Key Takeaways
-
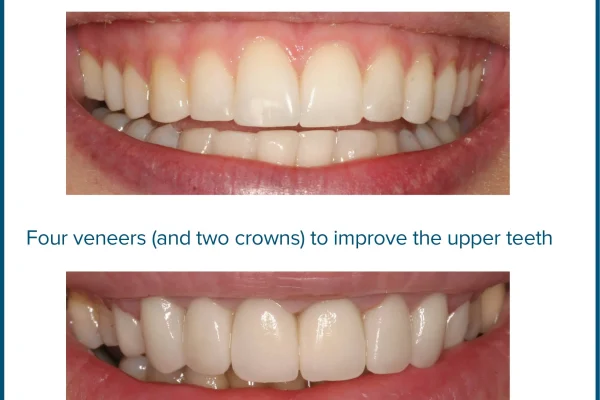
- Porcelain caps (dental crowns) are custom coverings used to *restore* and protect damaged or weakened teeth.
-
- They effectively bring a tooth back to its original shape, size, and strength, significantly improving its function and appearance.
-
- Porcelain is highly valued for its ability to mimic the translucency and color of *natural tooth enamel*, making crowns virtually indistinguishable from surrounding teeth, especially in visible areas.
-
- The process typically involves two appointments: tooth preparation, impression/scan, and permanent bonding.
-
- The cost of a porcelain cap varies significantly (often £500 – £3000+ per tooth), influenced by factors like location, material type, case complexity, and insurance coverage, but is considered a **long-term investment** in oral health.
-
- A well-maintained porcelain crown typically lasts between **5 and 15 years**, but *can* potentially last 20, 30, or even more with optimal care and conditions.
-
- While the porcelain itself cannot decay, the underlying natural tooth structure is still vulnerable to cavities, particularly at the crown’s margin.
-
- Disadvantages can include potential chipping/fracture risk under extreme forces, and the need for significant tooth reduction during preparation.
- Diligent oral hygiene, regular dental check-ups, and avoiding harmful habits are *essential* for maximizing the lifespan and preventing complications with porcelain crowns.
Stepping into the dentist’s office can often feel like entering a foreign land, a place filled with specialised tools, complex terminology, and procedures that sound simultaneously miraculous and slightly intimidating. Among the myriad solutions offered to restore a smile, one stands out for its blend of aesthetic appeal and robust functionality: the porcelain cap. Often referred to by its more formal name, the dental crown, this ubiquitous restoration is a cornerstone of modern reconstructive and cosmetic dentistry. But what exactly is this “cap” or “crown,” and why might your dentist recommend one for you? At its core, a porcelain cap is a custom-made covering designed to encase the entire visible portion of a damaged or weakened tooth. Think of it as a meticulously crafted, high-tech helmet for your tooth, providing protection, restoring its original shape and size, and significantly improving its appearance. Its primary mission is one of preservation and renewal. When a tooth is compromised by extensive decay that’s too vast for a filling, fractured by trauma, severely worn down, or weakened after a root canal procedure where the nerve has been removed (which can make the tooth brittle), a simple filling or bonding won’t suffice. These situations require a more comprehensive solution, something that can bear the brunt of chewing forces while preventing further degradation of the remaining tooth structure. That’s where the porcelain cap steps in. It fits snugly over the prepared tooth, extending down to the gum line, effectively becoming the tooth’s new outer layer. This not only shields the vulnerable underlying tooth from further damage but also restores its structural integrity, allowing it to function normally in chewing and speaking. The material of choice, porcelain, is favoured for its ability to mimic the look and feel of natural tooth enamel, making these restorations particularly popular for visible teeth. The process of getting a cap involves careful preparation of the existing tooth – essentially shaping it down to create a stable base – followed by the creation of the crown in a dental lab (or sometimes in-office using advanced technology) and finally, bonding it securely into place. It’s a multi-step process requiring precision and skill, resulting in a durable, long-lasting, and aesthetically pleasing repair that can dramatically extend the life and utility of a compromised tooth. Understanding this fundamental role is key to appreciating why porcelain caps are such a vital tool in the dentist’s arsenal for maintaining oral health and ensuring smiles remain both healthy and beautiful.
What Are Porcelain Caps and How Do They Work?
Dive a little deeper, and the concept of a porcelain cap unfolds as a remarkable piece of bio-mimicry, a fusion of engineering and artistry designed to seamlessly integrate with your existing oral landscape. At its heart, a porcelain cap, or crown, serves as a surrogate tooth surface, a carefully sculpted shell made from durable ceramic material intended to fit precisely over a tooth that has lost a significant amount of its natural structure or strength. Their function is multi-faceted: they act as guardians, shielding weakened teeth from the immense forces exerted during chewing, which can be upwards of 150 pounds per square inch in the back of the mouth. This protective layer prevents cracks from propagating, decay from spreading further into vulnerable areas, and ensures the tooth can withstand the daily rigors of mastication without risking catastrophic failure. Beyond protection, they are master restorers of form and function. A badly broken or worn tooth not only looks unsightly but can also disrupt your bite, leading to discomfort, jaw pain, and even damage to opposing teeth. A custom-designed porcelain cap brings the tooth back to its original size, shape, and alignment, restoring proper occlusion (the way your upper and lower teeth meet) and allowing you to bite and chew effectively and comfortably again. The process typically begins with your dentist carefully preparing the tooth, which involves removing any decay and shaping the existing tooth structure so that the crown can fit over it without feeling bulky or interfering with your bite. An impression (either traditional putty or a digital scan) is then taken of the prepared tooth and the surrounding teeth, as well as the opposing arch, to ensure the new crown will integrate perfectly into your mouth. This impression is sent to a dental laboratory, where skilled technicians use the information to fabricate the custom porcelain crown, meticulously crafting it to match the colour, shape, and size of your natural teeth. In some modern dental practices, CAD/CAM (Computer-Aided Design/Computer-Aided Manufacturing) technology allows for the crown to be designed and milled from a block of ceramic right there in the office, sometimes even on the same day. Once the permanent crown is ready, it is bonded onto the prepared tooth using a strong dental adhesive, sealing the underlying tooth from bacteria and providing a durable, stable restoration. The aesthetic advantage of porcelain lies in its translucency and ability to be stained and glazed to precisely match the shade of surrounding teeth, making the restoration virtually indistinguishable from natural enamel. This blend of robust mechanical function and superior aesthetic properties makes porcelain caps an incredibly versatile and effective solution for a wide range of dental woes, from structural damage to cosmetic imperfections, providing a second life for teeth that might otherwise be lost. The adaptability of this material, combined with advancements in bonding techniques, has cemented the porcelain cap’s status as a go-to solution for comprehensive dental repair and enhancement, offering patients a durable, functional, and beautiful outcome that feels and looks like a natural part of their smile. It’s not merely a covering; it’s a reconstruction, a reinforcement, and a revitalisation all rolled into one meticulously crafted package.
What is the Difference Between a Cap and a Crown?
In the sometimes perplexing vernacular of dentistry, terms can occasionally overlap or seem confusingly similar, and perhaps no pairing exemplifies this better than “cap” and “crown.” Patients often ask for clarification, wondering if there’s some subtle, clinically significant distinction between the two. The straightforward answer, in the vast majority of dental contexts, is a resounding “there is none.” These two terms are, for all intents and purposes when referring to a dental restoration, completely interchangeable. Both describe the same type of prosthetic device: a custom-made covering that is fitted over the entire visible portion of a tooth, from the gum line upwards, to restore its shape, size, strength, and appearance. Think of it like different words for the same thing – trousers or pants, lift or elevator, boot or trunk (if you’re talking cars). They mean the same object, serving the same fundamental purpose. The term “crown” is the more official, clinical term used by dental professionals in technical discussions, academic literature, and clinical notes. It accurately reflects the way the restoration “crowns” or covers the top of the prepared tooth. “Cap,” on the other hand, is a more colloquial, patient-friendly term. It conjures a simpler image of something being placed over or ‘capped’ onto something else, which is intuitively understandable from a layperson’s perspective. Its use is widespread in everyday conversation between patients and dentists, particularly in informal settings or when a dentist is trying to explain a procedure in easily digestible language. The reasons for this dual terminology aren’t particularly rooted in scientific differences but likely stem from historical usage, regional linguistic preferences, and the evolution of patient education. Some regions or dental practices might lean more heavily on one term than the other out of habit. For example, you might find “dental cap” more common in casual conversation or certain older texts, while “dental crown” is standard everywhere clinically. Ultimately, whether your dentist says you need a “cap” or a “crown,” they are referring to the same vital restoration designed to protect and revitalise a compromised tooth. The function, the materials used (be it porcelain, metal, or a combination), the preparation process, and the intended outcome are identical regardless of which term is employed. So, rest easy knowing that if you hear either word, you’re on the path to reinforcing your smile with the same robust, full-coverage restoration. The key takeaway is not the specific word used, but the understanding that this procedure involves fitting a strong, custom-made covering over your tooth to safeguard its health and structural integrity for the long haul.
What Are Porcelain Crowns?
Let’s zero in specifically on the material that gives “porcelain crowns” their name and, frankly, much of their appeal: dental porcelain. Moving beyond the interchangeable nature of “cap” and “crown,” focusing on the material itself sheds light on why these restorations are so highly valued, particularly for their aesthetic qualities. Porcelain, in the dental context, isn’t the same brittle material you might find in a teacup, though it shares some ceramic origins. Dental porcelain is a highly refined ceramic material, specifically engineered for strength, durability, and the ability to mimic the optical properties of natural tooth enamel. When we talk about porcelain crowns, we are referring to crowns where the primary restorative material used is this advanced dental ceramic, whether it’s entirely made of porcelain (an all-ceramic crown) or fused over a metal or zirconia substructure (like Porcelain-Fused-to-Metal or Zirconia-based crowns with a porcelain layer). The magic of dental porcelain lies in its unique characteristics that make it an exceptional choice for restoring teeth, especially those that are visible when you smile or speak. Natural tooth enamel isn’t uniformly opaque; it possesses a subtle translucency that allows light to pass through it and reflect off the underlying dentin, giving teeth their depth and natural lustre. High-quality dental porcelain is manufactured to replicate this translucency, allowing crowns to blend seamlessly with adjacent natural teeth rather than looking flat or artificial. Furthermore, porcelain can be meticulously coloured, shaded, and stained by skilled dental technicians to precisely match the hue, value, and chroma of your surrounding teeth, taking into account the variations within a single tooth and across your entire smile. The surface can also be glazed and polished to mimic the natural texture and light-reflecting qualities of enamel. This meticulous attention to detail in crafting porcelain crowns is what elevates them from simple dental repairs to pieces of dental artistry. They encase the entire visible portion of the prepared tooth, acting as its new exterior, effectively replacing lost enamel and dentin with a material that is both strong and beautiful. The process involves shaping the tooth, taking a precise impression, and then the lab technician (or CAD/CAM machine) building the crown layer by layer or carving it from a block of porcelain. Once fabricated, the crown is carefully fitted, adjusted for bite, and permanently bonded to the prepared tooth. While porcelain is renowned for its aesthetics, modern dental porcelains and ceramics, such as lithium disilicate (often marketed as E-Max) and certain types of zirconia layered with porcelain, also offer impressive strength, making them suitable for areas of higher chewing force. This evolution in materials means that “porcelain crown” now encompasses a range of ceramic options, all leveraging the aesthetic potential of porcelain while addressing the need for robustness, providing dentists with versatile tools to restore smiles with materials that are durable, biocompatible (well-tolerated by the body), and remarkably natural-looking. It’s a sophisticated solution for restoring not just the function, but the natural beauty of a tooth, ensuring that your smile looks and feels whole again.
