Key Takeaways
-
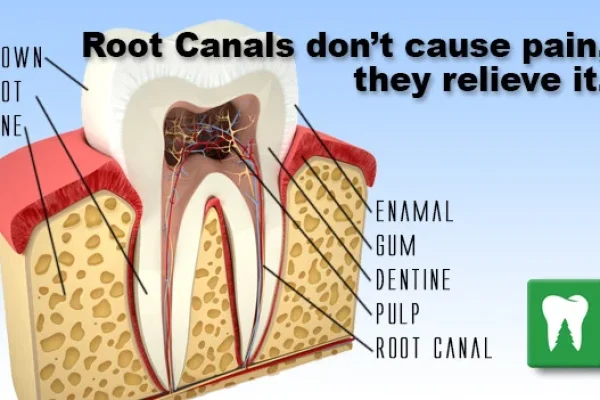
- Modern **canal root treatment** is a safe, highly successful procedure designed to *relieve* pain, not cause it.
-
- It saves your natural tooth by removing infected pulp, cleaning, and sealing the internal space.
-
- Common signs you might need one include severe toothache, lingering sensitivity, or gum swelling.
-
- Delaying treatment can lead to painful abscesses, bone loss, tooth fracture, and eventual extraction.
-
- The procedure is performed under local anaesthesia and is typically no more uncomfortable than a deep filling.
-
- Post-treatment soreness is usually mild and manageable, lasting a few days.
-
- A permanent restoration, often a crown, is usually needed after the root canal to protect the tooth.
-
- Preventative care like brushing, flossing, and regular check-ups is the best way to avoid needing a root canal.
- The cost varies depending on the tooth’s location and complexity, but saving a tooth is often more cost-effective long-term than extraction and replacement.
Canal root treatment: What Exactly Is It?
So, what is this procedure that carries such a heavy, often unfair, reputation? At its heart, **canal root treatment** is a specialized dental procedure focused on the interior of the tooth. When the soft tissue inside your tooth, known as the dental pulp, becomes infected or inflamed – typically due to deep decay, repeated dental procedures, faulty crowns, or trauma – it needs urgent attention. The pulp contains nerves, blood vessels, and connective tissue; it’s vital for the tooth’s development but not necessary for its continued function once it’s fully formed. When this pulp is compromised, bacteria can proliferate, leading to infection, swelling, and often, intense pain. Left untreated, this infection can spread beyond the tooth root into the surrounding bone, potentially causing an abscess and threatening overall health. Root canal treatment, or endodontic treatment as it’s formally known, is the process of removing this damaged or infected pulp, meticulously cleaning and disinfecting the inside of the tooth (specifically the pulp chamber and the root canals – hence the name), and then filling and sealing the space. This sealing process is critical to prevent future infection. Essentially, you’re removing the diseased core while preserving the tooth’s outer structure. It’s a marvel of micro-dentistry, working within tiny, complex anatomical spaces. Dispelling the myth of inevitable pain is crucial; the *pain* you feel is almost always from the *infection* itself, and the treatment is what stops it. With modern techniques and effective local anaesthesia, the procedure is often no more uncomfortable than having a deep filling placed. Understanding this purpose – stopping infection, relieving pain, and saving the tooth – is key to appreciating the value of **canal root treatment**. It’s not about ‘killing’ the tooth; it’s about allowing the tooth structure to remain a functional part of your mouth, supported by the surrounding bone and tissues, without the internal threat of disease.
root canal def: Understanding the Dental Procedure
At its core, a “root canal” refers to two things: firstly, the natural passageways within the tooth root where the dental pulp resides, and secondly, the clinical procedure used to treat issues within these canals. The tooth’s anatomy is surprisingly complex. The visible part above the gum is the crown, covered in enamel. Below the gum line, roots anchor the tooth to the jawbone. Inside the enamel and a layer of dentin is the pulp chamber, which extends down into the roots via narrow tunnels called root canals. This pulp is a living tissue containing nerves, blood vessels, and connective tissue, crucial during tooth development. However, if deep decay or injury reaches the pulp, bacteria can enter, leading to inflammation (pulpitis) and infection. This triggers pain because the nerves are trapped within a rigid structure. **Root canal treatment** addresses this by removing the infected pulp and sealing the now-empty canals to prevent reinfection.
When Might You Need canal root treatment? Recognizing the Signs
Understanding *why* a root canal becomes necessary is just as important as knowing *what* the procedure entails. It’s not a treatment administered on a whim; it’s typically required when the delicate pulp tissue inside your tooth becomes irreversibly damaged, inflamed, or infected. This often happens due to factors like deep decay that reaches the pulp chamber, repeated dental procedures on the same tooth, cracks or chips that expose the pulp to bacteria, or trauma to the face or mouth, even if there’s no visible damage to the tooth itself initially. The body’s natural defence mechanisms can’t effectively fight off infection deep within the tooth’s core, where blood supply is limited and there’s nowhere for swelling to expand, leading to intense pressure and pain. Recognising the early warning signs is crucial, not just for prompt treatment and pain relief, but also to prevent the infection from escalating. Ignoring symptoms can lead to more severe complications, including the spread of infection to neighbouring teeth, gums, and bone, and potentially even systemic health issues, though this is rare. Dentists use a combination of methods to diagnose the need for endodontic treatment, including detailed patient history regarding symptoms, thorough clinical examination, testing the tooth’s response to stimuli (like temperature), and most importantly, taking dental X-rays, which can reveal changes in the bone around the root tip indicative of infection or abscess formation. Sometimes, the need is discovered during a routine check-up or when investigating unrelated symptoms. Timely intervention is paramount; waiting too long allows the infection to cause more damage, potentially making the tooth unrestorable and necessitating extraction, a far less desirable outcome than saving your natural tooth with **canal root treatment**. Being attuned to changes in your dental comfort level is your first line of defence.
What are the signs of needing a root canal? Identifying Symptoms
The most common symptom is severe toothache, especially pain that is persistent, throbbing, or wakes you up at night. Sensitivity to hot and cold liquids or food that lingers long after the stimulus is removed is another key indicator. You might notice swelling and tenderness in the surrounding gums, sometimes accompanied by a small pimple-like bump (called a fistula or sinus tract) on the gum, which is where pus is draining from the infection. Discoloration of the tooth (it might look darker) can also signal pulp damage. Pain might initially be sharp, then become a dull ache, or even disappear entirely if the pulp dies, but this doesn’t mean the infection is gone – it simply means the nerves are no longer functioning to signal pain, while the bacteria continue to spread.
What happens if you don’t get a root canal? Consequences of Delay
Delaying or avoiding needed **canal root treatment** is a gamble with high stakes for your oral and potentially overall health. The infection originating in the tooth’s pulp will not resolve on its own because the body’s immune system cannot effectively reach and clear the bacteria inside the sealed root canal system. Instead, the infection will continue to fester and spread. This can lead to a painful abscess at the root tip, a pocket of pus that can cause significant swelling in the face, jaw, or neck. The infection can also destroy the bone supporting the tooth, weakening it and eventually leading to tooth loss. In severe, though less common, cases, the infection can spread to other parts of the body, potentially causing serious systemic health problems. Furthermore, delaying treatment allows the tooth structure to weaken, making it more susceptible to fracture. Ultimately, neglecting a tooth that requires root canal treatment almost invariably results in the tooth needing to be extraction, which then opens up a new set of challenges and costs, including the need for prosthetic replacement like a bridge, implant, or denture to restore function and prevent adjacent teeth from shifting. Saving your natural tooth through a root canal is almost always the preferred, most conservative, and often most cost-effective long-term solution compared to the consequences of allowing the infection to progress unchecked and losing the tooth.
