering health and specific needs.
Who can benefit from PRF injections?
Platelet Rich Fibrin (PRF) injections are a versatile tool, and a wide range of individuals can potentially benefit from their regenerative capabilities, targeting specific aesthetic and medical concerns. The benefit comes from the precise delivery of concentrated growth factors and cells directly into the tissue that needs rejuvenation or repair.
Individuals who can significantly benefit from PRF injections include those seeking:
-
- Under-Eye Rejuvenation: Individuals with dark circles, mild to moderate hollowness (tear troughs), fine lines, or crepey skin under the eyes can see significant improvement. PRF injected into this area helps to thicken the skin, improve circulation, and stimulate collagen production, leading to a brighter, less tired appearance. It’s a powerful natural alternative for this delicate area.
-
- Improvement in Skin Texture and Tone: Those bothered by dull skin, uneven texture, enlarged pores, or mild discolouration can benefit from PRF injections, which stimulate collagen and elastin for smoother, more radiant skin.
-
- Reduction of Fine Lines and Wrinkles: PRF injections can soften fine lines and wrinkles, particularly those caused by loss of elasticity and collagen, such as crow’s feet, lines around the mouth, and forehead lines, by boosting the underlying skin structure.
-
- Scar Revision: Individuals with atrophic scars (like acne scars) or certain surgical scars can benefit from PRF injections, which help to remodel scar tissue, stimulate collagen in the depressed areas, and improve the overall texture and appearance of the scar.
-
- Subtle Volume Enhancement: When processed into a gel (Injectable PRF Gel), PRF can benefit individuals seeking subtle, natural volume restoration in areas of mild volume loss, such as the cheeks or temporal hollows, while simultaneously improving skin quality. It’s ideal for those who want a very natural look rather than the more pronounced volume of synthetic fillers.
-
- Hair Restoration: Men and women experiencing hair thinning or early stages of balding (androgenetic alopecia) can benefit from PRF injections into the scalp. The growth factors stimulate dormant hair follicles, promoting the growth of thicker, healthier hair and potentially slowing down the rate of hair loss.
- Accelerated Healing of Specific Tissues: Patients in medical fields needing enhanced healing of tendons, ligaments, joints (e.g., osteoarthritis, tendinopathy), or bone grafts following dental or orthopaedic procedures can benefit from targeted PRF injections into the affected sites to stimulate tissue repair and reduce inflammation.
In essence, anyone with a localised area of tissue that could benefit from amplified natural regeneration – be it aging skin, damaged collagen, inactive hair follicles, or injured connective tissue – is a potential candidate for PRF injections, provided they meet the general health criteria and have realistic expectations. The targeted nature of injections makes it particularly effective for addressing specific, defined concerns.
How Many Sessions of PRF are Needed for Optimal Results?
Achieving optimal results with Platelet Rich Fibrin (PRF) treatment is typically a process that unfolds over time and requires a series of treatment sessions, rather than being a one-time procedure. This is because PRF is a regenerative therapy that works by stimulating your body’s natural healing and tissue-building processes, and these biological processes require repeated signals and time to build significant, cumulative improvements.
The exact number of sessions needed can vary depending on several factors:
1. The Condition Being Treated: Different conditions respond at different rates and require varying degrees of stimulation. For example, treating mild skin texture issues might require fewer sessions than addressing deeper acne scars or significant hair thinning. Musculoskeletal injuries might also have different protocols.
2. The Severity of the Condition: More advanced signs of aging, deeper wrinkles, more extensive scarring, or greater degrees of hair loss will typically require more treatment sessions to achieve satisfactory results compared to milder concerns.
3. Individual Response: Each person’s body responds uniquely to regenerative stimuli. Factors like age, overall health, genetics, and lifestyle (e.g., smoking status) can influence how effectively and quickly your tissues regenerate. Some individuals may see excellent results with fewer sessions, while others might need more.
4. Desired Outcome: Your personal goals also play a role. If you’re aiming for subtle improvement, fewer sessions might suffice. If you desire more significant rejuvenation or regeneration, a more extensive treatment course will likely be recommended.
While a single PRF session can provide some initial benefits and initiate the regenerative cascade, the most significant and lasting improvements are typically achieved through a course of treatments. The commonly recommended number of sessions for most aesthetic applications (like facial rejuvenation, under-eyes, or hair restoration) is 3 to 4 sessions. These sessions are usually spaced approximately 4 to 8 weeks apart. This spacing allows enough time for the initial regenerative effects from one treatment to begin taking hold before the next session provides a booster stimulus, building upon the progress made.
After completing the initial series (e.g., 3-4 sessions), patients often see their optimal results continue to develop for another few months (2-3 months after the last session). To maintain these results over the long term, many practitioners recommend periodic maintenance treatments, typically a single session every 6 to 12 months, to provide ongoing stimulation and counteract the effects of natural aging.
In summary, while the specific number will be tailored to your individual needs and discussed during your consultation, you should generally expect that multiple sessions (most commonly 3-4) will be needed to achieve optimal and sustained results from PRF treatment for most aesthetic and many medical applications. This series approach leverages the cumulative nature of biological regeneration.
How many PRF injections are needed?
When we talk about the number of PRF injections needed, we can interpret this in two ways: the number of *needle sticks* per session, or the number of *treatment sessions* required. Based on the context of the grouped questions, it most likely refers to the number of *sessions* needed to see optimal results from PRF delivered via injection.
Assuming the question is asking about the number of *treatment sessions* involving PRF injections to achieve satisfactory outcomes, the typical recommendation aligns with the general guidelines for PRF therapy. For most aesthetic applications treated with injections – such as facial rejuvenation, reducing fine lines/scars, under-eye treatment, or scalp hair restoration – a series of 3 to 4 treatment sessions is commonly advised for optimal results.
These injection sessions are usually scheduled with a specific interval between them to allow the tissues to respond to the initial stimulation before the next treatment reinforces the regenerative process. The typical spacing is every 4 to 8 weeks. This frequency is chosen because the fibrin matrix from the previous injection has largely degraded by this time, having released its growth factors, and the early stages of new tissue formation are underway, making the area ready for another stimulus.
The rationale behind needing multiple injection sessions is that a single delivery of growth factors provides a powerful but relatively transient stimulus. To achieve significant tissue remodelling, robust collagen production, or sustained hair follicle activity, repeated exposure to these regenerative signals is necessary. Each subsequent injection session builds upon the progress made from the previous one, leading to cumulative and more pronounced improvements over time.
The exact number of injections *per session* (i.e., needle sticks) is highly variable and depends entirely on the treatment area size and the specific concern. Treating crow’s feet might involve a dozen or two injection points, while treating a full scalp for hair loss could involve scores or even hundreds of micro-injections to cover the thinning area adequately. But this is distinct from the number of visits needed.
So, in terms of how many *times you need to undergo the PRF injection procedure*, the standard recommendation for most aesthetic and hair restoration purposes is a series of 3 to 4 appointments. Following this initial series, maintenance sessions (perhaps one per year) might be suggested to prolong the benefits. The precise number of sessions will be determined by your practitioner based on your individual assessment and goals.
How many treatments of PRF gel are needed?
PRF Gel is a specific preparation of Platelet Rich Fibrin, created by heating liquid PRF to form a mouldable gel, often used for subtle volume enhancement alongside its regenerative effects, particularly popular for the under-eye area. When PRF is used in this gel form, typically delivered via injection, the number of treatments needed for optimal results follows a similar pattern to standard liquid PRF injections.
For aesthetic applications utilizing PRF Gel, such as addressing under-eye hollowness, improving fine lines with a subtle filling effect, or contouring certain areas, a series of treatments is generally recommended to achieve both the initial subtle volume correction and the desired level of long-term tissue regeneration. The commonly advised number of sessions for PRF Gel treatment is also in the range of 2 to 4 sessions.
The rationale remains the same: while the gel provides some immediate, subtle volume, its primary long-term benefit is the sustained release of growth factors stimulating collagen and elastin production. This regenerative process requires repeated stimulation to build cumulative results.
-
- For under-eye treatment with PRF Gel, a series of 2 to 3 sessions spaced about 6-8 weeks apart is a very common protocol. This helps address hollowness and significantly improves skin quality and dark circles over the course of the treatments.
