Key Takeaways
-
- Full mouth dental implants offer a comprehensive, long-term solution for extensive tooth loss, significantly improving chewing, aesthetics, and confidence.
-
- The procedure involves surgically placing titanium posts into the jawbone, which fuse with the bone (osseointegration) to support a full arch of prosthetic teeth.
-
- Costs in the UK for full mouth implants can range widely, typically from £15,000 to £30,000+ per arch, with various financing options available.
-
- “Same Day” or “Teeth in a Day” options allow for the placement of implants and a temporary prosthesis in a single appointment, with the final prosthesis fitted after full healing.
-
- Key benefits over traditional dentures include superior stability, prevention of jawbone loss, enhanced comfort, improved speech, and a wider dietary range.
-
- Longevity of the implant posts can be lifelong with proper care, though the prosthetic teeth (the bridge or denture) may need refurbishment or replacement after 10-20+ years.
-
- NHS availability for full mouth dental implants is extremely limited; treatment is predominantly accessed privately.
- Choosing a GDC-registered dentist with specific, demonstrable experience in full arch implantology is crucial for a successful outcome.
What Exactly Are Full Mouth Dental Implants and How Do They Function?
Full mouth dental implants are a sophisticated and comprehensive dental solution designed to replace all or most missing teeth in either one or both jaws, functioning by anchoring a full-arch prosthesis to surgically embedded titanium posts that integrate directly with your jawbone, effectively becoming artificial tooth roots. Think of them not just as replacements, but as a bionic upgrade for your entire dental landscape. These aren’t your grandmother’s dentures, slipping and sliding at inopportune moments. We’re talking about a marvel of bioengineering where tiny, biocompatible titanium screws are meticulously placed into the jaw. Over time, a fascinating process called osseointegration occurs – the bone literally fuses with these implants, creating an unshakeable foundation. Upon this solid footing, abutments (connector pieces) are attached, which then serve as the docking station for your brand-new, full-arch prosthesis – be it a high-tech bridge or a state-of-the-art denture designed to look, feel, and chew like the real deal. The aim here isn’t just to fill gaps; it’s to provide a stable, enduring, and aesthetically pleasing replacement that mimics the function and form of natural teeth, allowing you to bite, chew, speak, and smile with a confidence you might have thought was lost forever. It’s a total system reboot for your oral architecture.
How Do Full Arch Dental Implants Differ from Single Implants?
Full arch dental implants differ from single implants primarily in their scope and support structure; instead of replacing individual teeth with a one-to-one implant-to-crown ratio, full arch solutions utilize several strategically positioned implants – often as few as four or six per jaw – to support an entire arch of new teeth, making it a more efficient and often less invasive approach for complete tooth loss. While a single dental implant is a masterpiece of engineering designed to replace one missing tooth (one implant post supporting one artificial crown), a full arch system is an orchestra. It’s about leveraging the strength of multiple implants working in concert. The fundamental principle of osseointegration – that miraculous fusion of titanium to bone – remains identical. The implants still become a part of you. However, in a full mouth scenario, these implants are the pillars supporting a much larger, unified structure, like a bridge spanning an entire jawline. This strategic placement means fewer surgical sites compared to replacing every single tooth with its own implant, which can translate to reduced overall treatment time, potentially lower costs, and a less taxing recovery. It’s a sophisticated blend of biomechanics and artistry, ensuring that the forces of your bite are distributed evenly across the supporting implants, providing robust, long-lasting function for an entire set of teeth, not just one.
Are There Other Names for Complete Sets of Dental Implants?
Yes, complete sets of dental implants are frequently known by several other names within dental practices and among patients, including “whole mouth dental implants,” “complete dental implants,” “full jaw implants,” and “full set of teeth implants,” all essentially referring to the same comprehensive restorative concept of replacing an entire arch of teeth using implant technology. While the core idea is consistent, these varying terms often highlight different facets or simply reflect regional or practitioner preferences in nomenclature. “Whole mouth dental implants” and “complete dental implants” are perhaps the most straightforward, emphasizing the totality of the restoration. “Full jaw implants” specifically points to the anatomical area being treated, whether it’s the maxilla (upper jaw) or mandible (lower jaw), or both. “Full set of teeth implants” focuses on the outcome – a complete new dentition. You might also encounter terms like “All-on-4®” or “All-on-6,” which are trademarked treatment concepts referring to specific protocols where a full arch of teeth is supported on four or six implants, respectively. Occasionally, “immediate prosthetic rehabilitation” might be used, particularly in contexts discussing rapid or same-day loading protocols where a temporary or even final prosthesis is fitted very soon after implant placement, though this describes more the timing and process rather than being a direct synonym for the implant set itself. Understanding these synonyms helps demystify conversations with dental professionals and navigate the wealth of information available.
What Is Meant by a “Full Set of Denture Implants”?
A “full set of denture implants,” more accurately termed implant-supported or implant-retained dentures, typically refers to a full-arch prosthesis, which visually resembles a traditional denture in its gum-colored acrylic base and artificial teeth, but is securely anchored to multiple dental implants rather than resting loosely on the gums, thereby offering significantly enhanced stability, function, and comfort. This is a crucial distinction. Traditional dentures rely on suction and the contours of your gums for stability, which can lead to issues like slippage, sore spots, and a reduced ability to chew effectively. Implant-supported dentures, however, clip or screw onto specially designed abutments attached to the implants embedded in your jawbone. This connection provides a remarkable improvement in retention – they don’t rock, they don’t float, and they certainly don’t require messy adhesives. While they are often removable by the patient for cleaning (implant-retained overdentures), some designs are fixed and can only be removed by a dentist (implant-supported fixed bridges, which might still be colloquially referred to as a type of “denture implant” by laypersons). The key takeaway is that the “implant” part signifies a foundational upgrade, transforming the denture experience from something potentially precarious to something reliably stable, allowing for a wider diet and greater confidence in social situations.
Is It Worth Getting Full Dental Implants and Who Can Benefit Most?
Deciding if full dental implants are worth the investment involves weighing their profound, long-term benefits in restoring oral function, aesthetics, and overall quality of life against the initial cost and treatment duration, with individuals suffering from extensive tooth loss, those deeply dissatisfied with conventional dentures, or those facing severe dental issues that compromise their entire dentition typically benefiting most profoundly. It’s not merely a financial calculation; it’s an investment in your daily existence. Imagine biting into an apple with gusto, speaking without fear of your teeth shifting, smiling openly in photographs – these are the qualitative returns that often tip the scales. For those who have struggled with loose, uncomfortable dentures, the transition to implant-supported teeth can feel nothing short of revolutionary. Similarly, individuals whose remaining natural teeth are failing due to widespread decay, advanced gum disease, or irreparable damage find in full mouth implants a chance to start anew, with a solution designed for longevity and stability. The “worth” is also found in the preservation of jawbone, as implants stimulate the bone like natural tooth roots, preventing the facial collapse often seen with long-term tooth loss or traditional denture wear. While the journey requires commitment, the destination—a fully functional, aesthetically pleasing, and confidently worn smile—is, for many, an invaluable outcome that far outweighs the initial outlay.
What Are the Key Benefits of Choosing Full Mouth Implants Over Traditional Dentures?
The key benefits of choosing full mouth implants over traditional dentures are numerous and transformative, primarily centering on superior stability that eliminates slippage, dramatically improved chewing efficiency allowing for a broader and more nutritious diet, the crucial preservation of jawbone integrity thereby maintaining facial structure, and significantly enhanced comfort and speech clarity. Let’s unpack these game-changers. Firstly, stability: implants are anchored in your bone, meaning your new teeth won’t budge, click, or embarrassingly dislodge while you’re eating, talking, or laughing – a stark contrast to the often-unpredictable nature of conventional dentures. This leads directly to improved chewing power; you can tackle tougher, crunchier, and more fibrous foods that denture-wearers often avoid, leading to better nutrition and greater enjoyment of meals. Critically, dental implants stimulate the jawbone much like natural tooth roots, halting the bone resorption (shrinkage) that inevitably occurs with tooth loss and traditional denture wear. This bone preservation helps maintain your facial contours, preventing that sunken-in look. Comfort is another huge plus – no more sore spots from dentures rubbing on gums, and no need for messy adhesives. Speech often improves too, as you can articulate more clearly without worrying about teeth moving. And let’s not forget the psychological uplift: the confidence that comes from a secure, natural-looking smile is, for many, priceless.
Who Is Typically Suitable for Full Mouth Dental Implant Treatment?
Individuals typically suitable for full mouth dental implant treatment are those experiencing significant tooth loss across one or both arches – whether they are already edentulous (toothless) or have numerous failing teeth – who possess good general health to comfortably undergo surgical procedures, and critically, have adequate jawbone density and volume to support the implants, or are candidates for bone grafting procedures to create sufficient bone. Good general health is key; conditions like uncontrolled diabetes or certain immune deficiencies might need careful management or could preclude treatment. Being a non-smoker, or willing to quit, is highly advantageous as smoking significantly impairs healing and increases implant failure rates. The state of your jawbone is paramount. Your dentist will use advanced imaging, like Cone Beam Computed Tomography (CBCT), to assess bone quantity and quality. If there’s insufficient bone due to long-term tooth loss, procedures like sinus lifts (for the upper jaw) or ridge augmentation (bone grafting) can often rebuild the necessary foundation, expanding candidacy. Furthermore, a commitment to excellent oral hygiene post-treatment and regular dental check-ups is non-negotiable for long-term success. Finally, realistic expectations about the treatment process, timeline, and outcomes are important; this is a journey, not an instant fix, but one with remarkable rewards.
