Table of Contents
ToggleKey Takeaways
- Fissure seals are thin plastic coatings applied to the chewing surfaces of back teeth.
- They serve as a preventive barrier to stop food and bacteria from causing cavities in deep grooves.
- Primarily recommended for children and adolescents, they also offer significant benefits for certain adults.
- The application procedure is quick, painless, and non-invasive.
- Sealants typically last 5-10 years but require regular dental monitoring.
- They are a cost-effective alternative to dental fillings, which treat existing decay.
- Scientific evidence confirms their safety and effectiveness in reducing decay by 80% or more when intact.
- DIY home application is unsafe and ineffective; professional application is essential.
Unlocking Healthier Smiles: Everything You Need to Know About Fissure Seals
Protecting your teeth from the relentless march of decay isn’t always about brushing twice a day and flossing (though, seriously, do that). Sometimes, the very architecture of your teeth presents sneaky hideouts for bacteria and food particles. Enter fissure seals – a clever dental innovation designed to fortify those vulnerable spots and lock out the potential for cavities. This isn’t just about fixing problems; it’s about proactively building a shield for your smile. We’re going to cut through the jargon, explore the science, and tell you exactly why these simple treatments are such a game-changer for dental health, from childhood right through to adulthood. Get ready to demystify dental sealants and empower yourself with the knowledge to make the best decisions for your oral well-being.
What are Fissure Seals and How Do They Protect Teeth?
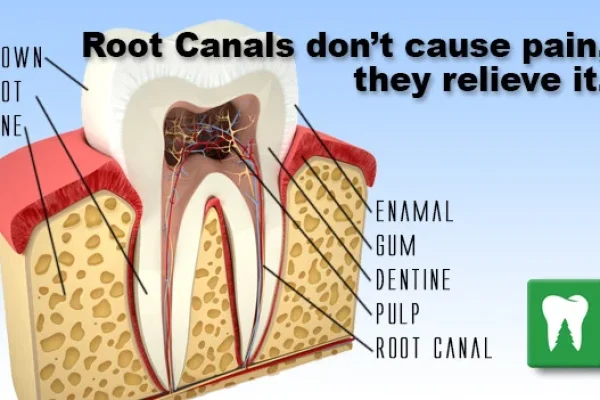
Let’s get anatomical for a second. Take a look at your back teeth – your molars and premolars. They aren’t flat. Far from it. Their chewing surfaces are a landscape of peaks and valleys, ridges, pits, and crucial grooves known as fissures. These intricate features are brilliant for grinding food, but they come with a significant drawback: they are absolute magnets for microscopic food debris and decay-causing bacteria. Even the most diligent brushing struggles to reach the very depths of these tight fissures, making them prime real estate for plaque to set up shop and start producing corrosive acids. This is precisely where the concept of dentist fissure sealing steps onto the stage. Think of a fissure seal, or dental sealant as it’s commonly known, as a microscopic, protective overcoat specifically tailored for these vulnerable chewing surfaces. It’s a thin, typically plastic-based liquid that a dental professional carefully applies, painting it directly onto the pits and fissures of the target teeth.
Once applied, this material flows into those tiny grooves and hardens, often with the help of a special light. The result? The once-complex, hard-to-clean surface is transformed into a smooth, easily brushable plane. This seamless barrier physically prevents food particles, plaque, and the acid they produce from settling into the fissures and initiating the decay process. Essentially, it seals off the entrance to the bacterial playground, drastically reducing the risk of cavities starting in these areas. When we talk about wanting to “seal teeth” or “seal tooth,” this is the precise preventive measure we mean. It’s a proactive strike against decay before it ever gets a foothold, offering a significant layer of defence, especially in young, newly erupted teeth that are particularly susceptible. It’s a simple, non-invasive procedure with profound long-term benefits for maintaining oral health.
What is a Fissure Sealant?
At its core, a fissure sealant is a highly effective dental material used as a preventive dental treatment. It’s specifically designed to protect the chewing surfaces of the back teeth – the molars and premolars. You might hear it referred to by various names; whether someone calls them “fisher seals on teeth,” “dental fissure sealant,” or just “fissure seal,” they’re all pointing to the same clever solution. The sealant material itself is a liquid that hardens into a tough, durable coating. Its main job is to smooth out the naturally uneven surfaces of these teeth, particularly those deep pits and fissures, creating a barrier that food and bacteria simply cannot penetrate. It’s a modern shield, providing a layer of protection where toothbrush bristles often fall short, significantly lowering the risk of cavities forming in these vulnerable zones.
What are Dental Fissure Sealants?
Taking a step back to a slightly more formal perspective, dental fissure sealants represent a widely accepted and incredibly common preventive dental treatment. They involve the application of a sealant material by a trained dental professional to the chewing surfaces of molars and premolars. While predominantly associated with protecting children’s teeth from decay, dental fissure sealants can also be immensely beneficial for adults, particularly those with deep fissures who are at higher risk of developing cavities. Their prevalence in modern dentistry underscores their proven effectiveness as a simple yet powerful tool in maintaining oral health and preventing the need for more extensive restorative work like fillings down the line.
What is Fissure Sealant Used For and Are They Necessary?
The primary, undeniable purpose of fissure sealants is singular and vital: to prevent tooth decay, specifically in the pitted and grooved chewing surfaces of your back teeth. These areas, as we’ve established, are notorious traps for food particles and bacteria, making them ground zero for cavity formation. The fissure sealant acts as an impermeable barrier, essentially quarantining these vulnerable zones from the harsh realities of the oral environment. You might wonder, “What is the purpose of pit and fissure sealants?” It’s elegantly simple: to block, to isolate, and to protect. By filling in these crevices, the sealant denies bacteria the shelter and fuel they need to produce cavity-causing acid. This physical barrier is remarkably effective.