- For other areas where PRF Gel might be used for subtle volume or regeneration, the recommendation is often 3 to 4 sessions spaced 4-8 weeks apart, depending on the area and the severity of the concern.
The exact number will depend on the individual’s specific needs, the volume deficit or regenerative goal, their response to treatment, and the practitioner’s preferred protocol. If the primary goal is regeneration with minimal volume, fewer sessions might suffice compared to a case where more noticeable subtle volume enhancement is desired.
After completing the initial series of PRF Gel treatments, the subtle volume effect will gradually diminish as the gel is absorbed (over maybe 2-4 weeks initially, though regeneration starts). However, the regenerative benefits continue to develop. To maintain both the regenerative improvements and potentially reinstate some subtle volume, periodic maintenance sessions (typically a single treatment every 6-12 months) are often recommended.
In essence, expect that achieving optimal results with PRF Gel, like other forms of PRF, will require a course of multiple treatments, usually ranging from 2 to 4 sessions, to maximise both the subtle filling effect and the long-term regenerative benefits in the treated area.
Is one PRF treatment enough?
In most cases, one PRF treatment is generally not enough to achieve optimal or significantly lasting results, especially for aesthetic or regenerative goals like improving skin quality, reducing wrinkles/scars, stimulating hair growth, or adding subtle volume. While a single session will initiate the regenerative process and provide a starting point for improvement, its effects are typically less pronounced and shorter-lived compared to those achieved with a full course of treatment.
Think of it like building a house. One brick (one session) lays the foundation, but you need many bricks, laid over time, to build the walls and complete the structure (optimal results). A single PRF treatment delivers a concentrated dose of growth factors and cells that signal the surrounding tissue to begin repair and regeneration. The fibrin matrix slowly releases these factors over 1-2 weeks, providing an initial period of stimulation. This kickstarts the production of new collagen, elastin, and blood vessels.
However, for significant tissue remodelling, which is required to make noticeable improvements in concerns like wrinkles, scars, or hair density, a single, several-week-long stimulus is usually insufficient to overcome years of aging, damage, or genetic predisposition to hair loss. The body needs repeated signals to continue and amplify the regenerative efforts over a longer period.
Subsequent PRF sessions, typically spaced 4-8 weeks apart, provide these crucial follow-up signals. Each treatment builds upon the progress made by the previous one, leading to a cumulative effect. The amount of new collagen, elastin, or stimulation of hair follicles achieved after 3-4 sessions is significantly greater than what is possible with just one.
While a single session might offer some mild, temporary improvement or serve as an introduction to the therapy, it is rarely sufficient to provide the level of results that patients typically seek and that PRF is capable of delivering when used optimally. For example, one under-eye PRF treatment might temporarily improve dark circles slightly, but it’s unlikely to resolve significant hollowness or make a dramatic, lasting impact on skin quality without follow-up sessions. Similarly, one hair treatment might stimulate a few follicles, but it won’t likely achieve significant, noticeable hair regrowth across a thinning area.
Therefore, while one PRF treatment *is* a treatment and will start a process, it is not typically enough to achieve the optimal results that PRF therapy is known for. Patients considering PRF should budget and plan for a series of sessions as the standard protocol for achieving satisfactory and longer-lasting outcomes.
How often should I have treatment?
The frequency of PRF treatment sessions depends on whether you are referring to the initial treatment phase to achieve optimal results or subsequent maintenance treatments to prolong those results.
Initial Treatment Phase:
During the initial phase, when you are aiming to build significant, cumulative regenerative results, PRF treatments are typically performed in a series of sessions spaced weeks apart. The most common interval recommended between PRF sessions for aesthetic applications (face, under-eyes, hair) is every 4 to 8 weeks.
-
- Every 4 weeks: This interval is often recommended for more aggressive or rapid regeneration goals, or in younger individuals with robust healing. It ensures continuous stimulation before the effects of the previous session’s signal entirely wane. It might be more common in the very beginning of a series.
- Every 6-8 weeks: This is a very common and widely adopted interval. It allows sufficient time for the body to respond to the previous PRF session (initiate collagen production, cellular activity) while still providing a booster before the regenerative momentum significantly slows down. This interval balances effective stimulation with patient convenience and recovery time between sessions.
The practitioner will recommend the ideal spacing based on your specific treatment plan, the area being treated, and your individual response. It’s important not to have the sessions too close together, as the tissue needs time to process the previous treatment’s signals and build new tissue. Having them too far apart means you might lose some of the cumulative benefit.
Maintenance Phase:
Once you have completed your initial series of treatments and achieved your optimal results, maintenance treatments are often recommended to sustain those benefits over the long term. These maintenance sessions are typically performed much less frequently, often every 6 to 12 months. The exact interval depends on how long your results from the initial series are lasting and your ongoing goals. A single maintenance session provides a renewed stimulus to help counteract the effects of ongoing aging and environmental factors, refreshing the regenerative process to help maintain the improved tissue quality or hair density.
In summary, expect to have PRF treatments in your initial series approximately every 4-8 weeks. After completing the series (usually 3-4 sessions), maintenance treatments are typically recommended less frequently, about once or twice a year, to prolong the regenerative benefits. Your practitioner will provide a specific schedule tailored to your needs.
How many PRF treatments do I need?
The question “How many PRF treatments do I need?” is a crucial one for planning and managing expectations, and while a precise number is determined during your consultation, there are widely accepted guidelines based on the cumulative nature of this regenerative therapy. You will likely need more than one treatment to achieve optimal results.
For most aesthetic and regenerative applications of PRF, including:
* Facial rejuvenation (improving skin texture, tone, lines)
* Under-eye treatment (dark circles, hollowness, crepey skin)
* Scar revision (acne scars, surgical scars)
* Hair restoration (scalp thinning)
* Subtle volume enhancement with PRF gel
The standard recommendation for an initial course of treatment to achieve significant, noticeable, and longer-lasting results is a series of 3 to 4 treatment sessions. These sessions are typically spaced approximately 4 to 8 weeks apart.
Here’s why a series of 3-4 is commonly recommended:
* Cumulative Effect: Each PRF treatment builds upon the previous one. The initial session kickstarts regeneration, the second session reinforces it, the third amplifies it, and often a fourth session helps consolidate the results and provides a robust foundation of newly regenerated tissue.
* Time for Response: Tissues require time to respond to the growth factor signals, produce new collagen and elastin, and remodel. Spacing sessions allows for this process to unfold while providing timely booster signals.
* Severity of Condition: For more challenging issues like deeper scars or more significant hair loss, a series of 4 sessions or potentially even more frequent or additional maintenance treatments might be necessary to see satisfactory improvement. For milder concerns, some individuals might be happy with results after 2 or 3 sessions.
After completing this initial series (e.g., 3-4 sessions), the regenerative effects continue to develop for another few months, and the visible benefits can last for 6-18 months. To maintain these results long-term, periodic maintenance treatments are usually recommended. This maintenance phase typically involves a single PRF session every 6 to 12 months.
So, while the exact number is personalised, you should anticipate needing an initial commitment of 3 to 4 PRF treatments to achieve the desired level of regeneration and visible improvement for most aesthetic concerns. Following this, yearly maintenance treatments are often suggested to prolong the benefits. Your practitioner will provide the most accurate recommendation based on your individual assessment during your consultation.
How often can I receive PRF Under Eye injections?
For PRF Under Eye injections, the frequency of treatment sessions is split into two phases: the initial treatment series aimed at addressing the specific concerns and achieving optimal rejuvenation, and the maintenance phase designed to prolong those results.
Initial Treatment Series:
To effectively treat concerns like dark circles, hollowness, fine lines, and crepey skin under the eyes with PRF, a series of treatments is recommended. The most common and effective frequency for these initial sessions is every 6 to 8 weeks. Some practitioners might recommend every 4 weeks in certain cases, but 6-8 weeks is widely adopted for the delicate under-eye area, allowing adequate time for the tissue to heal and respond between treatments.
A typical initial series for under-eye rejuvenation with PRF involves 2 to 3 sessions spaced at this 6-8 week interval. The delicate nature of the area means sometimes fewer sessions are needed initially compared to full-face rejuvenation, but the cumulative effect is still crucial.
