Table of Contents
ToggleKey Takeaways
- Bleeding gums are *not* normal and signal underlying inflammation or disease, most often gingivitis.
- Causes go beyond poor hygiene, including vitamin deficiencies (C & K), hormonal changes, medications, smoking, and systemic conditions like diabetes.
- Persistent bleeding can indicate serious gum disease (periodontitis), potentially leading to tooth loss and impacting overall health.
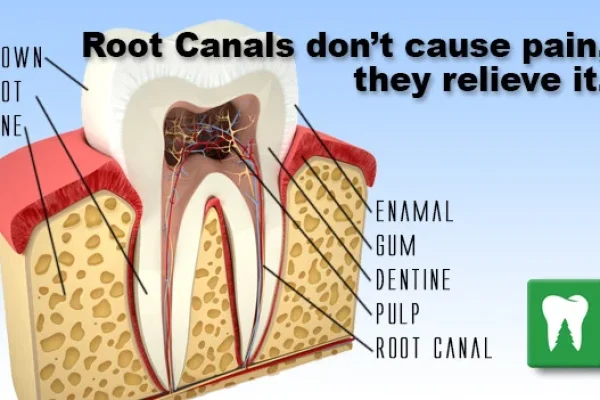
- Immediate remedies offer temporary relief, but long-term solutions require addressing the *root cause* through improved oral hygiene and professional care.
- Diligent daily brushing and flossing, regular dental check-ups, and a healthy lifestyle are key to preventing bleeding gums.
Why Are My Gums Bleeding, and What Does It Mean?
Spotting blood in the sink after you’ve brushed or, perhaps even more unnervingly, just finding it there seemingly out of nowhere, is rarely a cause for celebration. It’s a moment that prompts pause, a flicker of concern – *why* is this happening? Your gums, the soft, pink tissue enveloping the base of your teeth, are generally resilient. They should be firm, healthy, and *not* prone to spontaneous or even brush-induced bleeding. So, when they decide to make a crimson appearance, consider it a signal. Think of it less as a random inconvenience and more as your body’s highly efficient, if somewhat alarming, alert system sounding off. Bleeding gums, sometimes clinically referred to as bleeding gingiva, or simply gum bleeding, blood from gums, bleeding in gum, or bleeding gum, are a common issue, yes, but this prevalence doesn’t equate to normalcy. In fact, the phrase “normal bleeding gums” is a contradiction in terms. Healthy gums, vibrant and robust, do not bleed under routine circumstances like gentle brushing or flossing. Their bleeding is, almost without exception, an indicator of underlying irritation or disease. What does this signal usually point to? More often than not, it’s inflammation. The delicate tissues have become irritated, often by bacterial plaque, causing them to become sensitive, swollen, and fragile – thus, prone to bleeding even with minimal provocation. This initial inflammatory response is the body’s attempt to fight off the irritant. Understanding this fundamental principle – that bleeding is a *symptom*, not just a thing that happens – is the crucial first step in addressing the issue effectively. It shifts the focus from simply stopping the bleeding (which is often temporary) to identifying and tackling the root cause. It’s your gums sending a message, loud and clear: something needs attention.
What Causes Bleeding Gum Beyond Poor Brushing?
While it’s true that insufficient or improper brushing and flossing techniques leading to plaque buildup are the undisputed heavyweight champion of bleeding gum causes, the story doesn’t end there. Plaque, that sticky film of bacteria constantly forming on teeth, is the primary culprit, inciting gingivitis – the earliest, and thankfully, most reversible form of gum disease. If plaque isn’t meticulously removed, these bacteria irritate the gums, causing inflammation, redness, swelling, and, critically, bleeding. However, pinning *all* bleeding gum issues solely on a toothbrush technical foul would be an oversimplification. Several other dental conditions can contribute; for instance, infections or abscesses near the gum line, or even cavities progressing below the visible tooth surface, can cause localised irritation and bleeding. But the plot thickens when we consider systemic factors – issues originating elsewhere in the body that manifest in the mouth. Vitamin deficiencies, particularly deficiencies in Vitamin C (essential for collagen and tissue repair) and Vitamin K (vital for blood clotting), are well-established culprits. When asked, “What deficiency causes bleeding gums?” or “What vitamin deficiency causes bleeding gums?”, these two vitamins are high on the list. A severe lack of Vitamin C can lead to scurvy, historically infamous for causing widespread bleeding, including in the gums. Similarly, conditions affecting blood clotting, such as certain blood disorders or anemia-related bleeding gums, can also make gums more vulnerable. Beyond nutritional shortcomings, the body’s hormonal fluctuations play a significant role. Pregnancy, for example, often leads to “pregnancy gingivitis” where increased hormone levels amplify the gum’s inflammatory response to plaque, causing bleeding. Menopause, puberty, and even menstruation can have similar, though often less pronounced, effects. Medications are another factor; blood thinners, in particular, make bleeding more likely throughout the body, including the gums. Even seemingly unrelated health conditions like diabetes, leukaemia, or immune system disorders can impact gum health and contribute to bleeding. The question “Can stress cause bleeding gums?” often arises, and the answer is yes, indirectly. Chronic stress can weaken the immune system and contribute to inflammation throughout the body, potentially exacerbating gum issues. Sometimes, people report “gums bleeding for no reason,” but this is almost never the case; the reason might be subtle or undiagnosed, perhaps a hidden plaque buildup, an ill-fitting crown irritating the gum margin, or an early systemic sign. Exploring lists like “7 Causes of Bleeding Gums” often reveals this broader spectrum of potential triggers beyond just neglecting your toothbrush. Even factors like smoking significantly reduce blood flow to the gums, impairing their ability to heal and fight infection, leading to more severe gum disease and bleeding. Waking up with blood from your gums at night might be due to the same underlying inflammation, potentially worsened by mouth breathing or reduced saliva flow during sleep, allowing bacteria to thrive. It underscores that bleeding gums are a complex symptom with a diverse list of potential contributors.