How Much Do Porcelain Caps Cost?
Ah, the inevitable question that accompanies any significant dental procedure: the price tag. Understanding the cost of porcelain caps, or crowns, is crucial for budgeting and making informed decisions about your dental health, but it’s rarely a single, simple number. The expense associated with getting a porcelain dental crown can vary quite dramatically, fluctuating based on a constellation of factors that reflect the complexity of the procedure, the materials used, the expertise involved, and even geographical location. On average, you might find the cost ranging anywhere from a few hundred pounds in some regions or with certain insurance plans, potentially up to several thousand pounds per tooth in more complex cases, higher-cost-of-living areas, or specialist practices. This isn’t merely paying for a piece of material; you’re investing in a highly skilled service that includes the dentist’s diagnostic expertise, the preparation of the tooth, the precision required to take accurate impressions or scans, the custom fabrication of the crown (which often involves intricate lab work by a skilled technician), the temporary crown needed between appointments, and the final placement and bonding of the permanent crown, along with follow-up checks. Each step demands specific materials, equipment, and a significant amount of professional time and training. Location plays a huge role; dental fees often reflect the general cost of living and operating a business in a particular area. A crown fitted in a major metropolitan city centre is likely to be more expensive than one in a rural town. The dentist’s experience and reputation can also influence cost; a highly experienced specialist might charge more for their expertise. Furthermore, the specific type of porcelain or ceramic material used matters. While often grouped under the “porcelain” umbrella, modern ceramics like E-Max or various types of zirconia crowns can have different costs associated with their material expense and manufacturing process. Is it a complex case involving multiple teeth or requiring foundational work like a root canal or build-up before the crown can be placed? Such complexities add to the overall fee. And, crucially, dental insurance coverage is a significant variable. Most dental insurance plans cover a portion of the cost of crowns, especially when they are deemed medically necessary to restore function after decay or breakage. However, coverage levels vary widely depending on your specific plan, deductible, annual maximums, and whether the procedure is classified more towards restorative or cosmetic. It’s essential to consult with your dentist’s office and your insurance provider beforehand to get an accurate estimate of your out-of-pocket expense. Considering the potentially long lifespan of a porcelain crown and its role in preserving the underlying tooth structure and maintaining oral health, many view the cost as a worthwhile long-term investment compared to alternative treatments or, worse, doing nothing and potentially losing the tooth entirely, which would necessitate far more expensive interventions like bridges or implants down the line.
What is the Cost of a Dental Cap?
Delving into the specific cost components of a dental cap, or crown, reveals that the figure quoted by your dentist encompasses much more than just the physical crown itself. When you’re given an estimate for a dental cap, you’re essentially receiving a package price for the entire restorative process, which is inherently tied to the labour-intensive, highly technical nature of placing a custom-fit dental prosthesis. While it’s challenging to give a universally applicable number without knowing your specific circumstances, typical ranges in the UK, for example, might fall between £500 to £1,500 or more per crown, sometimes reaching higher depending on the factors previously mentioned. In the US, this range can be significantly wider, potentially $800 to $3,000+ per tooth. Breaking down what contributes to this figure provides clarity. Firstly, there’s the dentist’s fee for the preparation appointment. This includes their time for the initial examination, diagnosis, planning, administering local anaesthesia, removing any existing decay or old filling material, shaping the tooth into the necessary form (the “prep”), and taking the impressions or digital scans. Then, there’s the cost of the temporary crown, which you wear for a week or two while the permanent crown is being fabricated. Although temporary, crafting and fitting this also requires materials and the dentist’s time. The lion’s share of the cost often goes towards the laboratory fee. Unless your dentist uses chairside CAD/CAM technology, your crown will be made by a specialised dental laboratory technician. These technicians are highly skilled artisans who meticulously build or mill your crown based on the impressions, ensuring it fits perfectly, functions correctly, and matches your natural teeth aesthetically. Their fee reflects the cost of the high-quality ceramic materials used, the sophisticated equipment required (like furnaces for firing porcelain or milling machines for zirconia), and their expertise and labour. Finally, there’s the fee for the second appointment, where the dentist removes the temporary crown, fits the permanent one, checks the margins, ensures the bite is correct, and permanently bonds the crown to your tooth. This fee covers their time, the bonding materials, and any necessary adjustments. Additional costs can arise if the tooth requires preliminary procedures before the crown can be placed, such as a filling to build up insufficient tooth structure (a “core build-up”) or root canal therapy to address nerve damage. If the tooth and gums aren’t healthy enough for immediate crowning, preliminary periodontal treatment might also be necessary. Understanding that the quoted cost covers this entire ecosystem of diagnosis, preparation, fabrication, and placement helps to contextualise the investment. It’s not merely the material cost of the porcelain itself, which is relatively small compared to the overall fee, but the sum of the skilled labour, precision technology, customisation, and clinical expertise required to successfully restore your tooth with a durable, well-fitting, and aesthetically pleasing dental cap.
Why Are Porcelain Crowns So Expensive?
The question of why porcelain crowns carry a significant price tag is valid and often stems from the perception that it’s “just covering a tooth.” However, the reality is that the cost reflects the intricate confluence of high-quality materials, advanced technology, and highly skilled labour involved in their creation and placement. It’s a bespoke restoration, tailored specifically to your mouth, your tooth, and your bite, which is inherently more costly than a mass-produced item. Firstly, the materials themselves, particularly advanced dental ceramics like lithium disilicate (E-Max) or aesthetic zirconia, are not inexpensive. These are not standard pottery materials; they are biocompatible, high-strength ceramics engineered to withstand the harsh environment of the mouth, resist wear, and mimic natural tooth structure optically. Developing and manufacturing these materials requires significant research and sophisticated processes. Secondly, the fabrication process is highly technical. Whether a crown is made in a dental lab by a technician or milled in-office using CAD/CAM technology, it requires specialised, expensive equipment. Dental labs utilise precision furnaces, staining palettes, and sometimes CAD/CAM systems. Chairside milling requires state-of-the-art scanners, design software, and milling machines, which represent a substantial capital investment for a dental practice. But perhaps the most significant factor contributing to the cost is the human expertise involved. Your dentist’s role goes beyond simply placing the crown; it begins with a thorough diagnosis, treatment planning, and executing a precise tooth preparation. This shaping of the tooth is a critical step that requires anatomical knowledge, manual dexterity, and an understanding of biomechanics to ensure the crown fits correctly and can withstand chewing forces without failing or damaging surrounding tissues. A poorly prepared tooth can lead to crown failure, tooth sensitivity, or periodontal problems. Furthermore, if the crown is fabricated in a lab, the dental technician who creates it is an artisan with years of training and experience. They don’t just follow a template; they interpret the dentist’s prescription and the tooth impressions to create a restoration that is unique in shape, size, and colour, meticulously layering or staining the porcelain to achieve a natural look. This level of custom craftsmanship is time-consuming and requires a keen artistic eye as well as technical skill. Finally, the placement appointment involves careful fitting, checking the bite, and permanently bonding the crown. The bonding process itself uses specialised dental adhesives and techniques to create a strong, durable seal. All of these steps – the advanced materials, the precision technology, the dentist’s clinical skill, and the lab technician’s artistry – contribute to the overall cost. You are paying for a durable, functional, and aesthetic restoration that has been custom-engineered and handcrafted for your specific needs, designed to last for many years and protect the health of your tooth, which, in the complex system of the mouth, is a valuable asset worth preserving.
How Long Do Porcelain Caps Last?
The lifespan of a porcelain cap, or crown, is a frequent and important question, and the answer, while not a simple fixed number, is generally encouraging. These restorations are designed to be durable, functional, and long-lasting, serving their purpose for many years. However, their longevity is not solely determined by the material they are made from but is heavily influenced by a multitude of factors related to oral hygiene, lifestyle habits, the tooth’s original condition, the crown’s location in the mouth, and the skill with which it was prepared and placed. On average, you can realistically expect a well-maintained porcelain crown to last somewhere between 5 and 15 years. This is a broad range, highlighting the variability involved. Some crowns may need replacement sooner due to unforeseen issues, while others can far exceed this average. The foundation on which the crown is placed is critically important; if the underlying tooth is severely compromised or experiences issues like decay or fracture underneath the crown, the restoration’s life will be shortened. Your daily oral hygiene routine is paramount. Meticulous brushing and flossing, paying particular attention to the gum line around the crowned tooth, are essential to prevent plaque buildup, gum disease, and recurrent decay at the margin where the crown meets the natural tooth. Regular check-ups and cleanings with your dentist and hygienist are also crucial for monitoring the crown’s condition, checking the surrounding gum health, and identifying any potential issues early. Chewing habits can significantly impact durability. Grinding or clenching your teeth (bruxism), habitual chewing on hard objects like ice or pens, or using your teeth to open packaging can place excessive stress on the porcelain, increasing the risk of chipping or cracking. Wearing a nightguard if you grind your teeth can help protect your crowns and natural teeth. The location of the crown in your mouth also plays a role; crowns on front teeth are primarily for aesthetics and subject to less intense chewing forces than those on molars, which bear the brunt of heavy chewing. Therefore, molars might experience more wear and tear over time. Furthermore, the initial quality of the crown’s fabrication and the precision of its fit by the dentist are fundamental to its long-term success. A well-made, properly bonded crown with seamlessly sealed margins is less likely to develop problems. While an average lifespan is a useful guideline, it’s best to discuss expected longevity with your dentist based on your specific situation and habits. Investing time and effort in proper care is the single most effective way to maximise the lifespan of your porcelain cap, ensuring it protects your smile effectively for as many years as possible, demonstrating the principle that proactive maintenance pays significant dividends in the world of dental health.
Can a Porcelain Crown Last 20 Years?
Yes, absolutely, a porcelain crown *can* last 20 years or even longer, although achieving this kind of longevity often requires a combination of ideal circumstances, diligent care, and sometimes a bit of good fortune. While the average lifespan is cited as 5 to 15 years, these are averages; the potential for a much longer service life exists and is not uncommon, especially with advancements in modern dental materials and techniques. Reaching the two-decade mark with a single porcelain crown moves it into the category of a truly successful, long-term restoration. The key factors that contribute to a porcelain crown’s ability to last 20 years are largely the same ones that influence its average lifespan, but they must be present and consistently maintained over a significantly longer period. The underlying tooth structure must remain healthy and free from new decay. This means impeccable oral hygiene is non-negotiable. Brushing twice a day, flossing daily, and using interdental brushes if recommended by your hygienist are vital for keeping the margins of the crown clean and preventing bacteria from infiltrating underneath. Regular professional dental check-ups are equally important. Your dentist and hygienist can spot early signs of potential issues, such as marginal leakage, gum recession exposing the crown edge, or changes in your bite that could be stressing the crown. They can also provide professional cleanings that remove stubborn plaque and calculus. The absence of adverse habits is also critical. Chronic teeth grinding or clenching without protection can exert forces that even the strongest porcelain can’t withstand indefinitely, leading to cracks or fractures over time. Wearing a custom-fitted nightguard if you grind your teeth can help protect your crowns and natural teeth. Avoiding using the crowned tooth (or any tooth, for that matter) to bite down on extremely hard foods like hard candy, ice, or nuts, or using teeth as tools, is essential to prevent chipping or fracture. The crown’s original condition and fit are foundational; a crown that was perfectly fabricated, meticulously bonded, and fitted with seamless margins and correct bite alignment from day one has a significantly higher chance of lasting longer. The location of the crown also matters; a crown on a front tooth, subjected primarily to biting forces rather than heavy chewing, might naturally last longer than one on a molar, assuming similar levels of care. Advances in ceramic materials themselves are also increasing the potential for extended lifespans. Newer materials like high-strength zirconia or reinforced porcelains are inherently more durable than older types. So, while a 20-year lifespan isn’t guaranteed for every porcelain crown, it is certainly achievable with diligent home care, regular professional maintenance, protective habits, and a high-quality initial restoration, representing a testament to the potential longevity and value of this type of dental work when all the stars align in your favour.
