Table of Contents
ToggleKey Takeaways
- Gum disease progresses from reversible gingivitis to irreversible periodontitis.
- Gingivitis is curable with professional cleaning and improved home care.
- Periodontitis cannot be reversed but its progression can be stopped and managed.
- Effective treatment requires a combination of professional dental intervention and diligent home care.
- Daily brushing and flossing are the most critical “home remedies”.
- Some home remedies may offer supportive benefits, but should never replace professional treatment or core hygiene.
How to Cure Gum Disease: Exploring Treatment Options
So, you’ve landed here, likely wrestling with the uncomfortable reality of gum issues. Perhaps you’ve noticed your gums looking a little puffy, seen a faint pink when you spit after brushing, or maybe a dental professional has given you the news – you have gum disease. The immediate, burning question is, “How do I get rid of this?” or “Can you actually cure gum disease?” It’s a perfectly natural reaction, this desire to hit the ‘undo’ button and restore things to factory settings. But the truth, as is often the case with matters of the human body, is a touch more complex than a simple on/off switch. The term “curing” gum disease isn’t universally applicable, and its possibility hinges almost entirely on the specific stage of the condition you’re facing.
Think of gum disease not as a single, monolithic entity, but as a spectrum. At one end, you have gingivitis, the early, milder form, characterised primarily by inflammation of the gums (gingiva) – redness, swelling, and bleeding during brushing or flossing. This stage is essentially a warning shot, a clear signal from your body that something isn’t quite right with your oral hygiene routine. The good news, the really good news, is that gingivitis is, in fact, reversible. With timely intervention and dedicated effort, you absolutely can turn the tide and restore your gums to health.
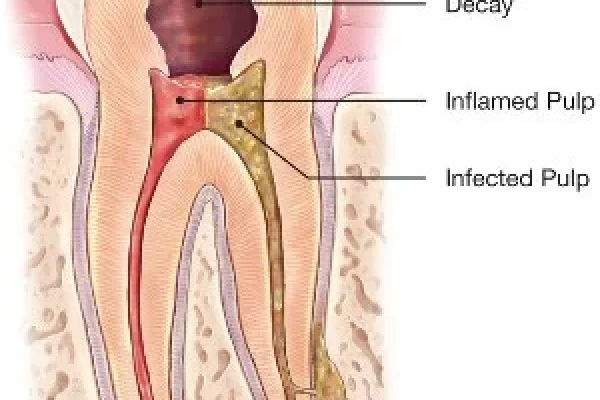
However, if this inflammation is ignored, if the bacterial assault continues unabated, it progresses. The infection begins to creep below the gumline, attacking the tissues and bone that support your teeth. This is periodontitis, the advanced stage. And this is where the conversation about “curing” becomes more nuanced. Periodontitis causes irreversible damage – the loss of bone and the formation of pockets between teeth and gums where bacteria can thrive unchallenged. You cannot, unfortunately, magically regrow the bone and tissue that has been destroyed by periodontitis. So, while you can’t technically “cure” periodontitis and bring the affected areas back to their original, pre-disease state, you can absolutely stop its progression, eliminate the active infection, and manage the condition effectively to prevent further loss and keep your teeth healthy for the long haul.
The path to tackling gum disease, regardless of stage, involves two fundamental, interconnected approaches: the essential work done by dental professionals and the absolutely critical, ongoing care you commit to at home. One without the other is like trying to bail out a leaky boat with a sieve – you won’t get very far. Professional treatment provides the necessary deep cleaning and, if needed, repairs to create an environment where healing is possible, while diligent home care is the daily patrol, preventing the bacterial invaders from re-establishing their foothold. Understanding this dual approach is the first, most vital step on your journey to healthier gums. This article will walk you through both sides of this equation, equipping you with the knowledge to not just treat, but effectively manage, gum disease.
Is Gum Disease Truly Curable? What You Need to Know
This is the million-dollar question, isn’t it? The one everyone asks when faced with a diagnosis of gum disease: “Can it be cured?” And as we touched upon, the answer isn’t a simple ‘yes’ or ‘no’; it’s a ‘sometimes,’ a ‘depends,’ and a ‘yes, but let’s define our terms.’ The crucial factor determining curability is the stage of the disease. Let’s break it down with clarity. The initial stage, gingivitis, is defined by inflammation of the gums caused by plaque buildup along the gumline. You might notice redness, swelling, tenderness, or bleeding when brushing or flossing. The key characteristic of gingivitis is that the damage is limited to the gum tissue itself. There is no irreversible loss of bone or connective tissue that holds your teeth in place.
Because the underlying support structures are still intact, gingivitis is, with appropriate and timely intervention, completely reversible. This means that by effectively removing the plaque and calculus (hardened plaque) that caused the inflammation, typically through professional cleaning and improved home hygiene, the gums can return to a healthy state – firm, pink, and non-bleeding. The inflammation subsides, and the signs and symptoms disappear. It’s a full recovery.