What Happens During the canal root treatment Procedure? A Step-by-Step Look
Okay, let’s pull back the curtain on the process itself. Knowing the steps involved in **canal root treatment** can significantly reduce anxiety and demystify the procedure. Far from being a brutal ordeal, it’s a carefully orchestrated series of precise steps aimed at thoroughly cleaning, disinfecting, and sealing the intricate internal space of your tooth. The goal is simple: remove the source of the problem (the infected pulp) and create a clean, sealed environment that prevents future bacterial invasion, thereby saving the tooth. The length of the procedure varies depending on the complexity of the tooth’s anatomy (molars, for example, have more roots and canals than front teeth) and the severity of the infection. Most root canals are completed in one or two appointments, each typically lasting from 30 to 90 minutes, sometimes longer for particularly complex cases. The number of visits depends on factors like the presence of significant infection requiring initial medication, or complex canal shapes that are easier to clean and seal after an initial cleaning and a period of healing. Throughout the entire process, patient comfort is paramount, ensured primarily through effective local anaesthesia. Think of it like micro-surgery, but instead of operating on a visible organ, the dentist (or specialist endodontist) is working within the tiny, hidden passageways of your tooth root. It’s a meticulous process, requiring significant skill and specialized instruments, including very fine files and sophisticated imaging techniques. The result is a tooth that is no longer experiencing internal disease and can continue to function as part of your natural bite for years, often decades, to come, provided it is properly restored and cared for.
Step-by-step breakdown of the treatment process
The procedure generally follows these stages:
- **Anaesthesia:** The area around the affected tooth is numbed using local anaesthetic. This is crucial for comfort; you should feel pressure or vibration but no pain during the procedure itself.
- **Access:** A small opening is made in the crown of the tooth to access the pulp chamber and root canals.
- **Pulp Removal:** Using fine instruments, the infected or damaged pulp tissue is carefully removed from the pulp chamber and the full length of each root canal.
- **Cleaning and Shaping:** The canals are thoroughly cleaned and shaped using increasingly larger dental files. This process removes remaining tissue and bacteria and creates a space that can be effectively filled. Irrigation solutions are used throughout this stage to flush out debris and disinfect the canals.
- **Filling (Obturation):** Once the canals are clean, dry, and shaped, they are filled with a biocompatible material, most commonly gutta-percha (a rubber-like material), usually combined with a sealing cement. This material fills the canal space completely.
- **Temporary Seal:** A temporary filling is placed in the opening in the tooth crown to protect the sealed canals until the final restoration is completed.
What to Expect Before and During the Procedure
Before your **canal root treatment**, you’ll have a consultation where your dentist or endodontist will examine the tooth, take X-rays, and discuss the diagnosis and treatment plan. Don’t hesitate to ask questions about the procedure and recovery. On the day of the appointment, the first step is administering local anaesthesia. You’ll feel a small prick initially, but the area will quickly go numb. During the procedure, the dentist will use a rubber dam to isolate the tooth, keeping it clean and dry and preventing instruments or solutions from entering your mouth. You’ll feel pressure as they work, and perhaps some vibrations from the instruments, but pain should not be an issue thanks to the anaesthesia. If you feel any discomfort, raise your hand, and the dentist can administer more anaesthetic.
Does a root canal remove the nerve? Understanding Pulp Removal
Yes, the dental pulp, which contains the tooth’s nerves and blood vessels, is removed during a root canal. It’s the removal of the *nerve* tissue within the pulp that eliminates the tooth’s ability to feel hot, cold, or pain signals originating from within the tooth structure itself (like from decay or infection). However, the tooth isn’t entirely “dead.” It’s still anchored in your jawbone by living tissues (the periodontal ligament), which provide feeling related to pressure and chewing. So, while the tooth no longer feels internal stimuli, it remains a living, functional entity supported by its surroundings. The term “dead” tooth is often used, but “non-vital” or “endodontically treated” tooth is more accurate.
Is anesthesia required for a root canal? Ensuring Comfort
Absolutely. Local anaesthesia is a standard and essential part of the **canal root treatment** process. Its purpose is to completely numb the tooth and surrounding tissues, ensuring that you do not feel pain during the procedure itself. For patients with significant dental anxiety, dentists may offer additional options like IV sedation, though this is less common for standard root canals and might require a specialist. The goal is always to make the experience as comfortable and stress-free as possible. Anaesthesia is administered at the beginning of the appointment once the dentist is certain the tooth is thoroughly numb, they will begin the procedure.
How many visits does a root canal take? Procedure Duration
The vast majority of uncomplicated **canal root treatment** procedures can be completed in a single appointment, typically lasting between 60 and 90 minutes. However, some situations necessitate two visits. These might include cases where there is a significant, acute infection or large abscess requiring drainage and medication within the tooth to settle down before filling, teeth with complex anatomy (such as very curved or narrow canals), or teeth that are particularly difficult to access. In a two-visit scenario, the initial appointment focuses on cleaning and disinfecting the canals, medication might be placed inside, and a temporary filling seals the tooth. The second visit, usually a week or two later, involves removing the temporary filling and placing the permanent gutta-percha filling. Your dentist will determine the appropriate number of visits based on your specific case.
Is canal root treatment Painful? Addressing a Common Concern
Let’s tackle the elephant in the room head-on: the deep-seated, often outdated, belief that **canal root treatment** is inherently agonising. This simply isn’t the case with modern endodontic practices. The truth is, the severe pain usually associated with “root canals” is the pain caused by the underlying *infection or inflammation* within the tooth’s pulp *before* you even get to the dentist. The root canal procedure itself is performed under effective local anaesthesia, specifically designed to eliminate this pain and prevent discomfort during the treatment. Think of it this way: you go to the dentist in pain, and the root canal is the process that *takes the pain away* by removing the source of the infection. While you might feel sensations like pressure or vibration from the instruments, you should not feel sharp pain during the actual cleaning and filling of the canals if the anaesthesia is adequate. Post-procedure soreness is common, similar to the discomfort you might feel after any dental work or minor surgery, but this is typically mild and manageable with over-the-counter pain relievers. It’s a temporary discomfort that pales in comparison to the constant, throbbing agony of an untreated infected tooth. The misconception that root canals are torturous is a relic of the past, perpetuated by old stories and pop culture references that don’t reflect the reality of today’s comfortable and efficient procedures. Your dentist’s primary goal during the treatment is to ensure you are completely numb and comfortable, turning what was once a feared experience into a relatively straightforward process focused on healing and pain relief. Trust the anaesthesia; it’s the key to a comfortable experience.
How much does a root canal hurt on a scale of 1 to 10? Managing Expectations
During the procedure itself, with adequate local anaesthesia, most patients report pain levels between 0 and 2 on a scale of 1 to 10. You might feel pressure or vibration, but not sharp pain. Once the anaesthesia wears off, you may experience some mild to moderate soreness or discomfort, typically in the range of 3 to 5. This is normal and is usually due to inflammation in the tissues surrounding the root tip as they begin to heal after the infection has been removed. This post-operative pain is usually well-managed with over-the-counter pain relievers like ibuprofen or paracetamol. It’s generally comparable to the discomfort after a deep filling or tooth extraction, not the severe pain that necessitated the root canal in the first place. If you experience severe or worsening pain, it’s important to contact your dentist.