Can a Crown Last 30 Years?
Pushing the boundary even further, the question arises: can a dental crown, specifically a porcelain one, truly last a remarkable 30 years? While statistically less common than a 10 or 20-year lifespan, the answer is still yes, it is within the realm of possibility for a crown to serve its purpose for three decades or even longer, becoming a lifelong companion for that particular tooth. Achieving a 30-year lifespan for a porcelain crown places it firmly in the category of exceptional longevity, bordering on outperforming even some natural teeth which might succumb to decay or wear over that period. This kind of extended service requires a confluence of near-perfect conditions and unwavering commitment to oral health. Firstly, the factors that contribute to a 20-year lifespan become even more critical and must be maintained *consistently* for an extended duration. This means impeccable, lifelong oral hygiene – a routine of brushing, flossing, and interdental cleaning so ingrained it’s second nature, effectively preventing decay and gum issues around the crown margins for decades. It means religious adherence to regular dental check-ups and professional cleanings, allowing your dental team to monitor the crown’s integrity, detect microscopic issues before they escalate, and maintain the surrounding periodontal health. Avoiding all damaging habits – no tooth grinding (or consistent nightguard use), no biting on hard objects, no using teeth as tools, period. The tooth underneath the crown must remain healthy; this means no new decay, no nerve issues requiring root canal treatment post-crowning (unless it was already root canal treated), and no root fractures. The initial placement and quality of the crown must be of the highest standard. A crown with even slight marginal discrepancies or a less-than-perfect bite fit is unlikely to withstand the test of 30 years of chewing forces. The material itself also plays a significant role. Newer, high-strength ceramic materials might inherently have a greater potential for extreme longevity than older or less robust porcelains. Location in the mouth is also a factor; a crown on a front tooth typically faces less stress over its lifetime compared to a back molar. Systemic health can even influence oral health over such a long period, potentially impacting gum health which is vital for crown retention. Ultimately, a 30-year-old porcelain crown is a testament to optimal patient care, high-quality dentistry, durable materials, and the absence of significant oral health complications or trauma over three decades. It’s not the average outcome, but it is a possible, and deeply satisfying, result of a successful restoration and a lifetime commitment to maintaining oral health, showcasing the incredible potential of modern dental materials and care when everything aligns perfectly.
Do Porcelain Crowns Crack?
Yes, it is a reality that porcelain crowns, while engineered for strength and durability, *can* crack or chip under certain circumstances. While modern dental ceramics are remarkably resilient and far stronger than the porcelains used decades ago, they are not indestructible. They are subject to the significant forces generated within the mouth during daily function, and just like natural tooth enamel, they have their limits. Understanding the potential for cracking and its causes is important for patients with porcelain crowns. The primary culprits behind a chipped or cracked porcelain crown are often excessive forces or trauma. Biting down unexpectedly hard on something rigid – like a piece of bone, a seed, unpopped popcorn kernels, or even using the tooth to open packaging – can generate a concentrated impact force that exceeds the material’s fracture strength, resulting in a chip or a more significant crack. Chronic habits like teeth grinding or clenching (bruxism) are another major risk factor. The repetitive, intense pressure and abrasive action of grinding teeth, especially during sleep, can gradually wear down the porcelain or lead to stress fractures that eventually manifest as cracks. Patients known to grind their teeth are often advised to wear a custom-fitted nightguard to protect their crowns and natural teeth from these destructive forces. Trauma to the face or mouth, such as a fall or sports injury, can also cause porcelain crowns to chip, fracture, or even become dislodged. Even without external trauma or habits, the location of the crown matters; molars subjected to heavy chewing forces are generally at a higher risk of fracture than front teeth. Furthermore, the type of porcelain used influences its susceptibility to cracking. Older, more brittle porcelains or Porcelain-Fused-to-Metal (PFM) crowns where the porcelain layer is relatively thin and unsupported in certain areas might be more prone to chipping compared to monolithic (single block) crowns made from high-strength ceramics like E-Max or zirconia. Small chips, particularly on the edges of front teeth, can sometimes be polished smooth or repaired using composite resin bonding if the damage is minor and doesn’t affect the crown’s structural integrity or marginal seal. However, a significant crack or fracture that compromises the fit, function, or seal of the crown typically necessitates replacement of the entire crown to prevent decay or damage to the underlying tooth. While the possibility of cracking exists, it shouldn’t deter you from choosing a porcelain crown if it’s the recommended treatment; with proper care, avoiding harmful habits, and being mindful of what you chew on, the risk can be significantly minimised, and the vast majority of porcelain crowns serve their purpose without fracturing.
What Are the Advantages of Porcelain Crowns?
Choosing a porcelain crown comes with a host of compelling advantages that make them one of the most popular and frequently recommended dental restorations available today. Their benefits span both functional and aesthetic realms, offering solutions that are robust, durable, and capable of restoring not just the health but the natural beauty of a smile. Perhaps the most celebrated advantage is their unparalleled aesthetic quality. Porcelain can be crafted to mimic the natural translucency, colour, and texture of tooth enamel with remarkable precision. Skilled dental technicians can layer and stain porcelain to match the subtle variations in shade found in natural teeth, ensuring the crown blends seamlessly with its neighbours. This makes porcelain crowns the go-to choice for restoring teeth that are visible when you smile or speak, as they are virtually indistinguishable from natural teeth, creating a natural and attractive appearance that metal crowns simply cannot replicate. Beyond looks, modern porcelain crowns, particularly those made from materials like E-Max or zirconia (which can be layered with aesthetic porcelain), offer impressive strength and durability. While older porcelains might have been more prone to chipping, contemporary ceramic materials are engineered to withstand the significant chewing forces present in the mouth, making them suitable for both front and back teeth depending on the specific material chosen. Another significant advantage is their biocompatibility. Porcelain is a ceramic material that is well-tolerated by gum tissues and doesn’t typically cause allergic reactions, unlike some metals used in other types of crowns. This makes them a suitable option for patients with metal sensitivities and contributes to healthy gum tissue around the crown margins. The smooth, glazed surface of porcelain is also resistant to staining, meaning your crown is unlikely to discolour over time in the way natural enamel or some other restorative materials might, helping to maintain a consistent, bright smile. Furthermore, because they cover the entire visible portion of the tooth, porcelain crowns effectively restore the tooth’s original shape and size, re-establishing proper contact points with adjacent teeth and contributing to a healthy bite (occlusion). This restoration of form prevents issues like teeth shifting or uneven wear. For teeth that are severely damaged, weakened by large fillings, or brittle after root canal treatment, a porcelain crown provides essential structural support, holding the remaining tooth together and protecting it from fracture, thereby preserving the tooth for many more years. Considering their ability to combine high strength with exceptional aesthetics and biocompatibility, the advantages of porcelain crowns make them an excellent choice for a wide range of restorative needs, offering patients a durable, functional, and naturally beautiful solution for a compromised tooth. They represent a harmonious blend of engineering, science, and art, designed to bring your smile back to its full glory.
Is a Porcelain Dental Crown Good?
Posing the question “Is a porcelain dental crown good?” is akin to asking if a tailor-made suit or a precision-engineered watch is good – if the criteria are performance, aesthetics, and lasting value, then the answer is unequivocally yes, a porcelain dental crown is very good, often excellent, depending on the specific situation and material type. Porcelain crowns are widely regarded by dentists and patients alike as a premier choice for dental restoration due to their powerful combination of functional benefits and outstanding aesthetic properties. They are particularly good when the goal is to restore a tooth’s integrity and appearance simultaneously, making them an ideal solution for visible teeth in the smile line (incisors, canines, and premolars), though increasingly, high-strength porcelains and ceramics are used for molars as well. Their ability to be sculpted, shaded, and matched to surrounding teeth is arguably their greatest strength, allowing them to blend so seamlessly that it becomes difficult, if not impossible, to distinguish the crown from natural enamel. This level of naturalness is simply unmatched by traditional metal restorations. Beyond the cosmetic aspect, a porcelain crown is “good” because it provides substantial structural support to a compromised tooth. When a tooth is weakened by a large cavity, a fracture, or has undergone root canal therapy which can make it brittle, a filling or bonding isn’t sufficient to protect it from the heavy forces of chewing. A crown encases the entire tooth, holding it together, preventing further breakage, and restoring its ability to function normally. This protection is critical for preserving the tooth long-term. Modern porcelain materials, especially those like E-Max or monolithic zirconia (which can be layered with porcelain for aesthetics), are also quite strong and resistant to wear, making them reliable even in areas of higher stress, though the specific material choice is crucial here. They are also biocompatible, meaning they are well-tolerated by the surrounding gum tissues and unlikely to cause adverse reactions. While no dental restoration is perfect or lasts forever, a porcelain crown, when indicated for the right clinical situation, expertly fabricated, and meticulously placed, represents a highly effective, durable, and aesthetically superior solution for restoring a damaged tooth. It provides robust protection while revitalising the appearance of your smile, making it a genuinely “good” investment in both your oral health and self-confidence. The widespread adoption and continued advancements in porcelain crown technology by the dental community are strong indicators of their proven efficacy and positive impact on patient outcomes.
Why Do Dentists Use Porcelain Crowns?
Dentists choose to use porcelain crowns for a variety of compelling clinical and aesthetic reasons, making them a staple in contemporary restorative dentistry practices. Their versatility and ability to address multiple issues simultaneously are key factors in their frequent recommendation. Primarily, dentists favour porcelain crowns for their exceptional aesthetic capabilities. In an era where patients increasingly value both function and appearance, porcelain’s ability to be customised to match the colour, shape, and size of natural teeth is unmatched by other materials like metal alloys. Dentists understand that restoring a tooth, especially in a visible area, isn’t just about function; it’s about restoring a patient’s smile confidence. Porcelain allows them to achieve this harmonious blend of repair and cosmetic dentistry enhancement. The translucency of dental porcelain is particularly appealing; it mimics the way light interacts with natural enamel, resulting in a lifelike appearance that prevents the tooth from looking opaque or artificial. Clinically, porcelain crowns are indicated in numerous scenarios where a tooth requires full coverage protection. Dentists turn to them when a tooth has suffered extensive decay that has compromised its structural integrity beyond what a filling can repair. They are essential for fractured or broken teeth, providing a strong shell that holds the remaining pieces together and prevents further fracture. A common reason is after root canal therapy; a root canal-treated tooth, while saved, becomes brittle and significantly weaker due to the removal of the pulp and often the need for a large access cavity. Crowning such a tooth with porcelain provides the necessary reinforcement to prevent it from breaking under chewing forces. Dentists also use porcelain crowns to correct significant cosmetic issues like severe discolouration, misshapen teeth, or misalignment where orthodontics isn’t suitable or desired, effectively giving the tooth a complete “facelift.” Furthermore, porcelain is biocompatible, making it a safe choice for patients and promoting healthy gum tissue response around the restoration. The material is also resistant to wear and tear, and its smooth surface makes it less likely to accumulate plaque compared to roughened natural tooth surfaces or certain other restorative materials, assuming good oral hygiene is maintained. While specific types of porcelain or ceramics (like zirconia or E-Max) might be chosen based on the tooth’s location and the required strength, the overarching reason dentists widely employ porcelain and ceramic crowns is their proven track record in providing durable, functional, and highly aesthetic restorations that meet the complex needs of modern dental care, effectively preserving teeth and smiles for the long term.