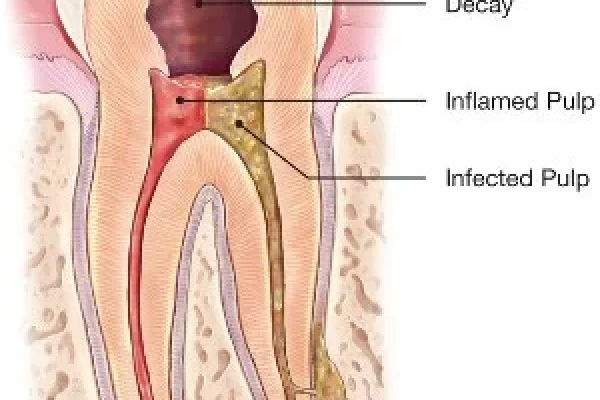
So, are fissure seals necessary? While perhaps not every single tooth in every single mouth requires one, for teeth with deep or complex fissures – which many molars and premolars naturally possess – they are incredibly beneficial, bordering on necessary for comprehensive decay prevention. Trying to clean these deep grooves effectively with just a toothbrush is like trying to scrub a tiny canyon with a single bristle; it’s simply not possible to reach the bottom. This is why, for teeth susceptible to decay in these specific spots, fissure seals are overwhelmingly “worth it.” They represent a highly cost-effective, non-invasive method to prevent future problems. The benefits of fissure sealants are substantial and well-documented: they can dramatically reduce the incidence of decay, which in turn helps prevent pain, avoids the need for potentially more complex and expensive treatments like fillings or root canals later, and helps preserve the natural structure of the tooth. They protect the tooth against the damaging acid byproduct of bacterial activity, maintaining the tooth’s integrity. For many individuals, particularly children whose newly erupted permanent teeth have not yet been exposed to significant wear and tear, the sealant offers a critical window of protection during a highly vulnerable phase.
What Are Dental Fissure Sealants and How Do They Work?
Understanding how dental fissure sealants function illuminates their protective power. The process begins with a clean, dry tooth surface. A dental professional then applies a mild acid solution, known as etchant, to the pits and fissures. This might sound alarming, but it’s a crucial, painless step. The etchant creates tiny microscopic pores on the tooth’s enamel surface, roughening it slightly. This isn’t damage; it’s preparation, creating a much better surface for the sealant material to bond to, ensuring it adheres securely and forms a durable seal. After rinsing and drying the tooth again, the liquid sealant material is carefully painted onto the prepared surfaces, flowing into all the nooks and crannies of the pits and fissures. The sealant is usually tooth-colored or clear, making it inconspicuous. Once in place, a special curing light (often a blue LED light) is used to quickly harden the liquid sealant into a tough, solid plastic layer. This hardened plastic forms a smooth, impenetrable shield over the vulnerable grooves. By physically filling and covering these areas, the sealant creates a barrier that prevents food particles, plaque, and bacteria from lodging there and producing acid that erodes enamel and leads to cavities. It’s a clever act of physical exclusion, simple yet profoundly effective at shutting down the most common pathways for decay on the chewing surfaces.
Benefits Of Fissure Sealants
The arguments in favour of fissure sealants are compelling and rooted firmly in preventive dental science. Chief among the benefits of fissure sealants is their proven ability to significantly reduce the risk of developing cavities on the chewing surfaces of back teeth (often by 80% or more when intact), prevention of associated pain and discomfort, preservation of natural tooth structure by avoiding the need for fillings, and long-term cost savings. Sealants make these vulnerable surfaces much easier to keep clean with regular brushing. On the other side, the potential risks are minimal and largely theoretical. These include the possibility of very low-level exposure to trace chemicals like BPA (deemed safe by health authorities), the rare chance of trapping decay if undetected before sealing (preventable with proper examination), and the possibility of the sealant wearing down or chipping over time, requiring monitoring and potential repair or replacement to maintain protection. When weighing these, the substantial, tangible benefits of decay prevention clearly position sealants as a highly advantageous treatment.
Who Can Benefit From Fissure Sealants and When Should They Be Applied?
While fissure sealants offer protective advantages across various age groups, they are most commonly and emphatically recommended for children and adolescents. The reason is straightforward: newly erupted permanent teeth, particularly the molars and premolars, have deep, complex pits and fissures that haven’t yet been worn down by years of chewing. Their enamel is also generally softer and less resistant to acid attacks compared to mature enamel. This makes them highly vulnerable to decay in the critical first few years after they emerge. The typical age range for sealant application aligns perfectly with the eruption schedule of these key teeth. The first permanent molars usually appear around age 6, and the second permanent molars arrive around age 12. Sealing these teeth shortly after they fully erupt is considered the ideal window of opportunity to provide maximum, long-lasting protection before decay even has a chance to start. This proactive approach is why fissure sealants for children are such a cornerstone of modern paediatric dentistry.
However, to address the question directly, “Can adults get fissure seals?” The answer is a resounding yes. While the highest benefit-to-cost ratio is often seen in children due to their high-risk, newly erupted teeth, adults can absolutely benefit, provided their teeth meet certain criteria. “Can adults teeth be sealed?” Absolutely, provided they are free of decay and have pits and fissures deep enough to warrant protection. For adults with a history of cavities, those with dry mouth, or those whose anatomy predisposes them to decay in these specific areas, sealing healthy, unrestored molars and premolars is a highly recommended preventive strategy. Determining which teeth should be sealed and which teeth require a fissure seal depends on a few factors, including the depth of the fissures, the individual’s risk of decay, and whether the tooth already has a filling or decay in those areas.
This brings us to the concept of “Indications and contraindications.” The “Indications” for sealant placement are the conditions that make it advisable – typically healthy molars and premolars (or primary teeth with deep fissures) with complex or deep anatomy that are difficult to clean effectively and are considered at risk of decay. On the flip side, “Contraindications” are the situations where sealants are generally not suitable. These include teeth that already have cavities in the pits and fissures, teeth that have existing fillings on the chewing surface, or teeth that haven’t fully erupted yet, making effective isolation and application challenging. While there aren’t strict age limits preventing adults from getting sealants, the decision is based more on the condition and anatomy of the tooth and the individual’s overall decay risk rather than age alone.
What is the Best Age to Apply Fissure Sealant?
While sealants can be applied whenever a susceptible tooth erupts, the consensus points to critical periods aligning with the eruption of permanent molars. The “best age to apply fissure sealant” is generally considered to be shortly after the first permanent molars erupt, typically around the ages of 6 to 8, and again after the second permanent molars erupt, usually between the ages of 11 and 14. Sealing these teeth within this timeframe captures them at their most vulnerable stage – newly erupted, often with deep grooves, and prior to significant exposure to decay-causing factors. This early intervention provides maximum protection during the years when children are developing their oral hygiene habits and consuming diets that may be higher in sugars. However, as mentioned, the opportunity doesn’t vanish with age; the key is sealing healthy, vulnerable teeth regardless of the patient’s age, although the highest return on investment in terms of prevention is often seen when sealants are applied early in childhood.