Why Do People Opt for Complete Mouth Dental Implants?
People opt for complete mouth dental implants primarily due to a profound desire for a permanent, highly functional, and aesthetically superior solution to widespread tooth loss, often driven by acute dissatisfaction with the numerous limitations and daily hassles of conventional dentures, a longing to reclaim a natural-looking and confident smile, and the overarching pursuit of an enhanced overall quality of life. The motivations are multifaceted. Many are simply fed up with the instability of traditional dentures – the slipping, the clicking, the dietary restrictions, the need for adhesives, the embarrassing moments. They crave the freedom to eat what they love and speak without anxiety. Others are focused on aesthetics; they want teeth that don’t just fill space but look and feel indistinguishable from a healthy, natural set, restoring not just a smile but also youthful facial contours often lost with bone resorption. The permanence aspect is a huge draw; unlike dentures that need frequent adjustments and replacements, implants are designed to be a long-term, even lifelong, solution when properly cared for. There’s also the significant psychological impact: restoring a full set of functional teeth can dramatically boost self-esteem, social confidence, and emotional well-being, allowing individuals to engage more fully and joyfully in life. It’s about moving beyond mere replacement to true oral rehabilitation.
Can Full Mouth Dental Implants Improve My Smile and Facial Structure?
Yes, full mouth dental implants can dramatically improve your smile by providing beautifully crafted, natural-looking replacement teeth tailored to your facial aesthetics, and they significantly enhance your facial structure by actively preventing the insidious bone loss that typically accompanies missing teeth, thereby restoring youthful facial contours, lip support, and overall facial harmony. When teeth are lost, the underlying jawbone, no longer stimulated by tooth roots, begins to recede or shrink – a process called resorption. This bone loss can lead to a sunken appearance in the lower face, thinner lips, and an increase in wrinkles around the mouth, prematurely aging one’s appearance. Full mouth dental implants, by integrating with the jawbone, provide the necessary stimulation to help maintain bone density and volume, effectively halting or slowing this process. This preserves the natural scaffolding of your face. Aesthetically, the prosthetic teeth are custom-designed by skilled technicians in collaboration with your dentist, considering factors like tooth shape, size, color, and alignment to create a smile that is not only beautiful but also uniquely yours and in proportion with your facial features. The result is often a rejuvenation that extends beyond just the teeth, lending a more vibrant and supported look to the entire lower face.
Are Full Mouth Dental Implants Noticeable to Others?
When expertly designed, meticulously crafted, and skillfully placed by an experienced dental team, full mouth dental implants are generally not noticeable to others as artificial; instead, they are intended to look, feel, and function just like a set of healthy, vibrant, natural teeth, blending seamlessly and harmoniously with your overall facial aesthetics. The goal of modern implant dentistry isn’t just to replace teeth, but to replicate nature as closely as possible. This involves several key factors. The materials used for the prosthetic teeth, such as advanced dental porcelains or zirconia, possess a translucency and light-reflecting quality that closely mimics natural tooth enamel. The shade, shape, and size of each tooth are carefully customized to complement your skin tone, facial features, and even your personality. Furthermore, considerable attention is paid to the emergence profile – how the teeth appear to emerge from the gum line – to create a truly lifelike appearance. Unlike some older forms of dentures that could look bulky or artificial, today’s full arch implant restorations are works of art, sculpted by dental technicians who are, in essence, ceramic artists. The only thing others are likely to notice is your confident, beautiful smile and perhaps a renewed spring in your step.
What Does the Full Mouth Dental Implant Procedure Involve from Start to Finish?
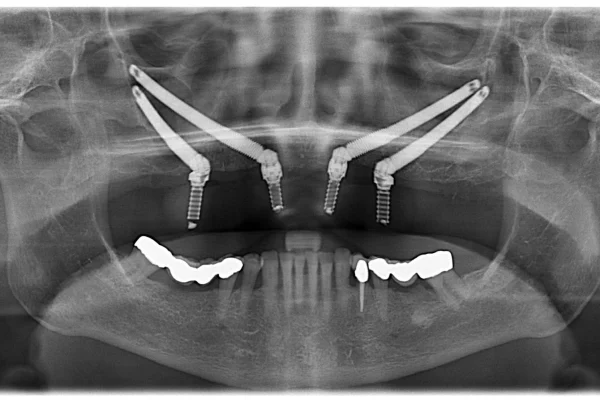
The full mouth dental implant procedure is a meticulously planned, multi-stage journey that typically involves an initial comprehensive consultation and diagnostic planning phase, followed by the surgical placement of the titanium implants into the jawbone, a crucial healing period allowing for osseointegration (the fusion of implant to bone), and finally, the intricate process of designing, fabricating, and attaching the custom-made full-arch prosthetic teeth. This isn’t a quick fix; it’s a carefully orchestrated process tailored to your unique anatomy and goals. The journey begins with a deep dive into your dental and medical history, advanced imaging like 3D CBCT scans to assess bone structure, and detailed discussions about your desired outcomes. From there, a precise treatment plan is mapped out, almost like an architectural blueprint for your new smile. The surgical phase, while significant, is performed with utmost precision, often utilizing guided surgery techniques. The subsequent healing phase is biologically critical – this is when the magic of osseointegration happens, typically taking three to six months. During this time, you may have a temporary prosthesis. Once your implants are rock-solid, the restorative phase begins: taking highly accurate impressions, crafting your final bespoke teeth in a dental laboratory, and then fitting them perfectly to the implants. It’s a collaboration between you, your dentist, the surgeon (if different), and the lab technician, all working towards a singular, transformative result.
How Does One Prepare for Full Mouth Dental Implant Surgery?
Preparation for full mouth dental implant surgery is a meticulous and vital process that begins with an in-depth consultation and includes detailed diagnostic imaging such as X-rays and advanced 3D Cone Beam Computed Tomography (CBCT) scans, comprehensive and individualized treatment planning, thorough health assessments to ensure you’re fit for surgery, and the completion of any necessary preliminary dental treatments, such as addressing gum disease, extracting failing teeth, or performing bone grafting procedures. During your initial consultation, your dentist will discuss your goals, explain the procedure in detail, answer all your questions, and outline potential costs. The CBCT scan provides a three-dimensional view of your jawbone, allowing for precise planning of implant placement and assessment of bone density. Your medical history will be carefully reviewed; certain conditions or medications might require adjustments to the treatment plan or consultation with your GP. If active gum disease is present, it must be treated first. Any teeth deemed unsalvageable will be scheduled for extraction, which can sometimes occur at the same time as implant placement. If bone volume is insufficient, bone grafting or a sinus lift may be performed as a preparatory step, requiring its own healing period. Pre-operative instructions might include guidance on diet, medications to take or avoid (like blood thinners, in consultation with your doctor), arranging for post-surgery transport and care, and possibly starting a course of antibiotics.
How Are Full Jaw Implants Actually Placed During the Surgical Phase?
During the surgical phase, full jaw implants are meticulously and precisely placed directly into the jawbone by a skilled oral surgeon or an implant-focused dentist, a procedure typically performed under effective local anaesthesia with various sedation options available (such as oral sedatives, IV “twilight” sedation, or even general anaesthesia) to ensure profound patient comfort and anxiety control, involving the careful creation of small access points in the gum, precise drilling of osteotomy sites (sockets) into the bone, and the gentle insertion of the sterile titanium implant posts according to the pre-determined, often digitally guided, treatment plan. The process begins with ensuring you are completely numb and comfortable. The surgeon then makes small incisions in your gum tissue to expose the underlying bone at the planned implant locations. Using a series of progressively wider, specialized drills, they create precise channels in the jawbone, carefully controlling the depth and angulation to match the dimensions of the implants and avoid any vital structures like nerves or sinuses. The implants are then gently threaded or tapped into these prepared sites. In some cases, a healing abutment or a temporary prosthetic component may be attached immediately. Finally, the gums are repositioned and closed with fine sutures, which may be dissolvable or require removal a week or two later. The entire surgical event is conducted in a sterile environment, often with the aid of surgical guides created from digital scans for enhanced accuracy.
How Many Dental Implants Are Typically Needed for a Whole Mouth Restoration?
The number of dental implants typically needed for a whole mouth restoration, meaning a full arch of teeth in either the upper or lower jaw, can vary depending on the specific treatment protocol chosen (such as All-on-4®, All-on-6, or All-on-8 concepts), individual patient factors like bone quality and quantity, and the type of final prosthesis planned, but common configurations often involve placing between four and eight implants per arch, strategically positioned to provide robust, balanced, and long-lasting support for the full-arch set of replacement teeth. For instance, the All-on-4® treatment concept, as the name suggests, utilizes just four implants per jaw – two placed vertically in the front and two tilted in the back – to support a full arch prosthesis. This approach is often favored as it can sometimes avoid the need for extensive bone grafting in the posterior regions. All-on-6 or All-on-8 protocols employ six or eight implants respectively, distributing the biting forces over a greater number of foundations, which some clinicians believe offers enhanced stability and longevity, particularly in cases with softer bone or for patients with stronger bites. The decision on the optimal number of implants is a critical part of the treatment planning phase, made by your dental surgeon based on a thorough assessment of your anatomical structures, the desired prosthetic outcome, and biomechanical principles to ensure the restoration can withstand the daily forces of chewing effectively and durably.