What Are the Disadvantages of Porcelain Crowns?
While porcelain crowns offer significant advantages, particularly in aesthetics, they are not without their potential drawbacks. Like any dental material or procedure, porcelain comes with certain limitations and considerations that patients should be aware of before choosing this type of restoration. Understanding these potential disadvantages provides a balanced perspective and helps in making an informed decision in consultation with your dentist. One of the most frequently cited potential disadvantages of porcelain crowns, particularly older or less robust types, is their susceptibility to chipping or fracture. While modern ceramics are much stronger, concentrated forces, like biting down hard on something unexpected, grinding teeth, or experiencing trauma, can still cause the porcelain to chip or, in more severe cases, crack the entire crown. This can necessitate repair (for minor chips) or complete replacement (for significant fractures), adding unexpected costs and inconvenience. Another consideration is the amount of tooth structure that typically needs to be removed to prepare a tooth for a porcelain crown. To create sufficient space for the porcelain material and ensure the crown isn’t bulky, the underlying tooth often needs to be significantly shaped down. This preparation is irreversible, meaning the tooth will always require a crown or similar restoration going forward. In some cases, particularly with Porcelain-Fused-to-Metal (PFM) crowns, the porcelain can cause wear on the opposing natural teeth over time, especially if the porcelain surface is not perfectly smooth or if the patient has a heavy bite or grinding habit. All-ceramic crowns, particularly newer materials, are often designed to be less abrasive to opposing enamel, but it remains a factor to consider. Porcelain crowns, especially those made of translucent materials like traditional porcelain or some all-ceramics, might show the colour of the underlying prepared tooth structure if it is discoloured or if there is a metal post or build-up present, although dentists use opaquers and different bonding cements to minimise this risk. For PFM crowns, the metal margin at the gum line can sometimes become visible if the gums recede, creating an unsightly grey line. While technically a material issue within a type of porcelain crown, this aesthetic drawback is often associated with “porcelain” restorations. Finally, as discussed earlier, the cost of porcelain crowns can be higher than other restorative options, such as metal crowns or large fillings, reflecting the material cost, manufacturing complexity, and aesthetic customisation involved. While often a worthwhile investment, the initial expense can be a disadvantage for some patients. Being aware of these potential downsides allows for a more realistic expectation and encourages practices that can mitigate risks, such as avoiding hard foods and using a nightguard if needed, ensuring the longevity and success of the porcelain crown while minimising the likelihood of encountering these disadvantages.
What is the Disadvantage of Porcelain Crowns?
To distil the core disadvantage of porcelain crowns, it often boils down to a trade-off between aesthetics and inherent material properties compared to alternatives, primarily their potential vulnerability to fracture and the preparatory tooth reduction required. While aesthetics are their superpower, making them look incredibly natural, porcelain, especially when used on its own without a strong substructure (in some older all-ceramic types) or as a thin veneer over metal (in PFM crowns), can be more brittle than metal alloys or even newer monolithic ceramic materials like zirconia. This means there’s a higher potential risk of chipping or fracturing under excessive biting forces or impact trauma compared to, say, a full gold crown or a monolithic zirconia crown, particularly in patients who grind their teeth heavily or have a very strong bite. This inherent brittleness is a key disadvantage; while repairs for small chips are sometimes possible, a significant fracture often means the entire crown needs to be replaced, incurring additional cost and inconvenience. Furthermore, the preparation of the natural tooth to receive a porcelain crown is often more extensive than for other types of restorations. A certain minimum thickness of porcelain is required to ensure adequate strength and aesthetics, necessitating the removal of more tooth structure compared to, for instance, a full gold crown, which can be thinner. This removal of healthy tooth structure is an irreversible step. While necessary for a successful crown, it means the tooth will permanently require a crown for protection. Lastly, while porcelain itself is stain-resistant, issues can still arise around the margins, and in the case of Porcelain-Fused-to-Metal crowns, the underlying metal can potentially show through or become visible at the gum line over time if the gums recede, creating a grey shadow that compromises the aesthetic benefit. So, while they excel in blending in beautifully with your natural teeth, the primary disadvantages centre around the material’s relative brittleness under extreme stress compared to metals or monolithic ceramics, the amount of tooth reduction required for placement, and potential aesthetic issues related to the underlying tooth or substructure showing through or being exposed by gum recession. These points highlight the importance of discussing the best material choice for your specific tooth location, bite forces, and aesthetic goals with your dentist.
Do Porcelain Crowns Look Natural?
This is arguably the biggest selling point and a primary reason why porcelain crowns are so widely used, especially for teeth visible in the smile. The simple answer is a resounding “yes, absolutely.” One of the foremost advantages and defining characteristics of porcelain crowns is their exceptional ability to look incredibly natural, often blending so seamlessly with adjacent teeth that it becomes challenging for anyone, even a dentist, to spot the difference. This natural appearance isn’t accidental; it’s a result of the material’s intrinsic properties and the meticulous craftsmanship involved in creating these restorations. Natural tooth enamel is not a single, opaque colour. It has a certain depth, translucency, and subtle variations in shade and texture. High-quality dental porcelain is specifically formulated to replicate these optical properties. Its translucency allows light to penetrate the surface and reflect off the underlying tooth structure (or the bonding cement), just like natural enamel, which gives the crown a lifelike depth and prevents it from looking flat or opaque like a solid block of material. Furthermore, dental porcelain is available in a wide spectrum of shades, and skilled dental technicians can use layering and staining techniques to replicate the subtle colour variations, gradients, and characteristics found in natural teeth, ensuring the crown blends harmoniously with your existing dentition. The custom fabrication process allows the crown to be shaped and contoured precisely to match the anatomy of a natural tooth, including surface texture and ridges, further enhancing its realistic appearance. Achieving this high level of naturalness is dependent not only on the material but also on the skill and artistry of both the dental lab technician who crafts the crown and your dentist who prepares the tooth, takes accurate impressions, selects the shade, and meticulously fits and bonds the crown, ensuring the margins are seamless and the bite is correct. While older porcelain materials or less precise techniques could sometimes result in crowns that appeared less natural (e.g., too opaque or the wrong shade), modern advanced ceramics like E-Max and high-translucency zirconia, combined with sophisticated CAD/CAM technology and skilled lab work, make it possible to create restorations that are astonishingly lifelike. For patients seeking to restore both the function and the natural beauty of a damaged tooth, the ability of porcelain crowns to integrate seamlessly into the smile is a significant advantage, providing confidence and a natural aesthetic outcome that is a hallmark of high-quality cosmetic dentistry.
Do Porcelain Crowns Turn Yellow?
This is a common concern rooted in the understanding that natural teeth can discolour over time due to factors like diet, aging, and lifestyle habits. However, the good news regarding porcelain crowns is that the ceramic material itself is highly resistant to staining and does *not* inherently turn yellow or change colour over time in the way natural tooth enamel does. The porcelain surface is very smooth and non-porous once it is glazed and fired, making it exceptionally resistant to absorbing pigments from foods, drinks like coffee, tea, or red wine, and tobacco smoke, which are common culprits for staining natural teeth. So, the porcelain material of your crown will maintain its original shade for years and years. However, while the crown material itself won’t discolour, it’s important to understand where potential colour issues *could* arise, which might give the *appearance* of the crown turning yellow or looking discoloured relative to adjacent teeth. Firstly, the natural teeth surrounding the crowned tooth *will* continue to age and potentially pick up stains over time. If you were to whiten your natural teeth after getting a porcelain crown, the crown would not whiten with them, and it might then appear relatively darker or yellower compared to your newly brightened natural teeth. This is why it’s often recommended to consider any desired teeth whitening *before* getting a crown made, so the crown can be matched to your whitened shade. Secondly, staining or discolouration can occur *around* the porcelain crown, particularly at the margin where the crown meets the natural tooth structure or the gum line. Plaque and calculus (hardened plaque) can build up around this margin, and these deposits can become stained, giving the *appearance* of the crown being discoloured, especially around its edges. This highlights the critical importance of diligent oral hygiene, including thorough brushing and flossing around the crowned tooth, to prevent such buildup. Gum recession can also expose the margin of the crown or, in the case of Porcelain-Fused-to-Metal (PFM) crowns, potentially expose the underlying metal collar, which can look grey or dark near the gum line (though this is not the crown turning yellow, it’s a change in appearance). In rare cases, if the bonding cement used to attach the crown was not completely light-cured or if there were issues during the bonding process, the cement itself might discolour slightly over a very long period, potentially affecting the crown’s overall appearance. But focusing specifically on the porcelain material, you can be confident that the ceramic itself is highly colour stable and will not turn yellow from external staining agents. Maintaining good oral hygiene and regular dental check-ups are key to ensuring the entire restoration and surrounding tissues remain healthy and aesthetically pleasing.
Do Porcelain Teeth Look Fake?
The goal of modern restorative dentistry, particularly with materials like porcelain, is precisely the opposite: to make the restoration look as natural and *unfake* as possible. When skillfully crafted and placed, porcelain crowns are designed to blend seamlessly with your natural smile, making them virtually undetectable to the casual observer. The potential for a porcelain crown to look “fake” is usually less about the material itself and more about the quality of the execution – the skill of the dental team and the dental lab technician involved, and the specific characteristics of your individual mouth. As discussed, high-quality dental porcelain possesses a lifelike translucency and can be matched precisely in colour and shape to your existing teeth. A skilled technician will study the nuances of your natural dentition – the subtle variations in shade from the top to the bottom of the tooth, the unique contours and surface textures, the way light reflects off the enamel – and replicate these details in the porcelain. A skilled dentist ensures the tooth preparation allows for adequate porcelain thickness to achieve the desired aesthetic, selects the correct shade, verifies the fit and appearance before permanent bonding, and manages the gum tissue to ensure a healthy, natural-looking emergence profile from the gums. When all these elements come together correctly, the porcelain crown should be indistinguishable from a natural tooth. However, instances where porcelain teeth might appear less natural can occur. If the porcelain is too opaque, it can look flat and lifeless compared to the surrounding teeth. If the colour match is off, it will stand out. If the shape is generic or doesn’t harmonise with your other teeth and facial features, it can look artificial. In Porcelain-Fused-to-Metal (PFM) crowns, the underlying metal can create an opaque look or, if the gums recede, expose a visible grey line at the margin, which is a dead giveaway of dental work. Poor tooth preparation or inadequate bonding can also compromise the final aesthetic result. Thankfully, with advancements in ceramic materials like high-translucency zirconia and lithium disilicate (E-Max), and increasingly sophisticated CAD/CAM technology and traditional lab techniques, the ability to create stunningly natural-looking porcelain restorations is better than ever. Choosing an experienced dentist and dental lab, and communicating your aesthetic goals are key steps in ensuring your porcelain crowns look genuinely natural, not fake, allowing you to smile with complete confidence. The vast majority of patients with modern, well-done porcelain crowns enjoy restorations that are virtually invisible in their smile.
Why Do Crowns Turn Grey?