Are Bleeding Gums Serious, and When Should You Worry?
Let’s cut to the chase: while a one-off instance of spotting pink on your toothbrush might be attributed to zealous brushing or perhaps a particularly sharp piece of food, persistent, frequent, or spontaneous gum bleeding is absolutely *not* something to shrug off. Healthy gums should be resilient enough to withstand the minor mechanical stress of proper oral hygiene without crying blood. So, the simple answer to “Is bleeding gums normal?” is a resounding no. Their bleeding is a flashing red light, a warning system indicating inflammation is present. And while gingivitis, the most common cause of this early bleeding, is reversible with diligent care, ignoring it is where the danger lies. This is where the question “Are bleeding gums serious?” becomes critical. Yes, they can be. Left untreated, gingivitis doesn’t just stay put; it can progress. The inflammation deepens, affecting the tissues and bone supporting the teeth – a condition known as periodontitis. This is a far more destructive disease, leading to gum recession, the formation of pockets between teeth and gums, bone loss, loose teeth, and eventually, tooth loss. This grim trajectory explains the serious risks of ignoring bleeding gums and clarifies “What happens if you don’t address bleeding gums?” It’s not just about losing a tooth; chronic inflammation in your mouth is increasingly linked to systemic health issues, a point we’ll touch on later. So, when should you genuinely start to worry about bleeding gums? Certainly, if the bleeding is persistent, occurring every time you brush or even spontaneously. Pay attention if the bleeding is accompanied by other concerning signs: redness, significant swelling, tenderness or pain (gums hurt bleeding, why is my teeth gum paining me?), gums pulling away from the teeth (recession), persistent bad breath or a bad taste in your mouth, changes in how your teeth fit together when you bite, or teeth that feel loose. These are all bad signs in gums, signalling that the inflammation may have progressed beyond early gingivitis. While minor mouth bleeding might seem trivial, if it originates from the gums and is ongoing, it warrants investigation. Resources like the NHS “Gum disease” pages or comprehensive guides such as “Periodontal Disease (Gum Disease): Everything You Need to Know” underscore that gum bleeding is the most visible symptom of a disease process that can have severe local and even systemic consequences if left unchecked. Don’t wait; persistent bleeding is your cue to seek professional advice.
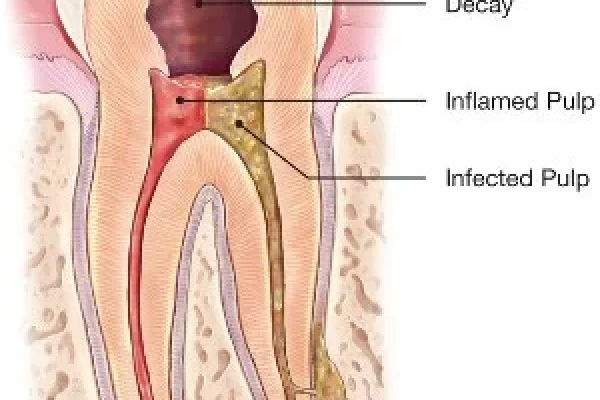
What Does Gum Disease Look Like and Feel Like?
