Table of Contents
ToggleKey Takeaways
- Gingivitis is inflammation of the gums, the earliest stage of gum disease.
- It’s primarily caused by bacterial plaque buildup due to insufficient oral hygiene.
- Common symptoms include red, swollen, and bleeding gums, often without pain.
- Gingivitis is highly treatable and reversible with professional cleaning and improved home care.
- Ignoring gingivitis can lead to periodontitis, an irreversible form of gum disease resulting in bone and tooth loss.
- Prevention relies on consistent brushing, flossing, and regular dental check-ups.
What is Gingivitis, and Why Should You Care?
Let’s cut to the chase: gingivitis is, quite simply, inflammation of the gums. Think of it as your body’s early warning system flashing red. It’s a remarkably common condition, often considered a mild form of gum disease, but don’t let ‘mild’ lull you into complacency. This isn’t some trivial annoyance; it’s the very first act in the potentially devastating play of periodontal disease. Catch it now, and you can rewind the clock. Ignore it, and you could be setting the stage for irreversible damage. It’s the kind of thing you might brush off (or, ironically, *not* brush off sufficiently), but it pays, massively, to understand its significance.
You might be wondering, “What can I expect if I have gingivitis?” Initially, perhaps not much that screams ’emergency’. Maybe a touch of redness around the gum line, a bit of puffiness, perhaps a metallic taste or a faint, unpleasant odour you can’t quite place. The real kicker, the undeniable sign for many, is seeing a little pink or red when you spit after brushing or flossing. That’s your gums telling you, in no uncertain terms, that something is amiss. It’s not normal for healthy gums to bleed. While gingivitis itself typically doesn’t cause the bone loss associated with more advanced gum disease (periodontitis), that bleeding is a clear signal of inflammation, and inflammation is the body’s distress call.
So, “Is gingivitis a serious problem?” In the grand scheme of oral health, yes, it’s significant. It’s serious because it’s the *precursor*. It’s the fork in the road. One path, taken with timely intervention and improved care, leads back to health. The other, paved with neglect, leads towards periodontitis – a condition where the inflammation spreads below the gum line, attacking the bone and connective tissues that hold your teeth in place. *That* is unequivocally serious, often leading to tooth loss. Gingivitis is your chance to act *before* you hit that irreversible point. Understanding it, respecting it, and addressing it means safeguarding not just your smile, but the very foundations of your teeth for years to come. Trust the experts on this one; the consensus across sources from academic deep dives like StatPearls and NCBI Bookshelf to trusted consumer guides like the MSD Manual and institutional wisdom from Mount Sinai is clear: gingivitis demands your attention.
What Causes Gingivitis and Increases Your Risk?
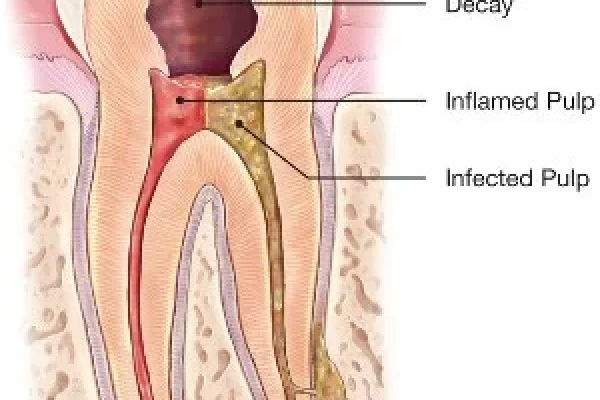
Alright, let’s unmask the primary culprit behind this gum-related drama. At its core, gingivitis is almost always instigated by one pervasive, insidious agent: **dental plaque**. This sticky, invisible film is a bustling metropolis of bacteria that constantly forms on your teeth. While some bacteria are harmless residents, others are decidedly less neighbourly. They feed on the sugars in the food particles left behind in your mouth, producing acids and, crucially for gingivitis, releasing toxins. These toxins are like tiny, inflammatory grenades tossed at your delicate gum tissues, triggering the characteristic redness, swelling, and bleeding. If plaque isn’t removed regularly through effective brushing and flossing, it hardens into calculus, or tartar, a substance so tenacious that no amount of brushing can remove it. Tartar provides a rough surface that attracts even more plaque, creating a vicious cycle that keeps the inflammation simmering. This is the most common origin story for gingivitis, a direct consequence of allowing the bacterial community on your teeth to flourish unchecked.
Beyond the ubiquitous plaque, however, several other factors can either directly cause gum inflammation (in cases classified as “Gingivitis Not Due to Plaque”) or significantly increase your susceptibility to the effects of plaque. It’s a complex interplay of your body’s internal state and external exposures.
What is the cause of gingivitis related to plaque?