How Long After Full Mouth Extractions Can Implants Be Placed?
The timing for placing dental implants after full mouth extractions can vary significantly, with options ranging from immediate placement on the very same day as the extractions, known as “immediate implant placement,” to a delayed placement protocol which might occur several weeks or even months later to allow for initial healing or following bone grafting procedures; this decision is highly individualized and influenced by critical factors such as the presence or absence of infection at the extraction sites, the quality and quantity of available bone post-extraction, and the overall comprehensive treatment plan. Immediate placement is often ideal if conditions are favorable – no acute infection, sufficient bone for initial implant stability – as it can reduce the total number of surgical procedures and shorten the overall treatment timeline. In such cases, a temporary prosthesis might also be fitted on the same day. However, if there’s significant infection, compromised bone, or if extensive bone grafting is required at the time of extraction, a delayed approach is usually preferred. This might involve waiting 6-8 weeks for soft tissue healing (early placement) or 3-6 months for more substantial bone healing and maturation of any graft material (delayed placement). Your surgeon will carefully evaluate your specific situation through clinical examination and imaging to determine the most predictable and successful timing for your implant placement.
What Can I Expect from a Full Mouth Dental Implant Treatment in Terms of Timeline?
You can generally expect the timeline for a full mouth dental implant treatment to span several months, typically ranging from three to nine months, and sometimes longer, from the initial surgical placement of implants to the final fitting of your permanent restoration; this duration encompasses the surgical phase itself, a crucial healing period of approximately three to six months for osseointegration where the implants securely fuse with the jawbone, and the subsequent stages involved in meticulously crafting and fitting your permanent prosthetic teeth. Several factors can influence this timeline. If preliminary procedures like bone grafting or sinus lifts are necessary, this will add several months of healing time before implant surgery can even begin. The osseointegration period is fairly standard but can vary slightly based on individual healing capacity and bone quality. If a “Teeth in a Day” or immediate loading protocol is used, you’ll receive a temporary fixed prosthesis on the day of surgery, but the final, more durable prosthesis is still fabricated and fitted after full healing. The restorative phase, once osseointegration is confirmed, involves taking precise impressions, several try-in appointments to ensure perfect fit, function, and aesthetics of the final teeth, and the laboratory fabrication time. While it demands patience, this carefully managed timeline is essential for achieving a predictable, stable, and long-lasting outcome.
Can Full Mouth Dental Implants Be Done in One Day with “Same Day” Procedures?
Yes, it is indeed possible for certain full mouth dental implant procedures to be effectively completed in a “same day” or “Teeth in a Day” fashion, which typically means that the surgical placement of the dental implants and the attachment of a functional, aesthetically pleasing, albeit often temporary, full-arch prosthesis all occur within a single, extended appointment; however, it’s crucial to understand that while you leave with teeth, the underlying implants still require several months to fully integrate with the jawbone before the final, more robust permanent prosthesis is subsequently designed and fitted. These immediate loading protocols are a significant advancement, offering patients the immediate psychological and functional benefit of not having to go without teeth or wear a removable temporary denture during the healing phase. The temporary prosthesis fitted on the day of surgery is carefully designed to be comfortable and look good, but it’s usually made from a lighter material and may not have the same long-term durability as the final version. This allows the implants to heal with minimal stress. Patient selection is key for same-day teeth; good bone quality and quantity are generally required to achieve sufficient initial implant stability for immediate loading. After the standard osseointegration period of three to six months, you’ll return for the fabrication and fitting of your permanent, highly durable, and precisely customized final set of teeth.
What Happens After Full Mouth Dental Implant Surgery During the Healing Phase?
After full mouth dental implant surgery, the healing phase involves an initial recovery period, typically lasting one to two weeks, characterized by manageable swelling, bruising, and discomfort which are well-controlled with prescribed pain medication and cold compresses, followed by a longer, more passive period of osseointegration where the implants biologically fuse with the jawbone over three to six months; during this entire time, you’ll receive specific post-operative care instructions and attend several follow-up appointments to meticulously monitor your progress and ensure optimal healing. In the immediate aftermath of surgery, rest is paramount. You’ll likely experience some swelling, which often peaks around day three, and bruising. A soft diet will be necessary to avoid putting undue pressure on the healing implants. Your surgeon will provide detailed instructions on oral hygiene, which might involve gentle rinsing with an antimicrobial mouthwash rather than vigorous brushing around surgical sites initially. Pain medication will be prescribed to keep you comfortable. Follow-up appointments are scheduled to check healing, remove sutures if necessary, and ensure there are no signs of infection or complications. The osseointegration phase is largely silent – you won’t feel it happening, but it’s the most critical part of the implant journey. If you’ve received immediate temporary teeth, you’ll need to be mindful of your diet to protect them. If not, you might wear a temporary removable denture or go without teeth in that arch, depending on your specific plan.
What Are the Different Options, Types, and Materials for Full Mouth Dental Implants?
Full mouth dental implants encompass a fascinating range of options, types, and advanced materials rather than representing a single, monolithic, one-size-fits-all treatment; these variations include different implant support systems like the well-known All-on-4® or more extensive All-on-6/8 configurations, and a diverse palette of sophisticated prosthetic materials for the final teeth such as durable acrylics, aesthetic composite resins, classic porcelain-fused-to-metal (PFM), or the increasingly popular high-strength, highly aesthetic monolithic zirconia, underscoring the crucial reality that not all full mouth solutions are created equal and highlighting the profound importance for patients to understand these nuanced choices to make informed decisions. The journey to a new smile is highly personalized. The number of implants, their specific placement, the design of the prosthesis (fixed bridge vs. removable overdenture), and the materials used are all tailored to your unique anatomical needs, aesthetic desires, functional requirements, and budget. Understanding that “full mouth implants” is a category, not a singular product, empowers you to engage in more meaningful discussions with your dental provider, ensuring the solution you choose aligns perfectly with your expectations for longevity, appearance, and feel. It’s about finding the perfect alchemy of engineering and artistry for your mouth.
What Are the Common Types of Full Mouth Implant Solutions (e.g., All-on-4/6/8)?
Common types of full mouth implant solutions include established and often trademarked protocols like All-on-4®, which ingeniously utilizes four strategically angled implants (two in the front, two tilted in the back) to support a full arch of teeth, thereby often avoiding the need for bone grafting in the posterior jaw, and variations such as All-on-6 or All-on-8, which employ a greater number of implants – six or eight respectively – for potentially increased support, enhanced load distribution across the jaw, and sometimes as a preference for patients with softer bone or those desiring maximum perceived stability, alongside other customized full arch fixed or removable restorations tailored to individual patient anatomy and specific clinical needs. The All-on-X systems are popular because they offer a fixed, full-arch solution efficiently. Implant-supported overdentures are another common type; these involve a smaller number of implants (often 2-4 in the lower jaw, 4+ in the upper) that have attachments (like locators or a bar) onto which a modified full denture “snaps” or clips, providing much better retention than traditional dentures, though they are still removable by the patient for cleaning. Fully fixed, screw-retained bridges, whether on 4, 6, 8, or even more implants, are designed to be as close to natural teeth as possible and are only removed by the dentist for maintenance. The choice depends on bone availability, financial considerations, patient preference for fixed versus removable, and the clinician’s expert recommendation.
What Materials Are Commonly Used for the Final Prosthetic Teeth in Full Mouth Cases?
The final prosthetic teeth in full mouth implant cases are commonly crafted from a variety of advanced and highly specialized dental materials, including durable, high-impact acrylic resins often reinforced with a metal framework, aesthetic and wear-resistant composite resins, classic porcelain-fused-to-metal (PFM) which combines a metal substructure for strength with a porcelain overlay for appearance, and increasingly, high-strength, exceptionally aesthetic, and biocompatible monolithic zirconia, each offering a different sophisticated balance of durability, natural appearance, tactile feel, reparability, and overall cost. Acrylic prostheses are often the most cost-effective initial option, offering good aesthetics and being relatively easy to repair or adjust, though they can wear down more quickly than other materials. Modern composite resins offer improved wear resistance and aesthetics compared to basic acrylics and can also be repaired chairside. PFM has a long track record, providing excellent strength from the metal core and good aesthetics from the porcelain, though there’s a small risk of porcelain chipping and the metal may sometimes show as a grey line at the gum if recession occurs. Monolithic zirconia, often milled from a solid block using CAD/CAM technology, is a premium choice, renowned for its exceptional strength (highly resistant to chipping and breaking), outstanding natural-looking aesthetics (it can be layered or stained to mimic enamel beautifully), and excellent biocompatibility. The choice of material will impact the longevity, look, and feel of your new smile, and your dentist will discuss the pros and cons of each in relation to your specific case.
Do All Dental Implants for the Whole Mouth Involve the Same Treatment Protocol?