How long will the pain last after a root canal? Postoperative Comfort
Post-treatment soreness typically lasts for a few days to about a week. The discomfort should gradually decrease each day. This initial phase of mild pain or sensitivity is part of the normal healing process as the inflammation around the tooth subsides. Your dentist may recommend or prescribe pain medication to help manage this. It’s important to follow their instructions regarding pain management. If the pain is severe, doesn’t improve, or worsens after the first few days, it could indicate a complication, and you should contact your dentist immediately. However, for the vast majority of patients, the significant pain they experienced *before* the root canal is gone, replaced by only minor, temporary soreness.
What to Do After Your canal root treatment? Post-Treatment Care and Recovery
So, the hard part’s over (the infection, not the procedure!), and you’ve had your **canal root treatment**. Congratulations – you’ve taken a crucial step towards saving your tooth! But the journey isn’t quite finished. Proper post-treatment care is vital for a smooth recovery and, more importantly, for the long-term success of the procedure. Your tooth has been cleaned and sealed internally, but it’s still vulnerable, especially if it has a temporary filling. The tissues around the tooth need time to heal after the infection has been cleared. Following your dentist’s instructions regarding care, diet, and activity is non-negotiable for ensuring the tooth remains healthy and functional. This phase is about allowing your body to recover and preparing the tooth for its final restoration, which is a critical step to protect it from fracture and future contamination. Think of the root canal as successfully treating the ‘heart’ of the tooth; now you need to protect its ‘body’ with a proper restoration. Neglecting post-operative instructions or delaying the final restoration can jeopardise the success of the entire treatment, potentially leading to the need for retreatment or even extraction. Taking these steps seriously will help ensure that the tooth you saved with **canal root treatment** serves you well for many years to come, allowing you to eat, speak, and smile with confidence, knowing you’ve preserved your natural dentition through a combination of skilled treatment and diligent self-care.
How to care for your treated tooth immediately following the procedure
Right after the procedure, the area will likely still be numb from the local anaesthetic. It’s crucial to avoid eating or drinking anything hot until the numbness completely wears off to prevent accidentally burning or biting your lip, cheek, or tongue. Once the feeling returns, stick to soft foods for the first day or two. While the temporary filling provides a seal, it’s not as strong as a permanent restoration. Try to avoid chewing directly on the treated tooth, especially hard, sticky, or crunchy foods, until your permanent crown or filling is in place. You can brush and floss the tooth gently, but be careful around the temporary filling. Mild soreness is normal and can usually be managed with the pain relief recommended by your dentist.
What not to do after root canal treatment? Important Restrictions
Avoid chewing on the treated tooth until it has received its final permanent restoration (either a filling or typically a crown). Teeth that have had root canal treatment, especially molars and premolars, can be more brittle before they are crowned, making them susceptible to fracture from chewing forces. Resist the temptation to test the tooth’s strength. If your dentist advised against smoking or strenuous activity immediately after the procedure (sometimes recommended if sedation was used or if there was significant swelling), follow their guidance. Don’t neglect oral hygiene, but be gentle around the tooth initially. Avoid alcohol, particularly if you are taking prescription pain medication, as it can interact with the medication and potentially hinder healing.
Can I eat after a root canal? Dietary Considerations
Yes, you can eat after a root canal, but you need to be mindful of the treated tooth. It’s best to wait until the local anaesthetic has completely worn off to prevent biting your lip, cheek, or tongue. For the first few days, opt for soft foods like soup, yogurt, mashed potatoes, or smoothies. Critically, avoid chewing on the side of your mouth where the treated tooth is located, especially if it only has a temporary filling. The tooth is weaker at this stage and can easily fracture under chewing pressure. Once the tooth has received its permanent crown or filling, you can generally resume your normal diet, although caution with extremely hard foods is always wise.
What happens after a root canal treatment? Next Steps
The **canal root treatment** addresses the infection inside the tooth, but it’s only part of the overall process to restore the tooth’s full function and protection. A follow-up appointment is almost always necessary for the final restoration. This involves removing the temporary filling and placing a permanent filling or, more commonly, a crown. Molars and premolars, which absorb the most chewing force, almost always require a crown to prevent fracture. Front teeth might sometimes only need a filling, but a crown offers superior protection and is often recommended. This permanent restoration seals the tooth definitively and restores its strength and shape. After the final restoration, continue with good oral hygiene practices, including regular brushing and flossing, and attend routine dental check-ups. These steps are crucial for the long-term health and survival of your treated tooth and your overall oral health.
Benefits of canal root treatment: Why Save Your Tooth?
In the face of a compromised tooth, the options often boil down to two main paths: extraction (removing the tooth) or saving it through **canal root treatment**. While extraction might seem like a quicker, simpler fix on the surface, the long-term benefits of choosing root canal therapy to preserve your natural tooth are overwhelmingly significant. Saving your tooth maintains your natural bite, preventing the cascade of problems that can occur when a tooth is lost. When a tooth is extracted, the adjacent teeth can begin to shift into the gap, affecting your alignment, bite function, and potentially leading to jaw joint issues (TMJ). The opposing tooth in the other jaw can also drift or over-erupt into the space. Furthermore, bone loss naturally occurs in the area where a tooth is missing, which can affect the stability of neighbouring teeth and the potential for future tooth replacement options like implants. Saving your natural tooth with a root canal avoids all these domino effects. It allows you to continue chewing efficiently and comfortably, speaking clearly, and maintaining the natural aesthetics of your smile and face – your facial structure can be affected by missing teeth over time due to bone loss. Choosing **canal root treatment** means choosing to preserve the integrity of your mouth’s architecture. While extraction necessitates a future, often more expensive and involved, procedure to replace the tooth (like a bridge, implant, or partial denture) if you want to avoid the long-term consequences of a gap, a successfully treated and restored tooth can function normally for a lifetime. It’s a conservative approach that prioritises keeping what nature gave you, proving itself time and again as a durable and effective solution compared to the complexities and ongoing maintenance often associated with artificial replacements.
How does endodontic treatment save the tooth? Preserving Natural Structure
Endodontic treatment, or **canal root treatment**, saves the tooth by removing the infected or damaged tissue *from within*, rather than removing the entire tooth structure itself. The outer layers of the tooth – the enamel and dentin – and the root structure remain intact and anchored in the jawbone. By cleaning and sealing the internal root canal system, the source of infection is eliminated, allowing the surrounding tissues to heal. The tooth is then restored, typically with a filling and a crown, to protect the remaining structure and restore its function and strength. Essentially, the “shell” of the tooth, which is supported by the jawbone and gums, is preserved and made healthy again, allowing it to continue to function as a vital part of your dental arch.
What are the potential benefits of root canals? Overall Advantages
The primary benefits of **canal root treatment** include:
- **Pain Relief:** This is often the most immediate and significant benefit, as the procedure eliminates the source of pain (the infected pulp).
- **Saving the Natural Tooth:** Preserving your original tooth is almost always preferable to extraction and replacement.
- **Maintaining Normal Chewing and Sensation:** A saved tooth functions like any other tooth, allowing you to chew efficiently and maintain the feeling of having a full set of teeth.
- **Protecting Aesthetics:** Saving the tooth maintains your natural smile and facial structure.
- **Preventing Adjacent Teeth from Shifting:** Keeping the tooth in place prevents neighbouring teeth from drifting into the gap, which can affect your bite.
- **Cost-Effectiveness (often long-term):** While initial costs can vary, saving a tooth can often be less expensive over time than extraction followed by the cost of a bridge, implant, or denture and associated future maintenance.
Alternatives to canal root treatment: Is Extraction an Option?