As mentioned, the primary mechanism here is straightforward, albeit often overlooked in its simplicity: insufficient oral hygiene. When you don’t effectively brush and floss, that bacterial plaque isn’t removed. It accumulates, particularly along the gum line where the tooth meets the soft tissue. The bacteria within this plaque release toxins. Think of these toxins as highly irritating substances that provoke an immune response in your gums. This response is inflammation – the body’s attempt to deal with the perceived threat. This manifests as the redness, swelling, and increased fragility of the gum tissues, leading to easy bleeding. Over time, if this process continues, minerals from your saliva cause the plaque to calcify into hard calculus (tartar), which is impossible to remove with a toothbrush and acts as a constant irritant and a haven for more bacteria. This persistent irritation is the direct cause of plaque-induced gingivitis.
What deficiency causes gingivitis or increases risk?
While less common in developed countries today, certain nutritional deficiencies can absolutely play a role, sometimes causing forms of gingivitis not directly driven by plaque accumulation, or significantly worsening the gum’s response to plaque. The most classic example is a severe **Vitamin C deficiency**, which leads to scurvy. A hallmark symptom of scurvy is severe gingivitis, characterised by swollen, bleeding, and spongy gums. Vitamin C is crucial for collagen formation and immune function, both vital for healthy gum tissue. Similarly, deficiencies in B vitamins or other nutrients could potentially impact overall oral tissue health and resilience, though Vitamin C is the most direct link to deficiency-related gingivitis.
Can medications cause gingivitis?
Absolutely. Your body is a complex system, and medications, while addressing one issue, can sometimes have unintended consequences elsewhere. Several classes of drugs are known to affect gum tissue. Calcium channel blockers (used for heart conditions and high blood pressure), certain anti-seizure medications (like phenytoin), and immunosuppressants (like cyclosporine) can lead to a condition called gingival hyperplasia, or gum overgrowth. While not *strictly* gingivitis itself in terms of the initial cause being inflammation, this overgrowth makes it incredibly difficult to clean effectively around the teeth, trapping plaque and leading to secondary inflammation that *looks* and *acts* like gingivitis. Oral contraceptives and other hormonal therapies can also sometimes exaggerate the gum’s inflammatory response to plaque.
How do hormone changes affect gingivitis risk?
Hormones are powerful messengers in the body, and fluctuations in their levels can significantly impact gum health, making tissues more sensitive to plaque bacteria. This is why certain life stages are particularly associated with increased gingivitis risk. Puberty, for instance, sees a surge in hormones that can make adolescent gums more reactive. Pregnancy is another classic example; “pregnancy gingivitis” is common due to elevated hormone levels that cause increased blood flow and sensitivity in the gums, making them more prone to inflammation from even small amounts of plaque. Similarly, menopause can lead to changes in oral tissues, sometimes resulting in drier mouth or more sensitive gums. Managing oral hygiene diligently is especially critical during these hormonal shifts.
What are other causes and risk factors for gingivitis?
Beyond plaque, deficiencies, medications, and hormones, a range of other factors contribute to gingivitis or increase susceptibility. **Systemic diseases** like diabetes can impair the body’s ability to fight infection and heal, making individuals more vulnerable to gum inflammation and its progression. Leukemia, though rare, can cause a severe form of gingivitis characterized by swollen, bleeding gums due to the proliferation of abnormal white blood cells in the gum tissue. **Smoking and tobacco use** are major risk factors; they reduce blood flow to the gums, impair the immune response, and interfere with healing, significantly increasing the risk and severity of gum disease. Ill-fitting dental restorations (like crowns or fillings) or appliances (like braces or partial dentures) can create areas that trap plaque and are hard to clean. Even factors like **genetics** can play a role in an individual’s predisposition, and **age** generally increases risk as the cumulative effects of plaque exposure build up and systemic health issues become more common. Less common causes include specific **infections** (viral or fungal) or localized irritation, such as inflammation around a partially erupted wisdom tooth (**gingivitis due to an impacted tooth**, also known as pericoronitis). Understanding these diverse contributors highlights why managing gingivitis often requires a holistic view of your health.
How Does Gingivitis Look and Feel?
Stepping away from the causes, let’s talk about the tangible reality of gingivitis – what you actually see and sense when it sets in. This is where the abstract concept meets the physical manifestation in your mouth. Healthy gums are typically firm, pink, and hug the teeth snugly. They don’t bleed when you touch or brush them. Gingivitis changes that picture quite dramatically. The visual transformation is usually the first thing people notice, often catching a glimpse in the mirror while brushing. But the experience isn’t purely visual; there are tactile and even olfactory symptoms involved. Recognising these signs early is key to addressing the problem before it escalates.
The appearance can vary in severity depending on how long the inflammation has been present and other contributing factors. Initially, it might just be a subtle change, easily dismissed. But left unchecked, it becomes more pronounced, painting a clear picture of irritation and distress. The feel of your gums can also shift; they might become puffy or tender to the touch, a noticeable difference from their usual resilient texture. This combination of visual cues and physical sensations provides the crucial indicators that your gums need some serious attention.