Maintenance Phase:
Once the initial series is complete and optimal results have been achieved (which continue to improve for a couple of months after the last session), periodic maintenance treatments are highly recommended to sustain the benefits. For the under-eye area, a single maintenance session is often advised every 6 to 12 months, depending on the individual’s response, age, and the rate at which aging signs reappear.
Regular maintenance helps counteract the ongoing effects of aging and environmental factors specifically impacting the thin skin and delicate tissues under the eyes, ensuring the regenerative improvements gained are supported over time.
In summary, during the initial phase of PRF Under Eye treatment, you can typically receive injections every 6 to 8 weeks for a series of 2-3 sessions. Following this, maintenance treatments are usually needed less frequently, approximately once or twice a year, to prolong the rejuvenating effects and keep the under-eye area looking refreshed and revitalized. Your practitioner will establish the precise schedule tailored to your needs and response.
What to Expect During and After Your PRF Treatment
Embarking on a Platelet Rich Fibrin (PRF) treatment journey means understanding the entire process, from the moments leading up to the procedure through the immediate recovery period. Knowing what to expect at each step helps alleviate anxiety and ensures you are well-prepared, contributing to a smoother and more comfortable experience. It’s a relatively straightforward clinical process, but being informed about the different phases makes all the difference.
Before Your Treatment: Preparation often begins before you even arrive at the clinic. Your practitioner might advise you on simple steps to take in the days leading up to your appointment. Staying well-hydrated is frequently recommended, as it can make the blood draw easier. You might also be advised to avoid certain medications or supplements that can increase bruising risk, such as aspirin, NSAIDs (like ibuprofen or naproxen), fish oil, or high doses of Vitamin E, for a specified period, *provided this is medically safe and approved by your prescribing physician if applicable*. Arriving at your appointment well-rested and having eaten a light meal is also generally helpful to prevent feeling lightheaded during the blood draw. Ensure your skin is clean on the day of the appointment.
During the Procedure: The treatment session itself follows a predictable sequence:
1. Blood Draw: A small amount of blood will be drawn from your arm, much like a standard blood test. This is usually quick and involves minimal discomfort.
2. PRF Processing: The tubes of blood are immediately placed in a centrifuge and spun for a specific duration (typically 5-15 minutes) to separate the PRF. You’ll wait comfortably while this happens.
3. Preparation of Treatment Area: While the blood is spinning or after the PRF is extracted, the area to be treated will be thoroughly cleansed. If injections are planned, a topical numbing cream will likely be applied to minimise discomfort. This takes 15-30 minutes to take effect.
4. PRF Application/Injection: Once the PRF is ready (either liquid or gel) and the numbing is effective, the practitioner will proceed with the application. This is typically done via injections using fine needles or cannulas. You may feel pressure, mild pricking, or a brief stinging sensation during injections, but significant pain is uncommon thanks to numbing. The number of injections and time taken depend on the treatment area. If applied topically (e.g., after microneedling), the PRF is gently massaged into the skin.
The entire treatment, from blood draw to completion, usually takes between 30 to 60 minutes.
Immediately After Treatment: Once the procedure is finished, the treated area will likely exhibit some immediate, temporary effects:
* Redness: The skin may appear flushed.
* Swelling: Mild to moderate puffiness is common, especially with injections.
* Tenderness: The area may feel slightly sore or sensitive to touch.
* Possible Bruising: Small bruises may be visible at injection sites.
These immediate side effects are normal and expected. Your practitioner will provide you with specific aftercare instructions to manage these symptoms and optimise healing.
Recovery Period (Hours to Days After Treatment):
The initial recovery for most PRF treatments is typically very quick, often with minimal downtime.
* Within a few hours: Redness and tenderness usually begin to subside.
* Within 24-48 hours: Swelling typically decreases significantly. Any discomfort is usually gone.
* Within a few days to two weeks: Bruising will gradually fade. Temporary small bumps at injection sites should also resolve.
Most individuals can return to their normal daily activities, including work, the same day or the day after treatment. However, specific aftercare guidelines should be followed diligently to ensure proper healing and best results. These guidelines often involve avoiding strenuous exercise, excessive heat (saunas, hot baths), swimming pools, direct sun exposure, and sometimes certain skincare products for a short period.
Longer-Term (Weeks to Months After Treatment):
Remember that PRF stimulates a regenerative process. You won’t see the full results immediately.
* Weeks: Subtle improvements may begin to appear.
* Months: More noticeable results develop as collagen builds and tissues regenerate.
* Ongoing: Improvements continue with subsequent sessions in a series.
Overall, expect a safe, well-managed clinical procedure with predictable, temporary minor side effects, followed by a brief initial recovery and gradual, natural improvements over weeks and months as your body responds to the regenerative stimulus provided by the PRF.
How to Prepare for PRF Injections
Proper preparation for Platelet Rich Fibrin (PRF) injections is a simple yet important step that can help ensure the procedure goes smoothly, minimise discomfort, and potentially reduce the risk of minor side effects like bruising. Taking a few proactive measures in the days leading up to your appointment can make a difference.
Here are key steps on how to prepare for PRF injections:
1. Stay Well-Hydrated: This is perhaps one of the most crucial preparation steps. Being well-hydrated in the 24-48 hours before your appointment makes your veins more prominent and easier to find, which facilitates a quicker and smoother blood draw at the start of the procedure. Drink plenty of water in the day or two leading up to your appointment.
2. Avoid Certain Medications and Supplements (Consult Your Doctor): Many practitioners advise patients to avoid medications and supplements that can increase the risk of bruising and bleeding for about a week to 10 days before the treatment. This commonly includes:
* Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) such as Aspirin, Ibuprofen (Advil, Motrin), Naproxen (Aleve).
* Certain dietary supplements like fish oil (Omega-3 fatty acids), Vitamin E, Ginkgo Biloba, Ginseng, Garlic, and St. John’s Wort.
However, it is absolutely critical that you consult your prescribing physician before stopping any prescribed medication. Do not stop taking medication without their approval. Discuss with your PRF practitioner which specific items you should avoid and for how long, based on your medical history and current prescriptions.
3. Limit Alcohol Consumption: Avoiding alcohol for at least 24-48 hours before your appointment is recommended, as alcohol can also thin the blood and increase the likelihood of bruising.
4. Eat Something Before Your Appointment: Arrive at your appointment having had a light meal. Coming on an empty stomach can make some individuals feel lightheaded or dizzy during or after the blood draw.
5. Inform Your Practitioner of Any Illnesses: If you develop a cold, flu, fever, or any active skin infection (like a cold sore) near the treatment area in the days leading up to your appointment, contact the clinic immediately. The treatment may need to be rescheduled until you are fully recovered.
6. Wash Your Skin: Arrive with clean skin, free of makeup, lotions, or creams in the area to be treated. Your practitioner will cleanse the area again before the procedure, but starting with clean skin is helpful.
7. Plan for Potential Downtime (Minimal): While downtime is usually minimal, it’s wise to schedule your appointment at a time when you don’t have a major social event immediately afterward, just in case you experience more bruising or swelling than anticipated.
By following these preparation steps, you contribute to a more comfortable and potentially less complicated PRF injection experience, setting the stage for optimal healing and results. Always follow the specific pre-treatment instructions provided by your practitioner, as protocols can vary slightly between clinics.
What to Expect During PRF Injections
Knowing precisely what happens during the PRF injection phase can help alleviate anxiety and prepare you for the sensations you might experience. This part of the treatment follows the blood draw and PRF processing and is where the regenerative material is delivered to your target tissues.
Here’s what you can typically expect during PRF injections:
1. Preparation of the Area: The practitioner will thoroughly cleanse the treatment area with an antiseptic solution to minimise the risk of infection. If you are receiving injections in a sensitive area like the face or scalp, a topical numbing cream would typically have been applied beforehand and will now be removed. You should expect the area to feel numb or significantly less sensitive to touch.
2. PRF Loading: The practitioner will carefully draw the prepared liquid PRF or PRF gel into sterile syringes, often using a larger gauge needle to extract the material and then switching to very fine needles or cannulas for the injections.
3. The Injections: This is the core of the procedure. The practitioner will begin making a series of precise injections into the target area. The technique, depth, and pattern of injections will vary significantly depending on the area being treated and the specific concern (e.g., shallow injections for fine lines, deeper injections for scars or under-eye hollowness, injections into the scalp for hair).
- Sensation: Even with numbing cream, you might feel some sensation. Common sensations include:
* Mild Pricking/Stinging: As the fine needle penetrates the skin.