No, emphatically, not all dental implants for the whole mouth involve the exact same, standardized treatment protocol; rather, each case is meticulously and highly customized based on a multitude of intricate factors including the patient’s unique oral anatomy (jaw shape, bone density, nerve pathways), the existing volume and quality of their jawbone, their specific aesthetic desires and functional goals for their new smile, their overall systemic health and any contributing medical conditions, the particular implant system and prosthetic materials chosen by the dentist and patient, and the clinician’s preferred surgical and restorative techniques. For example, a patient with significant bone loss in the upper jaw might require a sinus lift procedure and a greater number of implants compared to a patient with ample bone who might be a candidate for a graftless All-on-4® approach. The decision to provide an immediate temporary prosthesis versus a delayed approach also varies. The type of final restoration—whether it’s a zirconia bridge, an acrylic hybrid, or an implant-retained overdenture—dictates different restorative steps and timelines. Furthermore, the use of digital planning tools, surgical guides, and specific implant brands or designs can also vary between practitioners. This customization is precisely why a thorough consultation and detailed treatment planning phase are so critical; they ensure the protocol is perfectly tailored to deliver the optimal outcome for your individual circumstances, making your full mouth restoration truly your own.
How Much Do Full Mouth Dental Implants Typically Cost and Are There Financing Options?
The cost of full mouth dental implants typically varies significantly, often ranging from tens of thousands of pounds, for example, from approximately £15,000 to £30,000 or even upwards of £50,000 or more for a complete restoration of both arches, depending on a multitude of complex factors, and reassuringly yes, various financing options are generally available through dental practices or third-party lenders to help patients manage this substantial yet often life-changing investment in their long-term oral health, function, and overall quality of life. It’s crucial to understand that this figure isn’t arbitrary; it reflects the complexity of the procedures, the high-quality materials used (biocompatible titanium implants, sophisticated prosthetic teeth), the advanced technology involved (3D imaging, CAD/CAM fabrication), and the extensive training and expertise required from the entire dental team, including surgeons, restorative dentists, and laboratory technicians. While the initial outlay is considerable, many view it as a worthwhile investment when compared to the ongoing costs and limitations of less permanent solutions, or the health implications of untreated tooth loss. The availability of financing, such as tailored payment plans or medical loans, can make this transformative treatment more accessible, allowing the cost to be spread over a manageable period.
What Factors Influence the Overall Price of Full Mouth Dental Implants?
Numerous critical and interconnected factors profoundly influence the overall price of full mouth dental implants, including, but not limited to, the precise number and specific type or brand of implants being surgically placed, the inherent complexity of the surgical procedure itself (such as the need for angled implants or addressing anatomical challenges), the choice of advanced materials for the final, custom-fabricated prosthesis (e.g., acrylic versus premium zirconia), the distinguished experience, specialist qualifications, and geographical location of the dentist and surgeon, and the absolute necessity for any preparatory procedures like intricate bone grafting, sinus lifts, or multiple tooth extractions prior to implant placement. For instance, using six or eight implants per arch will naturally cost more than an All-on-4® approach. Premium implant brands with extensive research backing them may carry a higher price tag. If your case requires complex bone augmentation to rebuild lost jaw structure, this adds significantly to both the cost and treatment time. The type of final teeth – a high-impact acrylic hybrid bridge versus a full monolithic zirconia bridge – represents a substantial cost differential. Furthermore, fees will vary between a general dentist with implant training and a board-certified specialist like an oral surgeon or prosthodontist. Urban centres often have higher overheads, impacting prices. Even the type of anaesthesia or sedation chosen can affect the final bill. It’s a bespoke solution, and the price reflects that individual tailoring.
What Is the Average UK Price Range for Full Dental Implants?
While providing an exact, universally applicable average UK price for full dental implants is inherently challenging due to the wide variability influenced by the numerous factors previously discussed, patients in the UK can generally expect a broad price range from approximately £15,000 to £30,000+ *per arch* for well-established solutions like All-on-4® using high-quality materials and experienced clinicians, meaning a comprehensive full mouth restoration involving both upper and lower arches could potentially range from £30,000 to £60,000 or even more for highly complex cases or those utilising premium-tier materials like full zirconia and involving specialist care; however, it is absolutely crucial to obtain personalized, detailed written quotes from several reputable local providers following a thorough consultation and diagnostic assessment. These figures typically aim to be inclusive of the initial consultation, diagnostic imaging (like CBCT scans), the surgical placement of the implants, the implants themselves, abutments, a temporary prosthesis (if part of the protocol), the final bespoke prosthesis, and a certain number of post-operative follow-up appointments. Always clarify exactly what is included in any quoted fee to avoid unexpected additional costs for things like extractions, bone grafting (if needed and not explicitly included), sedation, or long-term maintenance visits. Remember, the cheapest option is rarely the best when it comes to complex medical procedures.
How Much Might Full Mouth Implants Cost in Turkey or Other International Locations?
Full mouth implants in Turkey or other popular international dental tourism destinations often present a significantly lower headline cost compared to the UK, potentially ranging from as little as £5,000 to £15,000 per arch for what appears to be a similar treatment; however, prospective patients must meticulously and critically factor in a host of additional, often less obvious, expenses such as multiple return flights, accommodation for extended stays, travel insurance that covers planned dental work abroad, and crucially, the inherent complexities, potential risks, and logistical challenges associated with obtaining adequate follow-up care, managing any post-operative complications from afar, understanding and enforcing warranties, and navigating potentially differing regulatory standards, material qualities, and clinician qualifications. While the initial quote can be tempting, the true total cost, both financial and non-financial, needs careful evaluation. Consider who will provide immediate aftercare if a problem arises once you’re back in the UK. Will your local dentist be willing or able to treat complications from work done overseas, and at what cost? Are the implant systems and materials used internationally recognized and serviceable in the UK? Language barriers, differing treatment philosophies, and the lack of long-term patient-dentist relationships are also vital considerations. While some patients report positive experiences, thorough research into specific clinics and surgeons, coupled with a realistic assessment of all potential downsides, is paramount before embarking on dental tourism for such complex procedures.
How Does the Cost of Full Mouth Dental Implants Compare to Traditional Dentures?
While the upfront, initial cost of full mouth dental implants is undeniably and significantly higher than that of traditional removable dentures, the long-term value proposition and overall cost-effectiveness often make implants the more prudent financial choice when considering the recurring, cumulative expenses associated with conventional dentures – such as the ongoing need for messy adhesives, periodic professional relines to adjust fit as the jawbone shrinks, and complete denture replacements typically required every 5 to 10 years – alongside the unquantifiable but very real costs associated with a potentially lower quality of life, persistent dietary restrictions, and the progressive, detrimental bone loss intrinsically linked to long-term denture wear. Traditional dentures might seem like a bargain at first glance. However, their maintenance is a continuous cycle: adhesives to try and keep them stable, relines as your gums and bone change shape (which they will, more rapidly under dentures), and eventual replacement as they wear out or no longer fit. Each of these incurs costs over time. Dental implants, conversely, are designed for longevity. The implants themselves can last a lifetime with good care, and while the prosthetic teeth may need refurbishment or replacement after 10-20+ years, the foundational support remains. Furthermore, implants help preserve jawbone, potentially avoiding more complex and costly bone grafting procedures in the future. When you factor in the improved chewing ability, better nutrition, enhanced confidence, and absence of daily denture hassles, the higher initial investment in implants often translates to superior long-term value.
Are There Finance Options Available for Full Jaw Dental Implants?
Yes, thankfully, numerous accessible finance options are typically available to help patients manage the considerable cost of full jaw dental implants, ranging from convenient in-house dental practice payment plans that allow the total sum to be spread over an agreed period, often with interest-free terms for shorter durations, to specialized third-party healthcare financing companies that offer longer-term medical loans with competitive interest rates, and also encompassing more traditional routes such as personal bank loans or, in some limited circumstances, potential partial contributions from private dental insurance policies if specific criteria are met. Many dental clinics understand that full mouth implants represent a significant financial commitment and have therefore partnered with finance providers or established their own systems to make treatment more attainable. These plans can break down the cost into monthly instalments, much like a car loan or mortgage. When exploring third-party financing, it’s essential to carefully review the terms and conditions, including the APR (Annual Percentage Rate) and total amount repayable. Some patients may choose to use savings, a credit card (though be mindful of interest rates if not a 0% promotional period), or a loan from their bank. It’s always wise to discuss these options openly with the clinic’s treatment coordinator, who can often guide you through the application process and help you find a solution that fits your budget, ensuring that the pathway to your transformed smile is financially manageable.
How Long Do Full Mouth Dental Implants Usually Last and How Should I Care for Them?
Full mouth dental implants, when expertly placed and meticulously cared for, can usually last for many, many years, often proving to be a lifetime solution for the implant posts themselves which are securely integrated within the jawbone, while the full-arch prosthetic component (the visible teeth) may require professional refurbishment, repair, or complete replacement after approximately 10 to 20 years or even longer, depending on the materials used and biting forces; their ultimate longevity is critically and inextricably dependent on the patient’s commitment to diligent daily oral hygiene practices and adherence to a schedule of regular professional maintenance and check-ups. Think of the implants as the foundations of a house – built to last. The prosthetic teeth are like the roof – robust and durable, but potentially subject to wear and tear over decades of daily use. With excellent home care – brushing, flossing with specialized aids, and using interdental cleaners – and regular visits to your dentist and hygienist for professional cleanings and assessments, you can significantly maximize the lifespan of both the implants and the prosthesis. Factors like smoking, teeth grinding (bruxism), or certain systemic health conditions can impact longevity, but for most, full mouth implants represent an enduring investment in oral health.
