Table of Contents
ToggleKey Takeaways
- A dental crown is a tooth-shaped “cap” placed over a tooth to restore its shape, size, strength, and improve its appearance.
- Crowns are often necessary for teeth that are weakened by decay, fractured, have undergone root canal treatment, or to cover a dental implant or hold a bridge.
- Different types of crowns exist, primarily differing by material: all-ceramic/porcelain, porcelain-fused-to-metal (PFM), metal alloys, and all-resin, each offering unique benefits in terms of aesthetics, durability, and cost.
- The terms “dental crown” and “dental cap” are interchangeable, referring to the same dental restoration.
- Proper oral hygiene, including regular brushing, flossing, and dental check-ups, is crucial for maintaining the longevity of a dental crown and the health of the underlying tooth.
What Is a Dental Crown? Understanding This Key Dental Restoration
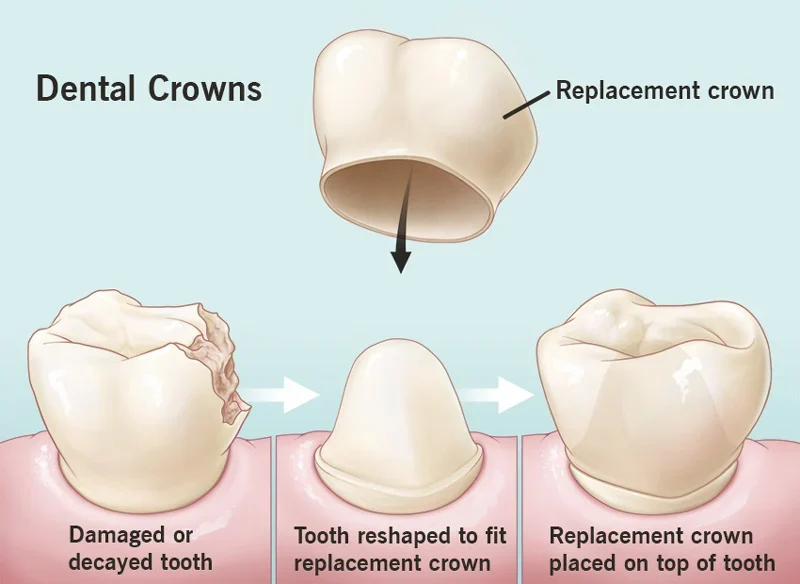
So, what precisely is this much-talked-about dental crown? Imagine a bespoke, tooth-shaped helmet, meticulously crafted to fit snugly over an existing tooth. That, in essence, is a dental crown, often referred to by the more colloquial term “cap.” It’s far more than just a cover-up, though. This is a highly engineered piece of dental artistry designed to encase the entire visible portion of a tooth that lies at and above the gum line, effectively becoming the tooth’s new outer surface. Its primary mission is multifaceted: to restore a tooth’s original shape, bring back its optimal size, bolster its strength, and significantly improve its appearance. Think of it as giving a damaged or compromised tooth a new lease on life, a protective shield that also happens to look and feel like the real deal.
The beauty of a dental crown lies in its comprehensive nature. It’s not a minor patch-up; it’s a full-coverage restoration. This makes it incredibly versatile, a go-to solution for a wide array of dental predicaments, from severe decay and fractures to cosmetic imperfections and the crucial final step in procedures like root canals or dental implants. This versatility is why it’s such a common fixture in restorative dentistry. When your dentist suggests a crown, they’re proposing a robust, long-term solution. And when we ask, “What’s behind your smile?”, for many, the answer involves the silent, sturdy work of a dental crown. It’s the unsung hero that allows you to chew your favourite foods without a second thought, to laugh without self-consciousness about a damaged tooth, and to maintain the structural integrity of your entire bite. It’s a testament to how dental science can artfully blend function and aesthetics, ensuring your smile is not just presentable, but powerfully resilient. The crown is, in many ways, a fresh start for a tooth that’s seen better days, allowing it to once again play its vital role in your oral health symphony.
Why Are Dental Crowns Needed and What Is Their Purpose?
The decision to place a dental crown isn’t arbitrary; it’s rooted in a clear set of needs and objectives, all geared towards preserving and enhancing your oral health. The primary, overarching purpose of a tooth crown is protection and restoration. Imagine a tooth weakened significantly by extensive decay, a large, old filling that’s compromised the tooth’s structural integrity, or a tooth that has unfortunately cracked. In such scenarios, the tooth is vulnerable; it’s at high risk of breaking further, potentially catastrophically, leading to pain or even tooth loss. A crown acts like a fortress, encasing the weakened tooth to shield it from the formidable forces of biting and chewing, effectively holding together parts of a cracked tooth and preventing the crack from propagating. Without this intervention, the tooth might simply crumble under pressure.