When a dental crown appears to turn grey, it’s usually not the porcelain material itself undergoing a chemical change to grey. This aesthetic issue is almost exclusively associated with a specific type of dental crown: the Porcelain-Fused-to-Metal (PFM) crown. Understanding the construction of a PFM crown is key to explaining the grey appearance. A PFM crown consists of a metal alloy substructure (the coping) that fits over the prepared tooth, with layers of dental porcelain fused onto the outside of this metal framework to provide a tooth-coloured, aesthetic appearance. The metal substructure is necessary to provide strength and a precise fit, particularly for back teeth or long dental bridges. The porcelain is layered over this metal to make the crown look like a natural tooth. However, one of the potential drawbacks of this design is that the underlying metal is inherently dark. While the porcelain is designed to cover this metal entirely, it needs to be opaque enough to block the dark colour from showing through, especially at the junction with the natural tooth and gum. The grey colour becomes visible primarily for two reasons. The most common reason is gum recession. Over time, the gum tissue around the tooth may recede, for instance, due to aging, aggressive brushing, or periodontal disease. When the gums recede, the very edge of the metal coping, which is typically located right at or slightly below the gum line, can become exposed. This exposed metal margin appears as a dark or grey line right at the gum margin, contrasting sharply with the natural pink of the gums and the tooth-coloured crown above it. This is a tell-tale sign of a PFM crown and can be quite noticeable, especially on front teeth. The second, less common reason, is if the layers of porcelain applied over the metal are too thin or if the opaque layer intended to block the metal colour is insufficient. In such cases, the dark shade of the metal can “show through” the porcelain, giving the entire crown a slightly grey or dull appearance, even if the gum margin is healthy. Pure porcelain crowns, often referred to as all-ceramic crowns (made entirely of ceramic material without a metal base), do not have this problem of turning grey because there is no underlying metal to show through. This is one of the primary reasons why all-ceramic and zirconia crowns have become increasingly popular, particularly for highly aesthetic areas, as they eliminate the risk of a grey margin appearing over time due to gum recession. So, if you observe a grey discolouration associated with a crown, it points strongly towards a PFM restoration where the metal base is somehow becoming visible, rather than the porcelain itself changing colour.
Which Type of Dental Crown is Best?
Navigating the various types of dental crowns available can feel like choosing from a complex menu, each with its own ingredients, preparation, and ideal serving scenario. The question of which type of dental crown is “best” is one that arises frequently, but like many things in dentistry, there’s no single, universally correct answer. The “best” crown is always the one that is most appropriate for your specific clinical needs, the location of the tooth in your mouth, your aesthetic goals, your budget, and your individual circumstances, such as habits (like teeth grinding) or allergies. Dentists consider a multitude of factors when recommending a crown material. These include the tooth’s location and function (Is it a front tooth needing aesthetics or a back molar needing strength?), the amount of remaining tooth structure, the condition of the opposing teeth, your bite forces, your aesthetic preferences, the cost, and any metal sensitivities you might have. Different materials excel in different areas. Full metal crowns (often gold alloy or base metal alloy) are exceptionally strong, highly durable, and very gentle on opposing teeth, causing minimal wear. They are often considered the “gold standard” for strength and longevity, particularly for back molars where aesthetics are less of a concern and chewing forces are highest. Their obvious drawback is their metallic appearance. Porcelain-Fused-to-Metal (PFM) crowns attempt to combine the strength of a metal substructure with the aesthetics of a porcelain outer layer. They are a traditional and reliable option, suitable for both front and back teeth and often used in bridges. However, they carry the risk of the metal margin showing at the gum line over time and the porcelain chipping. All-ceramic crowns, made entirely of ceramic or porcelain materials (like Empress, E-Max, or zirconia), offer superior aesthetics, closely mimicking the translucency and colour of natural teeth. They are an excellent choice for front teeth and are increasingly used for back teeth, especially with stronger ceramics like zirconia. Zirconia crowns, made from zirconium dioxide (a very hard ceramic), are incredibly strong and durable, making them suitable for back teeth, and newer versions offer improved aesthetics. They are often considered a strong alternative to metal or PFM for posterior teeth, and monolithic zirconia offers fracture resistance. Layered zirconia has a porcelain overlay for better looks but is more prone to chipping than monolithic. The “best” choice is a decision made collaboratively with your dentist after a thorough examination and discussion of the pros and cons of each material relative to your unique situation. It’s about selecting the material and type of crown that offers the optimal balance of strength, durability, aesthetics, and biocompatibility for the tooth requiring restoration, ensuring the best possible long-term outcome for your oral health and smile.
Which is Better Zirconia or Porcelain Crown?
The comparison between zirconia and porcelain crowns is a frequent one in modern dentistry, reflecting the advancements in ceramic materials that have provided excellent alternatives to traditional metal or PFM crowns. The question isn’t about which is universally “better,” but rather which material is “better suited” for a particular situation, as they each have distinct strengths and weaknesses. Zirconia, specifically zirconium dioxide, is an exceptionally strong and durable ceramic material. It is known for its high flexural strength and fracture resistance, making it an excellent choice for areas of the mouth that bear heavy chewing forces, such as molars. Monolithic zirconia crowns (made from a single block of zirconia) are particularly robust and are highly resistant to chipping and cracking, sometimes even surpassing the strength of PFM crowns. This makes them a preferred option in patients with strong bites or those who grind their teeth. However, traditional zirconia can be quite opaque compared to natural tooth enamel, which means while they are incredibly strong, they historically haven’t offered the same level of natural translucency as some types of porcelain. This limitation made them less ideal for front teeth where aesthetics are paramount. Recent advancements have led to the development of more translucent types of zirconia, and zirconia crowns can also be fabricated with a layered approach, using a strong zirconia base layered with aesthetic porcelain. While this layering improves aesthetics, it can reintroduce the risk of the porcelain chipping, though less likely than with PFM. Porcelain crowns, particularly all-ceramic types like E-Max (lithium disilicate), are renowned for their superior aesthetics. They can be fabricated with a high degree of translucency and can be meticulously stained and glazed to mimic the intricate details and colour variations of natural tooth enamel. This makes them the material of choice for crowns on front teeth, where achieving a natural, beautiful look is the primary goal. While some all-ceramic porcelains like E-Max are quite strong and suitable for premolars and even some molars, they may not be as inherently fracture-resistant as monolithic zirconia, especially in situations of extreme bite force or heavy grinding. So, in summary: Zirconia is generally preferred for maximum strength and durability, especially for back teeth and in patients with bruxism, while newer types are improving aesthetically. Porcelain (especially materials like E-Max) is generally preferred for superior aesthetics and translucency, making it ideal for front teeth and suitable for some back teeth where aesthetics are also a high priority and bite forces are not excessive. The “better” choice depends entirely on balancing the need for strength against the need for aesthetics for the tooth in question, a decision best made in consultation with your dentist.
Which is Cheaper Gold or Porcelain Crowns?
Comparing the cost of gold versus porcelain crowns involves looking at two materials that represent very different approaches to dental restoration – one leaning into traditional strength and biocompatibility, the other into aesthetics and evolving ceramic science. Generally speaking, the cost comparison between gold and porcelain crowns can fluctuate and is subject to the price of gold, which varies on the global market, but porcelain crowns tend to be the more expensive option upfront. Full gold crowns (made entirely of a gold alloy, although not pure gold as it would be too soft, but an alloy that includes gold, copper, and other metals for strength) have been used in dentistry for decades and are known for their exceptional durability, biocompatibility, and gentleness on opposing teeth, as they wear at a similar rate to natural enamel. Their primary drawback is, of course, their distinctive metallic colour. The cost of a gold crown is directly tied to the amount of gold alloy used and the current market price of gold. When gold prices are high, gold crowns become more expensive. However, the fabrication process for a full gold crown, while requiring skill, can sometimes be less complex or require less expensive equipment compared to some of the advanced milling or layering techniques used for modern porcelain crowns. Porcelain crowns, particularly all-ceramic types like E-Max or zirconia layered with porcelain, involve not only the cost of the sophisticated ceramic materials but also the cost associated with high-tech manufacturing processes (such as CAD/CAM milling or intricate lab layering) and the significant artistry required by the lab technician to achieve natural aesthetics. This customisation and the technology involved often make the production cost of a high-quality porcelain or ceramic crown higher than that of a gold crown, assuming standard alloy types are used. Furthermore, while gold crowns are placed relatively simply with dental cement, some porcelain crowns, especially all-ceramics, require more technique-sensitive bonding procedures, which also contribute to the overall clinical cost. So, while the price of gold is a variable factor, the complexity of fabrication, the material costs of advanced ceramics, and the aesthetic demands often push the overall cost of porcelain and ceramic crowns above that of gold crowns in many practices. However, it’s always best to get specific quotes from your dentist, as costs can vary based on the specific alloy used in the gold crown (high noble alloys are more expensive), the type of porcelain/ceramic chosen, and the overheads of the dental practice.
What is the Difference Between a Metal Cap and a Porcelain Cap?
The fundamental difference between a metal cap (crown) and a porcelain cap (crown) lies in the material composition and the resulting aesthetic and functional properties. A metal cap, or full metal crown, is fabricated entirely from a dental alloy. Traditionally, these were gold alloys, which contain a high percentage of gold along with other metals like copper, silver, and palladium to enhance strength and durability. Nowadays, other non-precious metal alloys (like nickel-chromium or cobalt-chromium) are also used. The defining characteristic of a metal crown is its metallic appearance – typically gold, silver, or grey, depending on the alloy. A porcelain cap, on the other hand, is primarily made of ceramic material designed to mimic the look of a natural tooth. This can be an all-ceramic crown (made solely of porcelain or similar ceramic like zirconia) or a Porcelain-Fused-to-Metal (PFM) crown, which has a metal core covered by porcelain. The most obvious difference is aesthetic. Metal crowns are visible as metal and are therefore typically used for back teeth (molars) where aesthetics are less critical. Porcelain crowns are tooth-coloured and can be matched precisely to your existing teeth, making them the preferred choice for front teeth and anywhere visibility is a concern. Functionally, metal crowns, particularly gold alloys, are known for their exceptional strength and durability. They are very resistant to fracture and wear down at a rate similar to natural enamel, which is gentle on opposing teeth. They can also be made relatively thin while maintaining strength, requiring less tooth structure removal during preparation compared to some porcelain types. Porcelain crowns (especially all-ceramics) can be stronger and more resistant to wear than natural enamel, which, while good for the crown, *can* potentially cause wear on the opposing natural tooth over time in patients with strong bites or grinding habits (though newer ceramics are improving in this regard). PFM crowns offer a balance of strength from the metal base and aesthetics from the porcelain, but carry the risk of the porcelain chipping and the metal margin showing. Biocompatibility is another point of difference. Metal alloys, particularly non-precious ones, can sometimes cause allergic reactions in a small percentage of patients, or in the case of PFM, the metal can potentially interact with gum tissue over long periods (though rare with noble alloys). Porcelain and ceramics are generally considered highly biocompatible and well-tolerated by surrounding tissues. In essence, the choice between a metal and a porcelain cap comes down to prioritising strength and longevity with less tooth removal (metal) versus prioritising natural appearance and biocompatibility (porcelain), with PFM offering a compromise between the two, and newer ceramics (like zirconia) bridging the gap between strength and aesthetics.
Are Porcelain Crowns Better Than Gold?