Can Adults Teeth Be Sealed?
Absolutely, let’s clarify this. While the narrative often centers on paediatric dentistry, the proactive benefits of dental sealants extend beyond childhood. “Can adults teeth be sealed?” Yes, under the right circumstances. If an adult has molars or premolars that are free of decay and fillings on the chewing surface, but possess deep, retentive pits and fissures that are prone to trapping food and bacteria, sealing these teeth can be an excellent preventive measure. Adults with a higher risk of developing cavities due to factors like dry mouth, certain medical conditions, or orthodontic treatment can also be strong candidates. It’s a conversation to have with your dentist, who can assess the anatomy of your teeth and your individual decay risk to determine if sealants are a beneficial treatment for you, effectively offering the same protection enjoyed by children against pit and fissure decay.
Which Teeth Require a Fissure Seal?
The focus for fissure sealing is primarily on the chewing surfaces of the posterior teeth – that is, the molars and premolars. These are the teeth with the most pronounced and deepest pits and fissures, making them the most susceptible to decay in these specific locations. When considering “which teeth require a fissure seal” or “which teeth should be sealed,” the dental professional will examine the anatomy of each tooth. Teeth with deep, narrow grooves that are difficult or impossible to clean effectively with a toothbrush are prime candidates. While the emphasis is often on permanent molars as they erupt, primary (baby) molars can also benefit from sealants if they have deep fissures and the child is at high risk of decay. The decision is based on the tooth’s structure and its vulnerability, not just its position in the mouth, though molars and premolars are overwhelmingly the teeth that fit the bill.
What is the Dental Fissure Sealant Procedure?
Undergoing a dental fissure sealant procedure is typically a straightforward, quick, and painless experience. It doesn’t involve any drilling into the tooth structure or needles, which is part of what makes it so patient-friendly, especially for children. The process generally takes just a few minutes per tooth. First, the tooth (or teeth) to be sealed must be thoroughly cleaned. This is usually done with a special abrasive paste to remove any plaque and debris from the pits and fissures. After cleaning, the tooth is carefully isolated to keep it dry and free from saliva during the procedure. This is often achieved using cotton rolls placed around the tooth or, in some cases, a dental dam. Keeping the tooth dry is absolutely critical for the sealant material to bond properly to the enamel.
Next, a mild acid solution, the etchant, is applied to the chewing surface of the tooth for a short period, usually 15-20 seconds. This etchant subtly alters the enamel surface, creating microscopic porosities that allow the sealant to mechanically lock onto the tooth effectively. After the etching time is up, the etchant is thoroughly rinsed off with water, and the tooth is dried completely again. The tooth surface will look slightly frosty or dull where the etchant was applied, indicating that the enamel has been prepared for bonding. Now comes the application of the sealant material itself. The liquid sealant is carefully painted onto the prepared pits and fissures using a small brush or applicator tip, ensuring it flows into all the grooves and crevices. The goal is to cover the entire susceptible surface without excess material. Finally, a special curing light, typically a high-intensity blue light, is shone onto the sealant for about 20-30 seconds per tooth. This light causes the liquid material to harden rapidly into a tough, protective plastic coating. The dentist will then check the hardened sealant to ensure it fully covers the fissures and that your bite feels comfortable, making any minor adjustments if needed.
How are Dental Fissure Sealants Applied?
The method by which dental fissure sealants are applied is a meticulous process designed to ensure maximum adhesion and effectiveness. After selecting the appropriate teeth – typically molars and premolars with deep pits and fissures – the first crucial step is thorough cleaning of the chewing surface. This removes any food particles or plaque. Following cleaning, strict isolation is paramount to keep the tooth completely dry and free of saliva contamination, as moisture will prevent the sealant from bonding correctly. Cotton rolls are commonly used, or a dental dam may be placed for superior isolation. A conditioning agent (etchant) is then applied, left on for a specific time, and rinsed off, preparing the enamel surface. After careful drying, the liquid sealant material is flowed into the pits and fissures. The dentist ensures complete coverage of all grooves using an explorer or brush. Finally, a curing light is used to polymerize (harden) the sealant material quickly. The technique emphasizes precise application to ensure the sealant reaches the base of the fissures and forms a smooth, integrated surface.
Resin Based Sealants Application Technique
The application technique for resin-based sealants, which are perhaps the most common type, follows a standard protocol. After cleaning and isolating the tooth, a phosphoric acid etchant is typically applied to the enamel surface for 15-20 seconds. This creates a micro-retentive surface. The etchant is then thoroughly rinsed off with water, and the tooth is dried completely. Maintaining a perfectly dry field is critical at this stage. Some resin systems require the application of a separate bonding agent after etching and rinsing, which is then lightly air-thinned and sometimes light-cured before the main sealant material is applied. Other resin sealants are self-etching or self-adhesive, simplifying this step. The liquid resin sealant is then carefully applied, ensuring it flows into all the pits and fissures. An explorer may be used to gently guide the material and remove air bubbles. The sealant is then cured using a visible light curing unit (blue light) according to the manufacturer’s instructions, typically 20-30 seconds per surface. The final step is to check the hardened sealant for complete coverage and evaluate the patient’s bite, adjusting if necessary using a fine dental bur.
GI Sealant Technique
Glass ionomer (GI) sealants represent another category of material used for sealing pits and fissures. The GI sealant technique differs slightly from resin-based sealants, primarily because glass ionomers have different properties, including the ability to bond chemically to tooth structure and release fluoride over time, which adds an extra layer of protection. While isolation is still important, GI sealants are less sensitive to moisture than resins, making them a good option in situations where achieving perfect dryness is difficult (e.g., very young or uncooperative children). The tooth surface is typically cleaned, and a conditioner (often a polyacrylic acid solution) is applied for about 10 seconds to prepare the surface, followed by rinsing and drying (though the surface doesn’t need to be bone-dry like with resin). The glass ionomer material, which comes as a powder and liquid mixed together or in pre-capsulated form, is then applied to the pits and fissures. It sets through an acid-base reaction, sometimes accelerated by a curing light, depending on the specific product (some are light-cured, others are self-curing). Because GI sealants are more wear-prone than resins, they are sometimes used as a temporary sealant or in areas not subjected to heavy chewing forces, or in situations where moisture control is problematic, serving as an interim protective measure until a resin sealant can be placed later.