The reasons for needing a crown are diverse. One of the most common scenarios is restoring an already broken tooth or a tooth that has been severely worn down, perhaps from habitual grinding (bruxism) or an abrasive diet over many years. If a tooth has undergone root canal treatment, especially a posterior tooth like a molar or premolar which endures significant chewing forces, a crown is often essential. Root canal therapy, while saving the tooth from infection, can sometimes leave it more brittle. A crown provides the necessary reinforcement. Furthermore, crowns play a pivotal role in cosmetic dentistry. They can be used to cover severely misshapen or intrinsically discolored teeth that don’t respond well to whitening treatments, transforming a tooth’s appearance dramatically. If you’re receiving a dental implant to replace a missing tooth, a crown is the custom-made, visible “tooth” part that attaches to the implant post. And let’s not forget their role in more extensive dental work: crowns are crucial for holding a dental bridge firmly in place, acting as anchors on the adjacent natural teeth. Essentially, a crown steps in whenever a tooth needs significant structural support, a cosmetic overhaul, or to complete another dental procedure.
How Do Dental Crowns Help Restore Your Oral Health?
Dental crowns are far more than just passive coverings; they are active participants in the restoration and maintenance of your oral health, offering a trifecta of benefits: functional restoration, comprehensive protection, and crucial structural support. When a tooth is damaged, decayed, or structurally unsound, its ability to perform its basic duties, like chewing, is often compromised. You might find yourself avoiding certain foods or chewing on one side of your mouth, leading to an imbalanced bite and potential jaw discomfort. A dental crown restores the tooth to its optimal shape and strength, enabling normal, comfortable biting and chewing. This improved masticatory efficiency means you can enjoy a wider variety of foods, which is beneficial for nutrition, and it helps distribute chewing forces evenly across your dental arch, preventing undue stress on other teeth.
Beyond function, the protective role of a crown is paramount. It acts as a robust shield, sealing off the underlying natural tooth from the oral environment. This is crucial for preventing further decay in a tooth that has already been compromised. It also protects against physical damage from accidental trauma or hard foods. For individuals suffering from tooth sensitivity due to enamel erosion or gum recession exposing the dentin, a crown can provide immense relief by covering the sensitive areas, shielding them from temperature extremes (hot or cold) and sweet or acidic stimuli that would otherwise trigger discomfort. Lastly, the structural support offered by a crown cannot be overstated. For a tooth that’s cracked, has a large filling, or is weakened after a root canal, a crown reinforces its structure, much like a splint supports a broken bone. It binds the tooth together, preventing existing cracks from worsening and new ones from forming, thereby significantly reducing the risk of catastrophic fracture and potential tooth loss. This reinforcement helps to preserve the natural tooth for as long as possible, which is always the primary goal in dentistry.
Who Typically Needs a Dental Crown or Cap?
While the reasons for needing a crown are varied, certain patient profiles and dental conditions more frequently lead to this restorative solution. One of the most common groups includes individuals with teeth that have very large fillings. Over time, especially with amalgam fillings, the remaining natural tooth structure around the filling can weaken and become prone to fracture. The larger the filling, the less natural tooth is left to bear the chewing forces, making a crown an excellent option to protect what remains and prevent the tooth from splitting. If you’ve ever been told you have a filling that occupies more than half the width of your tooth, a crown might be in your future to ensure its long-term stability.
Patients who have undergone root canal therapy, particularly on their posterior (back) teeth like molars and premolars, are also prime candidates. These teeth are subjected to immense chewing forces. While a root canal saves the tooth from infection by removing the pulp, the process can sometimes render the tooth more brittle and hollowed out. A crown is then placed to protect this treated tooth from fracturing under load, ensuring its longevity. Anterior (front) teeth that have had root canals might not always require a crown if sufficient tooth structure remains, but it’s a very common recommendation for back teeth. Furthermore, individuals diagnosed with specific conditions such as “cracked tooth syndrome” – where a tooth has a crack that might be too small to see on an X-ray but causes sharp pain on biting – often find relief and protection with a crown. Similarly, those who suffer from significant tooth wear due to bruxism (chronic teeth grinding or clenching) may need crowns to restore the lost tooth height, protect the remaining structure from further abrasion, and re-establish a proper bite. Without intervention, these conditions can lead to further complications, pain, and even tooth loss, making crowns a crucial preventative and restorative measure.