Now, enter periodontitis. This stage develops when gingivitis is left untreated. The bacterial infection spreads below the gumline, leading to inflammation and destruction of the deeper tissues that support the teeth, including the periodontal ligament and the alveolar bone. This is where things become irreversible. The bone and connective tissue that are lost to periodontitis do not naturally regenerate. You cannot simply reverse this damage and regrow what has been destroyed through standard cleaning or home care. Therefore, periodontitis is not considered “curable” in the sense of fully restoring the lost structures to their original state.
However – and this is a massive, significant ‘however’ – while the damage cannot be undone naturally, the active progression of periodontitis can be stopped and the condition can be effectively managed. Treatment for periodontitis focuses on eliminating the infection, reducing inflammation, shrinking the periodontal pockets (the spaces that form between the gum and tooth as the gum pulls away due to tissue loss), and preventing further bone and tissue loss. With successful treatment and vigilant ongoing maintenance, you can halt the disease process, stabilise the affected teeth, and preserve your smile.
So, to recap: gingivitis is reversible and effectively ‘curable’ with proper care. Periodontitis is not reversible in terms of regenerating lost support structures, but its progression can be stopped and the condition managed to prevent further damage. Understanding this fundamental difference is vital for setting realistic expectations and committing to the right course of action. It underscores the importance of early detection and intervention when gingivitis first appears.
Can Gum Disease Go Away or Repair Itself?
Let’s address this hopeful thought directly: can gum disease simply vanish on its own, perhaps with a bit of wishful thinking or just improved luck? The short, unvarnished answer is generally no. While the very earliest, mildest forms of gum inflammation might fluctuate slightly in severity day-to-day depending on food debris or temporary irritants, established gingivitis – the stage characterised by persistent redness, swelling, or bleeding – typically requires active intervention to resolve. Simply hoping it will go away is a gamble you don’t want to take, because the default trajectory for untreated gingivitis is progression, not spontaneous resolution.
Your body’s immune system is constantly battling the bacteria in your mouth, but the persistent presence of plaque and calculus along the gumline and below creates an environment where the bacteria have the upper hand. Without physical removal of this bacterial biofilm and calculus, the inflammation persists and the immune response becomes a chronic, destructive force. So, no, gingivitis doesn’t usually repair itself or disappear without dedicated effort in cleaning.
Now, let’s talk about advanced gum disease, periodontitis. Can this severe form repair itself? Absolutely not. Periodontitis is a destructive, progressive disease. The hallmark of periodontitis is the irreversible loss of the bone and ligament that hold your teeth in place. This lost support structure does not regenerate spontaneously. If periodontitis is left untreated, it will inexorably worsen over time. The bacterial infection continues its assault, the periodontal pockets deepen, more bone and tissue are lost, teeth may become loose, shift, or eventually require extraction. The inflammation often becomes more severe, potentially impacting your overall health. Think of it like erosion – once the soil is washed away, it doesn’t just magically reappear. The damage from periodontitis is cumulative and permanent.
This is why intervention at any stage is so critically important. For gingivitis, intervention means full reversal. For periodontitis, intervention means halting the destruction and saving what remains. The idea that either condition, particularly periodontitis, will somehow correct itself is a dangerous misconception that can lead to significant, irreparable harm to your oral health. Early detection and proactive treatment are not options; they are necessities to either reverse or effectively manage this condition.
Can You Get Rid of Periodontitis?
Okay, let’s get straight to the heart of it: “getting rid of” periodontitis. Based on what we’ve established about its irreversible nature, the phrase “get rid of” needs careful handling here. You can’t “get rid of” the damage that periodontitis has already caused. The bone and tissue that have been lost? They’re gone. The spaces that have formed between your gums and teeth (the periodontal pockets)? While they can often be reduced in depth through treatment, the underlying tissue loss remains. So, if by “get rid of,” you mean restoring everything to its pristine, pre-disease state as if it never happened, then no, you cannot “get rid of” periodontitis in that sense.
However, if by “get rid of,” you mean eliminating the active infection, stopping the progression of the disease, and establishing a stable, healthy environment in your mouth to prevent further destruction, then the answer is a resounding yes. Periodontitis, while causing permanent damage, is not an unstoppable force. With the right treatment and ongoing care, the bacterial assault can be neutralised, the inflammation calmed, and the disease process halted. The goal of treating periodontitis is to eliminate the bacteria residing in the deep periodontal pockets, remove the calcified plaque (calculus) that harbours them, reduce the pocket depth to make future cleaning manageable, and stabilise any loose teeth. This involves professional deep cleaning procedures (scaling and root planing), potentially surgical interventions to access deeper areas or repair damaged tissue, and a strict, lifelong commitment to enhanced home care and regular professional maintenance appointments. It’s less about ‘getting rid of’ and more about ‘taking control of.’
You are stopping the enemy in its tracks, clearing the battlefield, and then establishing a robust defence system to prevent them from regrouping and launching future attacks. While you live with the history of the damage (the lost bone/tissue), you don’t have to live with the active disease itself. You can achieve a state of periodontal health, where the infection is gone, the bleeding has stopped, and the gums are stable, even if they aren’t exactly as they were before the disease took hold. So, yes, you can eliminate the active disease process of periodontitis and prevent its return, but the physical remnants of its destruction remain. This is why terms like “managing periodontitis” or “stopping the progression of periodontitis” are more technically accurate and helpful than “getting rid of periodontitis.”