What color are unhealthy gums affected by gingivitis?
This is one of the most telling visual signs. Healthy gums are typically a pale to medium pink colour, consistent throughout the mouth. When gingivitis takes hold, the colour shifts. The gums, especially along the edge right where they meet the teeth (the gum line), become noticeably redder. This redness can range from a bright, angry scarlet in early, acute inflammation to a deeper, more purplish-red hue in more chronic or severe cases. This change in colour is a direct result of the increased blood flow to the area as the body’s immune system responds to the bacterial toxins causing inflammation. So, if your gums are looking less like healthy pink flesh and more like an irritated, reddish border, gingivitis is highly likely.
What does stage 1 gingivitis look like?
In its earliest, most fundamental stage, often referred to simply as “initial gingivitis,” the visual signs might be quite subtle. You might see just a slight hint of redness or puffiness along the gum margin. The classic and often first noticeable *functional* symptom of stage 1 gingivitis, however, is **bleeding**. This bleeding typically occurs during mechanical action, like brushing or flossing. It might be just a tiny trace when you rinse, or more noticeable streaks in the sink. The gums might feel slightly tender or sensitive. At this stage, the inflammation is confined to the gingiva (the gums) and hasn’t yet started to affect the underlying bone or connective tissue. It’s reversible at this point, but its appearance is your body’s gentle nudge (or not so gentle, depending on the bleeding) that things are starting to go south.
Is gingivitis painful?
Surprisingly for many, simple gingivitis is often **painless**, particularly in its early stages. This lack of pain is part of what makes it insidious; you might have bleeding gums and chronic inflammation without experiencing any discomfort that prompts you to seek help immediately. Pain can develop, however, especially if the inflammation is more severe, if there’s accompanying infection, or if the gums are particularly swollen and tender from aggressive brushing or other irritation. When gingivitis progresses to periodontitis, pain is still not guaranteed, but abscesses or increased tooth sensitivity due to root exposure can cause significant discomfort. So, while pain isn’t a reliable early warning sign, *lack* of pain certainly doesn’t mean you don’t have gingivitis. Bleeding is a far more common and important indicator.
Does gingivitis smell?
Yes, it often does. One of the less pleasant symptoms associated with gingivitis is bad breath, or halitosis. This isn’t just standard morning breath. The bacteria that accumulate in the plaque and calculus causing the inflammation produce volatile sulfur compounds as byproducts of their metabolism. These compounds are the same ones responsible for the unpleasant odour. Furthermore, the inflammation itself can lead to the breakdown of tissues, adding to the bacterial load and the resulting smell. While bad breath can have many causes, persistent halitosis, especially when combined with bleeding or swollen gums, is a strong indicator that gingivitis (or more advanced gum disease) is present and contributing to the issue.
What are the signs and symptoms of gingivitis?
To summarise the key indicators, the signs and symptoms of gingivitis include:
- **Red or purplish gums:** A noticeable change from the healthy pink colour.
- **Swollen or puffy gums:** The gum tissue appears engorged.
- **Bleeding gums:** Occurring during brushing, flossing, or sometimes spontaneously. This is often the earliest and most common sign.
- **Tender gums:** Gums that are sore or sensitive to the touch.
- **Bad breath (halitosis):** A persistent unpleasant odour.
- **Receding gums (sometimes):** In some cases, chronic inflammation can lead to the gum tissue pulling away from the teeth, making the teeth appear longer.
- **Changes in how teeth fit together when biting (in later stages or periodontitis):** This is more characteristic of the progression to periodontitis.
It’s important to note the distinction between gingivitis and periodontitis symptoms (What are the symptoms of gingivitis and periodontitis?). While both involve inflamed gums, periodontitis is marked by additional, more severe signs: gum recession leading to visible tooth roots, the formation of pockets between the teeth and gums where infection thrives, loose teeth, changes in bite, and eventually, tooth loss. Gingivitis is the stage *before* these irreversible changes typically occur, making symptom recognition and early intervention crucial.
How Do You Get Rid of Gingivitis? Treatment Options
Right, you’ve identified the signs, understood the causes – now for the crucial part: how to fight back and reclaim your gum health. The good news, the really *excellent* news, is that gingivitis is highly treatable. This isn’t a life sentence for your gums. The path back to health involves a two-pronged attack: professional help and rigorous self-care. Neither is fully effective without the other, but together, they are a formidable force against gum inflammation. Think of the dental professional as clearing the major blockades, and your daily routine as maintaining the peace and preventing the enemy from regrouping.