How Long Do Fissure Seals Last?
One of the common questions people have is about the lifespan of this preventive treatment. So, “how long do fissure seals last?” Generally speaking, a properly applied fissure seal can last for several years. They are designed to be a durable barrier against decay. However, they are not indestructible, nor are they typically considered permanent. The longevity of a sealant depends on several factors, including the material used (some resins are more durable than others), the skill of the application (ensuring good bonding is key), the patient’s chewing habits (grinding or clenching can wear them down faster), and overall oral hygiene and diet. They can withstand the normal forces of chewing, but sometimes they can chip, wear away, or even partially detach over time.
It’s important to understand that while they offer long-term protection, they are not necessarily permanent. They provide a protective shield for a significant period, often through the years when a tooth is most vulnerable to decay. This addresses the query, “Are fissure sealants permanent?” While they are a long-lasting solution, they aren’t designed to last forever without monitoring. Regular dental check-ups are essential so your dentist can examine the sealants, ensure they are intact, and recommend repair or replacement if they show signs of wear or damage. A sealant that is chipped or has lost its seal is no longer providing full protection and needs attention. The effectiveness of fissure sealants in preventing decay is highly dependent on their retention – meaning, how well they stay bonded to the tooth. As long as the sealant remains fully intact, it provides excellent protection. If it’s lost or damaged, the tooth becomes vulnerable again.
Are Fissure Sealants Permanent?
Let’s be clear: “Are fissure sealants permanent?” No, not in the sense that they will last your entire lifetime without any maintenance or possibility of needing replacement. They are a durable, long-lasting preventive treatment, but they are not designed to be a permanent fixture on the tooth. Think of them more like a long-wearing coat of paint or a protective layer that needs occasional inspection and potential touch-ups or reapplication. The materials used are strong plastics or glass ionomers that bond securely to the tooth, but the constant forces of chewing, the presence of acids in the mouth, and wear and tear over time can cause them to chip, wear down, or lift away from the tooth surface. Their effectiveness is directly tied to their integrity; an intact sealant provides excellent protection, while a compromised one does not. Regular dental visits allow your dentist to check the condition of your sealants and ensure they are still doing their job, replacing them if necessary.
How Long Do Pit and Fissure Sealants Last?
To reiterate and provide a general timeframe, “How long do pit and fissure sealants last?” Typically, with proper application and good oral hygiene, you can expect pit and fissure sealants to last anywhere from 5 to 10 years. Some may last even longer, while others, subjected to heavier wear or placed in a less ideal environment, might need attention sooner. The critical point is that their protection is contingent on them remaining fully bonded and intact, effectively sealing off the pits and fissures. This is why ongoing monitoring during routine dental check-ups is so vital. During these appointments, the dentist or hygienist will visually inspect each sealed tooth to ensure the sealant hasn’t chipped, cracked, or worn away. If a sealant is found to be deficient, it can usually be repaired or replaced easily and quickly, restoring the protective barrier. So, while not a one-and-done for life, they offer a significant, multi-year defense against decay in the most vulnerable areas.
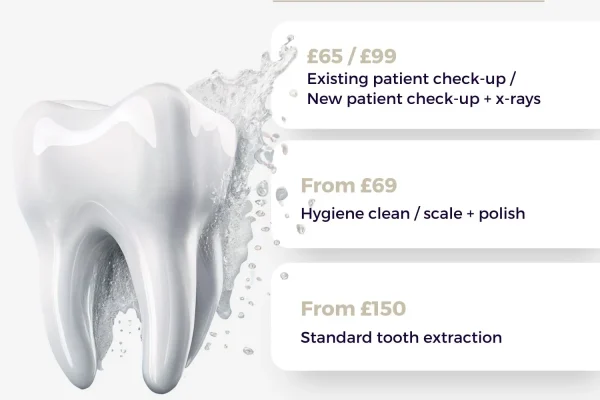
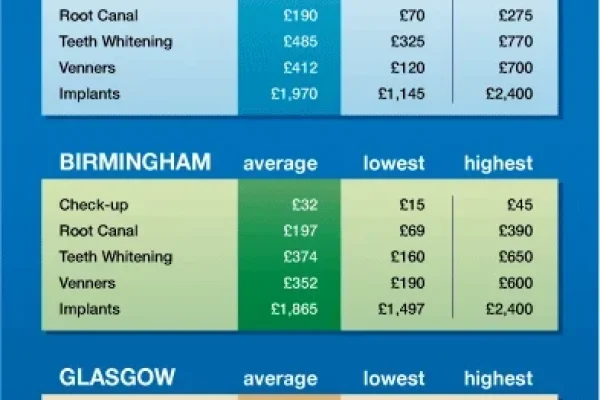
How Much Do Fissure Seals Cost?
Understanding the financial aspect is naturally part of deciding on any dental treatment. So, “how much do fissure seals cost?” The cost of fissure sealants can vary, but they are widely considered a very affordable preventive measure, especially when compared to the cost of treating a cavity. Typically, the price is quoted per tooth. You can expect the typical cost range for fissure sealants to fall somewhere between £20 and £50 per tooth in the UK, though this can fluctuate based on factors such as the dental practice’s location (costs might be higher in metropolitan areas), the individual dentist’s fee structure, and whether you have dental insurance or are covered by a national health service scheme (like the NHS in the UK) which might cover sealants for children or specific risk groups. It’s always best to get a specific quote from your dental practice before proceeding.
When considering the price, it’s crucial to compare “how much does fissure sealant cost?” to the alternative: the cost of a filling. The price of a dental filling varies significantly depending on the size of the cavity and the material used, but it is almost invariably more expensive than a sealant, often by a factor of two to four times or more per tooth. Furthermore, a tooth that requires a filling is already compromised; some of its natural structure has been lost to decay. A sealant, conversely, is applied to a healthy tooth, preserving its original state. This highlights why fissure seals are worth it from a financial perspective alone. The relatively small investment in a sealant upfront can save you a considerably larger amount down the line by preventing the need for restorative work, not to mention avoiding the potential discomfort and time associated with drilling and filling.