How Can I Treat Gum Disease? Professional & Home Approaches
So, you’ve got gum disease, or suspect you do. You understand the difference between gingivitis and periodontitis, and you know that action is required. The next logical question is, “Okay, what do I actually do?” The roadmap to treating gum disease effectively isn’t a single, straight line; it’s more of a two-lane highway, where both lanes are essential and lead to the same destination: improved oral health. On one lane, you have the crucial role of the dental professional – the dentist, the periodontist (a gum specialist), and the dental hygienist. These are the experts who have the tools, the training, and the knowledge to assess the severity of your condition, reach the areas you simply cannot access yourself, and perform procedures necessary to clean deep below the gumline and, if necessary, repair damaged tissues. Their intervention provides the foundational treatment, clearing out the bacterial strongholds that are driving the disease, particularly in cases of periodontitis where calculus has built up in deep pockets. Think of their work as the heavy artillery, necessary to dismantle the main enemy camps.
However, their work alone, no matter how expertly performed, is not enough to ensure long-term success. This brings us to the second, equally vital lane of the highway: your commitment to effective home care. This is where you become the daily patrol, the first line of defence. The bacteria that cause gum disease are constantly reproducing and forming new plaque biofilms. If you don’t consistently and effectively remove them through your daily routine, they will quickly repopulate the treated areas, and the disease process will reignite. Your home care routine is what maintains the healthy state achieved by professional treatment. It prevents gingivitis from developing or returning and keeps periodontitis under control, preventing further damage.
Neither the professional nor the home approach can succeed in isolation when dealing with anything beyond the very mildest, incipient gingivitis. Professional treatment creates the possibility of health by removing established irritants and infection in hard-to-reach areas. Home care actualises and sustains that health by preventing the build-up that causes the problem in the first place. This is why any guide on treating gum disease must meticulously cover both aspects, highlighting their distinct but complementary roles. The following sections will delve into the specifics of what happens in the dentist’s chair and, crucially, what needs to happen in your bathroom every single day.
How Do Dentists Treat Gum Disease?
Alright, let’s talk about the heavy lifting – what happens when you visit the professionals to tackle gum disease? Dental treatment for gum disease is highly tailored to the individual’s needs and the severity of their condition. For gingivitis, professional treatment is typically straightforward: a thorough cleaning, often called prophylaxis or a standard dental cleaning. During this visit, the dental hygienist or dentist will meticulously remove all plaque and calculus (hardened plaque) from the surfaces of your teeth, both above and just below the gumline. This eliminates the primary irritants causing the inflammation, allowing your gums to heal, provided you maintain good oral hygiene at home afterwards. It’s essentially resetting the clock and giving your gums a fresh start.
Now, for periodontitis, the treatment becomes more involved because the infection has spread deeper and caused more significant damage. The standard initial treatment for periodontitis is a procedure known as scaling and root planing (often referred to as a “deep cleaning”). This is a non-surgical treatment performed under local anaesthesia to ensure your comfort. Scaling involves scraping away plaque and calculus from the tooth surfaces and within the periodontal pockets below the gumline. Root planing follows, where the root surfaces are smoothed. This smoothing helps remove bacterial toxins and makes it harder for plaque to adhere in the future, creating a clean surface for the gums to potentially reattach to (or at least lie more closely against, reducing pocket depth). Scaling and root planing is a more extensive procedure than a standard cleaning and may require multiple appointments depending on the severity and extent of the disease.
Following scaling and root planing, the dentist or hygienist will typically recommend a schedule of regular maintenance cleanings, often more frequent than standard check-ups (e.g., every three to four months instead of six). These periodontal maintenance appointments are crucial for preventing the recurrence of periodontitis, as they allow the professional to clean those deeper areas again and monitor your gum health. In more advanced cases of periodontitis, where deep pockets persist or significant bone loss has occurred, surgical interventions may be necessary. These can include flap surgery (where the gums are lifted back to allow direct access to clean the roots and bone), bone grafting (to help regenerate lost bone structure), or tissue grafting (to cover exposed root surfaces and improve gum contour). The goal of these surgical procedures is to reduce pocket depth, make the area easier to clean, and in some cases, attempt to regenerate some of the lost support. Adjunctive therapies like local antibiotics placed directly into pockets or prescribed oral antibiotics might also be used in conjunction with scaling and root planing or surgery to help control bacterial infection. The dentist’s role is foundational: they tackle the entrenched infection and damage you cannot reach yourself, setting the stage for your home care efforts to be effective.
Can You Treat Gum Disease at Home?
This is a question often driven by a desire for convenience, perhaps a bit of anxiety about dental visits, or a hope for a quick fix. And the answer is, yes, absolutely – but with significant caveats, particularly if you’re dealing with periodontitis. For gingivitis, the early, reversible stage, dedicated and effective home care is the cornerstone of treatment and prevention. In many cases of mild gingivitis, simply improving your daily oral hygiene routine can indeed reverse the condition entirely. Brushing effectively twice a day, flossing diligently daily, and potentially using an antimicrobial mouthwash can remove the plaque that causes the inflammation, allowing the gums to heal. So, in the case of gingivitis, you can significantly treat – and often reverse – the condition at home through diligent self-care.