The cornerstone of successful gingivitis treatment lies in the effective removal of the plaque and calculus that instigated the problem in the first place. You might be doing a decent job at home, but once plaque hardens into calculus, it’s impervious to your toothbrush and floss. That’s where the professionals come in, wielding specialised tools to perform a thorough cleaning above and below the gum line. This is typically a standard dental cleaning (prophylaxis), sometimes requiring ‘scaling’ if calculus buildup is significant. Once the irritant is removed, your gums get a fighting chance to heal. But the responsibility doesn’t end when you leave the dental chair; maintaining that healthy state becomes your daily mission. This dual approach is fundamental to getting rid of gingivitis and ensuring it doesn’t return or worsen.
Is gingivitis treatable, and can it be cured?
Let’s be crystal clear: **Yes, gingivitis is absolutely treatable and, in most cases, can be entirely reversed or ‘cured’.** The term ‘cured’ in this context means restoring your gums back to their healthy, non-inflamed state – pink, firm, and not bleeding. This is perhaps the most important takeaway about gingivitis. Unlike periodontitis, which involves irreversible loss of bone and connective tissue (and thus cannot be fully ‘cured’ in the sense of regrowing lost tissue, only managed), gingivitis is an inflammatory process in the soft tissue that *can* heal completely once the irritants are removed and good oral hygiene is established. Achieving this state requires prompt action and consistent effort, but the outcome is highly favourable.
How can I treat gingivitis at home initially?
Your home care routine is your first line of defense and a critical component of treatment. While professional cleaning is usually necessary to remove calculus, diligent home care is essential for removing the daily plaque buildup that fuels the inflammation. This means committing to a robust and effective brushing and flossing regimen.
- **Proper Brushing:** (How to brush gingivitis?) Brush your teeth twice a day for two minutes each time. Use a soft-bristled brush. Angle the brush at about 45 degrees towards the gum line, using gentle, circular motions or short back-and-forth strokes. Make sure you clean all surfaces of your teeth – outer, inner, and chewing surfaces. Pay particular attention to the gum line itself, as this is where plaque accumulates most readily. Don’t scrub aggressively, as this can further irritate already inflamed gums.
- **Daily Flossing:** Flossing is non-negotiable. It removes plaque and food particles from between your teeth and under the gum line, areas your toothbrush simply can’t reach. Gently slide the floss between your teeth, curving it into a ‘C’ shape against one tooth and sliding it gently below the gum line. Repeat this for the adjacent tooth. Do this at least once a day.
- **Mouthwash:** Using an antiseptic mouthwash recommended by your dentist can be a helpful adjunct to brushing and flossing. It can help reduce bacteria in the mouth and soothe inflammation, but it should never be seen as a substitute for mechanical cleaning.
What is the best toothpaste for gingivitis?
While no single toothpaste is a magic bullet, many are formulated with ingredients specifically aimed at controlling plaque and promoting gum health. Look for toothpastes containing fluoride (essential for strengthening enamel and protecting against cavities) and antibacterial agents like stannous fluoride or triclosan (though triclosan use is becoming less common in toothpaste). Some toothpastes marketed for “gum health” or “gingivitis control” contain these ingredients. Popular brands often have specific product lines for gum care. For instance, toothpastes from brands like Colgate (Is Colgate good for gingivitis?) or Sensodyne (Does Sensodyne cure gingivitis?), particularly those explicitly designed for gum health, often contain beneficial ingredients and can help reduce plaque and inflammation when used as part of a comprehensive oral hygiene routine. The “best” one for you might also come down to personal preference and any specific recommendations from your dentist.
Does salt water help gingivitis?
Yes, warm salt water rinses can offer temporary relief and support the healing process, but they are not a cure. Rinsing with warm salt water (dissolve about half a teaspoon of salt in a glass of warm water) can help soothe inflamed gum tissues, reduce swelling, and create an environment that is less hospitable to bacteria. It acts as a mild antiseptic and can help flush out debris. However, it does not remove plaque or calculus and therefore cannot resolve the underlying cause of gingivitis on its own. It’s a helpful supplementary treatment for symptom relief, particularly after professional cleaning, but it doesn’t replace brushing, flossing, or dental visits.
What is the best medicine or drugs for gingivitis?
For most cases of simple gingivitis, improved oral hygiene and professional cleaning are the primary treatments. ‘Medicine’ in the traditional sense (like antibiotics) is rarely the first-line approach. The most common prescription medication used is an **antiseptic mouthwash**, specifically one containing chlorhexidine gluconate. These are significantly stronger than over-the-counter washes and are often prescribed for short periods after professional cleaning to help manage bacterial load and reduce inflammation. However, they can stain teeth and affect taste with long-term use, so they are typically used under dental supervision.
Antibiotics (What is the best antibiotic for gingivitis?) are generally *not* needed for simple gingivitis. They are typically reserved for more severe gum infections, abscesses, or when gum disease is associated with specific systemic health conditions or aggressive forms of periodontitis. Using antibiotics for simple gingivitis is inappropriate and can contribute to antibiotic resistance. Creams or gels (What cream is good for gingivitis?) containing antiseptic or anti-inflammatory agents might occasionally be recommended by a dentist for targeted application in specific areas, but again, these are not a substitute for removing the cause (plaque/calculus). Always consult your dentist before using any prescribed medications for gum issues.