When faced with a tooth requiring **canal root treatment**, the primary alternative is almost always extraction – simply removing the tooth entirely. While extraction might seem like a simpler, quicker, and potentially less expensive option in the short term, it’s crucial to understand the implications and consequences of choosing this path instead of saving the tooth. Extraction creates a gap in your smile and your bite, which, as we’ve discussed, can lead to a host of secondary problems like shifting teeth, bite changes, and bone loss in the jaw. To mitigate these issues, replacing the extracted tooth is usually recommended, which involves further procedures such as placing a dental implant (a surgical procedure to insert a titanium post into the jawbone, followed by placing a crown on top), a fixed bridge (which uses the adjacent teeth as anchors for a false tooth), or a removable partial denture. Each of these replacement options involves additional time, cost, and potentially more complex dental work down the line. While there might be rare cases where other, highly specific, or experimental regenerative procedures could theoretically be considered (often not widely available or proven long-term), for the vast majority of patients with infected or damaged pulp, the realistic clinical choice is between saving the tooth with a root canal or removing it. It’s a decision that shouldn’t be taken lightly, weighing the immediate relief of extraction against the long-term benefits and stability of preserving your natural tooth structure through **canal root treatment** and subsequent restoration. Discussing the pros and cons thoroughly with your dentist is essential to make the best decision for your specific circumstances, considering your oral health, overall health, and financial situation.
Is it better to have a root canal or extraction? Weighing the Options
From a dental health perspective, saving the natural tooth with **canal root treatment** is almost always the preferred option whenever possible. Natural teeth function better than artificial replacements and help preserve jawbone structure. Extraction creates a space that needs replacement, and each replacement option (bridge, implant, denture) has its own costs, maintenance requirements, and potential complications. A successfully treated and restored tooth can last a lifetime. However, in cases of severe tooth damage (extensive decay, large fractures) or significant bone loss supporting the tooth, extraction might be the only viable option if the tooth is deemed unrestorable. Cost can also be a factor, as the upfront expense of a root canal plus crown can sometimes be higher than a simple extraction, though it is often less than an extraction *plus* an implant or bridge. It’s a decision to be made in consultation with your dentist, considering the long-term prognosis and your individual circumstances.
Risks and Complications of canal root treatment
Like any medical or dental procedure, **canal root treatment**, while having a very high success rate (often exceeding 95%), isn’t entirely without potential risks or complications. It’s important to be aware of these possibilities, not to cause undue alarm, but to be informed and know what to look out for, however rare they may be. The vast majority of patients experience a smooth recovery with no significant issues. However, on occasion, challenges can arise. These might range from minor, temporary side effects to more significant complications requiring further treatment. Understanding these potential issues helps manage expectations and reinforces the importance of following post-treatment care instructions and attending follow-up appointments for the final restoration. Dentists and endodontists are highly trained to minimise these risks through meticulous technique, sterile procedures, and advanced equipment. For example, they use sophisticated imaging and instruments to navigate the complex anatomy of root canals, reducing the chance of procedural errors. Being informed about these potential, albeit uncommon, risks allows you to have a more productive conversation with your dental professional and feel more in control of your treatment journey. Remember, the goal of **canal root treatment** is to resolve a problem that, if left untreated, carries far greater and more certain risks, such as spreading infection, severe pain, and tooth loss. The risks associated with the procedure are generally low compared to the consequences of inaction.
Are there any side effects of root canal treatment? Potential Issues
While side effects are generally rare and mild, potential issues after **canal root treatment** can include:
- **Mild to moderate pain or soreness:** This is common for a few days as the surrounding tissues heal.
- **Swelling:** Some minor swelling in the gum area around the treated tooth can occur.
- **Sensitivity:** The tooth might be sensitive to biting pressure for a while.
- **Persistent infection:** In rare cases, despite thorough cleaning, some bacteria may remain or reinfection can occur, requiring retreatment or other procedures.
- **Instrument fracture:** Very rarely, a tiny file used to clean the canals can break off inside the canal. Often, these can be left safely or removed, but sometimes they can complicate treatment.
- **Tooth discoloration:** While less common with modern techniques, a treated tooth can sometimes darken over time. This can often be addressed cosmetically (internal bleaching, veneer, crown).
- **Perforation:** Creating an unintended opening through the side of the tooth root or pulp chamber during cleaning. This is rare but can complicate the tooth’s prognosis.
Can You Avoid canal root treatment? Prevention Strategies
Nobody *wants* to need a root canal. While some factors like trauma are unpredictable, many instances requiring **canal root treatment** are a direct result of preventable dental problems, primarily deep decay. This means that in many cases, with diligent effort and consistent dental care, you can significantly reduce your risk of ever needing this procedure. The path to avoiding root canals is fundamentally the same as the path to maintaining excellent overall oral health: proactive care and timely intervention when issues are small. It starts at home with the fundamentals of good hygiene, extends to regular check-ups with your dentist, and includes being mindful of your habits and protecting your teeth from injury. Thinking preventatively is key. Addressing cavities when they are small and manageable, before they have a chance to burrow deep enough to infect the pulp, is perhaps the single most effective strategy. It’s a classic case of an ounce of prevention being worth a pound of cure – or, in this case, potentially saving you from a root canal! Don’t wait for pain to be your only motivator for a dental visit. Regular check-ups allow your dentist to spot problems like early decay, cracks, or other vulnerabilities that could eventually lead to pulp damage before they escalate to the point of needing **canal root treatment**. Being proactive about your dental health isn’t just about keeping your smile looking good; it’s about preserving the health and structure of your teeth, potentially bypassing the need for more involved procedures down the line.
How to avoid a root canal? Preventative Steps
Here are the key strategies to reduce your risk of needing **canal root treatment**:
- **Maintain Excellent Oral Hygiene:** Brush your teeth twice a day with fluoride toothpaste and floss daily. This removes plaque and food particles, preventing decay from starting or progressing.
- **Regular Dental Check-ups and Cleanings:** Visit your dentist for routine examinations and professional cleanings. They can spot early signs of decay or cracks before they reach the pulp and provide preventative treatments like fluoride applications or sealants.
- **Get Cavities Treated Promptly:** If your dentist finds a cavity, get it filled as soon as possible. The longer you wait, the deeper the decay goes, increasing the risk of it reaching the pulp.
- **Protect Your Teeth from Injury:** Wear a mouthguard during contact sports or activities where there’s a risk of facial impact. Avoid chewing on hard objects like ice or popcorn kernels that could crack a tooth.
Can root canal heal naturally? Understanding Pulp Damage
No, once the dental pulp is infected or irreversibly damaged (due to decay or trauma), it cannot heal on its own. Unlike other tissues in the body, the pulp is enclosed within the rigid walls of the dentin and enamel, limiting its ability to swell and prohibiting effective blood flow and immune response to fight off infection. Bacteria within the confined space will continue to multiply, causing irreversible damage to the pulp tissue. At this point, the only options to resolve the issue and prevent further complications are either **canal root treatment** (removing the infected pulp) or extraction (removing the entire tooth). The body cannot clear this type of infection internally.
Infection and Antibiotics in canal root treatment
Infection plays a central role in why **canal root treatment** is often necessary. When bacteria infiltrate the dental pulp, they cause inflammation and infection within the confined space of the root canal system. This bacterial invasion is the source of the severe pain and swelling that often drives patients to seek emergency dental care. Understanding the relationship between infection and treatment is crucial for demystifying the role of antibiotics in this context. While antibiotics are powerful tools for fighting bacterial infections throughout the body, their effectiveness within the root canal system is limited. The reason for this is the compromised or non-existent blood supply within the infected pulp tissue. Antibiotics travel via the bloodstream to reach the site of infection. If the blood vessels in the pulp are damaged or destroyed by the infection, the antibiotics cannot effectively penetrate the area to kill the bacteria residing deep within the root canals. Therefore, antibiotics alone cannot cure an infection inside the root canal system. They might temporarily help manage swelling or prevent the spread of infection to surrounding tissues in some cases, particularly before definitive treatment, but they cannot eliminate the source of the bacteria within the tooth itself. The only way to truly eradicate the infection from within the tooth is through the mechanical process of **canal root treatment** – physically removing the infected pulp tissue, thoroughly cleaning and disinfecting the canals, and then sealing them off to prevent reinfection. Antibiotics might be prescribed *in conjunction* with a root canal in specific circumstances, such as if there is significant swelling extending beyond the tooth into facial tissues, or if the patient is medically compromised. However, they are an adjunct to the treatment, not a standalone cure.