However, the landscape changes dramatically when we talk about periodontitis, the advanced form of gum disease. Once the infection has progressed below the gumline, leading to pocket formation and bone loss, home care alone is typically insufficient to eliminate the problem. Why? Because you simply cannot effectively clean deep into those periodontal pockets (spaces between the gum and tooth that are 4mm or deeper) with a toothbrush and floss. Calculus forms in these areas, which is hardened plaque that cannot be removed by brushing alone; it requires professional scaling instruments. While excellent home care is essential for managing periodontitis and preventing its return after professional treatment, it cannot cure the condition or reverse the damage once it has occurred. Relying solely on home remedies or increased brushing and flossing when you have established periodontitis is akin to trying to fix a leaking roof with a teacup – it might catch a few drips, but it won’t address the fundamental issue.
Think of home care for periodontitis as the crucial maintenance crew that keeps the facility running smoothly after the professional construction team has repaired the major structural damage. Without the initial repair (scaling and root planing, potentially surgery), the maintenance crew has an impossible job. Without the maintenance crew (your daily hygiene), the repaired facility will quickly fall back into disrepair. So, while you can treat gingivitis effectively at home, and home care is an indispensable part of managing periodontitis, you generally cannot treat established periodontitis alone at home and expect to halt its progression or reverse the damage. Gum disease self-care is powerful and necessary, but its efficacy is intrinsically linked to the stage of the disease and the partnership with professional dental care.
Treating Gum Disease at Home: Remedies and Self-Care
Alright, boots on the ground. The dental professionals have done their part – they’ve assessed, diagnosed, and perhaps performed a deep clean to remove the entrenched bacterial culprits. Now, the daily battle shifts to your home front. This is where consistency, technique, and the right tools make all the difference. Effective treatment and management of gum disease hinge enormously on what you do every single day, multiple times a day. Think of your mouth as a garden; the dentist can weed the really stubborn, deep-rooted invaders, but you need to tend it daily to keep new weeds (plaque) from taking over and to ensure the soil (gums and bone) stays healthy. This section is dedicated to equipping you with the knowledge and practical steps for winning that daily battle.
We’ll focus on the foundational pillars of oral hygiene, explore some of the popular ‘home remedies’ often discussed online (and scrutinise their actual effectiveness), and provide actionable advice for incorporating these practices seamlessly into your life. The goal isn’t just to ‘treat’ gum disease in the moment, but to establish a sustainable routine that keeps your gums healthy long-term, preventing recurrence or further progression. This involves mastering the basics of brushing and flossing, understanding how specific products like therapeutic mouthwashes can play a supportive role, and potentially looking at other aids like interdental brushes or water flossers that can reach areas traditional brushing misses. It’s about empowering you to be an active participant in your oral health journey. While the internet is awash with quick fixes and miracle cures, the reality of effective home treatment for gum disease boils down to diligent, informed, and consistent effort. We’ll navigate through the noise to highlight what truly works and why, ensuring you’re not wasting time or potentially causing harm with ineffective or risky practices. This is where the rubber meets the road in managing gum disease, transforming knowledge into action and paving the way for a healthier smile. Let’s dive into the practicalities and uncover the most effective home strategies.
What Home Remedies Help Gum Disease?
The term “home remedies” can encompass a wide range of practices, from established oral hygiene techniques to more unconventional natural substances. When discussing what home remedies “help” gum disease, it’s crucial to distinguish between fundamental, scientifically proven oral hygiene practices and supplementary or alternative methods that may offer some benefit but should never replace standard care. The absolute foundation of any home treatment plan for gum disease is diligent, effective brushing and flossing. These aren’t just routine tasks; they are the primary means by which you physically remove the bacterial plaque that causes gum disease. Brushing removes plaque from the tooth surfaces accessible by the brush, while flossing (or using other interdental cleaners) is essential for removing plaque from between the teeth and under the gumline, areas where a toothbrush simply cannot reach. Neglecting either of these makes the fight against gum disease significantly harder, if not impossible.
Beyond these non-negotiables, certain rinses are often cited as helpful. A simple salt water rinse is one of the most commonly recommended home remedies. While not a cure for established gum disease, warm salt water can help soothe inflamed tissues, reduce swelling, and create a less favourable environment for bacteria due to its mild antiseptic properties. It can be a helpful supportive measure, particularly after more intensive cleaning or if your gums are sore. Other substances sometimes mentioned include rinses with hydrogen peroxide (usually diluted), though caution is needed as overuse can be harmful, or certain essential oils found in some therapeutic mouthwashes (like tea tree oil or peppermint oil), which may have some antimicrobial effects. However, the efficacy and safety of using concentrated essential oils directly in the mouth is questionable and often risky; using commercially prepared, ADA-approved mouthwashes containing these ingredients is generally safer and more reliable.