Can I treat gingivitis on my own, or can it heal naturally?
While improving your home oral hygiene is absolutely *essential* for treating gingivitis, relying *solely* on home care often isn’t sufficient, especially if calculus (hardened plaque) has formed. Calculus cannot be removed by brushing or flossing; it requires professional dental instruments (scaling). So, while diligent brushing and flossing are crucial for *preventing* gingivitis or managing very early, plaque-only stages, professional cleaning is usually necessary to effectively *treat* established gingivitis where calculus is present. Gingivitis generally will **not** simply “go away by itself” without intervention, either professional or a drastic improvement in home care that removes the daily plaque. It’s reversible, but it needs active treatment.
What is the best natural treatment for gingivitis?
The term “natural treatment” needs careful handling in the context of gingivitis. The most effective “natural” treatments are simply meticulous mechanical cleaning – brushing and flossing – as these are your body’s natural defense mechanisms (saliva, immune response) combined with physical removal of the irritant (plaque). However, some people look for complementary remedies. Options sometimes mentioned include rinses with diluted tea tree oil (known for its antiseptic properties), aloe vera, or specific herbal formulations designed for oral health. Salt water rinses, as discussed, are also a simple, natural option for soothing. It’s crucial to approach these with caution and, ideally, discuss them with your dentist. Many natural remedies lack robust scientific evidence, and some, like direct application of abrasive substances (Can baking soda cure gingivitis?) or acidic ones (Can lemon cure gingivitis?), can actually damage tooth enamel or gum tissues. They should never be used as a replacement for professional cleaning and established oral hygiene practices.
How to remove gingivitis quickly or cure gingivitis in a week?
Managing expectations is important here. While you can see significant improvement in symptoms relatively quickly with the right approach, achieving a complete ‘cure’ – meaning the gums are fully healthy and resilient again – depends on the severity of the initial inflammation and your consistency with home care. After a professional cleaning, the gums often begin to heal rapidly; redness and swelling can subside within days, and bleeding usually reduces dramatically or stops within a week or two of implementing excellent daily oral hygiene. So, while you might *notice* major improvements quickly, thinking of a complete ‘cure in a week’ might be overly ambitious. The process involves removing the cause professionally and then maintaining a high standard of cleaning *every single day* going forward. Diligent professional cleaning combined with immediate, consistent home care is the fastest route to recovery, but full tissue regeneration and resilience take a little more time.
Can You Reverse Gum Disease (Gingivitis)? Prognosis
Let’s get back to the heart of the good news: Gingivitis, as a stage of gum disease, is remarkably forgiving. Unlike its aggressive big sibling, periodontitis, the damage caused by gingivitis is confined to the soft tissues of the gums. It hasn’t yet attacked the bone and ligaments supporting your teeth. This crucial distinction means that yes, you absolutely *can* reverse it. Think of it as catching a cold before it turns into pneumonia. The symptoms are unpleasant, the body is fighting, but with the right care, you can make a full recovery, leaving no lasting damage. This potential for complete reversal is the most positive aspect of a gingivitis diagnosis and highlights why early detection and intervention are so vital. It offers a clear path back to health, provided you commit to the necessary steps.
Reversal means that the inflammation resolves completely. The redness disappears, the swelling goes down, the bleeding stops, and the gums return to their healthy, firm, pink state, tightly sealed around the teeth. The tissues regenerate to their original healthy form. There’s no lingering loss of support structure for the teeth. This favourable prognosis stands in stark contrast to periodontitis, where the damage to bone and connective tissue is permanent. While periodontitis can be managed to prevent further loss, the lost support cannot be naturally regained. Gingivitis, however, offers that reset button. It’s a powerful reminder that while gum disease can be serious, its initial phase is a wake-up call, not a final verdict.
How to reverse gum disease (Gingivitis)?
The roadmap to reversing gingivitis is clear and well-defined:
- **Professional Dental Cleaning:** This is typically the necessary first step, especially if calculus has formed. Your dentist or dental hygienist will perform scaling to meticulously remove plaque and tartar from the surfaces of your teeth, both above and below the gum line. This eliminates the primary source of irritation and inflammation.
- **Improved and Consistent Home Oral Hygiene:** This is where you take control daily. You must adopt and maintain a rigorous routine of brushing twice a day and flossing once a day, effectively removing the plaque that forms continuously. Using an antimicrobial mouthwash might also be recommended as an adjunct.
- **Addressing Contributing Factors:** If other issues are contributing (like ill-fitting restorations, smoking, or managing systemic conditions like diabetes), these need to be addressed alongside cleaning.