Understanding what healthy gums *should* look like is the first step to identifying when something is amiss. Healthy gums are typically firm, pale pink, and fit snugly around your teeth, with a scalloped appearance. They don’t bleed easily when you brush or floss. In contrast, gum disease, particularly in its initial stage, gingivitis, presents a noticeable deviation from this healthy baseline. So, “What does stage 1 gum disease look like?” Often, the first visible signs are redness or a change in colour from that healthy pink to a deeper red or even purplish hue. The gums may appear swollen or puffy, losing their firm, tight appearance around the teeth. As inflammation takes hold, they become tender and are much more likely to bleed when touched, such as during brushing or flossing. This bleeding is often one of the earliest and most obvious symptoms, making it a critical warning sign. Many people might also notice bad breath or a persistent bad taste in their mouth, caused by the bacteria accumulating in the affected areas. While gingivitis itself might not always be painful, some individuals experience discomfort or mild tenderness (“gums hurt bleeding”, “why is my teeth gum paining me?” might be indicative of progressing inflammation or other issues alongside gum disease). The classic signs of Gum Disease and Symptoms of Gum Disease consistently list bleeding, redness, and swelling as primary indicators. If gingivitis is left untreated, it advances to periodontitis, the more severe form of gum disease. At this stage, the signs become more alarming. The gums may start to pull away from the teeth, creating pockets that become infected. Teeth may appear longer due as the gums recede. Pain becomes more common, often described as a dull ache or soreness. You might notice pus oozing from the gum line, a clear sign of infection. In advanced periodontitis, the bone supporting the teeth begins to erode, leading to loose teeth and changes in bite alignment. The visual changes become more pronounced – not just red and swollen, but potentially appearing visibly shrunken or damaged around the base of the teeth. So, what color are unhealthy gums? Typically red, swollen, sometimes shiny or stretched-looking, or even purplish in more severe inflammation, a stark contrast to the healthy pale pink. Recognising these visual cues and physical sensations is vital for seeking timely treatment before the disease causes irreversible damage.
How Can You Stop Bleeding Gums Immediately and in the Long Term?
When you see blood, the immediate instinct is simple: make it stop. Addressing how to stop gum bleeding immediately often involves practical, gentle measures aimed at controlling the current bleed. Rinsing your mouth gently with cool water or a mild saline solution (we’ll discuss salt water more later) can help clear away blood and debris. Applying gentle pressure with a clean piece of gauze might also temporarily staunch the flow if it’s from a specific spot. However, it’s crucial to understand that these are primarily first-aid steps to manage the *symptom* of bleeding. While useful in the moment, they don’t address *why* your gums are bleeding in the first place. Achieving a long-term cessation of bleeding requires tackling the underlying cause, which, as we’ve established, is most commonly inflammation driven by plaque and gum disease. So, when people ask “How do you cure bleeding gums?”, the answer isn’t a quick fix from a bottle or a simple rinse; it involves eliminating the source of the problem. Bleeding gums treatment encompasses a range of approaches, starting with improving daily oral hygiene to disrupt plaque buildup. Professional dental cleaning (scaling) is often necessary to remove hardened plaque (calculus) that home care can’t touch. In more advanced cases of gum disease, deeper cleaning procedures or even surgical interventions might be required to restore gum health. Think of it this way: stopping the bleeding *immediately* is like putting a bandage on a cut – it manages the wound. *Curing* the bleeding gums means healing the tissue so the cut doesn’t happen in the first place, which requires treating the infection or inflammation that made the tissue fragile. Various resources detail these methods, with titles like “How to Stop Bleeding Gums: 10 Methods to Try” often blending immediate tips with long-term strategies. For instance, improving your brushing technique and flossing regularly are fundamental *treatment* strategies because they remove the cause of the inflammation, thereby preventing future bleeding. Using an antiseptic mouthwash recommended by a dentist can also help reduce bacterial load. Addressing systemic factors, like getting nutritional deficiencies treated or managing conditions like diabetes, is also a vital part of the long-term solution. Ultimately, the most effective strategy for how to stop bleeding gums permanently isn’t just about applying something to stop the flow, but adopting consistent habits and seeking professional care to nurture your gums back to a state of health where bleeding is no longer a part of their story. How to treat bloody gums effectively is a combination of diligent self-care and professional intervention.
What Are Effective Home Remedies for Bleeding Gums?