How much does fissure sealant cost?
To give a more direct answer to “how much does fissure sealant cost?”, while exact figures depend on your specific provider and location, budget-wise, you should anticipate a cost somewhere in the £20-£50 per tooth range in the UK. For practices in particularly expensive areas or those using premium materials, the price might edge slightly higher, but it generally remains one of the least expensive dental procedures. It’s highly recommended to ask your dentist for a detailed fee breakdown before your appointment. Also, inquire about coverage from your dental insurance provider or if your child qualifies for sealants under a public health program, as this can significantly reduce or eliminate the out-of-pocket expense.
What the tooth sealant cost?
Addressing the question phrased as “What the tooth sealant cost?”, it refers simply to the price per tooth for applying a dental sealant. As discussed, this cost is typically in the lower range of dental procedures, making it a highly accessible preventive treatment. The price per tooth is influenced by the factors mentioned earlier – location, practice fees, and insurance/coverage. The emphasis should always be placed on the value proposition: paying a relatively small amount now to potentially avoid a larger expense and preserve tooth structure later. It’s an investment in long-term dental health that pays dividends by preventing the development of cavities in these particularly vulnerable areas.
What are the Disadvantages and Risks of Fissure Sealants?
While fissure sealants are overwhelmingly safe and beneficial, it’s reasonable to consider any potential downsides or risks, however minimal they might be. One concern that occasionally surfaces relates to the material used. Some types of resin-based sealants may contain trace amounts of Bisphenol A (BPA) or related compounds. This has led some to question, “Are fissure seals safe?” Extensive research and reviews by major health and dental organisations worldwide, including the American Dental Association (ADA) and the Centers for Disease Control and Prevention (CDC), have consistently concluded that the minute levels of exposure to these substances from sealants are extremely low and pose no known health risk. The amount of BPA exposure from sealants is negligible compared to daily exposure from many common consumer products, including food packaging. The overwhelming scientific consensus is that the significant benefits of preventing tooth decay far outweigh any theoretical risk from BPA exposure. “Are Sealants on Teeth Safe?” Yes, based on decades of use and scientific evaluation, they are considered a safe and effective preventive treatment.
Another theoretical risk is the possibility of trapping bacteria under a sealant if decay was present but undetected before application, or if the seal becomes compromised. However, with proper dental examination techniques, including visual inspection, tactile examination with an explorer, and sometimes radiographs, dentists are highly skilled at identifying existing decay before sealing. If decay is detected, a filling is required instead of a sealant. When sealants are applied using correct isolation and bonding techniques, the risk of trapping bacteria is very low. A well-bonded, intact sealant prevents new bacteria from entering the fissure. Should a sealant become chipped or partially dislodged, the area becomes vulnerable again, and bacteria could potentially get underneath, but regular dental check-ups allow for timely detection and repair or replacement of compromised sealants before this becomes a significant issue. Allergic reactions to sealant materials are exceedingly rare, but theoretically possible, as with any material placed in the body.
So, why might parents choose not to have their kids teeth sealed? Often, it stems from a lack of awareness about the benefits, concerns about the cost if not covered by insurance or public health programs, or misinformation circulating regarding the safety of the materials (despite the overwhelming evidence to the contrary). Sometimes, parents might believe that excellent brushing alone is sufficient, unaware of how difficult it is to clean the deep fissures effectively. Understanding the benefits and potential risks associated with fissure sealants involves balancing the proven, significant reduction in the risk of painful and costly cavities against the minimal, largely theoretical risks associated with the materials and application. For the vast majority of individuals, the protective advantages offered by sealants make them a highly recommended preventive measure.
Are Sealants on Teeth Safe?
Let’s address this directly and definitively: “Are Sealants on Teeth Safe?” Yes, according to the consensus of leading dental and public health organizations globally, dental sealants are considered a safe and highly effective preventive treatment. While some resin-based sealants may contain or release tiny amounts of BPA, scientific studies and reviews have shown that the levels are remarkably low and pose no discernible health risk. The amount released is transient and significantly less than exposure from many other sources. The critical point is that the proven, substantial benefit of preventing tooth decay – which is a widespread disease – far outweighs any theoretical concerns about minimal chemical exposure. Dentists have been safely using sealant materials for decades with excellent results in cavity prevention.
What are some of the benefits and potential risks associated with fissure sealants?
To summarise, the primary and most significant benefits associated with fissure sealants include a dramatic reduction in the risk of developing cavities on the chewing surfaces of back teeth (often by 80% or more when intact), prevention of associated pain and discomfort, preservation of natural tooth structure by avoiding the need for fillings, and long-term cost savings. Sealants make these vulnerable surfaces much easier to keep clean with regular brushing. On the other side, the potential risks are minimal and largely theoretical. These include the possibility of very low-level exposure to trace chemicals like BPA (deemed safe by health authorities), the rare chance of trapping decay if undetected before sealing (preventable with proper examination), and the possibility of the sealant wearing down or chipping over time, requiring monitoring and potential repair or replacement to maintain protection. When weighing these, the substantial, tangible benefits of decay prevention clearly position sealants as a highly advantageous treatment.
What is the Difference Between Fissure Sealants and Fillings?
This is a crucial distinction that often causes confusion. While both fissure sealants and fillings involve applying a material to a tooth, their purpose, the state of the tooth they are applied to, and the procedure itself are fundamentally different. The core distinction lies in their function: sealants are preventive, while fillings are restorative. A fissure sealant is applied to a healthy tooth that has deep pits and fissures but is currently free of decay. Its entire purpose is to prevent decay from ever starting in those vulnerable areas by sealing them off. It’s like putting a protective coating on a surface before it gets damaged. The procedure is non-invasive, requiring no drilling into the tooth.
Conversely, a dental filling is used to restore a tooth that already has decay. When a cavity forms – meaning the tooth structure has been damaged and eroded by acid – the decayed portion of the tooth must first be removed by drilling. Once the decay is cleaned out, the resulting hole (the cavity) is filled with a material (like composite resin, amalgam, or glass ionomer) to restore the tooth’s shape, function, and prevent the decay from spreading further. It’s like patching a hole that has already formed. This procedure is invasive as it requires the removal of tooth material. Therefore, the critical difference boils down to this: sealants prevent cavities on healthy teeth, while fillings repair cavities on teeth that have already suffered decay. They address entirely different stages of tooth health and involve fundamentally different procedures.