What Is the Expected Lifespan of a Full Mouth Implant Restoration?
The expected lifespan of a full mouth implant restoration sees the titanium dental implants themselves – the posts surgically embedded in the jawbone – demonstrating remarkable longevity, with high success rates indicating they can potentially last a lifetime when properly cared for and successfully integrated with the bone; whereas the prosthetic component, which is the visible bridge or denture attached to these implants, typically has a lifespan of around 10 to 20 years, or even longer for premium materials like zirconia, before it may require professional repair, relining, or complete replacement due to normal wear and tear from daily chewing, subtle changes in the oral environment, or aesthetic considerations. Clinical studies consistently show implant survival rates exceeding 90-95% over 10-15 year periods, and many last much longer. The prosthetic arch, whether made of acrylic, composite, PFM, or zirconia, is subject to the forces of biting and chewing daily. Acrylic and composite may wear or stain more quickly than zirconia, which is exceptionally durable. However, even the most robust materials can eventually show signs of wear or may suffer accidental damage. Regular dental check-ups allow your dentist to monitor both the implants and the prosthesis, addressing any minor issues like a loose screw or a small chip before they become bigger problems, thus extending the functional life of your restoration.
How Do You Properly Clean Under Full Mouth Dental Implants?
Properly cleaning under and around full mouth dental implants is absolutely crucial for their long-term health and success, and involves a dedicated daily oral hygiene routine using a combination of specialized tools designed to access and remove plaque and food debris from all surfaces, including areas where the prosthesis meets the gum tissue; this typically includes gentle brushing with a soft-bristled toothbrush and low-abrasive toothpaste, meticulous use of interdental brushes of appropriate sizes to clean between any supporting abutments, employing superfloss or floss threaders to navigate under the fixed bridge, and often incorporating a water flosser (oral irrigator) on a low to medium setting to effectively flush out particles from hard-to-reach areas, all supplemented by regular professional cleanings by a dental hygienist experienced with implant care. A soft toothbrush ensures you don’t abrade the prosthesis or irritate the gums. Interdental brushes, sometimes called “proxy brushes,” are excellent for cleaning the sides of implants if accessible and around any abutments. Superfloss has a stiffened end to thread it under the bridge, a spongy section to clean broader surfaces, and regular floss for other areas. A water flosser is invaluable for dislodging debris from beneath the prosthesis where bristles and floss might struggle. Some dentists may also recommend an antimicrobial mouth rinse. The key is consistency and thoroughness, ensuring no plaque biofilm is allowed to accumulate, which could lead to gum inflammation (mucositis) or bone loss around the implants (peri-implantitis).
What Are the Essential Steps to Take Care of Your Smile After Full-Mouth Dental Implants?
The essential steps to take meticulous care of your new smile after receiving full-mouth dental implants revolve around establishing and maintaining consistent, thorough daily oral hygiene practices as outlined by your dental team, strict adherence to a prescribed schedule of regular professional dental check-ups and specialized hygienist cleanings, consciously avoiding detrimental habits such as smoking or using your new teeth as tools to open packages or bite inedible objects, protecting your investment by wearing a custom-made nightguard if you clench or grind your teeth (bruxism), and promptly addressing any unusual concerns or changes with your dental professional. Your daily cleaning routine is paramount – it’s your first line of defence against complications. Professional check-ups, typically every six months (or more frequently if advised), allow your dentist to assess implant stability, the integrity of the prosthesis, and the health of your gum tissues, while the hygienist performs a deep clean, removing any calculus or plaque you might have missed. Quitting smoking is one of the single best things you can do for implant longevity, as smoking severely compromises healing and immune response. Using your teeth for anything other than eating can lead to fractures or damage. If bruxism is suspected, a nightguard will protect your prosthetic teeth from excessive forces. Early detection of any issue, like slight mobility or gum inflammation, allows for prompt intervention, often preventing more serious problems.
What Is the Experience Like Regarding Pain and Recovery After Full Dental Implant Procedures?
The experience regarding pain after full dental implant procedures is generally reported by patients as being surprisingly manageable, with any significant discomfort typically concentrated in the first few days post-surgery and effectively controlled with prescribed or readily available over-the-counter pain medication; the overall recovery period involves an initial phase of soft tissue healing and resolution of swelling over approximately one to two weeks, followed by the longer, silent biological process of full bone integration (osseointegration) which unfolds over several months, with patients receiving detailed post-operative instructions and support from their dental team to ensure as smooth and comfortable a process as possible. While any surgical procedure will involve some level of discomfort, modern anaesthetic techniques, sedation options, and pain management strategies have made the full mouth implant journey far more comfortable than many anticipate. Most patients describe the post-operative feeling as similar to that following multiple tooth extractions – a manageable soreness rather than acute pain. Adherence to aftercare instructions, including rest, proper diet, and medication use, plays a significant role in the recovery experience. The dental team is there to support you, address concerns, and make adjustments as needed to keep you comfortable.
Are Full Mouth Dental Implants Painful to Have Fitted?
While the prospect of undergoing surgery can naturally evoke anxiety about discomfort, having full mouth dental implants fitted is typically not painful *during* the actual procedure itself due to the highly effective administration of local anaesthesia, which thoroughly numbs the surgical areas, often supplemented by various sedation options (like oral sedatives, IV “twilight” sedation, or even general anaesthesia) for enhanced patient comfort and profound anxiety management; post-operatively, patients usually experience a degree of manageable discomfort, swelling, and bruising for a few days to a week, which can be well-controlled with prescribed pain relief medication, over-the-counter analgesics like ibuprofen, and proper home aftercare such as applying cold compresses. During the surgery, you might feel pressure or vibration, but not sharp pain. The dental team is highly attuned to patient comfort and will ensure you are adequately anaesthetized throughout. The post-operative phase is when you’ll manage soreness. The intensity and duration vary per individual but most find it less challenging than they imagined. Following your surgeon’s instructions meticulously regarding medication, diet (soft foods initially), rest, and oral hygiene will significantly contribute to a smoother, more comfortable healing period. Any pain that is severe, worsening, or not controlled by medication should be reported to your dentist immediately.
How Long Does It Generally Take to Recover from a Full Dental Implant Procedure?
General recovery from a full dental implant procedure unfolds in distinct stages: the initial, more noticeable functional recovery, where significant post-operative discomfort, swelling, and bruising substantially subside, typically takes about one to two weeks, allowing most individuals to return to their normal daily activities and a less restricted (though still somewhat soft) diet; however, the complete biological recovery, which refers to the crucial and largely invisible process of full osseointegration where the dental implants securely and permanently fuse with the surrounding jawbone, requires a more extended period, generally lasting from three to six months, and sometimes longer in certain clinical situations. During the first 24-48 hours, you’ll focus on rest, managing swelling with ice packs, and taking prescribed medications. By the end of the first week, much of the initial soreness and swelling should have diminished significantly. Stitches might dissolve or be removed around 7-14 days. While you might feel “back to normal” relatively quickly in terms of daily functioning, the underlying bone healing is a slower, vital process that cannot be rushed. It’s during this 3-6 month period that the implants achieve the stability needed to support the final prosthesis long-term. Patience during this phase is key to the overall success of the treatment.
How Will Eating and Chewing Be Affected with Full Mouth Dental Implants?
Eating and chewing will be profoundly and positively affected with full mouth dental implants, allowing individuals, once the implants are fully healed and the final, robust prosthesis is expertly fitted, to enjoy a remarkably wide variety of foods with a newfound confidence, comfort, and efficiency that is often comparable to that experienced with strong, healthy natural teeth, marking a significant and liberating improvement over the considerable limitations and frustrations commonly imposed by missing teeth or ill-fitting, unstable traditional dentures. This restoration of oral function is one of the most celebrated benefits. The stability afforded by implants anchored in the jawbone translates directly into increased biting force and chewing power. Foods that were previously off-limits or challenging – think crunchy fruits and vegetables, nuts, or a hearty steak – can often be reintroduced into the diet. This not only enhances the sheer pleasure of eating but can also lead to improved nutrition, as a wider range of healthy foods becomes accessible. The experience is a world away from the careful, often tentative chewing associated with loose dentures, where fear of dislodgement or discomfort is a constant companion. With full mouth implants, eating becomes a natural, enjoyable act once more.
Can You Eat Normally with Full Mouth Dental Implants Once Healed?
Yes, absolutely, once your full mouth dental implants are fully healed, osseointegration is complete, and your final, precisely fitting prosthesis is securely in place, you can confidently expect to eat normally, enjoying a diverse, nutritious, and satisfying diet without the pervasive restrictions, discomfort, or anxieties often associated with the experience of having missing teeth or struggling with ill-fitting traditional dentures; these advanced restorations are specifically designed to effectively restore your natural chewing capacity, allowing you to bite into and masticate foods with ease and pleasure. “Normally” in this context means being able to tackle a wide spectrum of food textures – from soft to firm, from crisp to chewy – much like you would with a full set of healthy natural teeth. You can anticipate returning to enjoying your favorite meals without worrying about your teeth slipping, rocking, or causing sore spots on your gums. This ability to chew efficiently not only improves digestion but also significantly enhances your overall quality of life and enjoyment of social dining. While it’s always wise to exercise some caution with extremely hard items (like cracking nutshells or chewing ice), the day-to-day experience of eating is dramatically and positively transformed.