When confronted with bleeding gums, many people first turn to their cupboards or pantries for a quick fix. Home remedies can offer temporary relief, reduce inflammation, and support overall oral health, acting as valuable complements to – but rarely replacements for – professional dental care, especially if gum disease has progressed. One of the most widely recommended and effective home-based approaches is rinsing with salt water. “Does salt water stop gum bleeding?” Yes, it can help. Saltwater acts as a mild antiseptic, helping to reduce bacteria in the mouth, and its osmotic properties can help reduce swelling in inflamed gum tissues, thus potentially lessening bleeding. The best home remedy for bleeding gums, in terms of widespread accessibility and evidence-based support for mild cases, is likely this warm salt water rinse, performed a few times a day. But “Can I rub salt on my gums?” is a different question, and generally, the answer is no. Applying dry salt directly can be abrasive and irritate the already sensitive tissues further; rinsing is the gentler, more effective method. Other natural agents are often explored. “Is turmeric good for bleeding gums?” Turmeric contains curcumin, a compound with potent anti-inflammatory and antioxidant properties. A paste made from turmeric and water or oil, applied gently to the gums, is sometimes used in traditional medicine to reduce inflammation, which can help with bleeding. “Does honey help gum disease?” Honey has natural antibacterial and anti-inflammatory properties, which could theoretically offer some benefit, but its high sugar content is a significant concern in an oral environment already battling bacteria. If used, it must be in small amounts and followed by thorough rinsing. “Does lemon stop bleeding gums?” This is generally ill-advised. While Vitamin C is crucial for gum health, applying acidic lemon juice directly to the gums and teeth can erode enamel and irritate soft tissues, causing more harm than good. Other remedies like applying cool, damp compresses or allowing a small ice cube to melt in the mouth (“Does ice stop gum bleeding?”) can help vasoconstriction and reduce immediate bleeding or swelling, similar to treating a minor injury elsewhere on the body. When considering “How can I treat gum disease without a dentist at home?”, it’s vital to be realistic. Excellent oral hygiene, healthy diet, and supportive home remedies can help manage *gingivitis* (early-stage gum disease) and prevent its onset. You *might* be able to reverse gum disease without a dentist if it’s just gingivitis, through stringent home care. However, established periodontitis, which involves damage below the gum line and bone loss, requires professional cleaning and treatment to halt its progression. Home remedies are best viewed as adjunctive care – ways to support professional treatment and maintain health, not cures for advanced disease. Looking at lists like “How to stop bleeding gums at home: 12 ways” can provide a broader range of safe, supportive methods.
How Does Oral Hygiene Affect Bleeding Gums?
Oral hygiene isn’t just about fresh breath and sparkling teeth; it’s the absolute cornerstone of gum health. The primary catalyst for gum inflammation and subsequent bleeding is dental plaque, a biofilm composed of bacteria that constantly forms on the surfaces of your teeth, especially along the gum line. These bacteria release toxins that irritate gum tissues. Your body’s immune response to these invaders causes inflammation, leading to the hallmark signs of gingivitis: redness, swelling, and crucially, bleeding. This is why scenarios like “bleeding gums when brushing,” “gums bleeding when brushing,” or simply “gums bleed brushing” are so incredibly common – the mechanical action of the brush, even if gentle, can trigger bleeding from tissue already made fragile by inflammation. However, this bleeding during brushing is a signal *not* to stop, but to *improve* your hygiene. Inadequate brushing leaves plaque behind, perpetuating the cycle of inflammation. Similarly, neglecting flossing allows plaque to accumulate between teeth, areas a toothbrush simply cannot reach effectively. This interdental plaque is a major contributor to gum disease and bleeding. Learning how to brush teeth properly involves angling the brush at a 45-degree angle towards the gum line, using gentle, circular strokes, and ensuring you cover all surfaces of every tooth, including the backs and chewing surfaces. The goal is to physically dislodge the plaque without causing trauma. Similarly, understanding how to correctly floss isn’t just about running a string between your teeth; it’s about guiding the floss gently between teeth and then curving it into a ‘C’ shape against one tooth, sliding it gently below the gum line to scrape away plaque, then repeating the process on the adjacent tooth. This action cleans the critical area where the tooth meets the gum. “Should I brush my gums?” Yes, gently brushing the gum line as part of your overall tooth cleaning process helps to remove plaque from this critical area and stimulates circulation. The key is consistency and technique. Regular, thorough removal of plaque through effective brushing twice a day and flossing once a day is the most potent weapon against gum disease and the most effective way to prevent and often reverse the bleeding associated with gingivitis. Improved oral hygiene reduces the bacterial load and inflammation, allowing the gum tissues to heal and become firm and healthy again.
Can Diet and Supplements Help Bleeding Gums?