* Pressure/Fullness: As the PRF material is being injected into the tissue.
* Occasional Brief Pinch or Burn: Particularly in areas that are harder to numb or are more sensitive.
* However, intense or sharp pain is generally not expected. If you experience significant discomfort, inform your practitioner immediately.
4. Use of Cannulas (Optional but often preferred in sensitive areas): In areas prone to bruising or where blood vessels are a concern (like the under-eyes), many practitioners use blunt-tipped cannulas instead of sharp needles. The skin is first pierced with a sharp needle to create a small entry point, and then the cannula is inserted. With a cannula, you’ll feel more pressure and a pushing sensation as it navigates beneath the skin, rather than multiple sharp pricks. Cannulas generally reduce bruising and the risk of injecting directly into a blood vessel.
5. Duration: The injection phase itself is usually quite quick, often lasting anywhere from 10 minutes for a small area to 20-30 minutes for a larger area like the full face or scalp.
6. Practitioner Technique: Expect the practitioner to be focused, precise, and potentially using techniques like stretching the skin taut, using their non-injecting hand to support tissues, or injecting slowly.
Throughout the process, your practitioner may check in with you to ensure you are comfortable. They will work methodically to ensure even distribution of the PRF across the treatment zone to achieve the most uniform and effective regenerative response. The sensations are typically tolerable, and the knowledge that the treatment is relatively quick helps many patients get through this part of the procedure comfortably.
What to expect after your PRF session
The period immediately following your Platelet Rich Fibrin (PRF) session comes with a set of common and expected physical changes in the treated area. These are normal responses of the body initiating the healing and regenerative process and are usually temporary and manageable. Understanding what to anticipate helps you navigate the brief recovery period comfortably.
Here’s a breakdown of what to expect after your PRF session:
1. Immediate Appearance: Right after the injections or application, the treated area will likely look red. You will also notice swelling, which can range from subtle puffiness to more noticeable swelling, depending on the area treated (under-eyes tend to swell more than the scalp, for instance) and the volume of PRF injected. The skin may also feel warm or tender to the touch.
2. Bruising: Bruising is a very common side effect, although its severity varies greatly. You may see small pinpoint bruises at injection sites or larger discoloured patches. Bruising can become more apparent in the hours or day following the treatment.
3. Tenderness or Soreness: The injection sites might feel sore, tender, or slightly bruised for a day or two. This discomfort is generally mild.
4. Tightness or Fullness: You might feel a sensation of tightness or fullness in the treated area, particularly if injections involved volume or stimulated significant initial swelling.
5. Small Bumps: It’s possible to feel or see small, temporary bumps at some of the injection points. These are typically the injected PRF settling into the tissue and should gradually smooth out within a few days or up to a couple of weeks as the material integrates and the swelling subsides.
Post-Treatment Care and Management: Your practitioner will provide specific aftercare instructions, which are vital to follow. These typically include:
-
- Avoid touching or rubbing the treated area immediately after the session.
-
- Applying cool compresses intermittently in the first few hours to help reduce swelling and bruising (avoiding direct ice on the skin).
-
- Avoiding strenuous exercise, excessive heat (hot showers, saunas, hot tubs), and swimming pools for at least 24-48 hours.
-
- Avoiding direct sun exposure on the treated area and using sunscreen.
-
- Avoiding certain skincare products (like retinoids, alpha hydroxy acids, or harsh exfoliants) for a period, as advised by your practitioner.
-
- Sleeping with your head elevated (using an extra pillow) the first night can help minimise facial swelling.
- Using recommended pain relief (like acetaminophen) if needed for discomfort, while potentially avoiding NSAIDs if previously advised for bruising risk.
The initial recovery period is generally short. Most people can return to work and light activities the same day or the day after. The visible temporary side effects (redness, swelling, bruising) typically subside significantly within 2-3 days. While the initial side effects are temporary, the regenerative process initiated by the PRF continues internally over weeks and months, leading to the gradual appearance of the actual, desired results.
What to avoid after PRF?
To ensure optimal healing, minimise potential side effects, and maximise the effectiveness of your Platelet Rich Fibrin (PRF) treatment, there are certain activities, substances, and environmental exposures you should generally avoid immediately after your session. Your practitioner will provide you with specific, tailored aftercare instructions, but here is a list of common things to avoid:
1. Strenuous Exercise: Avoid vigorous physical activity, heavy lifting, or intense workouts for at least 24-48 hours after your PRF session. Increased blood flow and sweating can exacerbate swelling and bruising and potentially increase the risk of infection at injection sites.
2. Excessive Heat: Stay away from sources of excessive heat for at least 24-48 hours. This includes hot showers, baths, saunas, steam rooms, and hot tubs. Heat can increase swelling and potentially affect the stability of the injected PRF.
3. Direct Sun Exposure and Tanning Beds: Avoid direct and prolonged exposure to sunlight and do not use tanning beds for at least 48-72 hours, and ideally for a week or more, especially if the treatment was on the face or other exposed areas. Sun exposure can increase swelling and redness and can be harmful to the skin, potentially interfering with the regenerative process. Use a broad-spectrum sunscreen when going outdoors after this initial period.
4. Swimming Pools and Saunas: Avoid swimming pools, lakes, oceans, and saunas for at least 24-48 hours to minimise the risk of infection from bacteria in the water or environment.
5. Touching or Rubbing the Treated Area: Try to avoid touching, rubbing, or massaging the treated area unnecessarily immediately after the procedure, unless specifically instructed to do so by your practitioner (e.g., gentle massage for certain types of injections). This helps prevent infection, displacement of the injected material, and reduces irritation.
6. Applying Makeup (Immediately): If treated on the face, it’s generally recommended to wait at least 6-12 hours, or ideally until the next day, before applying makeup to reduce the risk of clogging injection sites or introducing bacteria. Ensure any makeup brushes or applicators are clean.
7. Alcohol: Avoid consuming alcohol for at least 24-48 hours post-treatment, as it can increase bruising and swelling and may impair healing.
8. Certain Medications/Supplements: Continue to avoid blood-thinning medications and supplements (NSAIDs, fish oil, etc.) for the period advised by your practitioner before the treatment, potentially for a couple of days after as well, to help minimise bruising. Always consult your doctor before stopping any prescription medication.
9. Harsh Skincare Products: Avoid using harsh or active skincare products (like retinoids, alpha hydroxy acids, strong exfoliants, or alcohol-based toners) on the treated area for at least 24-72 hours, or as advised by your practitioner, to avoid irritation and allow the skin to begin healing. Stick to gentle cleansers and moisturisers as recommended.
10. Smoking: While avoiding smoking is beneficial anytime, it is particularly important to avoid smoking immediately after PRF treatment (and ideally long-term), as smoking significantly impairs blood flow and healing, which can compromise the results of the regenerative therapy.
Following these guidelines is crucial for a smooth recovery and to ensure your body can effectively utilise the regenerative power of the PRF you received. Always defer to the specific post-treatment instructions provided by your clinic.
Can I wash my hair after PRF treatment?
The ability to wash your hair after PRF treatment depends on whether the treatment was performed on the scalp for hair restoration or on other areas. If the PRF treatment was performed on your scalp for hair restoration, there will be numerous injection points. It is generally recommended to avoid washing your hair or scalp for at least 12 to 24 hours after the treatment session.
Here’s why this waiting period is advised after scalp PRF injections:
1. Minimise Infection Risk: The injections create tiny punctures in the scalp skin. Allowing these sites to close and begin healing before washing reduces the risk of bacteria from water or shampoo entering the skin and causing an infection.
2. Allow PRF Integration: While the PRF is injected into the tissue, avoiding immediate washing or vigorous rubbing helps ensure the material begins to integrate with the scalp tissue without being disrupted.
3. Reduce Irritation: The scalp may be sensitive or tender after injections. Washing and rubbing can cause additional irritation or discomfort.
After the initial 12-24 hour period (or as specifically advised by your practitioner), you can typically wash your hair using a gentle shampoo and lukewarm water. Avoid scrubbing the scalp vigorously in the first day or two; instead, gently massage the shampoo in and rinse carefully. Avoid using harsh chemicals, strong styling products, or excessive heat on the scalp immediately after treatment.
