Table of Contents
ToggleKey Takeaways
- Cavities are permanent holes in teeth caused by tooth decay.
- Tooth decay is a disease process driven by bacteria, sugar, and acid.
- Early cavities often have no symptoms; pain usually indicates advanced decay.
- Cavities cannot heal on their own and require professional dental treatment.
- Prevention through good hygiene, diet control, fluoride, and regular dental visits is key.
- Leaving cavities untreated leads to worsening pain, infection, tooth loss, and potentially serious health complications.
Understanding Cavity: What Are They and Why Do They Occur?
Stepping beyond the casual “it’s a hole,” let’s get granular. A cavity, clinically known as dental caries, is essentially permanently damaged areas in the hard surface of your teeth that develop into tiny openings or holes. This damage is progressive; it doesn’t appear overnight. It starts as tooth decay, a biological process driven by a complex interplay of factors within your mouth. Imagine your tooth enamel, the outermost layer, as a formidable shield, incredibly strong and resistant. However, certain conditions can weaken this shield. The primary culprits are specific types of bacteria that live in your mouth, constantly forming a sticky film called plaque. These bacteria have a particular fondness for sugars and other fermentable carbohydrates left behind after you eat or drink. When they consume these substances, they produce acids as a byproduct. It’s these acids, not the sugar itself directly, that are the foot soldiers of decay. They attack the minerals in your enamel in a process called demineralization. Initially, this is a microscopic assault, invisible to the naked eye. Your saliva can help counteract this by neutralizing acids and providing minerals for remineralization, a natural repair process. But if the acid attacks are too frequent – say, you’re constantly sipping on sugary drinks or snacking throughout the day without cleaning your teeth – the balance tips. Demineralization outpaces remineralization, the enamel weakens, and eventually, the surface structure breaks down. That’s when a cavity, a literal hole or lesion, begins to form. While cavities are exceedingly common across all age groups, especially among children and older adults, their prevalence doesn’t equate to normalcy in a health context. They are the most common chronic disease globally, according to the World Health Organization, a testament to our modern diets and, often, inadequate oral hygiene practices. Therefore, while you might know many people with cavities, viewing them as an inevitable or ‘normal’ part of having teeth isn’t accurate; they are preventable. Understanding this fundamental process – the bacterial-sugar-acid connection leading to enamel erosion and eventual cavity formation – is paramount. It moves cavities from the realm of bad luck into the territory of a treatable and largely preventable condition, offering hope and empowering individuals to take charge of their oral health destiny. This knowledge forms the bedrock of effective prevention and timely intervention.
What is a Cavity and Tooth Decay?
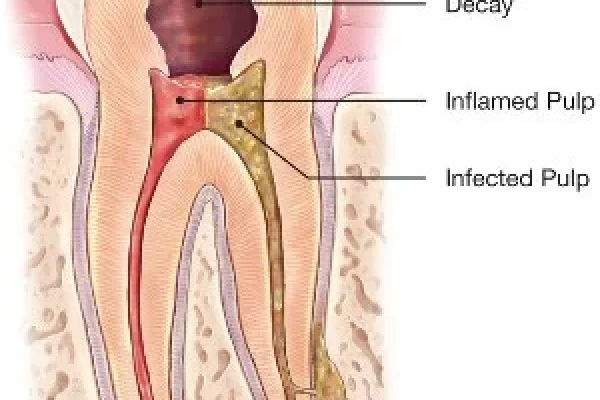
To truly grasp what a cavity is, we need to start with its origin story: tooth decay. Think of tooth decay, or dental caries, as the chronic disease process itself – the relentless assault on your tooth structure. A cavity is the result of this process, the physical manifestation of the damage. It’s like the difference between the disease (cancer) and the tumor (the physical lump). Tooth decay begins when acids produced by bacteria in plaque dissolve the mineral structure of the enamel. This demineralization process weakens the enamel, initially appearing as white spots on the tooth surface (more on stages later!). If this process continues unchecked, the enamel will eventually break down, forming a hole – the cavity. This hole can then expand, progressing deeper through the tooth layers, from the enamel to the softer dentin beneath, and eventually reaching the pulp, which contains the nerves and blood vessels. This journey through the tooth’s architecture is the progression of decay. The terms “cavity” and “tooth decay” are often used interchangeably in everyday conversation, which is understandable because the cavity is the decayed area, but it’s helpful to remember that decay is the ongoing disease, and the cavity is the hole it creates. This distinction highlights that managing dental caries isn’t just about filling the hole, but also about addressing the underlying disease process to prevent new ones and stop the existing one from worsening. Resources like the Mayo Clinic, MedlinePlus, the American Dental Association (ADA), the NHS in the UK, and even Wikipedia provide extensive information on this topic, consistently defining dental caries as the disease leading to cavities and emphasizing the bacterial and acid-driven nature of the problem. They explain how the breakdown of enamel and dentin leads to the formation of these structural defects, which are the hallmark of advanced decay, underscoring the importance of understanding the biology behind this common affliction.
What Causes Cavities and What Puts You at Risk?