You are, in many ways, what you eat, and that definitely extends to the health of your gums. Nutrition plays a significant supporting role in maintaining healthy oral tissues and bolstering your body’s ability to fight off infection and inflammation. Certain nutrients are particularly vital for gum health. Is vitamin C good for gums? Absolutely. Vitamin C is indispensable for the synthesis of collagen, a crucial protein that provides structural integrity to your gum tissues and blood vessels. It also acts as a powerful antioxidant, helping to protect cells from damage and supporting the immune system. A deficiency in Vitamin C weakens gum tissue, making it more susceptible to inflammation and bleeding – recalling our earlier point, “What vitamin deficiency causes bleeding gums?”. While Vitamin C is key, Vitamin K also plays a role due to its necessity in blood clotting. Ensuring adequate intake of both is important. How much Vitamin C to stop bleeding gums? There’s no magic number specifically for “stopping” bleeding (as that requires addressing the underlying cause), but ensuring you meet the recommended daily intake is foundational. Some sources suggest therapeutic doses might help the body heal, but supplementation should always be discussed with a healthcare provider. Focusing on incorporating Vitamin C-rich foods into your diet is a delicious strategy. What fruit is good for your gums? Citrus fruits (oranges, grapefruits), berries (strawberries, blueberries), kiwi, and even vegetables like bell peppers and broccoli are packed with Vitamin C. Crunchy fruits and vegetables can also help clean teeth naturally while you eat them. What drink is good for healing gums or what drink is good for bleeding gums? Water is always the best choice, helping to rinse away food particles and bacteria. Green tea contains antioxidants called catechins, which have been shown to reduce inflammation and fight oral bacteria, making it a beneficial beverage. Avoiding sugary and acidic drinks is crucial, as sugar feeds harmful bacteria and acid erodes enamel and can irritate gums. The question “Can lemon heal gums?” is problematic due to its high acidity; while it contains Vitamin C, direct application or consumption of large amounts of lemon juice can damage oral tissues. A balanced diet rich in vitamins, minerals, and antioxidants supports a robust immune system capable of fighting off gum infections and maintaining healthy connective tissue, providing a vital foundation for overcoming and preventing bleeding gums.
How Long Does It Take for Bleeding Gums to Improve?
Patience is a virtue, especially when coaxing inflamed tissues back to health. The timeframe for how long it takes for gums to stop bleeding isn’t a one-size-fits-all answer; it largely depends on the underlying cause, the severity of the condition, and, critically, the consistency and effectiveness of the treatment initiated. If the bleeding is primarily due to mild gingivitis caused by recent plaque buildup, you might see a significant improvement relatively quickly once you adopt a rigorous and proper oral hygiene routine (brushing twice daily, flossing daily). For many people, initiating this improved home care, sometimes combined with an antiseptic rinse or warm salt water rinses, can lead to a reduction or complete cessation of bleeding within a few days to a couple of weeks. Think of it as giving your gums the chance to recover once the constant irritation from plaque is removed. So, “How long does it take for gums to stop bleeding?” and “How many days does it take for gums to stop bleeding?” often have answers ranging from a few days to a week or two for early-stage, hygiene-related bleeding. However, if the bleeding is a symptom of more advanced gum disease (periodontitis), or if it’s linked to systemic health issues, medications, or other complex factors, the healing process will take longer and will almost certainly require professional dental intervention. A deep cleaning (scaling and root planing) might be necessary to remove hardened plaque and bacteria from below the gum line. After such a procedure, gums can take several weeks to heal and firm up, and occasional bleeding might still occur during this period. For other causes, like nutritional deficiencies, bleeding will likely subside only once the deficiency is corrected through diet or supplements, which also takes time. Healing cut gums from accidental trauma is usually a faster process, typically resolving within a few days with gentle care and keeping the area clean. The key takeaway is that if bleeding persists beyond a couple of weeks of diligent home care, it indicates the issue is likely more than just mild gingivitis and requires professional assessment to determine the cause and appropriate treatment plan. Don’t fall into the trap of thinking “How long can you go with bleeding gums?” is irrelevant; chronic bleeding signals ongoing disease that needs attention to prevent further damage.
What About Bleeding Gums in Specific Situations Like Pregnancy?
Life changes can sometimes throw unexpected curveballs, and your oral health isn’t immune. Bleeding gums can become particularly prominent during certain physiological shifts, and pregnancy is a classic example. Bleeding gums in pregnancy, often referred to as “pregnancy gingivitis,” is remarkably common, affecting up to 70% of expectant mothers. This isn’t necessarily because pregnant individuals suddenly neglect their oral hygiene; rather, the significant increase in hormone levels, particularly progesterone and estrogen, makes the gums more sensitive to the bacteria in plaque. This heightened sensitivity leads to an exaggerated inflammatory response, causing the gums to become red, swollen, and much more prone to bleeding, even with the smallest amount of plaque present. It’s the same bacteria, but the body’s reaction is amplified. While pregnancy gingivitis typically subsides after the baby is born and hormone levels return to normal, it’s crucial not to ignore it during pregnancy. Increased inflammation in the gums can still potentially progress to periodontitis, and there are studies suggesting a link between severe gum disease and adverse pregnancy outcomes, such as preterm birth and low birth weight. Therefore, maintaining excellent oral hygiene throughout pregnancy is paramount, including regular brushing, flossing, and attending scheduled dental check-ups (which are safe and recommended during pregnancy). Dentists can provide professional cleanings and advice tailored to expectant mothers. Beyond pregnancy, other hormonal shifts like puberty or menopause can sometimes make gums more sensitive. Starting new medications can also impact gum health or clotting ability, potentially leading to increased bleeding – it’s always wise to inform your dentist of any new prescriptions. Significant stress, as mentioned before, can also suppress the immune system and make you more vulnerable to inflammation, potentially exacerbating gum bleeding. Recognising that certain life events or medical changes can predispose you to gum bleeding allows you to be proactive and seek appropriate advice or ramp up your preventive care during these times.