By removing the cause (plaque and calculus) and preventing its rapid return through diligent home care, the inflamed gum tissues can heal. The body’s natural healing processes take over once the chronic irritation is gone, allowing the gums to regain their healthy architecture and function. Consistency is key; reversing gingivitis isn’t a one-time fix, but a shift towards sustainable oral health habits.
Can gum disease be reversed entirely?
Yes, **gingivitis** (the early stage of gum disease) can be reversed entirely. The tissues affected (the gums) can heal back to their original healthy state. However, it is absolutely critical to understand the distinction between gingivitis and periodontitis. **Periodontitis** (the more advanced stage, where the infection has spread to the bone and supporting ligaments) cannot be reversed entirely. The bone and tissue loss that occurs in periodontitis is permanent. While treatment for periodontitis can stop or slow down the progression of the disease and manage the condition, it cannot regrow the lost support structures. So, when people ask “can gum disease be reversed?”, the answer is yes, *if* it’s caught at the gingivitis stage. Once it progresses to periodontitis, the focus shifts from reversal to management and prevention of further damage.
Is gingivitis permanent if left untreated?
Gingivitis itself is not permanent in the sense that the inflammation is *always* there at the same level. However, if left untreated, it is highly likely to progress. Think of it as an untreated infection. The body might try to fight it, but without removing the source (plaque/calculus), the battle is lost. Left unchecked, the chronic inflammation will gradually spread from the gums to the deeper supporting structures of the teeth – the periodontal ligaments and the alveolar bone. When this happens, the condition has progressed from gingivitis to periodontitis. Periodontitis *does* cause permanent damage (bone loss, tissue loss). So, while gingivitis isn’t *inherently* permanent as inflammation, its untreated state almost inevitably leads to the permanent damage characteristic of periodontitis. It’s the critical, reversible gateway. Ignoring it means accepting the high probability of progressing to irreversible problems.
How is Gingivitis Diagnosed?
Diagnosing gingivitis is a relatively straightforward process for a dental professional. It doesn’t typically require complex machinery or invasive procedures; it’s primarily based on a thorough clinical examination and a review of your medical and dental history. Your dentist or dental hygienist is trained to spot the often subtle (and sometimes not-so-subtle) signs that indicate your gums are not in optimal health. The process involves a visual inspection, careful probing, and a conversation about your symptoms and habits. This diagnostic step is crucial because while you might notice some signs at home, a professional can confirm the diagnosis, assess the severity, rule out other conditions, and formulate the most effective treatment plan tailored to your needs.
The initial step is usually a visual examination of your mouth. The dentist will look for the characteristic signs of inflammation in your gums: changes in colour (redness or purplish hues), swelling, and texture (they might appear puffy or less firm). They will also look for visible plaque and calculus buildup on your teeth. Part of the examination often involves gently assessing for bleeding. Even slight bleeding upon gentle touch or probing is a key indicator of gingivitis.
Next, they will likely use a small measuring tool called a periodontal probe. This probe is gently inserted into the space between your teeth and gums (the sulcus) to measure the depth. In healthy gums, this space is typically shallow (3mm or less) and there is no bleeding. In gingivitis, the inflammation can cause the gum tissue to swell, sometimes creating slightly deeper pockets, and the tissue will often bleed readily when gently probed. While deeper pocket depths (>4mm) are more indicative of periodontitis (where the attachment of the gum to the tooth has been lost), bleeding upon probing is a classic sign of active inflammation associated with gingivitis.
Finally, the dentist will review your medical history, asking about any systemic health conditions (like diabetes), medications you’re taking (as some can affect gum health), smoking habits, and your current oral hygiene routine. They might also ask about your diet. This information helps them identify potential contributing factors to your gingivitis and provides context for your treatment plan. Radiographs (X-rays) are typically not needed to diagnose gingivitis, as gingivitis does not involve bone loss, which is what X-rays primarily reveal in the context of gum disease. However, X-rays might be taken as part of a routine check-up or if there’s suspicion of underlying issues or progression to periodontitis. Based on this comprehensive assessment – the visual inspection, probing, and history review – your dentist can confidently diagnose gingivitis and recommend the appropriate course of action.
How Can I Reduce My Risk for Gingivitis? Prevention Tips
Knowing what causes gingivitis and how to treat it naturally leads to the question: how do you stop it from happening in the first place, or prevent it from coming back after treatment? The good news is that preventing gingivitis is largely within your control. It comes down to consistency, diligence, and smart habits. Think of it as laying down a robust defence system against the bacterial invaders trying to set up camp in your mouth. Prevention is not just about avoiding a health problem; it’s about maintaining comfort, confidence (no more worrying about bleeding or bad breath!), and protecting your long-term oral health investment – your teeth.