Other remedies like using turmeric, coconut oil pulling, or certain herbal pastes are frequently discussed online. While some of these substances possess anti-inflammatory or antimicrobial properties in a lab setting, the scientific evidence supporting their effectiveness as standalone treatments for gum disease in humans is often limited, preliminary, or based on small studies. They should be viewed strictly as supplementary approaches, if used at all, and never as replacements for mechanical plaque removal (brushing and flossing) or professional dental treatment. The most effective “home remedies” are consistently good brushing and flossing, perhaps supported by an appropriate mouthwash and the occasional soothing salt water rinse. Anything else should be approached with caution and discussed with your dental professional.
How to Get Rid of Gum Disease at Home? Practical Steps
Okay, let’s translate the theory into action. How do you actually wage this daily war against gum disease from the comfort of your own bathroom? While, as we’ve discussed, you generally can’t “get rid of” periodontitis alone at home, you absolutely can reverse gingivitis and provide critical support for managing periodontitis through meticulous daily care. Here are the practical steps you need to embrace:
- Master Your Brushing Technique: It’s not just about putting toothpaste on a brush and moving it around. Use a soft-bristled brush (manual or electric). Angle the brush at 45 degrees towards the gumline. Use gentle, short strokes or small circles. Don’t scrub aggressively – this can damage gums. Brush all surfaces: outer, inner, and chewing surfaces of every tooth. Don’t forget to brush your tongue to remove bacteria causing bad breath. Aim for two minutes, twice a day. Electric toothbrushes, particularly those with oscillating or sonic action, can often be more effective at removing plaque than manual brushes for many people, but technique remains crucial.
- Floss Like Your Smile Depends On It (Because It Does): Brushing misses significant portions of your tooth surface – specifically, the sides where teeth touch. This is where floss comes in. Use about 18 inches of floss, wrapping most around one middle finger and the rest around the other. Hold it taut between your thumbs and index fingers. Guide it gently between your teeth using a back-and-forth motion. Once it reaches the gumline, curve the floss into a ‘C’ shape against one tooth and slide it gently into the space between the gum and tooth. Move the floss up and down several times against the side of the tooth, then repeat on the adjacent tooth. Don’t snap the floss – this can injure your gums. If traditional floss is difficult, try floss picks, interdental brushes (small brushes designed to clean between teeth, particularly effective if you have gaps or braces), or a water flosser (which uses a stream of water to remove debris and plaque). Whatever method you choose, consistency is key: do it at least once a day, ideally before brushing in the evening to dislodge particles that can then be brushed away.
- Consider a Therapeutic Mouthwash: Not all mouthwashes are created equal. Cosmetic rinses might freshen breath but do little for gum disease. Therapeutic mouthwashes, particularly those containing antimicrobial agents like chlorhexidine (often prescription-only for short-term use), cetylpyridinium chloride (CPC), or essential oils, can help reduce bacteria and inflammation as an adjunct to brushing and flossing. Follow the product instructions carefully, as some require rinsing for a specific duration or avoiding food/drink immediately afterwards. Crucially, mouthwash is a supplement to mechanical cleaning, not a replacement.
- Be Mindful of Your Diet: Sugary and starchy foods contribute to plaque formation. Reducing their frequency, especially between meals, can help. Drinking plenty of water can also help rinse away food particles and bacteria.
- Avoid Smoking: Smoking is a major risk factor for gum disease, significantly impairing blood flow to the gums and hindering healing. Quitting smoking is one of the most impactful steps you can take for your gum health.
Consistency and thoroughness are the watchwords. It takes dedication to make these steps a daily habit, but this daily commitment is the most powerful tool you have at home for preventing, reversing (gingivitis), or managing (periodontitis) gum disease. It’s about making your mouth a hostile environment for the bacteria that cause the problem.
What is the Fastest Way to Get Rid of a Gum Disease?
Ah, the quest for speed! We live in a world of instant gratification, and nobody wants to wait around when their gums are bleeding or sore. So, naturally, the question arises: what’s the quickest path to resolution? The answer, frustratingly for those seeking a magic bullet, depends heavily on which gum disease you’re dealing with and its severity. For gingivitis, the earliest and most reversible stage, the “fastest way” involves immediate, aggressive, and consistent intervention. This means scheduling a professional dental cleaning ASAP to remove the plaque and calculus driving the inflammation. Simultaneously, you must initiate and strictly adhere to an excellent home care routine: brushing thoroughly twice a day, flossing or using interdental cleaners daily, and potentially using a therapeutic mouthwash as recommended by your dentist. With this combined professional cleaning and dedicated home effort, you can often see significant improvement in gingivitis symptoms – reduced redness, swelling, and bleeding – within days to a couple of weeks. The gums can return to a healthy state relatively quickly because no irreversible damage has occurred. So, for gingivitis, the fastest way is prompt professional cleaning paired with rigorous, consistent home hygiene.