Are Sealants and Fillings the Same?
No, absolutely not. To answer directly, “Are Sealants and Fillings the Same?” is incorrect. They are distinct dental treatments serving different purposes. Sealants are preventive coatings applied to healthy teeth to stop cavities from forming in the pits and fissures. They are non-invasive and preserve the original tooth structure. Fillings, on the other hand, are restorative materials used to repair teeth that already have cavities. They require the removal of decayed tooth structure before the material is placed to fill the resulting hole. While both involve placing material on or in a tooth, the why and the how are completely different. Understanding this distinction is key to appreciating the value of sealants as a frontline defense before damage occurs.
What Material is Used For Fissure Sealants?
The materials used for fissure sealants are specifically formulated to be highly fluid when applied, allowing them to flow deeply into the narrow pits and fissures, and then to harden into a tough, wear-resistant barrier. The most common types of materials used are primarily resin-based plastics and glass ionomers.
Resin-based sealants are typically made from dental composite resin, similar to the material used for tooth-colored fillings, but often less viscous (thinner) so they can flow better into the narrow grooves. These resins are usually methacrylate-based and require etching the tooth surface with acid beforehand to create microscopic pores for strong mechanical bonding. They are then hardened using a special curing light. Resin sealants are known for their durability and good retention on the tooth surface when properly applied. Examples of commercially available resin-based sealants mentioned in the provided keywords include Grandio Seal, Fissurit FX, and Fissurit F. These materials are designed to be wear-resistant and maintain their seal over time, providing a long-lasting barrier against bacterial invasion into the fissures. Their composition allows for good aesthetics, as they can be clear, tooth-colored (white or slightly tinted), making them virtually invisible or easily monitored.
Glass ionomer sealants are another option. These materials are distinct from resins. They bond chemically to the tooth structure, which can be advantageous in areas where achieving perfect dryness is challenging. An added benefit of glass ionomers is that they release fluoride over time. This released fluoride can help strengthen the surrounding enamel and make it more resistant to acid attacks, adding an extra layer of preventive power. However, glass ionomer sealants are generally considered less wear-resistant than resin sealants and may require more frequent monitoring and reapplication, particularly in areas subjected to heavy chewing forces. They are sometimes used as interim sealants, especially for very young children or in situations where moisture control is problematic, serving as an interim protective measure until a resin sealant can be placed later. Both material types serve the same primary function: creating a protective barrier in the pits and fissures to prevent decay. The choice of material may depend on the specific clinical situation, the patient’s age, moisture control capabilities, and the dentist’s preference.
What are fissure sealants made of?
Fissure sealants are predominantly made of either resin-based polymer materials or glass ionomer cement. The resin-based materials are typically methacrylate-based polymers, similar in composition to composite filling materials but formulated to be more fluid to penetrate narrow fissures effectively. These resins require an etching step and light-curing to harden and bond to the enamel. They often contain fillers to enhance strength and wear resistance. Glass ionomer sealants, on the other hand, are made from a mixture of glass powder and a liquid acid (like polyacrylic acid). When mixed, an acid-base reaction occurs, causing the material to set. They bond chemically to the tooth and release fluoride. Both types are biocompatible and specifically designed for dental use to create a smooth, protective coating over the vulnerable chewing surfaces of back teeth. They are formulated to be retained on the tooth surface for an extended period, providing a physical barrier against food, plaque, and acid, thereby preventing cavities.
What Can I Expect After My Dental Fissure Sealant Application?
One of the great aspects of getting dental fissure sealants is that the post-procedure experience is typically very uneventful and comfortable. You won’t leave the dental chair feeling numb or sore in the way you might after a filling or extraction. Immediately after the sealant has been applied and cured, you might notice a slight feeling of the material on the chewing surface with your tongue. It might feel a little different initially because the once-grooved surface is now smooth. However, this sensation is usually mild and something you get used to very quickly, often within a few hours. The sealant hardens instantly under the curing light, so there’s no need to wait for it to set.
A common question is, “Will the treatment hurt?” The answer is almost universally no. The procedure is non-invasive. There’s no drilling involved, and no injection is needed, so there’s no pain during the application. The cleaning and etching steps are painless. The only potential discomfort could be if you have to keep your mouth open for a prolonged period or if the cotton rolls used for isolation are slightly uncomfortable against your gums, but these are minor and temporary. Regarding eating after the procedure, “Can you eat after fissure sealants?” Yes, in most cases, you can eat and drink immediately after leaving the dental office. Since the sealant is hardened with the light, it is fully set and ready to function as soon as the appointment is finished. Your dentist might advise you to be mindful of hard or sticky foods on the sealed teeth for the rest of the day, just to be cautious while the bond fully settles, but generally, normal activities can resume right away.
Occasionally, you might experience a temporary sensation that your bite feels slightly ‘high’ on the sealed tooth. This happens if the sealant material is slightly thicker in one spot than it should be. This is usually very subtle and often resolves on its own within a day or two as you bite and chew. If it feels significantly high or bothers you, you should contact your dentist, who can quickly and easily polish the sealant down a tiny bit to adjust the bite. “Why do my teeth hurt after sealants?” It’s quite uncommon for teeth to hurt after sealant application. If you experience mild sensitivity, it might be due to the tooth being kept dry during the procedure or a temporary reaction to the etching agent, but this should be very brief. Significant pain is not typical and should be reported to your dentist immediately, although this is extremely rare with sealant placement. As for continued oral care, “Do I still have to clean my teeth?” Absolutely! Sealants protect the chewing surfaces, but the rest of your tooth surfaces (sides, front, back) and the areas between your teeth are still vulnerable to decay and gum disease. Sealants are an addition to, not a replacement for, regular brushing and flossing. You should continue your excellent oral hygiene routine and attend regular dental check-ups. These check-ups are vital for the dentist to monitor the condition of the sealants and ensure they remain intact and effective.
Can You Eat After Fissure Sealants?