What Is the Difference Between a Dental Cap and a Crown for Your Teeth?
Navigating dental terminology can sometimes feel like learning a new language, and the terms “cap” and “crown” often pop up, leading to a perfectly reasonable question: is there a difference? The short and sweet answer, much to the relief of those fearing more complexity, is no. In the world of dentistry, “dental crown” is the formal, clinical term used by professionals to describe the restoration we’ve been discussing. “Dental cap,” on the other hand, is a colloquial, layperson’s term for the very same thing. Think of it like “refrigerator” versus “fridge” – one is more formal, the other more common in everyday chat, but both refer to the appliance that keeps your food cold.
The term “cap” likely arose because, visually, a crown does indeed look like it’s capping the tooth. It’s a descriptive, easy-to-understand word that patients started using, and it stuck. So, if your dentist mentions you need a “crown,” and your friend tells you they have a “cap” on their tooth, you’re both talking about the same protective, restorative dental procedure. There is absolutely no clinical difference in the treatment, the materials used, or the outcome. Dentists will almost universally use the term “crown” in their diagnoses, treatment plans, and clinical notes because it’s the precise, accepted terminology within the profession. Understanding that these terms are interchangeable can be helpful for patients. It demystifies conversations and ensures you’re on the same page as your dental care provider. So, rest assured, whether you call it a cap or a crown, you’re referring to that same tooth-shaped hero working diligently to restore strength, function, and aesthetics to a tooth in need. Knowing this helps in clear communication and in confidently understanding the treatment being proposed for your oral health.
What Types of Dental Crowns Are Available and How Do They Differ?
Once you understand why a crown is needed, the next logical question is about the options available. Dental crowns are not a one-size-fits-all solution; they come in various types, primarily differentiated by the materials they are made from and their intended duration of use. Broadly, crowns can be categorized into permanent and temporary. A temporary crown, as the name suggests, is a short-term fix. It’s usually made in the dental office from materials like acrylic or stainless steel and is designed to protect the prepared tooth and maintain aesthetics while your permanent crown is being meticulously fabricated by a dental laboratory. It’s not built for the long haul.
The real stars of the show are the permanent crowns, designed for durability and longevity. The main basis of differentiation among these permanent crowns lies in several key factors: the material used in their construction, their resulting aesthetic qualities (how natural they look), their strength and durability (how well they stand up to chewing forces), and, inevitably, their cost. Each material offers a unique balance of these characteristics, making certain types more suitable for specific situations or patient preferences. For instance, a crown on a highly visible front tooth will prioritize aesthetics, while a crown on a back molar might prioritize strength. Your dentist will consider the location of the tooth, the health of your gums, the amount of natural tooth remaining, your biting and chewing habits (e.g., if you grind your teeth), and your personal preferences when recommending the most appropriate type of crown. The goal is to select a crown that not only fixes the immediate problem but also integrates seamlessly into your smile and functions effectively for years to come. Understanding these differences is key to making an informed choice alongside your dental professional.
What Are Some Common Types of Dental Crowns?
When it comes to permanent dental crowns, a palette of materials is available, each with its own set of superpowers. One of the most aesthetically pleasing options is the all-ceramic or all-porcelain crown. These are lauded for their ability to mimic the translucency and color of natural teeth, making them an excellent choice for front teeth where appearance is paramount. Modern ceramics, like zirconia or E-max (lithium disilicate), offer impressive strength alongside their beauty, making them increasingly viable for molars too. They are also highly biocompatible.
Then there are Porcelain-Fused-to-Metal (PFM) crowns. These have been a reliable workhorse in dentistry for decades. They feature a metal substructure for strength and support, which is then covered with a layer of tooth-colored porcelain for a more natural look. PFM crowns offer a good balance of durability and aesthetics, though the porcelain can sometimes chip, and a dark line of metal may occasionally become visible at the gum line over time if gums recede.
For unparalleled strength and durability, especially on back molars that endure significant chewing forces, metal crowns are often considered. These can be made from gold alloys (which are very kind to opposing teeth and highly biocompatible) or base-metal alloys (like nickel or chromium, which are very strong and corrosion-resistant). While not the most aesthetic choice due to their metallic color, they are incredibly long-lasting and require less tooth structure to be removed compared to some other types.