How Can You Prevent Bleeding Gums in the First Place?
The good news is that, in most cases, bleeding gums are preventable. Since the vast majority of cases stem from plaque-induced gingivitis, the most effective prevention strategy centres on consistently removing plaque before it can cause significant irritation. So, “Can I prevent my gums from bleeding in the first place?” Yes, absolutely, through diligent daily care and regular professional check-ups. The core pillars of how to Prevent Bleeding Gums are surprisingly simple, though they require commitment. Firstly, and most importantly, master your oral hygiene routine. This means brushing your teeth thoroughly twice a day for two minutes each time, using fluoride toothpaste and a soft-bristled brush. Pay close attention to the gum line, using a gentle, angled motion. Secondly, flossing daily is non-negotiable. This removes plaque from the tight spaces between your teeth and under the gum line where your toothbrush cannot reach. It might cause slight bleeding initially if you already have gingivitis, but persevere – this action is crucial for healing. Learning the correct techniques for brushing and flossing is vital to clean effectively without causing trauma. Thirdly, regular dental check-ups and professional cleanings (usually every six months) are essential. Dentists and hygienists can remove hardened plaque (calculus) that you can’t remove at home, spot early signs of gum disease you might miss, and provide personalised advice on your oral hygiene routine. Can bleeding gums and dental bleeding be prevented? Yes, largely by controlling the factors that cause inflammation and trauma. Beyond daily hygiene, lifestyle choices play a significant role. A healthy diet, low in sugary and acidic foods and drinks, reduces the fuel source for harmful oral bacteria. Quitting smoking is one of the most impactful steps you can take for your gum health, as smoking severely impairs the gums’ ability to heal and fight infection. Managing stress can also indirectly support your immune system and overall health, benefiting your gums. Using therapeutic mouthwashes, as recommended by your dentist, can offer additional support by reducing bacterial load. Resources like “How To Treat & Prevent Bleeding Gums” or “Bleeding Gums: Causes, Prevention, and Treatments” consistently highlight this combination of diligent home care, healthy habits, and professional oversight as the golden standard for keeping your gums firm, pink, and blessedly blood-free. Prevention isn’t complicated, but it requires consistency.
Are Bleeding Gums Linked to Other Health Problems?
For decades, the mouth was often viewed in isolation from the rest of the body. However, modern medical science increasingly understands the profound and complex links between oral health and overall systemic health. Your gums, being highly vascular tissue with direct access to your bloodstream, can act as a gateway or a warning system for issues elsewhere. This connection elevates the question “Are bleeding gums serious?” beyond just oral implications. Chronic inflammation in the gums, particularly periodontitis, is no longer considered just a dental problem; it’s a chronic inflammatory disease that can have repercussions throughout the body. One of the most significant links is the potential impact on cardiovascular health. Studies have shown that people with gum disease have a higher risk of heart disease, stroke, and other cardiovascular events. “Can bleeding gums affect your heart?” While the exact mechanisms are still being researched, the prevailing theory is that bacteria from infected gums can enter the bloodstream, travel to other parts of the body, and contribute to inflammation and plaque buildup in arteries. The chronic inflammatory state associated with gum disease also releases inflammatory markers into the bloodstream, which can similarly impact systemic health. Beyond heart disease, gum disease has been linked to a range of other conditions. It can make it harder for people with diabetes to control their blood sugar levels, creating a bidirectional relationship where diabetes also makes individuals more susceptible to gum disease. There are also suspected links to respiratory diseases (through inhaling bacteria from the mouth), rheumatoid arthritis, kidney disease, certain cancers, and even cognitive decline. Complications of bleeding gums and dental bleeding, therefore, extend far beyond the risk of tooth loss. While gum bleeding itself isn’t directly causing these conditions, it’s a visible symptom of underlying inflammation and bacterial presence that can contribute to their development or worsening. This strong connection underscores why addressing bleeding gums and the underlying gum disease is not just about saving your teeth; it’s a crucial part of managing your overall health. Discussions around “Bleeding gums and your health” emphasise this holistic perspective. Your oral health is a vital component of your total well-being.
What Dental Products Are Best for Bleeding Gums?