The question of whether porcelain crowns are “better” than gold crowns is a classic comparison in dentistry, and the answer, again, depends entirely on the criteria you are prioritising and the specific clinical situation. Neither is definitively superior in all aspects; they simply excel in different areas and are suitable for different needs. If your primary concern is aesthetics, particularly for teeth visible when you smile, then porcelain crowns are unquestionably “better” than gold. Their ability to be matched in colour, shape, and translucency to natural teeth provides a seamless, invisible restoration that gold, with its metallic appearance, cannot compete with. For visible teeth, porcelain is the clear winner for aesthetic appeal. However, if your primary concern is maximum durability, sheer strength, resistance to fracture, and longevity, particularly in areas of the mouth subjected to very high chewing forces (like back molars), and you are less concerned about appearance, then gold crowns are often considered “better.” Gold alloys are incredibly strong, resist chipping and fracture exceptionally well, and, importantly, they wear down at a rate very similar to natural tooth enamel. This makes them very gentle on the opposing teeth, preventing excessive wear, which can sometimes be an issue with harder ceramic materials. Gold crowns can also be fabricated with thinner walls than porcelain crowns while maintaining strength, meaning less natural tooth structure may need to be removed during preparation. Gold is also highly biocompatible and has been used safely in dentistry for a very long time. So, for a back molar where aesthetics are not a factor and durability under heavy load and kindness to opposing teeth are paramount, many dentists would still argue that a gold crown is the “better” functional choice. For a front tooth, where appearance is key, porcelain is undoubtedly the “better” choice. For teeth in between (premolars), or situations requiring a balance of aesthetics and strength, the newer ceramic materials (like E-Max or zirconia, sometimes layered with porcelain) often represent a compromise or an evolution that blends some of the best aspects of both traditional options. The “better” crown is the one that aligns best with the specific tooth’s needs, your functional requirements, your aesthetic desires, and your individual oral habits and health. It’s a choice that should be made in close consultation with your dentist, weighing the unique pros and cons of each material for your particular case.
What Type of Crown is Most Expensive?
Determining the single “most expensive” type of dental crown can be tricky, as costs fluctuate based on location, dentist fees, lab fees, and specific material brands. However, generally speaking, the crowns that often sit at the higher end of the price spectrum are typically all-ceramic crowns made from advanced materials and those requiring complex, high-precision fabrication techniques, which often include modern CAD/CAM restorations or intricately layered aesthetic crowns. All-ceramic crowns, particularly those made from materials like high-quality lithium disilicate (E-Max) or certain types of aesthetic zirconia (often layered with porcelain), tend to command higher prices than traditional options like full metal (including gold) or standard Porcelain-Fused-to-Metal (PFM) crowns. This is largely due to the cost of the advanced ceramic materials themselves, which are the result of significant research and development. Furthermore, the fabrication process for achieving the desired strength and, crucially, the high level of aesthetics with these materials often involves sophisticated technology, such as precise CAD/CAM scanning, design, and milling equipment, or highly skilled lab technicians who meticulously hand-layer and stain the porcelain for optimal naturalness. Both the investment in advanced technology by the dental practice or lab and the time and artistry of skilled technicians contribute to the higher cost. While gold crowns can be expensive when the price of gold is high, the labour and technology involved in crafting a standard gold crown might be less complex than creating a multi-layered, highly aesthetic all-ceramic restoration or utilising cutting-edge CAD/CAM systems for chairside milling. The most expensive crowns often represent the pinnacle of dental material science and aesthetic achievement, offering superior natural appearance and often excellent durability depending on the material chosen and the specific application. Custom-designed CAD/CAM crowns, especially those milled and finished in-office, can also be among the more expensive options due to the significant technological investment by the practice. Ultimately, the cost is a reflection of the materials used, the complexity of the fabrication process, the technology involved, and the skill and expertise required from both the dental lab technician and the dentist. Therefore, crowns leveraging the latest aesthetic ceramics and precision manufacturing techniques are frequently found at the top end of the cost scale.
The Process of Getting a Porcelain Crown Explained
Embarking on the journey to get a porcelain crown involves a carefully orchestrated sequence of steps, typically requiring at least two dental appointments, though modern technology like chairside CAD/CAM can sometimes condense this into a single visit. Understanding the process demystifies the procedure and helps you know what to expect. The initial step is usually a comprehensive examination by your dentist. They will assess the tooth requiring the crown, take X-rays to check the root and surrounding bone, and determine if a porcelain crown is the most suitable treatment option based on the tooth’s condition, location, and your overall oral health. This is the planning stage, where your dentist decides on the best material and approach. The first clinical appointment is primarily focused on preparing the tooth. This involves administering local anaesthesia to numb the tooth and surrounding gum tissue, ensuring you are comfortable throughout the procedure. The dentist will then carefully remove any decay, old filling material, or damaged tooth structure. The tooth is then shaped down – filed or ground – to create a foundation or “preparation” onto which the crown will fit securely. The amount of tooth structure removed depends on the type of crown being placed, but it’s enough to ensure the crown won’t feel bulky or interfere with your bite. If there isn’t enough tooth structure remaining to support a crown, the dentist may first perform a “core build-up,” using filling material to create a more substantial base. Once the tooth is prepared, the dentist takes a highly accurate impression or digital scan of the prepared tooth, the surrounding teeth, and the teeth in the opposing jaw. This impression serves as a blueprint for the dental lab (or the in-office milling machine) to create a crown that fits precisely and aligns correctly with your bite. The dentist will also work with you to select the correct shade for your porcelain crown to match your existing teeth. Before you leave this first appointment, the dentist will place a temporary crown over the prepared tooth. This temporary crown protects the vulnerable prepared tooth, prevents teeth from shifting, and allows you to eat and speak relatively normally while your permanent crown is being made. You’ll receive instructions on how to care for the temporary crown, as they are not as strong as the permanent ones. The impression or scan and shade information are then sent to a dental laboratory (or processed by in-office CAD/CAM), where skilled technicians fabricate your custom porcelain crown, a process that typically takes one to two weeks, depending on the lab and the complexity. Once the permanent crown arrives back at the dental office, you’ll schedule your second appointment for the placement.
What is the Process of Placing a Porcelain Crown?
The second appointment in the porcelain crown process is typically shorter and less involved than the first, focused entirely on fitting and permanently bonding your custom-made crown. This appointment begins with the dentist removing the temporary crown that you’ve been wearing. They will carefully clean away any remaining temporary cement from the prepared tooth. The permanent porcelain crown is then tried onto the prepared tooth. This is a crucial step where the dentist meticulously checks the fit of the crown at the margins (where the crown meets the tooth structure near the gum line). A precise fit here is paramount for the long-term health of the tooth and the success of the crown, as a poor margin can allow bacteria to leak underneath the crown, leading to decay or gum problems. The dentist will also assess the crown’s contact points with the adjacent teeth and, critically, check your bite (occlusion). You’ll be asked to bite down gently, and the dentist will use articulating paper (a thin, coloured paper) to identify any high spots on the crown that might be interfering with your natural bite or placing excessive pressure on the crown or opposing teeth. Adjustments will be made by carefully polishing down these high spots on the crown until your bite feels comfortable and balanced. If the crown requires aesthetic approval, especially on front teeth, the dentist will also evaluate the shade and appearance in different lighting conditions to ensure it blends well with your smile. This might involve holding a mirror for you to look at it and confirm you are happy with how it looks before it is permanently cemented. Once the dentist is satisfied with the fit, bite, and appearance, and you are happy with the look (if it’s in a visible area), the crown is ready for permanent bonding. The prepared tooth surface and the inside of the porcelain crown are cleaned and prepared (often etched or treated with a bonding agent) according to the specific type of bonding cement being used. A strong, durable dental cement (adhesive) is applied to the inside of the crown, and the crown is then seated firmly onto the prepared tooth. Excess cement is carefully removed from around the margins. For many modern porcelain and ceramic crowns, light-cured or dual-cured resin cements are used, and a special curing light is shined on the crown to harden the cement and create a strong bond between the tooth structure and the crown. Finally, the dentist will give the crown a final polish and check your bite again to ensure everything feels comfortable. You’ll receive post-operative instructions on how to care for your new crown, which essentially involves maintaining excellent oral hygiene, just like your natural teeth. The placement process is designed to be thorough, ensuring the crown is not just attached, but perfectly integrated into your mouth for optimal function, comfort, and longevity.
Types of All Porcelain Crowns | How Are They Made?
The term “all-porcelain crowns” broadly refers to dental crowns made entirely from ceramic materials, without a metal substructure. This category actually encompasses several distinct types of crowns, each utilising different ceramic compositions and fabrication methods to achieve varying balances of strength, aesthetics, and durability. Understanding these types provides insight into why your dentist might recommend one over another. Historically, early all-porcelain crowns were made from feldspathic porcelain, similar to the material used for veneers. While highly aesthetic and translucent, they were relatively brittle and prone to fracture, limiting their use primarily to front teeth with minimal bite force. Their fabrication involved meticulous layering of porcelain powder and liquid, which was then fired in a furnace. Significant advancements in dental ceramics have since introduced much stronger options. One prominent type is **Lithium Disilicate**, often marketed under the brand name E-Max. These crowns are significantly stronger than traditional porcelains while still offering excellent translucency and aesthetics, making them suitable for both front and back teeth (including single posterior crowns). E-Max crowns can be fabricated in two ways: using the traditional lost-wax technique where a wax pattern is pressed into a ceramic ingot and heated (pressed ceramic), or more commonly, milled from a block of lithium disilicate ceramic using CAD/CAM technology. Both methods result in a strong, homogenous restoration, which is then stained and glazed for final aesthetics. Another major category within all-ceramics, though sometimes discussed separately due to its unique properties, is **Zirconia**. Zirconia (zirconium dioxide) is an extremely strong ceramic, initially used primarily for the substructures of crowns and bridges (Porcelain-Fused-to-Zirconia) or for monolithic (single-block) crowns on back teeth where strength is paramount and aesthetics less critical due to its opacity. Newer generations of zirconia, however, offer increased translucency (“high-translucency zirconia”), making monolithic zirconia crowns a viable, very strong, and aesthetic option for a wider range of applications, including premolars and even front teeth in some cases. Zirconia crowns are primarily fabricated using CAD/CAM technology; a block of zirconia is milled into the desired crown shape based on a digital scan, and then sintered (heated to high temperature) to achieve its final strength and density, followed by staining and glazing. A hybrid approach is also **Porcelain-Veneered Zirconia**, where a zirconia coping provides strength, and aesthetic porcelain is layered on top. This aims to combine zirconia’s strength with porcelain’s superior aesthetics, though it reintroduces the risk of the porcelain chipping from the zirconia base. Thus, all-porcelain crowns are a diverse group, with materials like E-Max and various forms of Zirconia being the most common contemporary options, fabricated through pressing, layering, or predominantly, sophisticated CAD/CAM milling processes, each tailored to provide optimal outcomes based on the tooth’s specific needs and location.
Are Specific Porcelain Crown Types Better?