If your PRF treatment was performed on a different area, such as your face or body, and *not* on the scalp, then your ability to wash your hair is generally unaffected. You can wash your hair as normal, being careful to avoid getting harsh shampoos or very hot water on the treated facial or body areas if they were near your hairline or neck, for example.
Always follow the specific post-treatment instructions given to you by your practitioner, as they may have a particular protocol they recommend based on the exact technique used and your individual needs. But as a general rule for scalp PRF: wait 12-24 hours before washing.
How to sleep after PRF?
Getting a good night’s sleep is important for healing, but finding a comfortable position after Platelet Rich Fibrin (PRF) treatment, especially if it was performed on the face or under-eyes, can be a minor consideration. The main goal for sleeping post-treatment is to minimise swelling and discomfort in the treated area.
Here are some tips on how to sleep after PRF treatment, particularly focusing on facial areas:
1. Elevate Your Head: Sleeping with your head elevated above your heart is highly recommended for the first night or two after facial PRF treatment, especially for procedures around the eyes, cheeks, or forehead. Use an extra pillow or two, or sleep in a recliner if that is comfortable. Elevation helps gravity assist in fluid drainage, which can significantly reduce swelling and make you more comfortable the morning after.
2. Sleep on Your Back: Try your best to sleep on your back (supine position). This helps to avoid putting direct pressure on the treated areas of your face. Sleeping on your side or stomach can press one side of your face into the pillow, potentially exacerbating swelling or bruising on that side and possibly disturbing the injected material’s initial settling phase (though this is less of a concern with PRF than with some fillers). If you are usually a side or stomach sleeper, you might find it helpful to prop pillows around your sides to prevent you from rolling over during the night.
3. Use Clean Pillowcases: Ensure your pillowcase is clean to minimise the risk of introducing bacteria to the treatment sites, especially if there was any minor bleeding or weeping immediately after the procedure.
4. Avoid Pressure on Treated Areas: If PRF was injected into other body areas (e.g., joints), try to avoid sleeping directly on the treated limb or side for the first night to minimise discomfort and pressure.
For scalp PRF treatments, sleeping position is generally less critical from a swelling perspective, but avoiding vigorous rubbing of the scalp against the pillow is advisable for the first night or two to allow the injection sites to heal and prevent irritation.
While it can be challenging to change your usual sleeping habits, making an effort to sleep elevated on your back for the first couple of nights after facial PRF can significantly contribute to a more comfortable recovery and potentially better results by reducing post-treatment swelling. After a few days, as the initial swelling subsides, you can usually return to your normal sleeping position.
What to eat before PRF?
While there aren’t strict dietary requirements specifically for Platelet Rich Fibrin (PRF) treatment, focusing on a healthy diet and ensuring you are well-nourished and hydrated before your appointment can contribute positively to the overall experience and potentially support your body’s healing response.
Here’s what to focus on eating and drinking before PRF:
1. Stay Well-Hydrated: This is the most important dietary/hydration tip. Drink plenty of water in the 24-48 hours leading up to your appointment. Being well-hydrated makes your veins more accessible for the blood draw, which is the first step of the PRF procedure. Aim for at least 8 glasses of water per day.
2. Have a Light Meal: It’s recommended to eat a light, balanced meal a few hours before your appointment. Avoid coming in on an empty stomach, as this can make you feel lightheaded or nauseous, especially in conjunction with the blood draw. A meal that includes complex carbohydrates and protein can help stabilise your blood sugar levels.
3. Focus on Nutrient-Rich Foods: While not mandatory for the treatment itself, generally eating a healthy diet rich in vitamins and minerals supports your body’s overall health and healing capacity. Include fruits, vegetables, lean proteins, and whole grains in your meals leading up to the appointment.
4. Consider Foods that May Help with Bruising (Long-Term Strategy): While not a quick fix, some nutrients are thought to help support vascular health and potentially reduce bruising over time. Including foods rich in Vitamin C (citrus fruits, berries, leafy greens) and Vitamin K (leafy greens like kale, spinach, broccoli) in your regular diet can be beneficial for overall skin and vascular health. However, this is a long-term dietary approach, not an immediate pre-treatment preparation step that will dramatically impact bruising risk from a single treatment.
What to Potentially Avoid (Relates to Bruising):
As mentioned in the preparation steps, while focusing on *eating* specific things isn’t critical, *avoiding* certain substances that can increase bruising risk is often advised. This includes alcohol (especially the day before) and supplements like fish oil or high-dose Vitamin E for about a week prior (consult your doctor before stopping any supplements or medications). These avoidance recommendations are more directly related to the risk of post-injection bruising than to the PRF process itself.
In summary, the most vital “what to eat/drink” preparation for PRF is staying well-hydrated and not coming in on an empty stomach. Beyond that, maintaining a generally healthy diet supports your body’s overall ability to heal and respond to the regenerative stimulus provided by the PRF. Always follow any specific dietary instructions given by your practitioner.
Platelet-Rich Fibrin Injections (PRF): The Benefits, Aftercare, And Results
Platelet-Rich Fibrin (PRF) injections represent a powerful and natural approach to stimulating tissue regeneration across various aesthetic and medical applications. As we’ve explored in depth, this treatment leverages the body’s own potent healing capabilities, concentrated from a small sample of your blood, to achieve revitalising outcomes. The journey involves understanding the compelling benefits PRF offers, adhering to crucial aftercare guidelines to ensure proper healing, and having realistic expectations regarding the timing and nature of the results.
The benefits of PRF injections are numerous and compelling, stemming from the concentrated release of growth factors, leukocytes, and stem cells embedded within a natural fibrin matrix. These include:
* Genuine Tissue Regeneration: Stimulating the production of new collagen, elastin, and blood vessels for improved skin quality, firmness, and vitality.
* Natural Appearance: Results develop gradually, leading to subtle, refreshed, and organic-looking improvements.
* Versatile Applications: Effective for facial rejuvenation (lines, texture, under-eyes), scar revision, and hair restoration.
* Accelerated Healing: Aids in faster recovery from injuries and procedures in medical contexts.
* High Safety Profile: Autologous nature eliminates the risk of allergic reactions or rejection.
* Minimally Invasive: Procedure involves simple blood draw and injections with minimal downtime.
* Sustained Stimulation: The fibrin matrix provides a prolonged release of regenerative factors over 1-2 weeks.
Crucial to maximising these benefits and ensuring a smooth experience is proper aftercare. Immediately after PRF injections, you should expect temporary side effects like redness, swelling, bruising, and tenderness at the injection sites. Adhering to aftercare instructions is vital:
* Avoid strenuous activity, excessive heat, and direct sun exposure for 24-48 hours.
* Avoid touching, rubbing, or applying makeup to the treated area immediately after.
* Follow specific cleansing and skincare recommendations from your practitioner.
* Avoid blood-thinning substances (alcohol, certain medications/supplements) as advised.
* Elevate your head while sleeping if treated on the face.
* Use cool compresses intermittently if needed to reduce swelling/bruising.
Finally, understanding the results timeline is key. Visible improvements are not immediate.
* Subtle changes may begin around 2-4 weeks.
* More noticeable results typically appear 6-12 weeks after the first session.
* Optimal results are usually seen 2-3 months after completing a recommended series (commonly 3-4 sessions spaced 4-8 weeks apart).
* For hair, visible growth may take 3-6 months.
The longevity of these regenerative effects typically lasts for 6 to 12 months or sometimes longer after a series, but maintenance treatments (often annually) are recommended to sustain the benefits against the tide of aging.
In summary, Platelet Rich Fibrin injections offer a powerful, safe, and natural path to regeneration, yielding gradual, beautiful results. Success hinges on understanding its mechanisms, diligently following aftercare, and having realistic expectations about the journey towards optimal rejuvenation and healing. It’s an investment in stimulating your body’s own innate ability to repair and revitalize itself.
What to expect during PRF Under Eye treatment?
Under-eye treatment with Platelet Rich Fibrin (PRF) is a common and effective application aimed at rejuvenating this delicate area, addressing concerns like dark circles, hollowness, fine lines, and crepey skin. The experience during the procedure is similar to other PRF injection treatments but with specific considerations for the sensitivity and anatomy of the under-eye region.