Can antibiotics cure a root canal? The Role of Medication
No, antibiotics cannot permanently cure an infection inside the root canal system. While they can help control the spread of infection to surrounding tissues and may reduce swelling temporarily, they cannot reach the bacteria living within the tooth’s infected pulp due to the poor blood supply in the area. The only way to remove the source of the infection is through the physical cleaning and disinfection process of **canal root treatment**. Antibiotics might be prescribed *before* a root canal in cases of severe spreading infection (cellulitis), but they are a temporary measure and do not replace the need for the root canal procedure itself.
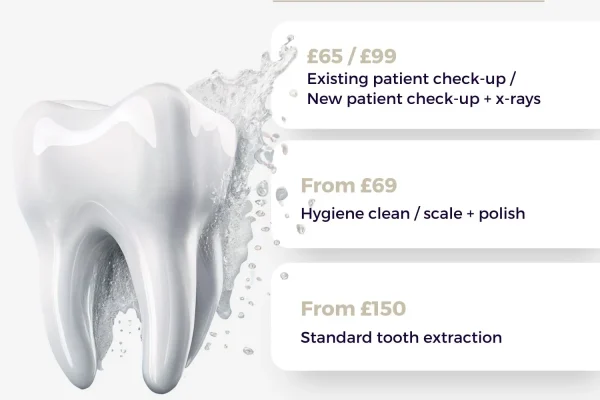
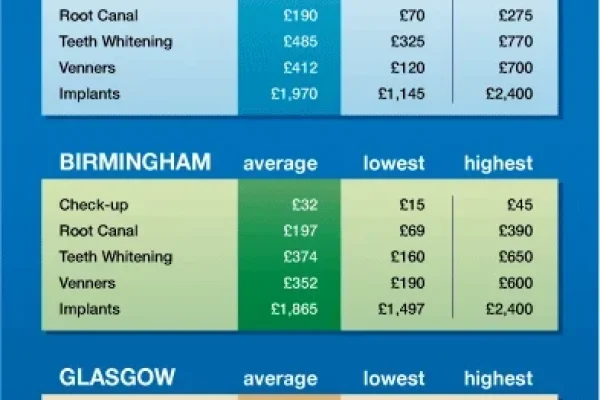
How Much Does canal root treatment Cost? Understanding the Investment
Let’s talk numbers, because cost is a legitimate consideration for any significant healthcare decision. The price tag associated with **canal root treatment** isn’t a fixed figure; it’s a variable that depends on several factors, primarily influenced by the complexity of the procedure, the location of the tooth in the mouth, your geographical location (costs vary significantly between regions and even within cities), and whether you see a general dentist or a specialist (an endodontist). Generally, front teeth (incisors and canines) are simpler procedures because they typically have only one root and one canal, making them less expensive. Premolars often have one or two canals. Molars, located at the back of the mouth, are usually the most complex because they have multiple roots (typically two or three) and three or more canals, which can be narrow, curved, or calcified, requiring more time, skill, and specialised equipment. This increased complexity directly impacts the cost. Seeing an endodontist, a specialist who has undergone additional years of training specifically in root canal procedures and uses advanced technology, may also incur a higher fee than a general dentist, but they are often recommended for complex cases due to their expertise and higher success rates in challenging situations. Dental insurance plays a significant role in the final out-of-pocket expense; coverage for endodontic procedures varies widely between plans, often covering a percentage of the cost. It’s crucial to check with your insurance provider beforehand to understand your benefits. While the initial cost might seem substantial, it’s essential to view it as an investment in saving your natural tooth. When comparing the cost of **canal root treatment** plus the necessary restoration (like a crown) to the alternative of extraction followed by a bridge or implant, saving the tooth often proves to be the more cost-effective solution in the long run, avoiding ongoing costs and potential complications associated with tooth replacement.
How much does a root canal cost? Pricing Factors
The cost of a root canal varies significantly but typically ranges from a few hundred to over a thousand dollars, and sometimes more for complex cases or specialist treatment. Key factors influencing the price include:
- **Tooth Location:** Front teeth (incisors/canines) are generally the least expensive. Premolars are mid-range. Molars are the most expensive due to complexity.
- **Severity of Infection:** More complex cases with extensive infection may require additional visits or procedures, increasing cost.
- **Practitioner:** Endodontists (specialists) typically charge more than general dentists.
- **Geography:** Costs vary based on the cost of living and dental practice overhead in your area.
- **Dental Insurance:** Your coverage level will significantly impact your out-of-pocket expense.
What is the cost of crown after root canal? Completing the Restoration
It’s crucial to understand that the cost of **canal root treatment** is separate from the cost of the final restoration, which is almost always necessary, especially for back teeth. The cost of a crown varies depending on the material used (porcelain, ceramic, metal, or a combination) and location, but it is a significant additional expense, often comparable to or exceeding the cost of the root canal itself. A filling is less expensive but is typically only suitable for front teeth with minimal structure loss. When budgeting for a root canal, it’s essential to factor in the cost of this subsequent restoration to get a clear picture of the total investment required to save and protect the tooth long-term.
Recovery Time After canal root treatment
One of the common questions after agreeing to **canal root treatment** is, “Okay, when can I get back to normal?” The good news is that the immediate recovery period is usually quite manageable, and most people can resume their regular activities fairly quickly. While the tooth might feel sensitive or sore for a few days as the tissues around the root tip heal from the inflammation and the removal of the infection, this discomfort is typically mild and temporary. Unlike major surgery, a root canal doesn’t require extensive downtime. Most patients report feeling well enough to return to work or school the day after the procedure. However, it’s wise to listen to your body and avoid strenuous activities if you feel the need to rest, particularly immediately following the appointment if you received any form of sedation. The *true* recovery of the tooth, in terms of restoring its full strength and function, occurs after the final restoration (usually a crown) is placed. Until then, the tooth is more vulnerable to fracture, which is why avoiding chewing on it is critical during this interim period. The goal is to allow the tooth and the surrounding bone and gum tissues to fully recover from the infection and the treatment process itself. While the internal cleaning is complete, the external healing process takes a little time. But rest assured, the period of significant post-operative discomfort is generally brief, paving the way for the long-term benefits of a healthy, functional tooth. It’s a relatively quick return to normalcy compared to the pain and limitations an infected tooth imposes.
How long does it take to recover from a root canal? Expected Timeline
Most patients feel comfortable resuming their normal daily activities, including work or school, the day after undergoing **canal root treatment**. You might experience mild soreness, tenderness, or sensitivity to biting pressure in the treated tooth for a few days up to about a week. This discomfort should progressively lessen each day and is usually easily managed with over-the-counter pain relievers recommended by your dentist. More significant pain or swelling beyond the first few days is uncommon and should be reported to your dentist. The full recovery process, including the placement of the permanent crown or filling, which is crucial for protecting the tooth long-term, happens in the weeks following the initial procedure. Once the final restoration is in place, the tooth is typically fully recovered and functional.