Yes, absolutely, specific types of porcelain or ceramic crowns are considered “better” depending entirely on the specific requirements of the tooth being restored and the patient’s individual circumstances. There’s no single “best” type for all situations, but rather optimal choices for different clinical scenarios, balancing priorities like strength, aesthetics, biocompatibility, and budget. For instance, if the tooth is a front incisor and the paramount goal is achieving the most natural, beautiful appearance possible, a highly aesthetic all-ceramic crown like **Empress Porcelain Crowns** (an older but still relevant type of pressed ceramic) or **E-Max (Lithium Disilicate)** might be considered “better” than a Porcelain-Fused-to-Metal (PFM) or monolithic zirconia crown. E-Max, in particular, offers excellent translucency and can be highly customised in shade and texture, making it superb for replicating natural enamel in the smile zone. Its strength is sufficient for many applications, including single anterior crowns and even some premolars or molars. However, if the tooth is a back molar, subjected to very heavy chewing forces, and the patient grinds their teeth, then a **monolithic Zirconia crown** might be considered “better” than E-Max or traditional porcelain due to its superior fracture toughness and strength. While monolithic zirconia used to be quite opaque, newer high-translucency versions offer significantly improved aesthetics while retaining much of their strength. This makes them increasingly suitable for premolars and even anterior crowns where strength is a significant factor (e.g., in patients with edge-to-edge bites or bruxism). **Porcelain-Fused-to-Metal (PFM)** crowns, while older technology, are still “better” in certain situations, particularly for long dental bridges where the strength of the metal substructure is crucial to span missing teeth, or in cases where significant tooth reduction is not possible. However, as discussed, they have aesthetic drawbacks like the potential for a visible grey margin and the porcelain chipping from the metal. **Porcelain-Veneered Zirconia** aims to offer a compromise, using a strong zirconia core with layered porcelain for aesthetics. It can be “better” than monolithic zirconia where high aesthetics are needed in a high-stress area, but the layered porcelain introduces a potential weakness compared to monolithic structures. Ultimately, the “better” type of porcelain or ceramic crown is determined by a detailed clinical assessment, considering the tooth’s position, the forces it will endure, the desired aesthetic outcome, the amount of remaining tooth structure, and the patient’s habits. Your dentist will recommend the specific material and type they believe offers the optimal balance of properties for the long-term success of your restoration, guided by the principle that the best dental work is that which is best suited to the individual need.
Can Porcelain Caps Get Cavities?
This is a question that requires a nuanced answer to avoid misunderstanding. The porcelain material itself, being a ceramic and not organic tooth structure, cannot get cavities. Cavities are caused by bacteria producing acid that demineralizes and breaks down tooth enamel and dentin. Porcelain is inert to these processes; bacteria and acid cannot decay the ceramic material. However, this does *not* mean that a tooth restored with a porcelain cap is immune to decay. The vulnerability lies not in the crown itself, but in the underlying natural tooth structure and, critically, at the margin where the edge of the porcelain crown meets the surface of the natural tooth or root. This margin is the interface between the restoration and the biological tooth, and it is the most common site for recurrent decay to occur on a crowned tooth. Even with a perfectly fitted crown, there is a microscopic junction line. If plaque bacteria are allowed to accumulate at this margin due to inadequate brushing and flossing, they will produce acids that attack the natural tooth structure just below the edge of the crown. Over time, this acid attack can lead to the formation of a cavity, which starts in the natural tooth tissue and can progress underneath the crown. This phenomenon is known as “recurrent decay” or “secondary decay.” If detected early, sometimes these cavities can be repaired with a filling placed at the margin, without removing the crown. However, if the decay is extensive or progresses significantly under the crown, it can compromise the fit and seal of the crown or weaken the underlying tooth structure to the point where the crown needs to be removed, the decay excavated, and a new crown fabricated and placed. Preventing cavities on a crowned tooth is therefore entirely dependent on maintaining excellent oral hygiene, focusing particular attention on cleaning thoroughly around the gum line and the margins of the crown. Daily brushing, flossing (using threader floss if needed to get under the crown’s contact point), and possibly using interdental brushes or water flossers are essential to remove plaque from this vulnerable margin. Regular dental check-ups and professional cleanings allow your dentist and hygienist to monitor the condition of your crown margins and detect any early signs of decay or gum issues. So, while the porcelain crown itself is impervious to decay, the tooth underneath remains susceptible, making diligent home care and regular professional visits absolutely vital for the long-term health of your crowned tooth and the longevity of the restoration. It’s a team effort between the durable material, the dentist’s skill, and your commitment to hygiene.
Do Porcelain Crowns Hurt?
Getting a porcelain crown and living with one should not be a painful experience, although it’s common to experience some temporary sensitivity or discomfort during and immediately after the procedure. The process of preparing the tooth for a crown involves the dentist working on the natural tooth structure, which contains nerve endings. To ensure your comfort during the preparation appointment, your dentist will use local anaesthesia to completely numb the tooth and surrounding tissues. This means you should not feel any pain while the dentist is shaping the tooth, taking impressions, or fitting the temporary crown. You might feel pressure or vibration, but not pain. After the local anaesthesia wears off following the first appointment, it’s normal to experience some temporary sensitivity in the prepared tooth, particularly to hot or cold temperatures, or tenderness in the gums around the tooth. This sensitivity is usually mild and can be managed with over-the-counter pain relievers. It typically subsides within a few days to a week as the tooth and gums recover from the procedure and adjust to the temporary crown. When you return for the second appointment to have the permanent porcelain crown placed, local anaesthesia may or may not be needed, depending on your comfort level and whether the tooth required a root canal (in which case the nerve is gone). Fitting the permanent crown should not be painful, though you might feel pressure as the dentist seats it and checks the bite. Once the permanent crown is bonded, you might experience some residual sensitivity for a short period, but this usually resolves quickly. If the crown is slightly “high” (meaning it hits before other teeth when you bite down), it can cause discomfort or even pain in the tooth or jaw joint due to uneven biting forces. This is why the dentist carefully checks your bite and makes adjustments during the placement appointment. If you feel the crown is high after you leave the office, you should contact your dentist for an adjustment. Persistent pain *under* a porcelain crown after the initial post-operative sensitivity has subsided is not normal and could indicate a problem with the underlying tooth, such as residual decay that wasn’t fully removed, a new cavity forming, infection in the nerve (necessitating root canal therapy through the crown or removal of the crown), or a fracture in the tooth root. Pain or tenderness in the gum tissue around the crown could indicate irritation from the crown margin or developing gum disease, often linked to inadequate hygiene. In summary, the procedure itself is made comfortable with anaesthesia. Temporary post-procedure sensitivity is common and normal. However, ongoing or new pain related to a crowned tooth warrants a prompt evaluation by your dentist to identify and address the underlying cause, ensuring the longevity and comfort of your restoration.
Can I Get an MRI with a Crown?
This is a very practical and important question for patients with dental crowns who may require an MRI (Magnetic Resonance Imaging) scan. The good news is that in the vast majority of cases, having a dental crown, including porcelain crowns, is perfectly safe and does not prevent you from undergoing an MRI procedure. MRI machines use powerful magnetic fields and radio waves to create detailed images of organs and tissues. The primary concern with metallic objects in or on the body during an MRI is that magnetic materials can be attracted to the magnet or cause artifacts (distortions) in the images, potentially obscuring the view of the area being scanned. The safety of a dental crown during an MRI depends on the materials it is made from. Most modern dental crowns, including all-porcelain crowns (made purely from ceramic) and all-zirconia crowns, are entirely ceramic and contain no magnetic metals. Therefore, they are completely safe in an MRI environment and will not be attracted to the magnetic field. Porcelain-Fused-to-Metal (PFM) crowns do contain a metal substructure. However, the metal alloys used in PFM crowns in dentistry are typically noble alloys (containing gold, palladium, or platinum) or base metal alloys (like nickel-chromium or cobalt-chromium). While some of these metals are ferromagnetic (attracted to magnets, like nickel), most modern dental alloys used in crowns contain minimal amounts of ferromagnetic materials or are made of non-ferromagnetic alloys. Even if a PFM crown contains some ferromagnetic material, it is usually very small and securely bonded to the tooth, posing no safety risk of being dislodged by the MRI magnet. The main potential issue with PFM crowns, or any dental metalwork like fillings or bridges, during an MRI is the possibility of creating artifacts or “signal voids” in the MRI images. These artifacts appear as distortions or dark areas on the scan and occur because the metal disrupts the magnetic field locally. If the area being scanned is close to the mouth (e.g., a scan of the brain, head, or neck), these artifacts *could* potentially obscure the view of important tissues or structures in that specific region. However, even in such cases, it doesn’t pose a safety risk to the patient. It is crucial to inform the MRI technician about *all* dental work you have, including crowns (specifying if they are porcelain, metal, or PFM if you know), fillings, bridges, implants, or dentures. This allows the technician to be aware of potential artifacts and, if necessary, adjust the scanning parameters or image interpretation. In summary, while some older PFM crowns *might* cause slight image distortion in scans of the head and neck area, they are generally safe for MRI procedures. All-ceramic and zirconia crowns pose no safety risk and do not cause significant artifacts. Always disclose your dental restorations to the MRI staff beforehand.
Frequently Asked Questions About Porcelain Caps
Navigating the world of dental restorations can bring up a host of questions, especially when considering options like porcelain caps (crowns). To make things clearer, here are some of the most commonly asked questions, providing quick yet detailed answers to help you feel more informed and confident about this popular dental treatment.
How Much Does a Porcelain Cap Cost?
Understanding the financial investment required for a porcelain dental cap is essential for planning. The cost isn’t fixed; it’s a variable figure influenced by numerous factors, generally ranging from several hundred to a few thousand pounds or dollars per tooth. In the UK, typical costs might be from £500 to £1500+, and in the US, $800 to $3000+ is a common range, but this can vary significantly based on your location, which impacts the cost of living and operating a dental practice, as urban centres tend to be more expensive than rural areas. The specific dentist’s fees, reflecting their experience and the overheads of their practice, also play a part. Crucially, the type of porcelain or ceramic material chosen impacts the cost; advanced ceramics like E-Max or certain types of zirconia can be more expensive than traditional porcelains or metal alloys used in other crown types, due to material costs and sophisticated manufacturing techniques. The fabrication process, whether through intricate lab work or high-tech chairside CAD/CAM milling, adds to the expense, requiring specialised equipment and skilled labour from either a dental technician or the dentist and their staff. The complexity of your specific case also matters; if the tooth requires preliminary treatments like a core build-up due to significant decay or breakage, or if root canal therapy is needed, these additional procedures will increase the overall expense. Finally, your dental insurance coverage is a significant determinant of your out-of-pocket cost; most plans cover a portion of medically necessary crowns, but the extent of coverage varies greatly depending on your policy, deductible, and annual maximum benefits. Getting a detailed estimate from your dentist and checking with your insurance provider beforehand is always recommended to get a clear picture of the total cost and your expected financial responsibility. While the initial cost can be substantial, it’s important to view it as a long-term investment in preserving your tooth’s health and function, potentially preventing more costly treatments like extractions and implants down the line, making it a valuable decision for maintaining your oral health and smile aesthetics for many years to come, provided proper care is maintained.
How Long Do Porcelain Crowns Last?