All-resin crowns are generally a more affordable option, but they tend to wear down faster and are more prone to fractures than PFM, ceramic, or metal crowns. They might be considered for temporary solutions or in specific, less demanding situations.
Lastly, Stainless Steel Crowns (SSCs) are typically used as a temporary measure for permanent teeth while a permanent crown is made, or more commonly, for restoring primary (baby) teeth in children, especially after a pulpotomy (a child’s root canal). They are cost-effective and provide good durability for the lifespan of a baby tooth. Each type presents a unique profile of benefits and considerations, allowing for a tailored approach to tooth restoration.
What Is a Post Crown and When Is It Indicated?
Sometimes, a tooth is so extensively damaged by decay or fracture, or has become so hollowed out after root canal treatment, that there isn’t enough sound tooth structure remaining above the gum line to securely support a conventional crown on its own. In these challenging situations, a post crown (often referred to as a “post-and-core crown”) becomes the solution of choice. A post crown is essentially a dental crown that gains additional retention and support from a small rod-like structure, the “post,” which is cemented down into the cleaned and shaped root canal of the tooth. This post then helps to anchor a “core buildup,” which is a mass of restorative material (like composite resin or dental amalgam) that effectively reconstructs the missing part of the tooth, creating a stable foundation onto which the final crown can be cemented.
The primary indication for a post crown is, therefore, a tooth that has undergone root canal treatment and has suffered significant loss of its coronal (above the gum) tooth structure. Without the post and core, attempting to place a crown on such a compromised tooth would be like building a house on an unstable foundation – it simply wouldn’t last. The post itself doesn’t inherently strengthen the tooth root; its main function is to retain the core material, which in turn provides the necessary support and retention for the final crown. Posts can be made from various materials, including metal (like stainless steel or titanium) or fiber-reinforced composite, with the choice depending on factors like the tooth’s location and aesthetic requirements. The core essentially replaces the missing tooth bulk, recreating the ideal shape for the crown to sit upon. So, if your dentist mentions a “post and core,” it means your tooth needs this extra internal scaffolding to ensure the long-term success and stability of your new crown.
What Are “Onlays” and “3/4 Crowns” and How Do They Differ from Full Crowns?
While a full dental crown encases the entire visible portion of a tooth, there are situations where a more conservative approach is possible and preferable. This is where onlays and 3/4 crowns come into play. These are types of partial crowns, designed to restore a tooth while preserving more of its natural, healthy structure compared to a full crown. Think of them as a middle ground between a simple filling and a full-coverage crown.
An onlay is a custom-made restoration that covers one or more cusps (the pointed or rounded projections on the chewing surface) of a tooth, as well as a portion of the occlusal (biting) surface. It’s more extensive than an inlay (which fits within the cusps) but less extensive than a full crown. Onlays are often chosen when a tooth has damage that is too large for a standard filling but not severe enough to warrant grinding down the entire tooth for a full crown. They are typically made from gold, porcelain, or composite resin and are bonded or cemented to the tooth.
A 3/4 crown, as the name subtly hints, covers most of the tooth – typically three out of the four axial walls and the occlusal surface – but leaves a significant portion, often the visible front (buccal or labial) surface, untouched. This approach is particularly useful for teeth where the front surface is still healthy and aesthetically pleasing, allowing the dentist to provide the necessary strength and protection while maintaining the natural appearance of that visible portion.
The key difference between these partial restorations and full crowns lies in their conservatism. By covering only the damaged or vulnerable parts of the tooth, onlays and 3/4 crowns allow for the preservation of more healthy tooth enamel and dentin. This is generally desirable because natural tooth structure is always best, and less invasive procedures often mean better long-term pulp health and a potentially stronger overall tooth. They are excellent options when applicable, fitting perfectly with the dental philosophy of minimally invasive treatment. However, if the tooth is too extensively damaged or weakened, a full crown will still be the most appropriate and durable solution.
What Materials Are Dental Crowns Typically Made Of?
The choice of material for a dental crown is a critical decision, significantly impacting its aesthetics, strength, longevity, and cost. Dentists have a range of sophisticated materials at their disposal, each with unique properties tailored to different clinical needs and patient preferences. As we’ve touched upon, common materials include all-ceramic or all-porcelain, renowned for their superb natural appearance, making them ideal for front teeth. Varieties like zirconia and lithium disilicate (E-max) offer enhanced strength, expanding their use to posterior teeth as well. They are also highly biocompatible, meaning they are well-tolerated by the surrounding gum tissues.