Specific Activities After canal root treatment
Beyond the general advice on managing discomfort and avoiding chewing on the treated tooth until its final restoration, patients often have specific questions about resuming certain daily activities. Can you travel? Can you talk normally? What about indulging in a drink or having a cigarette? These are valid concerns as you navigate the period immediately following your **canal root treatment**. While the procedure itself is generally not debilitating, certain activities should be approached with caution or temporarily avoided to ensure a smooth recovery and protect the tooth before its permanent shield (the crown or final filling) is in place. Your dentist will provide specific post-operative instructions tailored to your case, but addressing common questions can help clarify what’s usually permissible and what’s best to postpone. The focus is on preventing stress on the temporarily restored tooth and ensuring that any medication you might be taking works effectively without negative interactions. Understanding these nuances helps you take the best possible care of your newly treated tooth, allowing it to heal properly and be ready for its final, protective restoration. It’s about being mindful of the temporary vulnerability and giving your body the best chance to recover efficiently from the process of clearing the infection.
Can you drink alcohol after a root canal? Post-Procedure Restrictions
It’s generally advisable to avoid alcohol immediately after undergoing **canal root treatment**, especially if you have been prescribed pain medication. Alcohol can interact with certain pain relievers, potentially increasing their sedative effects or causing nausea. Furthermore, excessive alcohol consumption can potentially interfere with the body’s healing process and may thin the blood, which isn’t ideal after any procedure involving tissue manipulation. While a small amount might be permissible once you’re off pain medication and feeling well, it’s best to err on the side of caution and avoid alcohol for at least 24-48 hours, or as advised by your dentist.
What Happens if canal root treatment Fails? Addressing Retreatment
While **canal root treatment** boasts an impressively high success rate, typically over 95%, it’s important to acknowledge that, like any medical procedure, there’s a small possibility it might not be successful in every single case. Understanding *why* a root canal might fail and what options are available if it does is crucial information, however statistically unlikely it might be for you personally. Failure isn’t an immediate disaster; it’s a challenge that can often be addressed with further intervention, most commonly a procedure known as retreatment. The reasons for failure can be varied. Sometimes, the tooth’s anatomy is extraordinarily complex with narrow or unusually shaped canals that were difficult to fully clean during the initial procedure. Other times, a new infection can develop if the tooth’s permanent restoration (crown or filling) leaks, allowing bacteria to re-enter the treated canals. A fractured tooth or root can also compromise the success of the initial treatment. Even if a root canal fails, it doesn’t automatically mean the tooth is lost. Endodontists and experienced general dentists have advanced techniques and tools to attempt to save the tooth through retreatment, which is essentially performing the root canal procedure again, often addressing the specific reason for the initial failure. In some cases where retreatment isn’t feasible or successful, other surgical endodontic procedures, like an apicoectomy (removing the tip of the root and sealing the end), might be considered to save the tooth. The key takeaway is that a failed root canal isn’t necessarily the end of the road for your tooth; often, there are still viable options to preserve it.
Can a root canal fail? Understanding Outcomes
Yes, although rarely, a **canal root treatment** can fail. This can happen for several reasons, including:
- **Complex Canal Anatomy:** Some canals are too narrow, curved, or calcified to be completely cleaned and sealed during the initial procedure.
- **Incomplete Disinfection:** Despite best efforts, some bacteria may survive and cause persistent infection.
- **New Decay or Restoration Leakage:** If new decay forms around the tooth or the crown/filling develops a leak, bacteria can re-enter the treated canals.
- **Fractured Tooth or Root:** A crack in the tooth or root can allow bacteria to get into the treated area, or the fracture itself may make the tooth unsavable.
Root canal retreatment explained
**Root canal retreatment** is the process of repeating the endodontic procedure on a tooth where the initial treatment was unsuccessful. It involves reopening the tooth, carefully removing the existing filling material from the canals, and then recleaning and reshaping the canals to address any missed areas or new infection. The canals are then refilled and sealed. Retreatment is often more complex than the initial procedure because the canals have already been altered and might contain previous filling material or blockages. It requires significant skill and often the use of specialized equipment like a dental operating microscope. If retreatment is not possible or successful, surgical options like apicoectomy might be considered to save the tooth.
Caring for a Treated Tooth After canal root treatment: Long-Term Care
Getting through the **canal root treatment** and receiving the final restoration is a major victory for your tooth’s health, but it doesn’t mean you can forget about it entirely. A tooth that has undergone root canal therapy, like any other tooth in your mouth, still requires diligent, ongoing care to ensure its long-term survival and prevent future problems like decay or gum disease. The internal infection has been dealt with, but the tooth’s outer structure is still susceptible to the same issues that affect natural teeth. Think of it as saving the internal workings of a car; you still need to perform regular maintenance, like oil changes and tune-ups, to keep it running smoothly. For your treated tooth, this means maintaining excellent oral hygiene habits at home and continuing with regular professional dental care. The crown or permanent filling protects the tooth from reinfection via the biting surface, but the roots are still embedded in your gums and bone, and the tooth structure above the gum line can still get cavities if not properly cleaned. Your surrounding teeth are also vulnerable to decay and gum disease, which can eventually impact the support structure of your treated tooth. Therefore, incorporating the treated tooth into your daily brushing and flossing routine is essential. It’s not a special tooth that needs to be avoided; it needs to be cared for just like its neighbours. These ongoing practices, combined with regular check-ups and cleanings at your dentist’s office, are the best way to ensure that the tooth you invested in saving remains healthy, functional, and part of your smile for a lifetime.
How do you clean a canal tooth? Maintaining Oral Hygiene
You clean a tooth that has had **canal root treatment** exactly the same way you clean all your other natural teeth: by brushing twice a day and flossing daily. Focus on gently brushing the tooth’s surface and around the gum line. Floss carefully between the treated tooth and its neighbours to remove plaque and food particles, just as you normally would. Pay particular attention to cleaning thoroughly around the crown or final filling. Maintaining excellent oral hygiene prevents new decay from forming on the tooth structure above the gum line and helps keep the surrounding gums and bone healthy, which are crucial for supporting the treated tooth long-term.
Patient Experience and Anxiety About canal root treatment
It’s perfectly understandable if the prospect of **canal root treatment** makes you feel a little nervous. The procedure has unfortunately been saddled with a legacy of fear and discomfort in the public consciousness. However, it’s important to recognise that much of this anxiety stems from outdated information and misconceptions rather than the reality of modern endodontic practice. Dentists and endodontists today are acutely aware of patient comfort and employ techniques and technologies specifically designed to minimise pain and stress. Effective local anaesthesia is paramount, ensuring that the area is completely numb before the procedure begins. The environment in a modern dental practice is also geared towards patient relaxation, often including amenities like music, TVs, and comfortable chairs. More importantly, the procedure is *designed* to eliminate the pain caused by the underlying infection, not to create new pain. For many patients, the relief they feel after the treatment, when the chronic ache or throbbing is gone, far outweighs any minor discomfort experienced during or after the procedure. Open communication with your dental team is key to managing any anxiety. Don’t hesitate to voice your fears, ask questions about what to expect, and discuss options like sedation if you have significant phobia. Knowing that your comfort is a priority and understanding the steps involved can significantly alleviate apprehension. Ultimately, undergoing **canal root treatment** is about resolving a painful problem and saving a valuable tooth, which should be a source of reassurance rather than dread. Modern care prioritises making this a tolerable, and often surprisingly comfortable, experience.