Yes, you can typically eat and drink immediately after the application of fissure sealants. Because the sealant material is hardened using a special curing light right in the dental chair, it is fully set and functional by the time your appointment is over. There is no required waiting period before you can use your teeth normally. However, it’s often a good idea to be slightly cautious with extremely hard or sticky foods directly on the sealed teeth for the remainder of the day, just to give the bond the best chance to settle optimally, although this is often more of a precaution than a strict necessity with modern materials. So, feel free to grab a snack on your way out!
Why do my teeth hurt after sealants?
It is very unusual for teeth to genuinely hurt following a fissure sealant application, as the procedure is non-invasive and does not involve drilling or injections. If you experience any sensation, it is typically mild and temporary. Potential reasons for slight, fleeting discomfort could include temporary sensitivity from the tooth being kept very dry during the process, or perhaps a brief reaction to the mild acid etching solution used to prepare the enamel. Occasionally, if the sealant makes your bite feel uneven or “high,” the pressure from biting down might cause a temporary ache in the tooth or surrounding jaw muscles. This sensation of a high spot should prompt you to contact your dentist for a quick bite adjustment, which usually resolves the issue immediately. Significant pain after sealants is not expected and should be reported to your dental professional to rule out any other underlying issues, although this is an extremely rare occurrence directly related to the sealant itself.
Can Fissure Sealants Be Removed?
Yes, although fissure sealants are designed to adhere strongly to the tooth surface and last for several years, they are not permanently fused in an irreversible way. Fissure sealants can be removed by a dental professional if necessary. While the goal is for them to stay intact and protective for as long as possible, there are situations where removal might be needed.
One reason for removal is if decay is detected underneath the sealant. Although dentists take great care to ensure the tooth is free of decay before sealing, in very rare instances, decay might be present but undetected, or a sealant that was once intact might chip or wear away, allowing bacteria to eventually get underneath and start a cavity. If regular dental check-ups reveal decay under or around a sealant, the sealant will need to be removed so the decay can be accessed and treated, usually with a filling. Another reason for removal or repair is simply if the sealant itself is failing – if it’s significantly chipped, worn through, or has come off entirely. In such cases, the old or damaged sealant material is removed, and a new sealant can be applied to restore the protection, assuming the tooth is still free of decay.
So, while they are intended to be long-lasting, they are not a barrier that forever prevents access to the tooth surface underneath. Your dentist retains the ability to access the tooth by removing the sealant if needed for diagnostic or restorative purposes.
How do you remove fissure sealant?
Removing a fissure sealant is a relatively simple process performed by a dental professional. The most common method involves using a small dental drill with a fine bur. The dentist carefully and gently uses the bur to essentially “grind” or “polish” away the sealant material from the pits and fissures of the tooth. Because the sealant material is much softer than the tooth enamel itself, the dentist can remove the sealant without damaging the underlying tooth structure, provided the tooth is healthy underneath. If decay is present, the dentist will continue to use the drill to remove the decayed tooth structure as well, preparing the tooth for a filling. The process is controlled and precise, ensuring that only the sealant material and any affected tooth structure are removed. It’s a quick procedure, similar in feel to having a filling adjusted or polished, and does not typically require local anesthetic unless there is underlying decay that needs to be addressed simultaneously.
What Colour are Fissure Sealants?
Fissure sealants come in a few different visual options, primarily for visibility and monitoring purposes. Generally, they are designed to be relatively inconspicuous, blending in with the natural tooth structure. Many fissure sealants are either clear or tooth-colored.
Clear sealants are, as the name suggests, transparent. When applied, they are virtually invisible on the tooth surface. The advantage here is aesthetics – you can’t really see them once they’re on. However, being invisible can make them harder for the dentist to see and check during subsequent appointments to ensure they are still intact and fully covering the fissures.
Tooth-colored sealants are opaque and are usually white or slightly tinted (often a pale yellow or pink) to match the natural shade of tooth enamel. These are much easier for the dentist to see clearly during routine check-ups. This visibility is a significant benefit, allowing the dental team to quickly assess the sealant’s integrity and determine if it’s chipped, worn, or needs repair or replacement. While slightly more visible than clear sealants, they still blend reasonably well with the tooth and are not as noticeable as, say, a silver amalgam filling. Some sealant materials contain opaque fillers specifically to make them visible for easier monitoring by the dental professional.
The choice of colour can sometimes depend on the dentist’s preference or the specific product being used. For instance, some sealants might be tinted when applied to help the dentist see exactly where they are flowing, but then they harden to a more translucent or tooth-colored finish. So, you can expect fissure sealants to range from completely clear to a visible white or tinted shade, all designed to protect your tooth surfaces effectively. Regarding whether “Is bond used for fissure sealant?”, yes, for most resin-based sealants, a bonding agent (which helps the sealant material adhere strongly to the etched enamel surface) is used as an intermediate step or is incorporated within the sealant material itself. This bond is crucial for the sealant’s retention and long-term success, and it is typically clear or tooth-colored like the sealant material.
What is the Success Rate of Fissure Sealants?
Fissure sealants boast a remarkably high success rate in preventing cavities on the chewing surfaces of back teeth, particularly when applied correctly and maintained over time. Studies consistently demonstrate that properly applied and intact sealants are highly effective in reducing the risk of decay in the pits and fissures. When a sealant remains fully intact and bonded to the tooth, it can reduce the incidence of cavities in that specific area by 80% or more compared to an unsealed tooth. This is a significant level of protection.
The “success rate of fissure sealants” is largely measured by their ability to stay bonded to the tooth surface and prevent decay underneath or around them. Factors influencing this success include the dentist’s technique during application (ensuring proper cleaning, isolation, etching, and curing), the quality of the sealant material used, and patient factors such as chewing forces, oral hygiene, and diet. While some sealants may partially or fully detach over time (which is why regular monitoring is essential), even partially retained sealants can offer some level of protection. However, for maximum effectiveness, the sealant needs to be fully intact. Dental research widely supports the clinical effectiveness of sealants as a cost-effective public health measure for preventing pit and fissure decay, validating their high success rate when used appropriately as part of a comprehensive preventive dental care program. Their ability to create and maintain a physical barrier against decay-causing agents is the key to their high success rate.
What are the Guidelines for Fissure Sealants?