Porcelain-fused-to-metal (PFM) crowns represent a hybrid approach, combining the strength of a metal alloy substructure with the tooth-like appearance of a porcelain outer layer. For many years, PFM crowns were the standard for a blend of durability and aesthetics, though the potential for the porcelain to chip or the metal margin to show at the gum line are considerations. Metal alloys themselves, such as gold alloys or base-metal alloys (e.g., nickel-chromium or cobalt-chromium), are also frequently used, especially for back molars where biting forces are greatest. Gold alloys are exceptionally durable, wear at a rate similar to natural tooth enamel (being kind to opposing teeth), and have excellent biocompatibility. Base-metal alloys offer superior strength and corrosion resistance. The obvious trade-off with metal crowns is their metallic appearance. All-resin crowns, made from dental composite resin, are generally less expensive but are also less durable and more prone to wear and fracture compared to other types. They may be used for temporary crowns or in specific, less demanding permanent restorations.
The choice of material is influenced by several factors. The tooth’s location is key: front teeth usually demand high aesthetics (favoring ceramics), while back teeth prioritize strength (favoring metals or strong ceramics like zirconia). The amount of tooth visible when smiling also guides aesthetic choices. The patient’s preferences, including any known allergies (e.g., to certain metals), cosmetic desires, and budget, play a significant role. The strength requirements, dictated by the patient’s bite and whether they grind their teeth (bruxism), will also steer the decision. Finally, cost varies considerably between materials, with precious metal alloys and high-end ceramics typically being more expensive than base-metal alloys or resin. Your dentist will discuss these factors with you to select the material that best suits your individual circumstances and clinical needs, ensuring a functional, durable, and aesthetically pleasing outcome.
How Is a Dental Crown Procedure Typically Performed?
The journey to receiving a dental crown typically unfolds over at least two visits to your dentist, a meticulously planned process designed to ensure a perfect fit and lasting result. The first visit is primarily for examination and tooth preparation. Your dentist will begin by examining the tooth to ensure a crown is the most suitable treatment, which may involve taking X-rays to check the roots of the tooth and the surrounding bone. Before starting the preparation, the tooth and surrounding gum tissue will be numbed with local anaesthesia to ensure your comfort throughout the procedure. The tooth then needs to be carefully reshaped by filing it down on all surfaces (chewing surface and sides) to create adequate space for the crown to fit over it. The amount of tooth removed depends on the type of crown being used; for example, metal crowns are thinner and require less tooth reduction than porcelain or PFM crowns.
After reshaping the tooth, an impression (or mold) is taken of the prepared tooth, as well as the opposing arch (the teeth it will bite against) and your bite registration. These impressions are crucial, providing an exact model for the dental laboratory to custom-fabricate your crown. Traditionally, this involves using a putty-like material, though increasingly, digital scanners are used to create a 3D image of your teeth. While your permanent crown is being made in the lab (a process that can take a couple of weeks), your dentist will place a temporary crown over the prepared tooth. This temporary crown, often made from acrylic or stainless steel, protects the exposed dentin, prevents sensitivity, allows for normal function, maintains aesthetics, and stops adjacent teeth from shifting into the empty space.
Your second visit occurs once the permanent crown is ready. The temporary crown is removed, and the underlying tooth is cleaned. Your dentist will then carefully place the permanent crown to check its fit, color, and your bite. Minor adjustments may be made to ensure it fits perfectly and your bite feels comfortable. Once both you and your dentist are satisfied, the new crown is permanently cemented into place using a special dental cement. Some dental practices offer same-day crowns using advanced CAD/CAM (Computer-Aided Design/Computer-Aided Manufacturing) technology, like CEREC. This involves digitally scanning the prepared tooth, designing the crown on a computer, and then milling it from a ceramic block right in the office, allowing the entire procedure to be completed in a single visit. This option, however, isn’t suitable for all cases or available at all clinics.
What Does Dental Crown Care Involve After the Procedure?
Securing a new dental crown is a significant step towards restoring your tooth’s health and function, but the journey doesn’t end when you leave the dentist’s chair. Proper care is essential to ensure its longevity and the health of the underlying tooth and surrounding gums. In the immediate aftermath of the procedure, particularly after the permanent crown is cemented, you might experience some temporary sensitivity to hot or cold, or perhaps some tenderness in the gum tissue around the crown. This is usually mild and subsides within a few days or weeks. Your dentist might recommend using a desensitizing toothpaste. If you had a temporary crown between visits, you would have been advised to be gentle with it, avoiding sticky or very hard foods, and flossing carefully by pulling the floss out sideways rather than lifting it up, to prevent dislodging it.