How Long After Full Mouth Dental Implants Can I Resume a Normal Diet?
You can typically begin to resume a more normal, varied diet gradually in stages after receiving full mouth dental implants: initially, for the first week or two post-surgery, a diet of very soft foods and liquids is essential to protect the healing surgical sites and allow for comfortable recovery; thereafter, you can progressively transition to firmer soft foods that require minimal chewing as your comfort allows over the next few weeks; however, a return to a largely unrestricted, normal diet, where you can confidently chew a wide range of foods, usually occurs once the implants have fully integrated with the jawbone and your final, permanent prosthesis has been fitted, a milestone typically reached several months after the initial implant placement. During the immediate post-operative phase, think smoothies, soups, yogurts, mashed potatoes – anything that requires little to no chewing. As healing progresses, often guided by your dentist and your own comfort levels (especially if you have a temporary prosthesis), you can introduce items like scrambled eggs, soft cooked pasta, fish, and well-cooked vegetables. It’s crucial to avoid putting excessive force on the implants while they are integrating. Once osseointegration is confirmed (usually 3-6 months) and your permanent, robust teeth are in place, you can then start reintroducing harder, chewier foods systematically, effectively reclaiming your full dietary freedom.
Is It Hard to Eat or Can You Chew Gum with Full Mouth Dental Implants?
No, it is generally not hard to eat with full mouth dental implants once they are fully healed and the final restoration is in place; in fact, for most people, eating becomes significantly easier, more comfortable, and far more enjoyable compared to living with missing teeth or struggling with conventional dentures, thanks to the stability and restored chewing power. As for chewing gum, while it’s usually permissible with most modern full mouth implant prostheses, especially if it’s sugar-free to protect overall oral health, it’s always a wise precaution to discuss this specific activity with your dentist. Some extremely sticky or tacky substances, including certain types of gum or chewy candies, might theoretically pose a slight risk to the bond of a cemented prosthesis or could be more challenging to clean around certain prosthetic designs, though this is less of a concern with screw-retained designs. Your dentist can advise based on the specific materials and design of your restoration. The overall experience of eating is one of liberation; the solid foundation provided by the implants means you can bite and chew with a force and confidence that closely mimics natural teeth, making mealtimes a pleasure rather than a challenge.
Can I Eat and Speak Normally with Full Mouth Dental Implants?
Yes, unequivocally, with properly designed and fitted full mouth dental implants, you can absolutely expect to eat and speak normally and with a renewed, often profound, sense of confidence; the exceptional stability and custom fit of the implants and the overlying full-arch prosthesis work in harmony to restore natural oral function, frequently correcting speech impediments or difficulties that may have arisen from missing teeth or ill-fitting, mobile dentures, while simultaneously allowing for comfortable, efficient, and enjoyable chewing of a wide and varied range of foods. Missing teeth or loose dentures can often lead to lisps, whistles, or slurred speech as the tongue and lips struggle to form sounds correctly without proper dental support. Implants provide a fixed, stable structure that allows for clear and natural articulation. Similarly, the ability to chew effectively is restored, meaning you can enjoy your meals without fear of your teeth shifting or an inability to break down food adequately. This dual restoration of function not only improves physical health (through better nutrition and digestion) but also has a significant positive impact on social interaction, self-esteem, and overall well-being, as you no longer have to feel self-conscious about how you eat or sound when you talk.
What Are the Potential Negatives or Problems Associated with Full Mouth Dental Implants?
While full mouth dental implants offer truly remarkable and often life-altering benefits, boasting impressively high long-term success rates when performed by skilled clinicians, potential negatives or problems can indeed arise, which may include the significant upfront financial cost of treatment, the inherently lengthy overall treatment timeline involving surgery and an extended healing period, the intrinsic risks associated with any surgical procedure such as the possibility of infection, nerve irritation, or, in rare cases, implant failure (though uncommon when protocols are followed), and the non-negotiable, lifelong need for meticulous oral hygiene and regular professional maintenance to ensure their continued success and health. It’s crucial to approach this transformative journey with a balanced perspective. The financial investment is considerable and can be a barrier for some. The time commitment, from initial consultation to final restoration, can span many months. Surgery, by its nature, carries risks, however small when managed by experienced hands – these can include bleeding, swelling, bruising, and, very rarely, more significant issues like sinus perforation (for upper jaw implants) or persistent numbness if a nerve is affected. Implant failure, where an implant doesn’t integrate with the bone or loses integration later, can occur, often linked to factors like smoking, uncontrolled systemic diseases, or excessive bite forces. Finally, these are not ‘fit and forget’ teeth; they require diligent care to prevent complications like peri-implantitis (inflammation and bone loss around implants).
What Are the General Cons or Downsides of Full Mouth Dental Implants?
The general cons or downsides of full mouth dental implants, despite their overwhelming advantages for many, primarily revolve around their substantial financial investment, which can be prohibitive for some individuals; the extended duration of the overall treatment process, which can take many months from start to finish and requires considerable patience; the intrinsically surgical nature of the implant placement procedure, which, like any surgery, carries inherent risks (though generally low and manageable); and the absolute, unwavering necessity for diligent, lifelong oral hygiene practices and consistent, regular professional dental care to maintain their health and success over the years. The cost is often the first hurdle patients consider. The treatment journey isn’t a quick fix; it involves multiple appointments, healing periods, and laboratory work. Surgical risks, while minimized with careful planning and execution, can include infection, bleeding, swelling, discomfort, and, rarely, damage to adjacent nerves or sinuses, or implant non-integration. Furthermore, the prosthetic component (the teeth) will eventually wear or may require repair or replacement after many years of service, incurring additional future costs. For some, the psychological aspect of undergoing surgery can also be a concern, though sedation options greatly help. It’s a significant commitment, not just financially, but also in terms of time and personal effort for upkeep.
Does Food Get Trapped Under Full Mouth Dental Implants, and How Is This Managed?
Yes, it is indeed possible for tiny food particles to occasionally get trapped under certain designs of full mouth dental implant prostheses, particularly at the subtle interface where the artificial gum portion of the bridge meets the patient’s own gum tissue, or in minute spaces around the implant abutments; however, this common concern is effectively managed and mitigated through meticulous, dedicated daily oral hygiene using specialized cleaning aids like water flossers (oral irrigators) and interdental brushes, coupled with careful, intelligent prosthetic design considerations by the dentist and laboratory technician to minimize potential food-impaction areas and facilitate easy cleaning. While the prosthesis is designed to fit snugly, the natural contours of the gums and the structure of the bridge mean that tiny crevices can exist. A water flosser is particularly invaluable for these situations, as it can direct a pulsating stream of water to flush out debris from underneath the bridge and around the implants where bristles might not reach effectively. Interdental brushes of various sizes can also help clean around the implant posts if they are accessible. Good prosthetic design aims for smooth, cleansable contours. If food trapping becomes a persistent or problematic issue, it’s important to discuss it with your dentist, as minor adjustments to the prosthesis or enhanced hygiene techniques might be all that’s needed. Regular professional cleanings are also vital to remove any stubborn debris or plaque.
Are There Alternatives to Full Mouth Implants for Complete Tooth Replacement?
Yes, there are indeed established alternatives to full mouth implants for achieving complete tooth replacement, primarily consisting of traditional removable full dentures, which are custom-made prosthetic devices that rest directly on the gums and underlying jawbone for support, and to a lesser extent for some specific clinical scenarios where a few healthy, strategically positioned natural teeth might remain, removable partial dentures can be considered, though it’s crucial to recognize that these conventional options do not offer the same superior level of stability, chewing function, comfort, or the vital long-term benefit of jawbone preservation that is characteristic of implant-supported solutions. For individuals who are missing all teeth in an arch, the most common non-implant alternative is a complete conventional denture. These have been used for centuries in various forms and can provide a reasonable aesthetic and functional outcome for some, especially if well-made and regularly maintained. However, they rely on suction and the shape of the residual alveolar ridge for retention, which can diminish over time as the bone resorbs. Implant-retained overdentures (which do use a few implants but are often considered a step below full fixed implant bridges) offer a significant improvement over conventional dentures in terms of stability, representing a hybrid option. For those seeking to avoid implants entirely, the choices are more limited and come with well-documented compromises in performance and long-term oral health impact.
How Do Full Mouth Dental Implants Compare to Traditional Full Dentures?