Now, let’s turn to periodontitis. If you have periodontitis, there is no “fast” way to “get rid of” it, because, as we’ve established, you cannot reverse the damage (lost bone and tissue). The process for treating periodontitis is about stopping the disease and managing it long-term. The initial phase of professional treatment, such as scaling and root planing, takes time (potentially multiple appointments) and healing follows over weeks and months. While the active infection can often be brought under control relatively quickly with professional intervention and initial healing might occur within a few weeks, achieving a stable, healthy state and preventing further damage requires ongoing vigilance. Periodontal maintenance appointments, typically every 3-4 months, become a necessary part of life. Therefore, for periodontitis, the concept of a “fastest way” to “get rid of” it is a misnomer. It’s a chronic condition that requires ongoing management. The fastest way to stop further damage is to seek professional treatment immediately upon diagnosis and commit to the recommended maintenance plan and home care routine. Trying to find a shortcut or a rapid home cure for periodontitis will inevitably lead to continued, irreversible damage. Focus instead on the most effective way, which is the combination of professional care and diligent home hygiene, understanding that this is a journey towards control, not a quick sprint towards complete reversal of all effects.
Specific Home Remedies: Salt Water, Turmeric, and More
Let’s zoom in on some of the popular contenders in the home remedy arena that often crop up in searches for gum disease treatment. While the fundamental pillars remain brushing and flossing, people are always curious about supplementary options.
Does Salt Water Help Gum Disease?
Yes, warm salt water rinses can be a helpful, simple, and often recommended supportive measure for gum health, particularly in the context of gum disease or after dental procedures. It’s important to understand what it helps with and what it doesn’t. Salt (sodium chloride) dissolved in water creates a mild antiseptic solution. Rinsing with this solution can help to reduce the bacterial load in the mouth, although it won’t remove the stubborn plaque and calculus adhered to the teeth and below the gumline (that requires mechanical action). More significantly, salt water is isotonic with your body’s tissues, meaning it has a similar salt concentration to your cells. This property, combined with the warmth, can help to soothe inflamed gum tissues, reduce swelling, and promote healing by drawing out excess fluid and potentially reducing irritation. It can be particularly comforting if your gums are sore or tender.
While a salt water rinse won’t cure periodontitis or replace professional cleanings and daily brushing/flossing, it can be a valuable adjunct for managing symptoms of gingivitis, supporting the healing process, and providing temporary relief from discomfort. How to use it? Dissolve about half a teaspoon of salt in a glass (8 ounces) of warm water. Swish the solution around your mouth for 30-60 seconds, focusing on getting it into the areas around your gums, and then spit it out. You can do this two or three times a day, especially after brushing. It’s a gentle, accessible remedy for temporary symptom relief and support, but keep those brushes and floss handy – they’re doing the real work.
Is Turmeric Good for Gum Health?
Turmeric, the vibrant yellow spice ubiquitous in Indian cuisine, contains a compound called curcumin, which has garnered significant attention for its potent anti-inflammatory and antioxidant properties. Given that gum disease is fundamentally an inflammatory condition driven by bacterial infection, the idea that turmeric or curcumin might help makes intuitive sense. And indeed, some preliminary studies and traditional practices suggest potential benefits. Curcumin’s anti-inflammatory action could theoretically help reduce the redness, swelling, and discomfort associated with gingivitis and periodontitis. Some research also indicates that curcumin possesses antimicrobial properties, which could help in the fight against the bacteria responsible for gum disease. Turmeric has been explored in various forms for oral health, including pastes made from turmeric powder and water applied directly to the gums, mouth rinses containing turmeric extract, or even taking curcumin supplements orally.
While these potential benefits are intriguing and warrant further robust scientific investigation, it’s crucial to view turmeric as a potential supplementary aid, not a primary treatment or cure for gum disease. The evidence from large-scale, high-quality clinical trials specifically demonstrating turmeric’s effectiveness as a standalone treatment for established gum disease is still limited. Applying abrasive pastes could potentially irritate delicate gum tissues. Relying on turmeric in place of professional dental care, diligent brushing, and flossing for treating gingivitis or periodontitis would be a significant mistake and could allow the disease to progress unchecked. If you’re interested in incorporating turmeric for its potential general health benefits, including potentially supportive effects on gum health, discuss it with your dental professional and healthcare provider. They can offer guidance on safe and effective ways to use it, ensuring it complements, rather than replaces, your essential dental care regimen.
What Natural Remedies Act Like Antibiotics for Gum Infection?
This is a particularly important area for clarity and caution. When people search for natural remedies that “act like antibiotics” for gum infections, they are often looking for ways to combat the bacterial component of gum disease, perhaps hoping to avoid conventional antibiotics or professional intervention. While many natural substances possess some degree of antimicrobial activity in a lab setting – meaning they can inhibit or kill bacteria under controlled conditions – this is vastly different from being a clinically effective antibiotic for treating a human infection, especially one as complex and entrenched as periodontitis below the gumline. Substances sometimes cited include tea tree oil, coconut oil (via oil pulling), certain herbal extracts like myrrh or bloodroot, or even garlic. While some research shows these have some effect on bacteria, their efficacy in the complex environment of the mouth, delivered in a way that can reach and eliminate the specific bacteria in periodontal pockets, is questionable and generally not supported by robust clinical evidence comparable to prescription antibiotics.