Should you be nervous for a root canal? Managing Fear
It’s natural to feel some apprehension about any dental procedure, and the outdated reputation of **canal root treatment** certainly doesn’t help. However, you should not feel *unduly* nervous. Modern techniques and the routine use of potent local anaesthesia mean that the procedure itself is typically painless. Many patients report that the discomfort they experienced *before* the root canal (from the infection) was far worse than anything felt during or immediately after the procedure. Frame it in your mind as a solution to pain, not a cause of it. Talking openly with your dentist about any fears you have is crucial; they can explain the process in detail, address your concerns, and discuss options like sedation if your anxiety is severe.
Restoration After canal root treatment: Why a Crown is Important
The **canal root treatment** itself successfully removes the infected pulp and seals the root canal system, addressing the internal problem. However, this is often only the first phase of fully restoring the tooth. Because the tooth’s internal structure (the pulp) has been removed, and often because the tooth had significant decay or a large filling necessitating the root canal in the first place, the remaining tooth structure above the gum line can be weakened. Furthermore, the access hole made in the crown of the tooth to perform the procedure also needs to be sealed permanently. Simply placing a filling in this access hole is often insufficient, especially for back teeth (molars and premolars) which bear the brunt of heavy chewing forces. These teeth are significantly more prone to fracture after a root canal if they are not properly protected. This is where the final restoration, typically a dental crown, becomes critically important. A crown is a custom-made cap that covers the entire visible portion of the tooth above the gum line. It acts like a protective shield, restoring the tooth’s strength, shape, and function while preventing bacteria from re-entering the treated root canal system. For molars and premolars, placing a crown after a root canal is almost always necessary to prevent fracture and ensure the long-term survival of the tooth. While front teeth might sometimes be adequately restored with a strong filling if there was minimal tooth structure loss, a crown still offers superior protection, especially if the tooth was significantly weakened. Skipping this crucial step of placing a permanent crown (or appropriate filling) after **canal root treatment** is a common reason for treatment failure or tooth loss down the line. It’s an essential investment to protect the tooth you’ve just saved and ensure it remains a functional part of your bite for years to come.
Do you need a crown after a root canal? Completing the Treatment
For molars and premolars (back teeth), a crown is almost always necessary after **canal root treatment**. These teeth withstand significant forces during chewing, and removing the pulp makes them more brittle and susceptible to fracture. A crown provides essential protection, restoring the tooth’s strength and preventing breakage. For front teeth (incisors and canines), which experience less chewing force, a large filling might sometimes suffice if there was minimal tooth structure loss. However, even for front teeth, a crown is often recommended, especially if the tooth was heavily restored or significantly weakened, as it offers the best long-term protection against fracture and leakage. Your dentist will assess the remaining tooth structure and recommend the most appropriate restoration for your specific tooth.
Who Performs canal root treatment? Dental Specialists
When you need **canal root treatment**, you might be treated by your general dentist or referred to a specialist. Both are qualified dental professionals, but their training and focus differ. General dentists are trained to perform a wide range of dental procedures, including preventative care, fillings, extractions, crowns, and often, routine root canal treatments. They are the primary care providers for most people’s oral health needs. However, root canal procedures can sometimes be quite complex, involving teeth with multiple roots, curved or narrow canals, or complicated anatomical variations. Severe infections, retreatment of previously failed root canals, or cases requiring surgical intervention also fall into the more complex category. For these more challenging situations, or simply because your general dentist prefers to refer patients for endodontic work, you might be sent to an endodontist. An endodontist is a dental specialist who has completed an additional two to three years of postgraduate training specifically focused on the diagnosis, causes, prevention, and treatment of diseases and injuries of the dental pulp and surrounding tissues. They are experts in performing root canal procedures and other related treatments, often using advanced techniques and specialized equipment like dental operating microscopes and 3D imaging to navigate complex cases successfully. Choosing between a general dentist and an endodontist for your **canal root treatment** depends on the complexity of your case and your general dentist’s preference and comfort level with the required procedure. For straightforward cases, a general dentist is perfectly capable. For challenging or re-treatment cases, a specialist often offers a higher level of expertise.
What kind of dentist does root canals? Specialists vs. General Dentists
**Canal root treatment** is performed by either a general dentist or a dental specialist called an endodontist. General dentists are trained in endodontics and routinely perform root canals, especially on teeth with simpler anatomy (like front teeth). An endodontist is a dentist who has completed advanced training specifically in diagnosing and treating problems related to the dental pulp and root canal system. They specialise in complex cases, retreatments, and surgical endodontics. Your general dentist will assess your situation and either perform the root canal themselves or refer you to an endodontist if your case is particularly complex or challenging.
Success Rate of canal root treatment: What to Expect
One of the most reassuring aspects of **canal root treatment** is its impressively high success rate. Despite its historical negative reputation, modern root canal therapy is a remarkably reliable procedure when performed correctly and followed by appropriate restoration. The goal is to save the tooth, eliminate infection, and restore it to full function, and statistics show that this goal is achieved the vast majority of the time. Success rates for initial root canal treatment are typically cited as being over 95%, and often even higher for cases handled by endodontists. This means that in over nine out of ten cases, the procedure successfully resolves the infection, the tooth becomes asymptomatic, and it remains a healthy, functional part of your mouth for many years. The long-term prognosis for a successfully treated tooth is excellent; with proper care (daily brushing, flossing, and regular dental check-ups) and a good final restoration (like a crown), a tooth that has had **canal root treatment** can often last a lifetime, just like any other natural tooth. Factors that influence the success rate include the initial condition of the tooth and surrounding bone, the complexity of the root canal anatomy, the dentist or endodontist’s skill and use of appropriate technology, and most critically, the timely placement of a proper permanent restoration (crown or filling) to protect the tooth from future leakage and fracture. While failure is a possibility, as discussed earlier, it is uncommon, and even then, options like retreatment or surgical intervention can often still save the tooth. The high success rate underscores that choosing **canal root treatment** is a reliable investment in preserving your natural smile.
How successful is root canal treatment? Outcome Statistics
**Canal root treatment** is highly successful. Success rates for initial treatments performed by general dentists are commonly cited as being above 90%, while for endodontists (specialists who handle more complex cases and use advanced equipment), rates often exceed 95%. A successfully treated tooth can last a lifetime with proper care and restoration. The success depends on factors such as the severity of the original infection, the complexity of the tooth’s anatomy, the quality of the root canal procedure, and the effectiveness of the final restoration (crown or filling) in preventing future bacterial entry.
Appearance and Nature of a Tooth After canal root treatment
Patients naturally wonder how their tooth will look and feel after undergoing **canal root treatment**. While the internal workings are changed, the goal is always to restore the tooth’s external appearance and functional nature as closely as possible to its original state. One common concern is whether the tooth will turn black or become discoloured. While historical cases, particularly involving older techniques or trauma, sometimes resulted in tooth darkening, modern endodontic methods have significantly reduced the incidence of noticeable discoloration. If it does occur, it’s often a greyish tinge rather than black and can frequently be addressed with cosmetic procedures. Another fundamental question relates to the tooth’s “liveliness” – does a root canal kill the tooth? As discussed earlier, it makes the tooth “non-vital” in the sense that the living pulp tissue (containing nerves and blood vessels that respond to stimuli like heat/cold) is removed. However, the tooth structure itself is still alive, nourished by the surrounding tissues (the periodontal ligament) that anchor it in the jawbone. This means the tooth is still supported, feels pressure when biting, and remains a functional part of your mouth, unlike an extracted tooth. The final appearance will depend heavily on the restoration used. A crown is designed to match the colour and shape of your other teeth, making the treated tooth blend seamlessly into your smile. Even a large filling is chosen to match the tooth’s shade. The tooth will look like a normal tooth and function like one too, allowing you to bite and chew effectively. The most noticeable change isn’t cosmetic (if properly restored) but rather the *lack* of the painful sensitivity you felt before treatment.