Full mouth dental implants compare very favorably and are generally considered vastly superior to traditional full dentures across nearly every critical aspect of performance and patient experience, most notably in terms of exceptional stability and retention, significantly enhanced chewing function and dietary freedom, superior comfort and speech clarity, and crucially, their positive impact on long-term oral health through the preservation of underlying jawbone structure; implants achieve this by being securely anchored directly into the jawbone, providing a fixed and robust foundation for the prosthetic teeth, whereas conventional dentures merely rest on the surface of the gums and are inherently prone to movement, slippage, and contributing to progressive bone resorption over time. With implants, your teeth are fixed – they don’t move when you eat, talk, or laugh. This stability allows for a bite force close to that of natural teeth, meaning you can eat a much wider range of foods. Traditional dentures, conversely, can limit chewing efficiency to as little as 20-30% of natural teeth. Implants eliminate the sore spots and rubbing often associated with dentures because the forces are transmitted to the bone, not just the gums. Speech is clearer with implants as there’s no palate coverage (for upper restorations) or loose appliance to contend with. Most importantly, implants stimulate the jawbone, preventing the shrinkage that makes dentures looser and facial appearance more aged over time – a process that dentures unfortunately accelerate. While dentures have a lower upfront cost, implants offer a far higher quality of life and better long-term oral health.
What Other Options Exist for Full Teeth Replacement Besides Implants?
Besides full mouth dental implants (which can be either fixed bridges or removable implant-supported overdentures), the primary other established option for achieving complete teeth replacement in an edentulous arch (an arch with no teeth) is a conventional full removable denture; this is a custom-fabricated acrylic prosthesis featuring artificial teeth, which rests directly on the gum tissues and the underlying residual alveolar ridge (jawbone) for its support and retention, relying on a combination of suction, muscle control, and sometimes dental adhesives to stay in place. These traditional dentures are a non-surgical option and have a significantly lower initial cost than implant-based solutions. They can restore basic function and aesthetics to a degree. However, their reliance on soft tissue support means they are prone to instability, especially in the lower jaw where there’s less surface area for suction. This can lead to difficulties with eating certain foods, occasional embarrassing slippage, and the need for denture adhesives. Over time, the jawbone beneath a conventional denture will continue to resorb (shrink) due to lack of stimulation, leading to a progressively poorer fit, requiring frequent relines and eventual replacement of the denture. While they serve a purpose, particularly for those who are not candidates for implants or for whom cost is the overriding factor, they come with inherent functional and biological compromises compared to implant solutions.
What Should I Consider Regarding Full Mouth Dental Implants in the UK, Including NHS Availability?
Regarding full mouth dental implants for patients based in the United Kingdom, key considerations must include a realistic understanding of the typically high private treatment costs, as NHS availability for this type of comprehensive, elective reconstructive procedure is exceptionally limited and generally reserved for very specific, non-routine clinical circumstances (such as severe trauma or consequences of cancer treatment); alongside this, the paramount importance of meticulously selecting a General Dental Council (GDC)-registered dentist or specialist with proven, demonstrable expertise and extensive experience in complex implantology is crucial, as is being fully aware of UK-specific financing options, clinic regulation by bodies like the Care Quality Commission (CQC), and adherence to stringent UK and EU material and procedural standards. The UK boasts a high standard of dental care, but advanced treatments like full mouth implants are predominantly offered in the private sector. This means thorough research into clinicians’ qualifications (e.g., postgraduate diplomas or master’s degrees in implantology, specialist registration in fields like prosthodontics or oral surgery) and their track record with similar complex cases is vital. Patients should also inquire about warranties, aftercare protocols, and ensure they receive a fully itemized treatment plan. Understanding your rights as a patient and the regulatory framework governing dental practices in the UK provides an additional layer of assurance.
Are Full Mouth Dental Implants Available on the NHS?
Full mouth dental implants are very rarely, almost exceptionally, available on the National Health Service (NHS) in the UK; NHS funding for dental implants of any kind is typically restricted to a narrow and stringent set of highly specific clinical needs, usually for patients who have lost teeth as a direct result of significant trauma (such as a major road traffic accident), oral cancer surgery and subsequent reconstruction, or for individuals born with severe developmental conditions like ectodermal dysplasia or significant cleft lip and palate where conventional dentures are demonstrably impossible or clinically inappropriate, meaning the vast majority of patients seeking full mouth restoration due to common reasons like widespread tooth decay, advanced gum disease, or general tooth wear will need to pursue and fund this treatment privately. The NHS provides essential dental care to maintain oral health, but comprehensive, elective, and high-cost procedures like full mouth implants fall outside the scope of routine NHS provision due to budgetary constraints and resource allocation priorities. If you believe you might fall into one of the exceptional categories, a referral from your general dental practitioner or a hospital consultant would be necessary for an NHS assessment, but it’s important to manage expectations as approval is uncommon for full arch rehabilitation. For most, the private dental sector is the pathway for this transformative treatment.
What Are Key Considerations for Seeking Full Mouth Dental Implants UK Based?
Key considerations for individuals seeking full mouth dental implants while based in the United Kingdom include, first and foremost, rigorously verifying the dentist’s or specialist’s qualifications, ensuring they are registered with the General Dental Council (GDC), and thoroughly scrutinizing their specific experience, training (such as postgraduate diplomas or MSc in Implantology), and extensive portfolio in successfully completing full arch implant cases; additionally, it’s vital to obtain and meticulously understand a detailed, itemized written treatment plan outlining all stages, associated UK pricing structures, and precisely what is included and excluded, while also inquiring about available warranties on implants and prosthetics, comprehensive aftercare arrangements, and the types of high-quality, regulated materials and advanced technologies (like CBCT scanning and digital planning) that will be utilized, all of which must adhere to stringent UK and European regulatory standards for safety and efficacy. Look for clinicians who are members of respected professional bodies like the Association of Dental Implantology (ADI) or the International Team for Implantology (ITI). Ensure the clinic is registered with and inspected by the Care Quality Commission (CQC) in England (or equivalent bodies in Scotland, Wales, and Northern Ireland), which regulates healthcare providers. Discuss financing options available through UK lenders or practice plans. Don’t hesitate to ask about success rates and how potential complications are managed. A transparent, communicative, and highly skilled UK-based team is essential for peace of mind and a successful outcome.
What Do Before and After Results of Full Mouth Dental Implants Typically Look Like?
The before and after results of full mouth dental implants typically showcase a truly dramatic, often profoundly life-enhancing transformation for patients, with common ‘before’ scenarios frequently depicting conditions such as significant tooth loss leading to an aged appearance, widespread dental decay or advanced gum disease compromising remaining teeth, or the daily struggles and aesthetic dissatisfaction associated with ill-fitting, worn-out traditional dentures; correspondingly, the ‘after’ results revealed following successful treatment unveil a fully restored, remarkably natural-looking, and aesthetically pleasing smile that not only rejuvenates one’s appearance but also significantly improves facial contours, restores confident function, and often radiates an overall boost in self-esteem and quality of life. These visual transformations can be astonishing. In “before” images, you might see collapsed bites, sunken cheeks due to bone loss, discoloured or missing teeth, and an understandably self-conscious expression. The “after” photographs, by stark contrast, usually present a vibrant, harmonious smile with well-proportioned, beautifully shaded teeth that look like they belong, supporting the lips and cheeks correctly, often leading to a more youthful and energetic appearance. Beyond the static images, the real “after” is seen in the patient’s renewed ability to eat, speak, and laugh without reservation. It’s a testament to how modern dentistry can not just repair but truly revitalize.
How Can I See Full Mouth Dental Implant Before and After Pictures?
You can typically see compelling full mouth dental implant before and after pictures by directly requesting to view a portfolio of successfully completed, similar cases during your comprehensive consultation with a prospective dental provider or implant surgeon, as many experienced and reputable implant dentists meticulously maintain these photographic records (always with explicit, prior patient consent) to visually demonstrate the quality and transformative potential of their work; additionally, some dental clinics also choose to showcase anonymized examples of their before and after results in dedicated galleries on their official websites or within patient information brochures and materials, offering a glimpse into the achievable outcomes. When you consult with a dentist, don’t hesitate to ask if they have examples of full mouth cases they’ve personally treated. This allows you to assess their aesthetic sense and the consistency of their results. On websites, look for high-quality images that clearly show the initial situation and the final outcome. Pay attention not just to the teeth, but also to how the new smile harmonizes with the patient’s facial features and the health of the surrounding gum tissues. Patient testimonials, sometimes accompanied by photos, can also provide valuable insights. Remember, these images should serve as an illustration of possibilities; your own results will be unique to your specific clinical situation and treatment plan. Ethical practitioners will always ensure patient privacy and consent when sharing such images.
How Do I Choose the Right Dentist for Full Jaw Implant Procedures?
Choosing the right dentist or specialist for incredibly intricate full jaw implant procedures involves a careful, diligent, and well-informed process of thoroughly researching their specific qualifications, explicitly looking for evidence of advanced postgraduate training and extensive, demonstrable hands-on experience in complex implantology and full arch restorations, meticulously reviewing genuine patient testimonials and scrutinizing comprehensive case portfolios showcasing their previous work, and crucially, ensuring there is clear, transparent communication, a comfortable rapport, and a sense of trust established during the initial consultation phase, as this relationship will be key throughout your transformative journey. This decision is arguably one of the most critical factors for treatment success. Don’t base your choice on cost alone. Look for dentists who have dedicated a significant portion of their practice to implant dentistry, particularly full arch cases. Consider specialists like prosthodontists (experts in tooth replacement), periodontists (gum and bone specialists with implant training), or oral surgeons (for the surgical phase), or experienced general dentists who have pursued significant additional qualifications in implantology. The consultation is your opportunity to gauge their expertise, their approach to patient care, and whether you feel confident placing your trust, and your smile, in their hands.