Crucially, relying on these natural substances as a substitute for prescribed antibiotics or professional dental treatment for an active gum infection, particularly periodontitis, is exceptionally dangerous. Undiagnosed or untreated gum infections can spread, lead to abscesses, cause significant bone loss, and even impact systemic health. Prescription antibiotics are powerful medications specifically formulated and delivered (systemically or locally) to target bacterial infections effectively and safely under medical supervision. Natural substances often lack the necessary potency, reliable concentration, ability to penetrate biofilms and tissues, or proper delivery mechanism to clear a significant infection. Furthermore, some natural substances can be toxic if used improperly (e.g., concentrated essential oils like tea tree oil must be heavily diluted and should never be swallowed) or can cause allergic reactions or irritation. The strongest “natural remedy” for preventing bacterial overgrowth in the mouth is the mechanical action of brushing and flossing to physically remove the bacteria. For established infections, particularly those causing periodontitis, always consult a dental professional. They can assess the need for antibiotics and provide the necessary treatment. Do not attempt to treat a significant gum infection solely with natural remedies; you risk serious complications and irreversible damage.
When Is It Too Late to Reverse Gum Disease? Understanding Severity
This is a fear many people harbour when they notice significant gum problems or receive a diagnosis of advanced disease: have I waited too long? Is the damage already irreparable? As we’ve discussed, the concept of “reversing” gum disease depends entirely on its stage. If you have gingivitis, it is virtually never too late to reverse it. Gingivitis is reversible by definition. As long as the underlying bone and supporting tissues are intact, eliminating the bacterial cause through professional cleaning and diligent home care will allow the gums to heal and return to a healthy state. So, if you have red, swollen, or bleeding gums but no significant bone loss or deep pockets, you are still firmly in the territory of full reversal.
The more challenging scenario arises with periodontitis. This is the stage where irreversible damage – the loss of bone and connective tissue – has occurred. When people ask if it’s “too late” for periodontitis, they often mean, “Is it too late to save my teeth?” or “Is it too late to get back to perfectly healthy gums?” Regarding the latter, yes, you cannot reverse the lost tissue. That damage is permanent. The spaces created by bone loss (periodontal pockets) and the gum recession are lasting reminders of the disease’s passage.
However, and this is critically important, it is almost never too late to treat periodontitis to halt its progression, save your remaining teeth, and improve your oral health significantly. Even in severe cases with extensive bone loss, treatment can still be highly effective at eliminating the active infection, stabilising loose teeth, reducing inflammation, and preventing further destruction. Treatment in advanced stages might involve more complex procedures, including surgery, but the goal is always to create a manageable environment where the disease cannot continue its destructive path. The signs of advanced periodontitis include significant gum recession (teeth looking longer), noticeable tooth looseness or shifting, persistent bad breath or taste, visible pus around the gums, and changes in your bite. If you are experiencing any of these, it signals that the disease is advanced, and while you cannot reverse the damage that has occurred up to that point, you can absolutely intervene to prevent it from getting worse and to save your remaining teeth. Waiting longer only increases the amount of irreversible damage. Therefore, while you might not be able to turn the clock back to a state of zero damage if you have periodontitis, it’s practically never too late to seek treatment and take control of the situation to preserve what you have and improve your quality of life. The time to act is always now, regardless of the stage, to either reverse or halt the disease.
Frequently Asked Questions About How to Cure Gum Disease
Let’s consolidate some of the key takeaways and address the most common questions head-on, providing clear, actionable answers based on the information we’ve covered. These are the queries that most frequently weigh on people’s minds when grappling with gum health issues, and understanding the nuances behind each answer is fundamental to successful treatment and management. Navigating the landscape of gum disease, from initial symptoms to advanced stages, can feel overwhelming, but armed with accurate information, you are empowered to make informed decisions and take effective steps towards a healthier mouth. This section aims to provide concise yet comprehensive answers to the burning questions that often arise, serving as a quick reference and reinforcement of the core principles of gum disease treatment and management. Let’s tackle these vital inquiries directly, ensuring you leave with clarity and confidence about addressing your gum health.
Is Gum Disease Truly Curable? What Stages Mean
Yes, gum disease can be truly cured, but this depends entirely on its stage. The early form, known as gingivitis, is characterised by inflammation of the gums (redness, swelling, bleeding) caused by plaque buildup. Crucially, at this stage, there is no irreversible damage to the bone or connective tissues supporting the teeth. Because the damage is limited to the soft tissues of the gums, gingivitis is completely reversible. With proper professional cleaning to remove plaque and calculus, combined with diligent daily brushing and flossing at home, the inflammation subsides, and the gums return to a healthy state. It’s a full recovery, meaning the disease process is stopped and the gums are restored. However, if gingivitis is left untreated, it can progress to periodontitis. Periodontitis is a more severe stage where the infection spreads below the gumline, leading to irreversible loss of the bone and ligaments that anchor the teeth. You cannot regenerate this lost tissue naturally. Therefore, periodontitis is not considered “curable” in the sense of reversing the damage that has already occurred. However, the active progression of periodontitis can be stopped and managed effectively through professional treatment and ongoing maintenance. So, curability depends on the stage: gingivitis is reversible/curable; periodontitis is not reversible in terms of damage but is treatable and manageable to prevent further loss. Early detection of gingivitis offers the opportunity for a complete cure.