Here’s what to expect during your PRF Under Eye treatment:
1. Preparation & Numbing: After cleansing the skin, a topical numbing cream will be applied generously to the under-eye area and potentially extends slightly onto the cheeks and temples. This step is crucial because the under-eye skin is very thin and sensitive. You should expect to wait 15-30 minutes for the numbing cream to take full effect, making the injections significantly more comfortable.
2. Blood Draw & PRF Preparation: While the numbing cream works, a small amount of your blood will be drawn, typically from your arm. This blood is immediately placed into a centrifuge and spun according to the specific PRF protocol (often optimized for creating injectable PRF gel for this area). This processing usually takes 5-15 minutes.
3. PRF Extraction: The practitioner will carefully extract the Platelet Rich Fibrin from the centrifuge tube. For under-eye hollowness, the PRF is often processed into a gel consistency (Injectable PRF Gel). This gel is then drawn into a small syringe.
4. The Injections: This is the main treatment phase. The practitioner will use a very fine needle or, more commonly and preferably for safety in this area, a blunt-tipped cannula to inject the PRF (often the gel form) into the under-eye region.
-
- Cannula Technique: If a cannula is used, the practitioner will first make a single entry point with a sharp needle (after local anaesthetic is injected at the entry point). Then, the cannula is inserted through this point and carefully guided under the skin to distribute the PRF gel evenly along the tear trough or hollow area. With a cannula, you’ll feel more pressure and a sensation of movement or pushing, but significantly less risk of bruising and hitting blood vessels compared to multiple sharp needle sticks.
-
- Needle Technique: If a needle is used (often for very superficial, precise injections addressing fine lines or skin quality rather than volume), you will feel multiple small pricks.
- Sensation: With adequate numbing, discomfort is usually minimal, ranging from mild pressure to a dull ache or occasional mild sting. Communicate any significant discomfort to your practitioner.
5. Injection Pattern & Volume: The practitioner will make precise injections or passes with the cannula to deposit small amounts of PRF or PRF Gel strategically along the area requiring rejuvenation – addressing hollowness, dark circles, or lines. The volume injected is carefully measured to avoid over-filling, which can look unnatural.
6. Gentle Massage (Optional): After injection, the practitioner might gently massage the area to ensure even distribution of the PRF, particularly with PRF Gel.
7. Duration: The injection process for both under-eyes is typically quite quick, often taking only 10-15 minutes after the numbing has taken effect. The entire appointment, including blood draw, numbing, and processing, usually lasts 45-60 minutes.
Expect the practitioner to be meticulous and focused, given the delicate nature of the area. You might hear sounds from the centrifuge and feel the cleansing and numbing sensations before the injections begin. The experience is designed to be as comfortable and safe as possible, leveraging the natural power of PRF to rejuvenate the under-eye region.
What to expect after your PRF Under Eye Filler treatment?
After undergoing Platelet Rich Fibrin (PRF) Under Eye “Filler” treatment (referring to Injectable PRF Gel used for subtle volume and regeneration), the immediate post-treatment experience will have specific characteristics due to the delicate nature of the under-eye area and the type of material injected. While generally well-tolerated, there are typical temporary effects you should be prepared for.
Here’s what to expect after your PRF Under Eye Gel treatment:
1. Immediate Appearance: You will likely notice some immediate fullness in the treated area due to the volume of the injected PRF Gel, which helps reduce the appearance of hollowness right away. However, this initial fullness is often accompanied by swelling, which can make the under-eye area look puffier than the final result will be. Redness and potentially some minor pinpoint bleeding at injection sites (or the cannula entry point) are also common.
2. Swelling: Swelling is a very common side effect under the eyes due to the thin skin and rich vascularity of the area, as well as the inflammatory response to the injections and the PRF itself. Swelling is often most noticeable in the first 24-48 hours and can make the area look temporarily worse than before treatment. It gradually subsides over the next few days to a week. Sleeping with your head elevated the first night is highly recommended to help reduce swelling.
3. Bruising: The under-eye area is highly susceptible to bruising. Even with skilled technique and the use of cannulas, some bruising is possible. Bruises can range from small spots to larger areas of discoloration and may take one to two weeks to resolve. They might change color (from purple to green to yellow) as they heal.
4. Tenderness/Soreness: The area might feel slightly tender or sore to the touch for a day or two.
5. Small Bumps or Irregularities: You might be able to feel small bumps or areas of firmness under the skin where the PRF Gel was injected. These are usually temporary as the gel integrates with the tissue and initial swelling resolves. Gentle, upward massage (if advised by your practitioner) might help smooth them out. Report any persistent, painful, or visible nodules to your practitioner.
6. Appearance of Dark Circles: Paradoxically, initial swelling and bruising can sometimes make dark circles temporarily appear worse before the long-term regenerative effects kick in to improve them.
Recovery and Aftercare:
* Downtime is usually minimal, but you might want to avoid social events for a few days if swelling or bruising is significant.
* Apply cool compresses gently (avoiding excessive pressure).
* Sleep with your head elevated.
* Avoid strenuous activity, hot environments, alcohol, and blood-thinning medications/supplements as advised.
* Follow specific instructions on cleansing and skincare.
* Avoid direct sun exposure and use sunscreen.
Timeline of Results:
Remember the “filler” effect is subtle and the regenerative benefits take time.
* Initial swelling resolves within days to a week or two.
* Any bruising fades within one to two weeks.
* The subtle, natural results from regeneration (improved skin quality, reduced dark circles) begin to appear around 2-4 weeks and improve over 2-3 months, building upon subsequent sessions if you are in a series.
* The full regenerative effects, leading to optimal improvement in the under-eye area, are typically seen a few months after completing a recommended series of treatments.
In summary, expect temporary swelling and possible bruising after PRF Under Eye Gel treatment, which are normal parts of the recovery. These initial effects subside relatively quickly, revealing gradual, natural improvements in skin quality, dark circles, and subtle volume over the following weeks and months as your body responds to the regenerative stimulus. Patience and diligent aftercare are key.
Is PRF Painful? What Level of Discomfort Can You Expect?
A common concern for anyone considering injectable treatments is the potential for pain or discomfort. When it comes to Platelet Rich Fibrin (PRF) treatment, especially involving injections, the level of discomfort is generally considered minimal to moderate and is typically very manageable. It’s not usually described as a significantly painful procedure.
The main sources of discomfort during a PRF treatment are the blood draw and the subsequent injections.
1. Blood Draw: Drawing the blood at the beginning of the session is similar to getting a standard blood test. You will feel a brief pinch or poke as the needle enters the vein, followed by a sensation of pressure or pulling as the blood is collected. For most people, this is a quick and relatively painless part of the process, causing only momentary discomfort. If you have a fear of needles or tend to feel faint during blood draws, informing your practitioner beforehand will allow them to take extra precautions to make you more comfortable.
2. Injections: The sensations experienced during the injection of the PRF depend heavily on a few factors:
* Treatment Area: Some areas of the body are more sensitive than others (e.g., lips, forehead, scalp can be more sensitive than cheeks).
* Use of Numbing Agents: For most aesthetic PRF injection treatments, especially on the face and scalp, a topical numbing cream is applied beforehand. This significantly reduces the sensation of pain. Once the numbing cream has taken effect (typically after 15-30 minutes), the area will feel numb or significantly less sensitive.
* Practitioner Technique: The skill of the injector plays a big role. An experienced practitioner will use fine needles or cannulas, inject smoothly, and work efficiently to minimise discomfort.
* Injection Depth: More superficial injections might feel like a series of small pricks, while deeper injections might feel more like pressure or fullness.
With proper numbing, you should expect to feel sensations ranging from mild pricking, slight stinging, or a pressure/fullness sensation during the injections. While not entirely painless, it is generally well-tolerated and brief. Most patients describe it as uncomfortable rather than truly painful. The level of discomfort is often comparable to or less than that experienced during treatments like dermal filler injections or botulinum toxin injections, especially when topical numbing is used effectively.
After the treatment, you might experience mild tenderness or soreness at the injection sites for a day or two, which is also usually manageable with over-the-counter pain relievers (avoiding NSAIDs if advised for bruising risk).
In summary, while you will feel sensations during the blood draw and injections, the discomfort associated with PRF treatment is typically mild to moderate, brief, and well-controlled with numbing agents and skilled technique. It is generally not considered a significantly painful procedure.
How painful is PRF?