What Qualifications and Experience Should I Look for in a Full Jaw Implant Dentist?
When choosing a dentist for complex full jaw implant procedures, you should diligently look for specific, advanced qualifications such as accredited postgraduate degrees (e.g., an MSc in Implant Dentistry), specialist registration with the General Dental Council (GDC) in relevant fields like Prosthodontics, Periodontics, or Oral Surgery (though experienced general dentists can also excel with appropriate training), or recognized diplomas in implant dentistry (e.g., DipImpDent RCS Eng); alongside these formal qualifications, it’s vital to seek demonstrable, extensive clinical experience specifically evidenced by a substantial and varied portfolio of successfully completed full arch implant cases, active membership in reputable national and international implant associations (like the ADI or ITI), and a clear commitment to ongoing professional development and staying abreast of the latest advanced implant techniques and technologies. Ask about the number of full arch cases they perform annually. Inquire about their training in handling complex situations, including bone grafting if required. A clinician who routinely uses modern diagnostic tools like CBCT scanners and digital treatment planning software, and perhaps utilizes surgical guides for precision, is often indicative of a commitment to best practices. Ultimately, you’re looking for a blend of robust academic credentials, a proven track record, and a dedication to the specialized field of full mouth implant rehabilitation.
What Questions Should I Ask During a Consultation for Full Mouth Dental Implants?
During a crucial initial consultation for full mouth dental implants, you should come prepared to ask a series of critical and insightful questions regarding the dentist’s specific, hands-on experience with cases directly comparable to yours, the intricate details of their proposed, individualized treatment plan including all anticipated stages, alternative options, and the rationale behind their recommendations, the precise types of high-quality implants, abutments, and prosthetic materials they intend to use and why, the advanced technology (like 3D imaging or guided surgery) they will employ, a full, transparent breakdown of all associated costs including what is and isn’t covered, and any available financing options, the anticipated recovery process and timeline, potential risks or complications specific to your case and how they would be managed, and their long-term success rates, patient satisfaction levels, and the nature of their aftercare support and warranties.Specifically, consider asking:
-
- “How many full arch implant procedures like mine have you personally performed, and can I see anonymized before-and-after examples of your work?”
-
- “What are all my treatment options, and why are you recommending this particular approach for me?”
-
- “Could you explain the entire process step-by-step, including the timeline for each stage?”
-
- “What brand and type of dental implants do you use, and what are your reasons for this choice?”
-
- “What materials will my final teeth be made from (e.g., acrylic, zirconia), and what are the pros and cons?”
-
- “What technology, such as CBCT scans or surgical guides, will be used in my planning and surgery?”
-
- “Can you provide a fully itemized quote, detailing all costs, including surgery, prosthetics, follow-ups, and any potential extras like bone grafting or sedation?”
-
- “What are the specific risks and potential complications I should be aware of in my case?”
-
- “What is your clinic’s protocol if an implant fails or if there are complications post-surgery?”
-
- “What does the aftercare involve, who provides it, and what warranties are offered on the implants and the final prosthesis?”
- “What sedation options are available to ensure my comfort during the procedure?”
A thorough dentist will welcome these questions and provide clear, comprehensive answers, fostering your confidence in their expertise and your treatment plan.
Frequently Asked Questions About Full Mouth Dental Implants
Can You Have a Full Mouth of Dental Implants?
Yes, you absolutely can have a full mouth of dental implants, as this highly effective and transformative procedure is specifically designed to replace all missing or failing teeth in either the upper jaw (maxilla), the lower jaw (mandible), or, as is often the case, comprehensively in both jaws, thereby providing a complete, robust, and permanent solution for individuals experiencing widespread tooth loss or severe dental compromise. This advanced treatment, often referred to as full arch dental rehabilitation, allows for the restoration of an entire set of teeth using a strategic number of dental implants – typically four to eight per jaw – which act as artificial roots to securely anchor a custom-made, fixed bridge or, in some cases, a highly stable implant-supported overdenture. It’s a well-established and predictable treatment modality in modern dentistry, suitable for many adults who have lost their teeth due to extensive decay, advanced periodontal (gum) disease, trauma, or other conditions. The outcome is not just a renewed smile but a significant improvement in chewing ability, speech clarity, facial aesthetics, and overall quality of life, making it a life-changing option for eligible candidates.
How Long Do Full Jaw Dental Implants Last?
Full jaw dental implants, referring specifically to the titanium implant posts that are surgically placed and integrate within the jawbone, are meticulously designed to be an exceptionally long-term, often permanent, solution and can indeed last for many decades, frequently for a patient’s lifetime, provided they are cared for with exemplary diligence through excellent daily oral hygiene practices and consistent adherence to regular professional dental maintenance and check-ups; however, it’s important to distinguish that the prosthetic teeth (the bridge or denture) attached to these implants, while also durable, are subject to wear and tear from daily function and may typically require refurbishment, repair, or complete replacement approximately every 10 to 20 years, or potentially longer depending on the specific materials used (e.g., zirconia often lasts longer than acrylic). Factors influencing the longevity of both the implants and the prosthesis include the patient’s overall health, smoking habits (smoking is detrimental), bite forces (e.g., from teeth grinding or clenching, which may necessitate a nightguard), the quality of the initial surgery and prosthetic work, and the rigour of the maintenance routine. With proper care, the implants themselves have a very high success rate and can provide a stable foundation indefinitely.
Are Full Mouth Dental Implants Worth the Investment?
Yes, for the vast majority of individuals facing the profound challenges of extensive tooth loss or severely failing dentition, full mouth dental implants are overwhelmingly considered to be unequivocally worth the significant financial investment due to their profound, multifaceted, and lasting benefits, which include a dramatic improvement in chewing ability allowing for a more nutritious and enjoyable diet, the complete restoration of natural-looking aesthetics and a confident smile, markedly enhanced speech clarity and social ease, the crucial preservation of underlying jawbone health thereby maintaining facial structure, and a substantial, often immeasurable, boost in overall quality of life, self-esteem, and psychological well-being. While the upfront cost is considerable when compared to alternatives like traditional dentures, the long-term value derived from implants is often far greater. This value isn’t just monetary (e.g., fewer ongoing costs for adhesives, relines, or frequent replacements associated with dentures), but is deeply rooted in the daily functional and emotional advantages. The ability to eat, speak, and laugh without fear or discomfort, the elimination of denture-related sore spots, the maintenance of facial integrity, and the sheer confidence that comes from a secure, beautiful smile are outcomes that many patients describe as priceless and truly life-altering, making the investment a worthwhile commitment to their health and happiness.
How Painful Are Full Dental Implants During the Procedure?
During the actual surgical procedure to place full dental implants, patients typically experience no pain, or at most, very minimal discomfort, due to the highly effective and targeted administration of local anaesthesia, which thoroughly numbs the jaw areas being treated; this is often supplemented by various forms of conscious sedation (such as oral sedatives or intravenous “twilight” sedation) or, in some cases, general anaesthesia, all tailored to ensure the patient remains completely comfortable, relaxed, and anxiety-free throughout the entire surgical event. Post-operatively, once the anaesthesia wears off, it is normal to experience some manageable discomfort, swelling, and bruising for a few days to a week, the intensity of which can vary but is generally described as similar to that following multiple tooth extractions. This post-surgical soreness is typically well-controlled with a combination of prescribed pain relief medication, over-the-counter analgesics like ibuprofen or paracetamol, and supportive home care measures such as applying cold compresses to the affected areas, adhering to a soft diet, and getting adequate rest. The dental team provides comprehensive aftercare instructions to minimize discomfort and promote smooth healing, and any pain that is severe or worsening should always be promptly reported.
How Much Does a Full Mouth Dental Implant Cost on Average?
On average, the cost for a comprehensive full mouth dental implant procedure (which could involve one or both arches) can vary extremely widely, but patients in the UK, for example, might typically expect a range starting from approximately £15,000 to £30,000 or more *per arch* for established solutions like All-on-4 using high-quality components and experienced clinicians; therefore, a complete restoration for both the upper and lower jaws could potentially range from £30,000 to £60,000, and in some instances, particularly for highly complex cases, those utilizing premium-tier materials such as full monolithic zirconia for the final prostheses, or involving extensive preliminary work like significant bone grafting and specialist care, the total cost could exceed this. It is crucial to understand that “average” can be misleading due to the highly personalized nature of this treatment. Key factors influencing the final figure include the number and brand of implants used, the specific type and material of the final prosthetic teeth, whether bone grafting or sinus lifts are required, the complexity of the surgery, the geographical location of the clinic, and the expertise and reputation of the dental surgeon and restorative dentist. The only way to obtain an accurate cost is through a thorough consultation and personalized treatment plan from a qualified dental provider, which should include a detailed, itemized breakdown of all anticipated fees.





![Dental-Implants-NHS-e1747325783549-1024×915[1] Dental-Implants-NHS-e1747325783549-1024x915[1]](https://dentale-albania.com/wp-content/uploads/elementor/thumbs/Dental-Implants-NHS-e1747325783549-1024x9151-1-r5xyg5ea74oh73k9z5uv5amgw2c45uxhewp2r8hqqo.webp)