Navigating the crowded aisles of the oral care section can feel overwhelming, especially when you’re looking for products specifically designed to help with bleeding gums. While no toothpaste or mouthwash is a standalone cure for advanced gum disease, the right products can significantly support your efforts to improve gum health, particularly when dealing with gingivitis or as part of a broader treatment plan for periodontitis. When considering “What’s the best toothpaste for gum disease?” or “Which toothpaste is best for bleeding gums?”, look for formulations specifically marketed for “gum health,” “gingivitis,” or “periodontal care.” These often contain ingredients aimed at reducing plaque and inflammation. Triclosan (though its use is becoming less common in some regions), stannous fluoride, or specific zinc compounds are examples of ingredients that can help reduce bacteria and inflammation. Toothpastes containing sensitive formulations might also be helpful if gum inflammation is causing discomfort during brushing, allowing you to clean more effectively without pain. As for mouthwash, “Which mouthwash is best for gum disease?” or “Mouthwash for Bleeding Gums,” antiseptic mouthwashes can be beneficial in reducing the bacterial load in the mouth. Ingredients like chlorhexidine (often prescription-strength for short-term use due to potential staining and altered taste), essential oils (like Listerine formulations), or cetylpyridinium chloride (CPC) can help kill bacteria that contribute to plaque and gingivitis. However, mouthwash should always be used *after* brushing and flossing, as it can’t physically remove plaque like mechanical cleaning can. It’s a supplemental tool, not a replacement. It’s also important to use an alcohol-free mouthwash if you experience dry mouth or sensitivity. A common question is “Can Sensodyne cure gum disease?” Sensodyne is primarily formulated to alleviate tooth sensitivity by blocking dentinal tubules. While good oral hygiene, which you can maintain using Sensodyne, is crucial for gum health, Sensodyne itself does not contain active ingredients specifically designed to cure gum disease. It can help manage sensitivity, allowing for better brushing, but it doesn’t treat the underlying infection or inflammation in the same way as an antiseptic or anti-plaque product. Always consult your dentist for personalised product recommendations based on your specific needs and the severity of your gum condition.
How Is the Cause of Bleeding Gums Diagnosed?
If you’re experiencing persistent or concerning gum bleeding, the path to effective treatment begins with a proper diagnosis by a dental professional. You might wonder, “How is the cause of bleeding gums or dental bleeding diagnosed?” It’s a systematic process that goes beyond a quick glance. Your dentist will start by taking a detailed medical history, asking about your oral hygiene habits, diet, any medications you’re taking, smoking habits, and any systemic health conditions you have (like diabetes, bleeding disorders, or hormonal changes like pregnancy), as these can all be contributing factors. They will then perform a thorough visual examination of your mouth, teeth, and gums, looking for signs like redness, swelling, recession, and the presence of plaque and calculus (hardened plaque). A key part of the diagnosis involves using a periodontal probe – a small, ruler-like instrument – to gently measure the depth of the pockets between your teeth and gums. In healthy gums, these pockets are typically shallow (1-3 mm). Deeper pockets indicate that the gum has pulled away from the tooth, a sign of periodontitis where bacteria can accumulate and cause further damage. Bleeding upon probing is a classic sign of inflammation and gum disease. The dentist will also check for tooth mobility, assess your bite, and examine the overall condition of your restorations (fillings, crowns, bridges) to ensure they aren’t contributing to irritation. Dental X-rays may also be taken to assess the health of the bone supporting your teeth and to identify any bone loss, which is a marker of periodontitis. Based on this comprehensive assessment – combining your history, visual examination, probing depth measurements, and X-rays – the dentist can accurately diagnose the cause and severity of your bleeding gums, determining if it’s simple gingivitis, more advanced periodontitis, or related to other local or systemic factors. This diagnosis is crucial for formulating the appropriate treatment plan.
What is Gum Infection, and How is it Treated?
The terms “gum disease” and “gum infection” are often used interchangeably, but it’s helpful to understand the nuance. Gum disease, in its initial stage (gingivitis), is primarily an inflammatory response to bacterial plaque. If left untreated, this inflammation can progress, and the condition becomes more accurately described as a gum *infection*, specifically periodontitis. Periodontitis is a serious bacterial infection that damages the soft tissues and bone supporting your teeth. Beyond bleeding, symptoms of gum infection can include persistent bad breath, a foul taste in the mouth, swollen and tender gums, gums pulling away from the teeth (recession), and the presence of pus between the teeth and gums. You might experience pain, leading to questions like “What is the best medicine for swollen gums?”. While over-the-counter pain relievers can help with discomfort, the “best medicine” for the swelling and pain of an infection is treating the infection itself. So, “What is the fastest way to heal a gum infection?” is not a single pill, but typically involves professional dental treatment to remove the bacteria and infected tissue. The primary treatment for periodontitis involves a deep cleaning procedure called scaling and root planing. Scaling removes plaque and calculus from above and below the gum line, while root planing smooths the tooth roots, making it harder for bacteria to reattach. This process effectively cleans out the infected pockets. In some cases, antibiotics (either oral or placed directly into the gum pockets) may be prescribed to help control the bacterial infection. For severe infections with extensive tissue or bone loss, surgical procedures may be necessary to reduce pocket depth, regenerate lost tissue or bone, or facilitate easier cleaning. While some might wonder “What drink kills bacteria in the mouth?”, such as antiseptic mouthwashes, these are adjuncts; mechanical removal of the bacteria and calculus through professional cleaning is paramount for treating an established infection. Addressing gum infection requires a multi-faceted approach, combining professional intervention to clear the infection with diligent home care to prevent its return.