The lifespan of a porcelain crown is a key consideration for anyone contemplating this restoration. While they are designed for durability and longevity, there’s no single, guaranteed duration, as multiple factors influence how long they will effectively serve their purpose. On average, the expected lifespan for a well-maintained porcelain crown typically falls within the range of 5 to 15 years. However, it is entirely possible for a porcelain crown to last much longer, even 20 or 30 years, under ideal conditions and with exceptional care. The durability of a porcelain crown is significantly impacted by the underlying tooth’s health; if the natural tooth structure beneath the crown develops decay or cracks, the crown’s life will be shortened, irrespective of its own condition. Meticulous oral hygiene is paramount; diligent brushing, flossing around the crown margins, and regular professional cleanings prevent plaque buildup and recurrent decay at the tooth-crown junction, which is the most vulnerable spot. Lifestyle habits play a crucial role; avoiding biting on hard objects (ice, hard candy, pens) and managing teeth grinding or clenching (bruxism), perhaps with a nightguard, are essential to prevent chipping or fracture of the porcelain under excessive forces. The location of the crown in the mouth also influences wear and tear; back molars endure significantly higher chewing forces than front teeth, potentially affecting lifespan. Furthermore, the quality of the crown’s fabrication and the precision of its placement by the dentist are foundational to its longevity; a perfectly fitted crown with sealed margins is less prone to leakage and subsequent problems. Advances in ceramic materials, like the development of stronger porcelains and zirconia, are continually improving the potential lifespan of these restorations. Regular dental check-ups allow your dentist to monitor the crown, the underlying tooth, and the surrounding gums, identifying and addressing any issues early before they compromise the restoration. While an average is provided, the ultimate lifespan of your porcelain crown is a dynamic outcome influenced by a combination of the crown’s intrinsic quality, your oral health status, your habits, and the consistency of your preventative dental care, underscoring that active maintenance is the best predictor of extended service from your dental crown.
What is the Disadvantage of Porcelain Crowns?
While porcelain crowns are highly valued for their aesthetic appeal and effectiveness in restoring damaged teeth, they do come with certain potential disadvantages that warrant consideration. Understanding these drawbacks helps patients make informed decisions and manage expectations. Perhaps the most commonly cited disadvantage is the potential for chipping or fracture, particularly with certain types of porcelain or under excessive stress. Although modern dental ceramics are significantly stronger than older versions, concentrated forces from biting down hard on unexpected objects, trauma, or chronic teeth grinding (especially without a protective nightguard) can still cause the porcelain layer to chip or crack, potentially requiring repair or replacement of the entire crown. This is generally less likely with full metal or monolithic zirconia crowns, which are inherently more resistant to fracture. Another consideration is the amount of tooth structure that typically needs to be removed to prepare a tooth for a porcelain crown. To ensure sufficient material thickness for strength and aesthetics without the crown feeling bulky, the underlying tooth often requires more aggressive shaping compared to preparations for thinner restorations like gold crowns. This tooth reduction is irreversible. Furthermore, while porcelain itself is highly aesthetic, issues can arise depending on the type of crown and the underlying tooth or substructure. With Porcelain-Fused-to-Metal (PFM) crowns, the dark metal coping can sometimes show through as an opaque area or become visible as an unsightly grey line at the gum margin if the gums recede over time. While this isn’t an issue with all-ceramic crowns, older all-ceramics could sometimes appear less vibrant or natural than desired if not perfectly matched. Lastly, while porcelain is biocompatible, its hardness can potentially lead to increased wear on the opposing natural teeth in patients with strong bites or grinding habits, though this risk is being addressed with advancements in ceramic materials. In summary, the primary disadvantages centre around the potential for fracture under high stress compared to some stronger alternatives, the requirement for potentially more significant tooth preparation, and possible aesthetic issues related to underlying materials or gum recession in certain crown types. These factors highlight the importance of selecting the appropriate crown material for the specific clinical situation and being mindful of habits that could stress the restoration.
Do Porcelain Crowns Look Natural?
The aesthetic appeal is arguably the strongest suit of porcelain crowns, and when executed properly, they look remarkably natural, often indistinguishable from surrounding natural teeth. This capability is what makes them the preferred choice for restoring teeth that are visible within the smile line. The natural appearance is achieved through the inherent properties of dental porcelain and the meticulous process of its fabrication and placement. High-quality dental porcelain possesses a degree of translucency that mimics natural tooth enamel, allowing light to pass through the surface rather than being reflected immediately, which gives the crown a lifelike depth and prevents it from looking flat or opaque like a solid block of material. Furthermore, dental porcelain is available in a wide spectrum of shades, and skilled dental technicians can use layering and staining techniques to replicate the subtle colour variations, gradients, and characteristics found in natural teeth, ensuring the crown blends harmoniously with your existing dentition. The custom fabrication process allows the crown to be shaped and contoured precisely to match the anatomy of a natural tooth, including surface texture and ridges, further enhancing its realistic appearance. Achieving this high level of naturalness is dependent not only on the material but also on the skill and artistry of both the dental lab technician who crafts the crown and your dentist who prepares the tooth, takes accurate impressions, selects the shade, and meticulously fits and bonds the crown, ensuring the margins are seamless and the bite is correct. While older porcelain materials or less precise techniques could sometimes result in crowns that appeared less natural (e.g., too opaque or the wrong shade), modern advanced ceramics like E-Max and high-translucency zirconia, combined with sophisticated CAD/CAM technology and skilled lab work, make it possible to create restorations that are astonishingly lifelike. For patients seeking to restore both the function and the natural beauty of a damaged tooth, the ability of porcelain crowns to integrate seamlessly into the smile is a significant advantage, providing confidence and a natural aesthetic outcome that is a hallmark of high-quality cosmetic dentistry.
Can Porcelain Caps Get Cavities?
This is a crucial point of clarification often needed by patients. The simple answer is no, the porcelain material itself cannot get cavities. Dental cavities are caused by the action of acids produced by bacteria breaking down the organic and mineral components of natural tooth structure (enamel and dentin). Porcelain is a non-organic ceramic material; it is inert and cannot be demineralized or decayed by bacterial acids. However, this does *not* mean that the tooth covered by a porcelain cap is immune to decay. The vulnerability lies at the margin, the junction where the edge of the porcelain crown meets the remaining natural tooth structure. This interface, even when the crown is perfectly fitted, is a potential trap for plaque bacteria if not kept meticulously clean. If plaque is allowed to accumulate along this margin, the bacteria within the plaque will produce acids that attack the natural tooth structure directly underneath and adjacent to the crown’s edge. This process can lead to the formation of a new cavity in the natural tooth, developing right at or just below the crown margin. This is known as recurrent or secondary decay, and it is the most common reason for failure or the need to replace an otherwise healthy dental crown. If recurrent decay is detected early, it might be possible to remove the decay and place a filling at the margin without removing the crown. However, if the decay is extensive and undermines the tooth structure beneath the crown or compromises the seal of the crown, the crown will likely need to be removed so the decay can be fully accessed and treated, followed by the fabrication and placement of a new crown. Therefore, preventing cavities on a tooth with a porcelain crown is entirely dependent on maintaining excellent oral hygiene focused on keeping the crown margins clean. This involves diligent brushing, flossing (using appropriate techniques like floss threaders if needed), and using interdental brushes as recommended by your dental professional to remove plaque and food debris from around the entire circumference of the crowned tooth, particularly at the gum line. Regular dental check-ups are also essential, allowing your dentist to visually inspect the crown margins and take X-rays to check for signs of decay developing underneath the crown or at the root. So, remember, while the porcelain is safe, the tooth beneath and around it still requires rigorous cleaning and professional monitoring to prevent decay and ensure the long-term success of your porcelain cap.
Do Porcelain Crowns Hurt?
Getting a porcelain crown and living with one should not be a painful experience, although it’s common to experience some temporary sensitivity or discomfort during and immediately after the procedure. The process of preparing the tooth for a crown involves the dentist working on the natural tooth structure, which contains nerve endings. To ensure your comfort during the preparation appointment, your dentist will use local anaesthesia to completely numb the tooth and surrounding tissues. This means you should not feel any pain while the dentist is shaping the tooth, taking impressions, or fitting the temporary crown. You might feel pressure or vibration, but not pain. After the local anaesthesia wears off following the first appointment, it’s normal to experience some temporary sensitivity in the prepared tooth, particularly to hot or cold temperatures, or tenderness in the gums around the tooth. This sensitivity is usually mild and can be managed with over-the-counter pain relievers. It typically subsides within a few days to a week as the tooth and gums recover from the procedure and adjust to the temporary crown. When you return for the second appointment to have the permanent porcelain crown placed, local anaesthesia may or may not be needed, depending on your comfort level and whether the tooth required a root canal (in which case the nerve is gone). Fitting the permanent crown should not be painful, though you might feel pressure as the dentist seats it and checks the bite. Once the permanent crown is bonded, you might experience some residual sensitivity for a short period, but this usually resolves quickly. If the crown is slightly “high” (meaning it hits before other teeth when you bite down), it can cause discomfort or even pain in the tooth or jaw joint due to uneven biting forces. This is why the dentist carefully checks your bite and makes adjustments during the placement appointment. If you feel the crown is high after you leave the office, you should contact your dentist for an adjustment. Persistent pain *under* a porcelain crown after the initial post-operative sensitivity has subsided is not normal and could indicate a problem with the underlying tooth, such as residual decay that wasn’t fully removed, a new cavity forming, infection in the nerve (necessitating root canal therapy through the crown or removal of the crown), or a fracture in the tooth root. Pain or tenderness in the gum tissue around the crown could indicate irritation from the crown margin or developing gum disease, often linked to inadequate hygiene. In summary, the procedure itself is made comfortable with anaesthesia. Temporary post-procedure sensitivity is common and normal. However, ongoing or new pain related to a crowned tooth warrants a prompt evaluation by your dentist to identify and address the underlying cause, ensuring the longevity and comfort of your restoration.
Can I Get an MRI with a Crown?
This is a very practical and important question for patients with dental crowns who may require an MRI (Magnetic Resonance Imaging) scan. The good news is that in the vast majority of cases, having a dental crown, including porcelain crowns, is perfectly safe and does not prevent you from undergoing an MRI procedure. MRI machines use powerful magnetic fields and radio waves to create detailed images of organs and tissues. The primary concern with metallic objects in or on the body during an MRI is that magnetic materials can be attracted to the magnet or cause artifacts (distortions) in the images, potentially obscuring the view of the area being scanned. The safety of a dental crown during an MRI depends on the materials it is made from. Most modern dental crowns, including all-porcelain crowns (made purely from ceramic) and all-zirconia crowns, are entirely ceramic and contain no magnetic metals. Therefore, they are completely safe in an MRI environment and will not be attracted to the magnetic field. Porcelain-Fused-to-Metal (PFM) crowns do contain a metal substructure. However, the metal alloys used in PFM crowns in dentistry are typically noble alloys (containing gold, palladium, or platinum) or base metal alloys (like nickel-chromium or cobalt-chromium). While some of these metals are ferromagnetic (attracted to magnets, like nickel), most modern dental alloys used in crowns contain minimal amounts of ferromagnetic materials or are made of non-ferromagnetic alloys. Even if a PFM crown contains some ferromagnetic material, it is usually very small and securely bonded to the tooth, posing no safety risk of being dislodged by the MRI magnet. The main potential issue with PFM crowns, or any dental metalwork like fillings or bridges, during an MRI is the possibility of creating artifacts or “signal voids” in the MRI images. These artifacts appear as distortions or dark areas on the scan and occur because the metal disrupts the magnetic field locally. If the area being scanned is close to the mouth (e.g., a scan of the brain, head, or neck), these artifacts *could* potentially obscure the view of important tissues or structures in that specific region. However, even in such cases, it doesn’t pose a safety risk to the patient. It is crucial to inform the MRI technician about *all* dental work you have, including crowns (specifying if they are porcelain, metal, or PFM if you know), fillings, bridges, implants, or dentures. This allows the technician to be aware of potential artifacts and, if necessary, adjust the scanning parameters or image interpretation. In summary, while some older PFM crowns *might* cause slight image distortion in scans of the head and neck area, they are generally safe for MRI procedures. All-ceramic and zirconia crowns pose no safety risk and do not cause significant artifacts. Always disclose your dental restorations to the MRI staff beforehand.