Long-term oral hygiene is paramount for maintaining your crown. While the crown material itself cannot decay, the natural tooth structure underneath, especially at the margin where the crown meets the tooth, is still vulnerable to cavities and gum disease. Therefore, meticulous oral hygiene is crucial. This includes brushing twice a day with fluoride toothpaste, paying particular attention to the gumline around the crown. Flossing daily is equally important to remove plaque and food debris from between the teeth and under the crown’s edge. Your dentist or hygienist might recommend specific techniques or tools, like interdental brushes or floss threaders, if accessing the area is tricky. Attending regular dental check-ups and cleanings (typically every six months, or as advised) is also vital. During these visits, your dentist will examine the crown to check its stability, the integrity of its margins, and the health of the surrounding gums and underlying tooth.
Finally, it’s wise to avoid certain habits that can damage your crown (and your natural teeth). Refrain from chewing on extremely hard foods like ice, hard candy, or popcorn kernels, as these can potentially chip or fracture the porcelain on PFM or all-ceramic crowns. Similarly, avoid using your teeth as tools (e.g., to open packages or bite fingernails). If you clench or grind your teeth (bruxism), your dentist might recommend a nightguard to protect your crown and natural teeth from excessive forces while you sleep. With diligent care, a dental crown can serve you well for many years, often ranging from five to fifteen years, or even longer.
Frequently Asked Questions About ‘what is a crown’
Even with a comprehensive overview, a few quick answers to common questions can be incredibly helpful. This section aims to provide concise summaries of the key points discussed, serving as a rapid-reference guide to the world of dental crowns. Understanding these fundamentals empowers you to have more informed discussions with your dental care provider and feel confident about your treatment options.
Why Are Dental Crowns Needed?
Dental crowns are needed for a variety of critical reasons, primarily to restore a tooth’s function, strength, and appearance. They are essential for protecting a weak tooth from fracturing (e.g., due to extensive decay or a large filling), to hold together parts of a cracked tooth, or to restore a tooth that is already broken or severely worn down. Crowns are also used to cover and support a tooth after root canal treatment, especially back teeth, to cover a dental implant, to hold a dental bridge in place, or to improve the cosmetic appearance of a misshapen or severely discolored tooth.
What Is the Purpose of a Tooth Crown?
The fundamental purpose of a tooth crown is to encase a damaged or compromised tooth, effectively becoming its new outer surface. This serves multiple goals: to restore the tooth to its original shape and size, enabling proper chewing function; to provide significant strength and support, preventing further damage or fracture; to protect the underlying tooth structure from decay or sensitivity; and to improve the tooth’s aesthetic appearance, contributing to a healthier and more confident smile. It’s a comprehensive solution for significant dental issues.
What Is the Difference Between a Dental Cap and a Crown for Your Teeth?
There is no clinical difference whatsoever between a “dental cap” and a “dental crown.” “Dental crown” is the formal, professional term used by dentists and dental professionals to describe this type of tooth restoration. “Dental cap” is simply a colloquial, or layperson’s, term for the exact same thing, likely arising from the visual appearance of the crown “capping” the tooth. Both terms refer to the tooth-shaped covering placed over a prepared tooth.
What Materials Are Dental Crowns Typically Made Of?
Dental crowns can be crafted from a range of materials, chosen based on factors like the tooth’s location, strength requirements, aesthetics, and cost. Common materials include all-ceramic or all-porcelain (excellent aesthetics, good for front teeth), porcelain-fused-to-metal (PFM) (good strength and aesthetics), metal alloys (such as gold alloys or base-metal alloys, offering superior strength and durability, ideal for molars), and all-resin (less expensive but less durable).
How Do Dental Crowns Help Restore Your Oral Health?
Dental crowns play a vital role in restoring oral health by addressing several key aspects. Functionally, they restore a tooth’s ability to bite and chew effectively. Protectively, they shield the underlying tooth from further decay, damage, or sensitivity by creating a durable barrier. Structurally, they reinforce weakened teeth, preventing fractures and preserving the natural tooth for as long as possible, thereby contributing to the overall stability and health of your bite and smile.