To reiterate directly, Platelet Rich Fibrin (PRF) treatment is generally considered to be minimally painful. The level of discomfort is typically low to moderate and is manageable with standard comfort measures. It is far less painful than surgical procedures and is often described as comparable to or less uncomfortable than receiving cosmetic injections with synthetic fillers or neuromodulators, particularly when steps are taken to enhance patient comfort.
The sensation of pain or discomfort primarily arises from two points in the procedure:
1. The Blood Draw: This is a standard medical procedure, and most individuals experience only a brief, sharp pinch or sting from the needle insertion, followed by a dull pressure sensation while the blood is collected. This part is typically very quick. For people who are anxious about needles, this might be the most uncomfortable part, but the physical pain is usually minimal and short-lived.
2. The Injections: This is where the PRF is delivered. The discomfort here is highly variable depending on the area being treated, the individual’s pain tolerance, and whether numbing agents are used.
-
- Without Numbing: If performed without any numbing (which is rare for aesthetic injections, but might occur for certain medical applications), injections could feel like sharp pricks or stings, potentially moderate in discomfort depending on the area.
- With Topical Numbing: When a topical numbing cream is applied (the standard practice for aesthetic facial and scalp injections), the skin’s sensitivity is significantly reduced. During the injections, you are likely to feel pressure, a mild pushing sensation (especially with a cannula), or occasional subtle pricks. Any stinging sensation is usually brief and localised. The discomfort is typically well within a tolerable range.
Areas with thinner skin (like under the eyes) or more nerve endings (like the lips or scalp) can inherently be more sensitive, but numbing cream significantly mitigates this.
After the procedure, some mild soreness or tenderness at the injection sites might be felt for a day or two, but this is rarely severe pain.
In conclusion, while no injection is entirely free of sensation, PRF treatment is not considered a highly painful procedure. With the aid of topical numbing cream, the discomfort from the injections is usually mild and well-tolerated, allowing most patients to undergo the treatment comfortably. The quick nature of the procedure also helps, as any uncomfortable sensations are brief.
Is PRF painful?
Let’s address the direct question: “Is PRF painful?”. The answer is typically no, PRF treatment is not generally considered painful in a significant or severe sense. It is usually associated with mild to moderate, transient discomfort, primarily during the blood draw and the injection phase.
Think of the discomfort level as comparable to having blood drawn for routine tests and receiving standard cosmetic injections (like dermal fillers or neuromodulators), and often less uncomfortable when effective numbing techniques are used.
The sensations you might feel are:
-
- Brief Pinch/Prick: At the moment the needle enters the skin for the blood draw and for each injection (unless a cannula is used).
-
- Pressure/Fullness: As the blood is drawn into the tube, and as the PRF material is injected into the tissue. This is a common sensation, especially when injecting volume or using a cannula.
-
- Mild Stinging or Warmth: Occasionally felt as the PRF is deposited, though usually brief.
- Soreness/Tenderness: A dull ache or sensitivity at the treatment sites for a day or two after the procedure.
Crucially, effective pain management strategies are employed to minimise discomfort during PRF injections:
1. Topical Numbing Cream: This is routinely applied to the treatment area before facial or scalp injections and significantly reduces sensitivity.
2. Local Anesthesia: For certain procedures or sensitive individuals, a small amount of injectable local anesthetic might be injected at the blood draw site or cannula entry point to further minimise discomfort.
3. Cannulas: Using blunt-tipped cannulas (where appropriate) instead of sharp needles for injections can reduce the number of needle sticks and cause less sharp pain, replacing it with a pushing or pressure sensation.
4. Skilled Technique: Experienced injectors are smoother, more efficient, and use less traumatic techniques, further reducing discomfort.
So, while PRF injections do cause sensations that involve some level of discomfort, and might be perceived as briefly painful by some during the procedure itself, these sensations are typically temporary, well-managed with numbing techniques, and generally considered tolerable. Post-treatment discomfort is usually mild soreness, not significant pain. For the vast majority of patients, the discomfort associated with PRF injections is not a barrier to treatment.
Do PRF injections cause pain?
Yes, PRF injections do cause *sensation*, and that sensation can range from mild discomfort to a feeling that some individuals might describe as briefly painful, depending on their pain tolerance, the injection site, and the methods used to manage discomfort. However, they are not typically described as causing *severe* or *prolonged* pain.
The physical act of inserting a needle or cannula into the skin and tissue inherently creates a sensation. When PRF is injected, this sensation is compounded by the pressure of the material entering the tissue and the potential temporary irritation as the body initially responds to the injected substance.
Specifically, PRF injections can cause:
-
- Pricking/Stinging Pain: This is felt when the needle tip penetrates the skin and tissue. The intensity depends on the needle size (fine needles are used for PRF) and the sensitivity of the area.
-
- Pressure/Aching: As the volume of PRF is injected into the tissue, you’ll likely feel pressure or a dull ache. This can be more noticeable with larger volumes or in tighter tissue planes.
- Brief Burning/Stinging Sensation: Some patients report a brief stinging or warming sensation as the PRF is injected, which is thought to be related to the biological factors within the PRF interacting with the tissue.
How is this discomfort managed?
Fortunately, practitioners use effective techniques to significantly reduce the discomfort associated with PRF injections:
1. Topical Numbing Cream: Applied to the treatment area beforehand, this is very effective at numbing the superficial layers of the skin, greatly reducing the pricking sensation from needle entry.
2. Local Anesthesia: In very sensitive areas or for cannula entry points, a small amount of injectable local anesthetic can provide more profound numbness.
3. Cannulas: Using blunt-tipped cannulas (where appropriate) instead of sharp needles for injections can reduce the number of needle sticks and cause less sharp pain, replacing it with a pushing or pressure sensation.
4. Skilled Technique: Experienced injectors are smoother, more efficient, and use less traumatic techniques, further reducing discomfort.
So, while PRF injections do cause sensations that involve some level of discomfort, and might be perceived as briefly painful by some during the procedure itself, these sensations are typically temporary, well-managed with numbing techniques, and generally considered tolerable. Post-treatment discomfort is usually mild soreness, not significant pain. For the vast majority of patients, the discomfort associated with PRF injections is not a barrier to treatment.
What Areas Can Be Treated with Platelet-Rich Fibrin (PRF)?
The versatility of Platelet Rich Fibrin (PRF) treatment is one of its significant strengths, allowing it to be applied to a wide range of areas across the face, body, and even internally for various aesthetic and medical purposes. Its ability to stimulate tissue regeneration, accelerate healing, and improve overall tissue quality makes it a valuable tool in numerous clinical scenarios. The specific areas treated depend on whether the goal is cosmetic enhancement, functional improvement, or therapeutic healing.
Common areas that can be treated with Platelet-Rich Fibrin (PRF) include:
Aesthetic Applications:
1. Face:
* Full Face: To improve overall skin texture, tone, elasticity, and radiance.
* Under-Eyes: Specifically addressing dark circles, hollowness (tear troughs), fine lines, and crepey skin.
* Cheeks: Improving skin quality, providing subtle volume, and reducing fine lines.
* Around the Mouth (Perioral Area): Softening fine lines, including “smoker’s lines.”
* Forehead: Improving texture and softening fine lines.
* Jawline and Neck: Addressing mild skin laxity and improving skin texture.
* Scars: Treating acne scars, surgical scars, and other depressed or textured scars on the face.
2. Scalp: To stimulate hair growth and improve hair density in areas of hair thinning or loss.
3. Décolletage (Chest) and Hands: To improve skin texture, tone, and reduce the appearance of sun damage and fine lines in these areas often affected by aging.
4. Body Scars and Stretch Marks: PRF can be injected or applied to improve the appearance of scars and stretch marks on various body areas.
Medical and Regenerative Applications:
1. Musculoskeletal System:
* Joints: Injection into joints affected by osteoarthritis or other degenerative conditions to reduce pain and inflammation and potentially stimulate cartilage regeneration (e.g., knees, hips, shoulders).
* Tendons and Ligaments: Injection into injured or chronically painful tendons (e.g., Achilles tendinitis, tennis elbow, rotator cuff issues) and ligaments to accelerate healing and reduce pain.
* Muscles: Can be used to aid in muscle injury recovery.
2. Oral and Maxillofacial Surgery:
* Extraction Sites: Placement in tooth sockets after extraction to promote faster healing and preserve bone volume.