The core strategy revolves around keeping the bacterial plaque under control. Plaque forms continuously, so your preventative efforts need to be daily and thorough. It’s a constant, low-level battle that, when fought correctly, ensures your gums remain healthy and resilient. Beyond the daily grind, regular professional check-ups add an essential layer of protection, catching potential issues early and removing the stubborn stuff you can’t tackle at home. Lifestyle choices also play a significant role, either bolstering your defences or creating vulnerabilities. By focusing on these key areas, you can drastically reduce your risk of developing gingivitis and keep your smile in top condition.
What stops gingivitis from developing or returning?
The single most effective strategy to prevent gingivitis or stop it from returning after successful treatment is **consistent and effective plaque removal**. This is achieved through:
- **Brushing Twice Daily:** Using a fluoride toothpaste and a soft-bristled brush, clean all surfaces of your teeth thoroughly, paying close attention to the gum line. This physically removes the plaque before it has a chance to irritate your gums and harden into calculus.
- **Flossing Daily:** This is non-negotiable. Flossing removes plaque and food particles from the spaces between your teeth and under the gum line, areas inaccessible to a toothbrush. Skipping this step leaves significant amounts of plaque behind to wreak havoc.
- **Using Antiseptic Mouthwash (Optional but Helpful):** While not a substitute for brushing and flossing, rinsing with an antimicrobial mouthwash can help reduce the overall bacterial count in your mouth and provide additional protection, especially if recommended by your dentist.
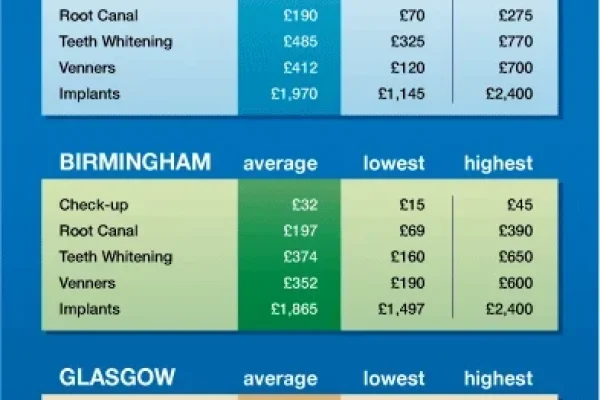
- **Attending Regular Dental Check-ups and Cleanings:** Visiting your dentist and hygienist for routine examinations and professional cleanings (typically every six months, or more often if recommended) is crucial. They can remove any calculus that has formed (which you can’t remove yourself), identify early signs of problems, and provide personalized advice on your oral hygiene technique.
- **Avoiding Smoking and Tobacco Products:** Tobacco use is a major risk factor for all forms of gum disease. Quitting significantly improves your gum health and ability to heal.
- **Managing Systemic Health Conditions:** Conditions like diabetes need to be well-controlled, as uncontrolled diabetes impairs immune function and increases susceptibility to infections, including gum disease.
- **Eating a Balanced Diet:** Limiting sugary snacks and drinks reduces the fuel source for plaque bacteria. A diet rich in vitamins and minerals supports overall tissue health.
By integrating these habits into your routine, you create an environment where gingivitis struggles to take hold.
What Organ is Affected by Gingivitis?
When we talk about gingivitis, we’re focusing specifically on one particular part of your anatomy. It’s a condition localized to a very specific type of tissue in your mouth. While poor oral health can have broader systemic implications over time, gingivitis itself directly targets the tissues that cradle your teeth. Understanding precisely which ‘organ’ is involved helps clarify the nature of the condition and why its effects are seen in the ways they are – the redness, swelling, and bleeding confined to this particular area.
This ‘organ’, in the context of gingivitis, is the **gingiva**, which is the medical term for your **gums**. The gingiva are the soft tissues that surround the base of your teeth, providing a protective seal and supporting structure around the roots. They are part of the periodontium, the complex set of tissues that anchor your teeth in your jawbone (which also includes the periodontal ligament and the alveolar bone). However, gingivitis is strictly limited to the *gingiva* itself. The inflammation affects the gum tissue but, by definition of gingivitis, has not yet spread to involve the deeper supporting structures like the bone. That progression marks the shift to periodontitis. So, if you’re wondering what specific part of your body is under attack with gingivitis, the answer is clear and confined: it’s your gums, the pink tissue hugging your teeth.
When Should I See a Dentist About Gingivitis?
Okay, so you’ve read through the signs and symptoms, understood the causes, and the question arises: when do you stop reading and pick up the phone to call the dentist? Given that gingivitis is often painless in its early stages, it’s easy to fall into the trap of thinking “it’s not bothering me, so it can wait.” This is a mistake. Timely intervention is perhaps the single most important factor in ensuring gingivitis is fully reversed and doesn’t progress to more serious, irreversible problems. Your dentist is your partner in oral health, equipped to accurately diagnose the issue and guide you toward recovery.