Will a tooth turn black after a root canal? Addressing Discoloration
Significant tooth discoloration (turning dark or black) after **canal root treatment** is less common with modern techniques than it used to be. When it does happen, it’s more often a greyish shade and can be caused by residual tissue, filling materials, or internal bleeding following trauma. If discoloration is a concern, especially for front teeth, there are cosmetic options available, including internal bleaching (bleaching the tooth from the inside), placing a veneer, or covering the tooth with a crown matched to your natural shade. Your dentist can discuss these options if discoloration occurs.
Does a root canal kill the tooth? Understanding “Dead” Tooth
Technically, yes, a **canal root treatment** makes the tooth non-vital or “dead” in the sense that the living pulp tissue (containing nerves and blood vessels) is removed. The tooth will no longer respond to hot or cold stimuli or feel pain signals originating from within the pulp chamber. However, the tooth structure itself, the enamel, dentin, cementum, and the periodontal ligament that connects the root to the jawbone, remain alive and are nourished by the surrounding tissues. So, while it lacks the internal “life” of the pulp, the tooth remains functional, anchored in the bone, and contributes to chewing and maintaining the integrity of your dental arch. It’s a preserved, functional structure, not a dead entity that will simply fall out.
Advanced Procedures Related to canal root treatment
While standard **canal root treatment**, performed through the crown of the tooth, successfully treats the vast majority of pulp infections and root canal issues, sometimes more complex or alternative endodontic procedures are required. These typically fall under the umbrella of surgical endodontics and are often performed by endodontists due to their specialised training. These procedures are considered when conventional non-surgical root canal treatment or retreatment is not possible, has failed, or when diagnosis requires accessing the root end directly. They represent a more advanced tier of endodontic care aimed at saving teeth that might otherwise need extraction. One of the most common surgical procedures is an apicoectomy, also known as root-end surgery. This involves making an incision in the gum tissue to expose the bone and the root tip. The infected tissue and the very end of the root tip are removed, and a small filling is placed in the end of the root canal to seal it. This is often done if infection persists at the root tip after a successful standard root canal or retreatment, or if there are anatomical complexities at the root end that cannot be addressed through the tooth’s crown. Other advanced procedures might include repair of root perforations or treatment of fractured roots. These surgical interventions highlight the lengths endodontics can go to preserve a natural tooth, demonstrating that the field extends beyond the standard non-surgical approach to tackle complex challenges and give teeth the best possible chance of survival when conventional methods is insufficient.
Can you fix a root canal without surgery? Non-Surgical vs. Surgical Options
Standard **canal root treatment** is considered a non-surgical procedure, as it is performed through the crown of the tooth without making incisions in the gum or bone. This is the most common approach. Surgical endodontic procedures, such as apicoectomy, are reserved for specific situations where non-surgical treatment isn’t possible, has failed, or when accessing the root tip is necessary for diagnosis or treatment of problems like persistent infection at the root end. While many root canal issues can be resolved non-surgically, surgical options provide a way to save teeth that cannot be treated or successfully retreated through conventional methods.
Can All Teeth Receive canal root treatment? Scope of Treatment
The great news is that the majority of teeth are candidates for **canal root treatment**, offering a pathway to saving them from extraction. This includes front teeth, premolars, and molars, regardless of whether they have one, two, or multiple roots and canals. Modern endodontic techniques are versatile and adaptable to the varying anatomy found throughout the mouth. However, there are certain situations where a tooth might unfortunately not be a suitable candidate for root canal therapy. These limitations typically arise when the tooth is too severely compromised to be saved or effectively restored. For instance, a tooth with extensive decay that has destroyed a significant portion of the structure above or below the gum line, leaving insufficient tooth remaining to support a crown, might be deemed unrestorable. Similarly, a tooth with a vertical root fracture (a crack running from the chewing surface down the root) often has a poor prognosis and cannot be effectively sealed, making it unsuitable for root canal treatment. Teeth with severe periodontal disease (gum disease) leading to significant bone loss around the roots may also not be good candidates because the tooth lacks adequate support in the jawbone, regardless of the condition of the pulp. While dentists and endodontists strive to save teeth whenever possible, they must also make realistic assessments based on the tooth’s overall condition and long-term prognosis. In such cases where **canal root treatment** is not feasible, extraction might be the only remaining option to address the infection and prevent further complications. Your dental professional will carefully evaluate your tooth’s condition, including examining X-rays and assessing bone support, to determine if root canal treatment is the right approach for you.
- Yes, most teeth can be treated endodontically, allowing them to be saved. This includes front teeth, premolars, and molars.
- However, a tooth might not be a candidate for **canal root treatment** if:
- It has insufficient tooth structure remaining due to extensive decay or fracture, making it unrestorable with a crown.
- It has a vertical root fracture that cannot be repaired or sealed.
- It has severe periodontal (gum) disease with significant bone loss, compromising the tooth’s support structure.
- The canals are completely blocked and cannot be accessed or cleaned (though this is rare with advanced techniques).
Your dentist will assess these factors to determine if saving the tooth via root canal is feasible and has a good long-term prognosis.
Frequently Asked Questions About canal root treatment
Navigating the world of dental procedures can bring up a lot of questions, especially when the procedure has a reputation, however undeserved, like **canal root treatment**. To wrap things up and provide quick answers to some of the most common queries, we’ve compiled a list of frequently asked questions. These questions touch upon the core aspects of the procedure that patients most often want clarified – from the fundamental definition and what happens during the appointment, to the concerns about pain and what comes after. Our aim throughout this guide has been to provide comprehensive, easy-to-understand information, cutting through the jargon and addressing the myths head-on. These FAQs serve as a quick reference point, revisiting the essential details we’ve covered in depth. Understanding the answers to these common questions can further empower you, ease any remaining worries, and prepare you for discussions with your dental team. Remember, informed patients are better equipped to make decisions about their health and feel more comfortable throughout their treatment journey. **Canal root treatment** is a powerful tool for saving teeth and eliminating pain, and feeling confident about the process is part of a positive outcome.
What is a Root Canal?
A “root canal” refers to the natural space inside the root of a tooth. **Canal root treatment**, or endodontic treatment, is the dental procedure to remove infected or inflamed pulp from within these canals, clean and disinfect the space, and then fill and seal it to save the tooth.
What Happens During a Root Canal Procedure?
During **canal root treatment**, the tooth is numbed with local anaesthesia. An opening is made in the crown to access the pulp. The infected pulp is removed, and the canals are cleaned, shaped, and disinfected. The canals are then filled with a material like gutta-percha and sealed. A temporary filling closes the opening.
Is it painful to have a root canal?
No, with modern techniques and effective local anaesthesia, **canal root treatment** is typically not painful. The procedure is designed to relieve the pain caused by the infection, not create new pain. You might feel pressure or vibration, but sharp pain should not occur during the treatment. Some mild soreness after the anaesthesia wears off is common but manageable with pain relievers.
What to do after root canal treatment?
After **canal root treatment**, avoid chewing on the treated tooth until your permanent crown or filling is placed. Follow your dentist’s instructions for pain management. Maintain excellent oral hygiene by brushing and flossing normally. Attend your follow-up appointment promptly for the final restoration, which is crucial for protecting the tooth long-term.
When might I need a root canal treatment?
You might need **canal root treatment** if the pulp inside your tooth becomes infected or inflamed, often due to deep decay, a crack, or trauma. Signs include severe or lingering toothache, sensitivity to hot/cold, swelling, or a pimple on the gums. Sometimes, there are no symptoms, and the need is identified during a dental check-up or on X-rays.