Can You Get Rid of Periodontitis?
You can “get rid of” the active infection and progression of periodontitis, but you cannot “get rid of” the damage it has already caused. Periodontitis leads to irreversible loss of the bone and supporting tissues around your teeth. This lost structure does not grow back naturally. Therefore, if you mean restoring your mouth to its exact state before periodontitis began, then no, you cannot “get rid of” it in that sense. However, the goal of treating periodontitis is precisely to eliminate the bacteria that are driving the disease, stop the inflammatory process, reduce pocket depths, and prevent any further destruction of bone and tissue. Professional treatments like scaling and root planing (deep cleaning) and potentially surgery are necessary to clean infected areas below the gumline that you cannot reach yourself. Following this foundational treatment, a strict regimen of excellent home care and regular periodontal maintenance appointments with your dental professional is essential. By successfully treating the active infection and maintaining rigorous hygiene, you can achieve a stable state of periodontal health where the disease is no longer progressing. So, while the physical consequences of past damage remain, you can eliminate the active disease process and live with healthy, stable gums and teeth, even with some prior tissue loss. It’s about controlling the condition and preventing future harm, rather than undoing history.
Can You Treat Gum Disease at Home?
You absolutely can treat gum disease at home, provided it is the early stage, gingivitis. Gingivitis is caused by plaque buildup, and diligent, effective daily home oral hygiene – specifically brushing properly twice a day and flossing (or using other interdental cleaners) daily – can remove this plaque, allowing the gums to heal and reversing the condition entirely. So, for gingivitis, home care is the primary treatment and is often sufficient to achieve a cure. However, if you have periodontitis, the advanced stage involving irreversible bone and tissue loss and the formation of deep pockets, home care alone is not sufficient to treat the condition. You cannot effectively remove the hardened plaque (calculus) and bacteria from deep periodontal pockets with just a toothbrush and floss; this requires professional instruments used during scaling and root planing. For periodontitis, home care is essential and forms a critical part of the overall treatment and long-term management plan, but it must be done in conjunction with professional dental treatment. Home care maintains the results achieved by the dental professional and prevents recurrence, but it cannot replace the deep cleaning needed to initially tackle the infection below the gumline in periodontitis. Therefore, you can treat gingivitis at home, but you cannot treat periodontitis effectively alone at home; it requires a partnership between your diligent self-care and professional dental intervention.
How Do Dentists Treat Gum Disease?
Dental professionals treat gum disease using methods tailored to the stage and severity of the condition. For gingivitis, standard professional cleaning (prophylaxis) is performed to remove all plaque and calculus from the tooth surfaces above and just below the gumline. This eliminates the cause of inflammation, allowing the gums to heal when combined with improved home care. For periodontitis, the initial non-surgical treatment is typically scaling and root planing, also known as a deep cleaning. This procedure involves using specialised instruments to meticulously scrape away plaque and calculus from the tooth roots deep within the periodontal pockets below the gumline and smoothing the root surfaces. This removes the infection and toxins. If periodontitis is advanced and deep pockets or significant bone loss remain after scaling and root planing, surgical interventions may be necessary. These can include flap surgery (lifting the gums to access roots and bone), bone grafting (using bone material to help regenerate lost bone), or tissue grafting (to cover exposed roots or improve gum contour). Dentists and hygienists also provide crucial education on proper oral hygiene techniques. Following initial treatment for periodontitis, regular periodontal maintenance appointments are scheduled – often every 3-4 months – for ongoing deep cleaning and monitoring to prevent the disease from recurring. Dental treatment provides the necessary deep cleaning and, if required, corrective procedures that are impossible to perform effectively with home tools alone, creating the foundation for successful long-term management.
What Home Remedies Help Gum Disease?
When considering home remedies for gum disease, it’s vital to prioritize scientifically proven methods and understand the limitations of others. The most effective “home remedies” are, unequivocally, consistent and proper brushing and flossing. These mechanical actions physically remove the bacterial plaque that is the root cause of gum disease (both gingivitis and periodontitis). Mastering techniques for using a soft-bristled brush (angled towards the gumline) and correctly using floss or interdental brushes daily is foundational. Beyond these essential hygiene practices, some supplementary rinses can offer benefits. Warm salt water rinses can help soothe inflamed gums, reduce swelling, and offer mild antiseptic properties; they are a simple, supportive measure. Therapeutic mouthwashes containing antimicrobial agents (like those with essential oils, CPC, or prescribed chlorhexidine) can help reduce bacterial load as an adjunct to brushing and flossing, but they do not replace mechanical cleaning. Other natural substances like turmeric, coconut oil (via oil pulling), or various herbal extracts are sometimes cited for their potential anti-inflammatory or antimicrobial properties. While preliminary research exists for some of these, they are generally not supported by robust clinical evidence as effective standalone treatments for gum disease. They should be considered, at best, supplementary aids after consultation with a dental professional, and never as substitutes for professional treatment or essential daily brushing and flossing, particularly for periodontitis. The most impactful “home remedies” are the ones you perform consistently and correctly to physically remove plaque.