* Bone Grafts: Mixing with bone grafting material or applying as a membrane to enhance bone regeneration for dental implants or reconstructive procedures.
* Periodontal Defects: Used to help regenerate gum tissue and bone around teeth affected by periodontal disease.
3. Wound Care: Application of PRF membranes or gel to chronic, non-healing wounds (e.g., diabetic ulcers, venous ulcers) or burns to accelerate tissue granulation and closure.
4. Post-Surgical Healing: Can be applied to surgical sites in various disciplines to promote faster and better quality tissue healing.
The specific method of PRF preparation (liquid PRF, PRF gel, PRF membrane) and the technique of application (injection, topical application, placement of a solid clot) are chosen based on the characteristics of the area being treated and the specific clinical objective. This wide range of applications highlights PRF’s versatility as a natural, regenerative tool.
What can be treated with PRF?
Platelet Rich Fibrin (PRF) is a remarkably versatile therapeutic agent, capable of treating a diverse array of conditions and concerns across both aesthetic and medical fields. Its fundamental action – stimulating tissue regeneration and accelerating healing through concentrated growth factors and cellular components – makes it applicable wherever the body’s natural repair processes need a powerful, localised boost.
Here’s a comprehensive look at some of the key issues and areas that can be treated with PRF:
-
- Aging Skin: Improving overall skin quality, including texture, tone, radiance, and elasticity on the face, neck, décolletage, and hands.
-
- Fine Lines and Wrinkles: Softening superficial lines and making deeper wrinkles less apparent, particularly around the eyes (crow’s feet), mouth (perioral lines), and on the forehead.
-
- Under-Eye Issues: Addressing dark circles, puffiness, hollowness (tear troughs), and crepey, thin skin beneath the eyes.
-
- Scars: Reducing the appearance of various types of scars, including atrophic acne scars, surgical scars, and stretch marks, by promoting tissue remodelling.
-
- Mild to Moderate Skin Laxity: Improving skin firmness and reducing mild sagging, particularly on the lower face, jawline, and neck.
-
- Hair Loss: Stimulating hair growth and increasing hair density in individuals with non-scarring alopecia, primarily androgenetic alopecia (male and female pattern baldness).
- Enlarged Pores: Helping to reduce the appearance of enlarged pores by improving overall skin structure and elasticity.
Medical & Regenerative Applications:
-
- Osteoarthritis: Injecting into arthritic joints (knees, hips, shoulders, etc.) to reduce pain, decrease inflammation, and potentially stimulate cartilage repair.
-
- Tendon and Ligament Injuries: Treating chronic or acute tendinopathies (e.g., tennis elbow, golfer’s elbow, Achilles tendinitis), sprains, and tears to accelerate healing and reduce pain.
-
- Muscle Injuries: Aiding in the repair and recovery of injured muscle tissue.
-
- Chronic Wounds and Ulcers: Accelerating the healing process in non-healing wounds, such as diabetic ulcers, venous ulcers, and pressure sores.
-
- Oral Surgery and Periodontics: Enhancing bone and gum tissue regeneration after tooth extractions, bone grafting procedures for dental implants, and treatment of periodontal defects.
-
- Maxillofacial Reconstruction: Used in procedures to enhance bone healing and tissue integration.
- Post-Surgical Healing: Can be applied to surgical sites in various medical specialties to promote faster, higher-quality tissue repair and potentially reduce scarring.
The broad applicability of PRF stems from the universal nature of the healing cascade it stimulates – processes vital to the repair and regeneration of nearly all tissue types in the body. By providing a concentrated source of the body’s own growth factors and cells, PRF can effectively enhance these processes wherever needed. The specific preparation and delivery method (injection, topical, membrane) are tailored to the condition and anatomical site.
Platelet-Rich Fibrin (PRF) Injections Treat…
Focusing specifically on the conditions addressed *via injection* of Platelet-Rich Fibrin, we highlight the concerns where direct, targeted delivery of the regenerative material proves most effective. PRF injections are preferred when the therapeutic agents need to reach specific tissue layers (like the dermis, subcutaneous tissue, periosteum, or synovial fluid in joints) or be precisely placed within a localised area of damage or concern.
Platelet-Rich Fibrin (PRF) injections are commonly used to treat:
-
- Fine Lines and Wrinkles: Injected into the dermis or subcutaneous tissue to stimulate collagen and elastin production, reducing the appearance of lines around the eyes (crow’s feet), mouth (perioral lines), forehead, and cheeks.
-
- Under-Eye Dark Circles and Hollowness: Precisely injected under the thin skin of the lower eyelid and into the tear trough area (often as PRF gel) to thicken the skin, improve circulation, reduce pigmentation from visible vessels, and provide subtle volume.
-
- Acne Scars and Other Atrophic Scars: Injected beneath depressed scars to stimulate collagen remodelling and lift the base of the scar, improving texture and blending with surrounding skin.
-
- Mild to Moderate Skin Laxity: Injected in areas like the cheeks, jawline, or neck to improve skin firmness and elasticity by boosting collagen production.
-
- Hair Thinning and Loss: Injected directly into the scalp in areas of miniaturised or dormant hair follicles to stimulate hair regrowth and increase hair density.
-
- Volume Loss (Subtle): PRF gel injections can be used to provide very natural, subtle volume in areas like the cheeks, temples, or under-eyes, often chosen by individuals seeking a more regenerative approach than synthetic fillers.
-
- Joint Pain and Osteoarthritis: Injected directly into affected joints (e.g., knee, shoulder, hip, ankle) to reduce pain and inflammation and promote cartilage health or repair.
-
- Tendon and Ligament Injuries: Injected into the site of injury or chronic pain (e.g., rotator cuff tendon, Achilles tendon, plantar fascia) to accelerate healing, reduce pain, and strengthen tissues.
-
- Muscle Tears: Can be injected into muscle injury sites to facilitate healing and recovery.
- Bone Defects (requiring graft integration): While PRF membranes/clots are often used, injectable PRF or PRF gel can also be used alongside bone grafts in dental or orthopaedic surgery to enhance integration and healing.
The injection method ensures that the concentrated growth factors and cellular components are delivered directly to the intended target tissue, bypassing surface barriers and maximising the local regenerative effect, making it the preferred delivery method for addressing these specific concerns where depth and precision are key.
What Can PRF Treatment Be Used For?
Platelet Rich Fibrin (PRF) treatment is employed for a broad spectrum of applications, fundamentally centered around its ability to stimulate biological regeneration and accelerate healing. Its uses span both aesthetic enhancement and medical therapeutics, making it a versatile tool in modern clinical practice.
PRF treatment can be used for:
1. Skin Rejuvenation: To revitalise aging skin, improve its texture, tone, and elasticity, reduce pore size, and restore a youthful radiance. This is achieved by stimulating collagen and elastin production and improving blood supply.
2. Wrinkle and Fine Line Reduction: To soften the appearance of facial lines, particularly those resulting from volume loss and decreased skin quality, by rebuilding the underlying skin structure.
3. Under-Eye Correction: To specifically address the common concerns of dark circles, hollowness (tear troughs), and fine lines in the delicate under-eye area, providing a natural and regenerative solution.
4. Scar Treatment: To improve the appearance of various types of scars, including acne scars and surgical scars, by promoting tissue remodelling and regeneration in the scarred area.
5. Hair Restoration: To stimulate hair growth and increase hair density in men and women experiencing hair loss or thinning by revitalising dormant hair follicles in the scalp.
6. Volume Enhancement (Subtle & Natural): When processed into a gel form, PRF can be used to provide subtle, natural-looking volume in areas of mild volume loss, such as the cheeks or temples, simultaneously improving skin quality.
7. Wound Healing: To accelerate the closure and healing of chronic wounds, ulcers, and burns that have difficulty healing on their own, by providing a scaffold and concentrated growth factors.
8. Bone and Tissue Regeneration (Medical/Dental): To enhance the healing and integration of bone grafts, promote bone formation, and regenerate soft tissues in dental procedures (like extractions, implants, periodontal surgery) and orthopaedic procedures.
9. Musculoskeletal Injury Treatment: To aid in the repair and recovery of injured tendons, ligaments, muscles, and joints affected by conditions like osteoarthritis, reducing pain and improving function.
10. Adjunct to Other Treatments: PRF