How Is Gum Disease Treated Clinically?
Clinical treatment for gum disease focuses on removing the cause of the disease – the bacterial plaque and hardened calculus (tartar) – and restoring the gums to health. The specific treatment approach depends on the stage and severity of the disease, as diagnosed by your dentist. For gingivitis, the earliest stage where damage is not yet irreversible, clinical treatment primarily involves a standard professional dental cleaning. This procedure removes plaque and calculus from the tooth surfaces above the gum line. Coupled with improving your daily oral hygiene routine at home, this is usually sufficient to reverse gingivitis, allowing the gums to heal and the bleeding to stop. However, if gum disease has progressed to periodontitis, the treatment becomes more involved. The standard non-surgical treatment is called scaling and root planing, often referred to as a “deep cleaning.” This procedure goes below the gum line to remove plaque and calculus from the root surfaces. The roots are then planed (smoothed) to remove bacterial toxins and make it more difficult for plaque to accumulate again in the future. This process aims to reduce inflammation, shrink periodontal pockets, and encourage the gums to reattach to the tooth roots. Depending on the extent of the disease, this might be done over one or multiple appointments, sometimes with local anaesthesia for comfort. For more advanced cases of periodontitis with significant bone loss or deep pockets that cannot be effectively cleaned with scaling and root planing alone, surgical interventions may be necessary. These can include flap surgery (where the gums are lifted back to allow for easier access to clean the roots), bone grafting (to regenerate lost bone), or guided tissue regeneration (to help regrow gum tissue). The goal of these treatments is to reduce pocket depths, eliminate infection, and stabilise the teeth. Discussions around “Treatment for gum disease” or “Gum Disease Treatment | teeth.org.au” will detail these procedures. When you ask “How to fix unhealthy gum?”, this typically refers to these professional treatments designed to remove the source of the inflammation, allow the tissues to heal, and prevent further progression of the disease, restoring the gums to a healthier state where they are no longer red, swollen, or bleeding.
Frequently Asked Questions About gum bleeding
Navigating the world of oral health can bring up a lot of questions, particularly when faced with the unsettling sight of bleeding gums. Here are some common queries, answered directly.
Is bleeding gums serious?
Yes, persistent bleeding gums are a sign of inflammation and should be taken seriously. While occasional bleeding might occur from vigorous brushing, chronic or frequent bleeding is usually an indicator of gingivitis or more advanced gum disease (periodontitis), which can lead to tooth loss and has potential links to systemic health issues if left untreated. It’s your gums telling you something is wrong.
Why are my gums bleeding?
The most common reason is plaque buildup along the gum line, leading to inflammation known as gingivitis. However, other causes include hormonal changes (like during pregnancy), certain medications, nutritional deficiencies (especially Vitamins C and K), smoking, stress, ill-fitting dental appliances, or underlying systemic health conditions like diabetes or blood disorders.
How to stop bleeding gums?
Immediately, gentle rinsing with cool water or mild salt water can help. However, for a long-term solution, you must address the cause. This primarily involves improving your daily oral hygiene (proper brushing and flossing), getting professional dental cleanings to remove calculus, and addressing any underlying medical or lifestyle factors contributing to the issue.
What deficiency causes bleeding gums?
Deficiencies in Vitamin C and Vitamin K are most commonly associated with increased susceptibility to bleeding gums. Vitamin C is crucial for healthy connective tissue, and Vitamin K is essential for blood clotting. Severe deficiencies, though rare in developed countries, can significantly impact gum health.
How long does it take for gums to stop bleeding?
If the cause is mild gingivitis treated with improved oral hygiene, bleeding can often reduce or stop within a few days to two weeks. However, if the cause is more severe (periodontitis) or related to other health issues, it may take longer, require professional treatment (like deep cleaning), and healing time will vary depending on the intervention and individual healing capacity.
Gum bleeding is a signal. Don’t ignore it. Understand what your gums are telling you, take action with diligent care at home, and don’t hesitate to seek professional help. Your smile, and potentially your overall health, will thank you for it.