The simple, direct answer is: **as soon as you notice any signs or symptoms of gingivitis.** Don’t wait for pain. Don’t wait for the bleeding to get worse. Don’t assume it will go away on its own (because, as we’ve discussed, it typically won’t). Seeing red when you brush, noticing your gums look puffy or swollen, or experiencing persistent bad breath could all be indicators. These are your body’s early warning signals, and they are best heeded promptly. Ignoring them gives the inflammation more time to potentially spread deeper and cause lasting damage.
Furthermore, even if you don’t notice any specific symptoms, regular preventive dental check-ups are crucial. Most dentists recommend a check-up and professional cleaning every six months. These appointments allow the dental team to spot gingivitis (or other oral health issues) in its earliest, most treatable stage, often before you’ve even become aware of the symptoms yourself. They can remove the hardened plaque (calculus) that your home care can’t tackle and provide personalized advice to optimise your cleaning routine. So, if it’s been more than six months since your last visit, or if you’ve spotted any hint of those tell-tale gingivitis signs, it’s time to make that appointment. Early action is your best friend when it comes to keeping your gums healthy and reversing gingivitis. Don’t delay; your smile’s future depends on it.
What Age is Gingivitis Commonly Seen?
Gingivitis isn’t a condition that strictly targets one demographic. While some health issues are heavily skewed towards older age groups or specific populations, gum inflammation due to plaque can potentially affect almost anyone with teeth, regardless of how many birthdays they’ve celebrated. However, its prevalence does tend to shift across the lifespan, often becoming more common as individuals age, but certainly not excluding younger people. Understanding the age distribution helps reinforce that maintaining good oral hygiene is a lifelong commitment, not just something to worry about later in life.
While it’s less common in very young children (though possible, especially if hygiene is poor), gingivitis often begins to make an appearance during periods of hormonal change or when complex dentition makes cleaning more challenging. Adolescence is a time when hormonal fluctuations can increase susceptibility, and inconsistent hygiene habits might develop. As people move into adulthood, the cumulative effect of years of plaque exposure, combined with factors like stress, diet, smoking habits, or the development of systemic health conditions, increases the likelihood. Consequently, gingivitis becomes increasingly prevalent throughout adulthood.
However, it’s crucial to note that gingivitis can occur at **any age**. Infants with erupting teeth can experience localised gum irritation. Children and teenagers can develop gingivitis if oral hygiene is inadequate. Pregnant women often experience it due to hormonal changes. Older adults are at higher risk due to potential challenges with manual dexterity, certain medications, or dry mouth, in addition to cumulative plaque exposure. So, while statistics might show it’s more common in older populations, thinking of it solely as an “old person’s disease” is a mistake. It’s a condition tied primarily to the presence of plaque and the body’s response to it, which can manifest at any point in life if the right conditions are met. Regardless of your age, if you have teeth and gums, maintaining excellent oral hygiene is your best defense.
Frequently Asked Questions About gingivitis
Navigating the world of gingivitis can bring up a lot of questions. You’ve likely encountered the key information throughout this article, but sometimes, having concise answers to the most common queries can be incredibly helpful. Here are a few frequently asked questions, distilled for clarity.
- What is gingivitis disease?
Gingivitis disease is the medical term for inflammation of the gums (gingiva). It’s the mildest and earliest form of periodontal (gum) disease, typically caused by the accumulation of bacterial plaque on the teeth. It’s characterised by symptoms like **red, swollen, and bleeding gums**, but usually doesn’t involve pain in its early stages.
- What is gingivitis disease?
- Is gingivitis a serious problem?
Yes, gingivitis should be taken seriously, not because it causes immediate tooth loss (it usually doesn’t at this stage), but because it is the precursor to **periodontitis**. If left untreated, gingivitis is highly likely to progress to periodontitis, which *is* a serious problem involving **irreversible bone loss** and potentially leading to tooth loss. It’s serious because it’s a warning sign that requires attention to prevent future, more severe issues.
- Is gingivitis a serious problem?
- What causes gingivitis?
The primary cause of gingivitis is the accumulation of **bacterial plaque** on the teeth due to inadequate oral hygiene. Bacteria in the plaque release toxins that irritate the gums, causing inflammation. Other factors like smoking, hormonal changes, certain medications, nutritional deficiencies, and systemic diseases can also contribute or increase risk.
- What causes gingivitis?
- Is gingivitis treatable?
Absolutely! Gingivitis is **highly treatable** and, in most cases, completely **reversible**. Treatment typically involves professional dental cleaning to remove plaque and calculus, followed by consistent and improved daily home oral hygiene (brushing and flossing) to prevent plaque from building up again.
- Is gingivitis treatable?
- Can you reverse gum disease?
You can reverse **gingivitis**, which is the early stage of gum disease. The inflammation in the gums can heal completely, restoring them to a healthy state. However, once gum disease progresses to **periodontitis**, which involves irreversible bone and tissue loss, it cannot be fully reversed, only managed to prevent further destruction.