Major dental and public health organizations worldwide issue guidelines and recommendations regarding the appropriate use of fissure sealants. These guidelines are based on scientific evidence and clinical best practices, helping dental professionals determine when and how to apply sealants for optimal effectiveness and patient benefit. Generally, the guidelines for fissure sealants recommend their application primarily on the chewing surfaces of molars and premolars that are free of decay and fillings, particularly in children and adolescents shortly after these teeth erupt. This is because newly erupted teeth are most susceptible to decay, and sealing them early provides protection during the most vulnerable period.
Specific guidelines often cover:
- Selection Criteria: Which teeth should be sealed (molars and premolars with deep pits and fissures, especially in individuals at high risk of decay) and which should not (teeth with existing decay or fillings on the chewing surface, or teeth that haven’t fully erupted).
- Application Procedures: Detailed steps for proper technique, emphasizing the critical need for thorough cleaning, effective isolation from moisture, proper etching of the enamel surface, precise application of the sealant material to cover all fissures, and adequate curing (hardening) of the material. These detailed steps are crucial for ensuring strong bonding and long-term retention of the sealant.
- Recall and Monitoring: Recommendations for regular dental check-ups to examine the sealants, assess their condition, and recommend repair or replacement if they are chipped, worn, or missing. This ongoing monitoring is vital to ensure the tooth remains protected.
Organizations like the American Dental Association (ADA), the Centers for Disease Control and Prevention (CDC) in the US, the Oral Health Foundation, and national dental associations in countries like the UK and New Zealand (as referenced in some source topics) provide updated guidance based on the latest research. Following these established guidelines helps dental professionals maximise the success rate of sealant applications and contribute significantly to the prevention of pit and fissure decay in their patients.
How Long Does the Fissure Sealing Procedure Take?
One of the major advantages of fissure sealing from a patient’s perspective, especially for children, is how quick the procedure is. It’s generally a very fast and efficient process. For a single tooth, the entire procedure – from cleaning the tooth and isolating it, to applying the etchant, rinsing, drying, applying the sealant, and finally curing it with the light – typically takes just a few minutes.
If multiple teeth are being sealed during one appointment, the total time will be longer, but it still tends to be a relatively short appointment compared to restorative procedures like fillings. Sealing all four first permanent molars, for example, might take anywhere from 15 to 30 minutes, depending on how easily the teeth can be isolated and the patient’s cooperation level. Sealing second molars later might add another similar timeframe. The “how long does it take?” question is best answered by saying it’s a procedure measured in minutes per tooth, making it a convenient and time-efficient way to provide significant long-term protection against decay. This speed and simplicity contribute to making it a very accessible preventive treatment for busy families and individuals.
Can You Seal Your Teeth at Home?
Let’s be absolutely clear on this point: You should not attempt to seal your teeth or anyone else’s teeth at home. While the concept might sound simple – applying a coating – the actual procedure requires specific dental knowledge, materials, tools, and techniques that are only available and safely used in a professional dental setting.
Attempting to seal teeth at home is strongly advised against for several critical reasons. Firstly, properly cleaning and isolating the tooth from saliva and moisture is paramount for the sealant material to bond correctly and effectively. Achieving the necessary level of dryness in the back of your own mouth or a child’s mouth without professional equipment like high-volume suction, cotton roll holders, or dental dams is virtually impossible. Moisture contamination is the leading cause of sealant failure. Secondly, the etching step, which uses a mild acid to prepare the enamel surface for bonding, needs to be applied precisely for a specific duration and then thoroughly rinsed off without contaminating other areas of the mouth. Using chemicals like this without proper training and safety measures is dangerous. Thirdly, applying the sealant material requires skill to ensure it flows only into the pits and fissures without creating thick spots that interfere with your bite or trapping air bubbles. Finally, hardening the sealant requires a specific high-intensity curing light; household lights will not work. An improperly applied sealant that doesn’t bond correctly won’t provide the intended protection and could potentially trap bacteria underneath, leading to decay that is then hidden from view. Therefore, the necessary expertise, materials, isolation techniques, etching precision, and curing equipment are all exclusively available and safely utilized by trained dental professionals. DIY sealant application is unsafe, ineffective, and could potentially harm your teeth.
Are Fissure Sealants Available Near Me?
Yes, absolutely. Fissure sealants are a very common and standard preventive procedure offered by most general dental practices and paediatric dentists. If you’re looking to find a provider who offers this service, the best way is to search online. Simply typing in “dentist fissure sealing” or “fissure seals near me” into a search engine should provide you with a list of local dental offices that offer the treatment. You can also check the websites of local dental clinics, which often list the services they provide, including preventive treatments like sealants. If you already have a dentist, you can simply call their office and ask if they offer fissure sealants and if they recommend them for you or your child. Dental practices are usually happy to discuss preventive options and schedule a consultation to assess suitability. So, finding a place to get fissure sealants is typically straightforward, whether you’re searching generally or looking for a specific practice like “Fissure Seals in Mitchell Park, Marion, Adelaide SA” if you’re in that particular area. They are a widely available and accessible dental service aimed at protecting smiles.
Frequently Asked Questions About ‘fissure seals’
What is a fissure sealant?
A fissure sealant is a thin, plastic coating applied by a dentist to the chewing surfaces of back teeth (molars and premolars) to fill in the pits and fissures, creating a smooth barrier that prevents food particles, plaque, and bacteria from getting trapped and causing cavities. It’s a preventive treatment.
How long do fissure seals last?
Fissure seals typically last for several years, often between 5 and 10 years, though this can vary depending on chewing habits, oral hygiene, and the sealant material used. They are not considered permanent and require monitoring during regular dental check-ups to ensure they remain intact and effective.
How much do fissure seals cost?
The cost of fissure seals varies but is generally quite affordable, typically ranging from £20 to £50 per tooth in the UK. This cost is significantly less than the price of a dental filling to repair a cavity, making sealants a cost-effective preventive measure. Prices can depend on location, the dental practice, and insurance coverage.
Are fissure seals safe?
Yes, fissure seals are widely considered safe by leading dental and public health organizations. While some materials may contain trace amounts of BPA, the levels are extremely low and deemed safe, with the benefits of preventing decay vastly outweighing any theoretical risk. Decades of use support their safety and effectiveness.
Can adults get fissure seals?
Yes, adults can get fissure seals. While most commonly applied to children’s newly erupted teeth, adults with healthy molars and premolars that have deep pits and fissures and are at risk of decay can also benefit from having them sealed. Suitability is determined by a dentist based on tooth anatomy and decay risk.