Okay, let’s talk turkey about the aggressors. You’ve heard the whisper – “sugar causes cavities.” But it’s not just the sugar loaf itself that’s the villain; it’s more nuanced, a true conspiracy involving microscopic life and specific consumables. The primary culprits in the cavity saga are specific strains of oral bacteria, most notably Streptococcus mutans and Lactobacillus. These aren’t just random freeloaders; they’re particularly good at sticking to your teeth and converting the sugars and other fermentable carbohydrates you eat into acids. We’re talking about sucrose (table sugar), glucose, fructose, and even the carbs found in bread, pasta, and starchy snacks. When these bacteria feast, they excrete lactic acid, which is highly corrosive to the mineral structure of your tooth enamel. This acid bath lowers the pH level in your mouth, especially within the plaque film where the bacteria are concentrated. The constant exposure of your enamel to this acidic environment leads to the gradual loss of minerals – calcium and phosphate – from the tooth surface. This is the demineralization process we touched on earlier. If these acid attacks happen frequently throughout the day, perhaps because you’re snacking often or sipping on sugary or acidic drinks over extended periods, your saliva doesn’t get a chance to neutralize the acid and help the enamel repair itself through remineralization. The result is a net loss of minerals, weakening the enamel until it eventually collapses, forming that dreaded hole we call a cavity. This acid erosion is the core mechanism of tooth decay. Beyond this fundamental process, several factors can significantly increase your risk of developing cavities. Poor oral hygiene is a big one – insufficient brushing and flossing allow plaque and bacteria to accumulate and thrive. A diet high in sugars and frequent snacking provide a constant food source for acid-producing bacteria. Dry mouth, or xerostomia, is another major risk factor because saliva plays a crucial role in washing away food particles, neutralizing acids, and remineralizing enamel; reduced saliva flow removes this natural defense mechanism. Certain medical conditions or medications can cause dry mouth. Eating disorders like bulimia can expose teeth to stomach acid, which is highly erosive. Even the location of a tooth can matter – back teeth (molars and premolars) have lots of pits and fissures that can trap food particles and plaque, making them more susceptible. Lack of fluoride exposure, either through toothpaste, fluoridated water, or dental treatments, weakens the enamel’s resistance. Worn dental restorations or poorly fitting fillings can create traps for food and bacteria. And finally, genetics can play a role in susceptibility, though lifestyle and hygiene are usually the dominant factors. Understanding these causes and risks allows for targeted prevention strategies, forming the basis of proactive oral health management to protect your smile from decay’s relentless progression.
Does Sugar Cause Cavities?
Let’s be crystal clear: while sugar doesn’t directly drill the hole, it is undeniably the primary fuel source for the bacteria that do the drilling. The relationship is intimate and destructive. When you consume sugar, particularly sucrose (the stuff in your sugar bowl, fizzy drinks, sweets, cakes, etc.), but also other fermentable carbohydrates found in many foods, the bacteria in the plaque on your teeth have a banquet. They metabolize these sugars incredibly quickly, producing acids – primarily lactic acid – as a waste product. This process happens within minutes of sugar exposure. The plaque acts like a tiny, acidic tent on your tooth surface, holding the acid in close contact with the enamel. This acid then begins to dissolve the minerals (calcium and phosphate) in the enamel. The longer the sugar sits on your teeth, and the more frequently you expose your teeth to sugar throughout the day, the more time these bacteria have to produce acid, and the longer your enamel is subjected to this demineralizing attack. Sipping on a sugary drink over an hour is far worse than drinking it quickly and then rinsing your mouth, as it prolongs the acid exposure. Snacking frequently on sugary or starchy foods without brushing or rinsing has the same effect. So, yes, sugar is a major instigator. It feeds the acid-producing bacteria, creating the acidic environment necessary for enamel demineralization and ultimately, cavity formation. Reducing your intake of sugary foods and drinks, especially between meals, and practicing good oral hygiene immediately after consuming them, are fundamental steps in starving these bacteria and protecting your enamel shield. It’s not just the quantity of sugar, but the frequency of exposure that dramatically increases the risk. Think of it as repeated small acid attacks throughout the day versus one larger one followed by cleanup time. This frequent exposure is the key driver, making consistent dietary choices and timely cleaning paramount in the battle against sugar-fueled decay.
Cavity Causes and Risk Factors Explained
Beyond the core trio of bacteria, sugar, and acid, several other factors conspire to increase your vulnerability to cavities. Think of them as weakening the defenses or accelerating the attack. First off, let’s talk about plaque itself. It’s a sticky biofilm that constantly forms on your teeth. If plaque isn’t removed regularly and thoroughly through brushing and flossing, it thickens, providing a safe haven for bacteria to multiply and produce more acid, concentrated right against your enamel. So, poor oral hygiene is a huge, gaping risk factor. Frequency of eating and drinking, especially fermentable carbohydrates, is another critical one. Every time you expose your teeth to sugars or starches, you initiate an acid-producing cycle. Constant grazing means constant acid attacks, giving your enamel no chance to recover. Dry mouth, or xerostomia, is a major player you might not immediately think of. Saliva isn’t just wet stuff; it’s a superhero of oral defense. It helps wash away food debris, neutralizes acids, and contains minerals that can help repair early demineralization (remineralization). Conditions like Sjogren’s syndrome, diabetes, or certain medications (antihistamines, decongestants, painkillers, diuretics, and antidepressants are common culprits) can reduce saliva flow, leaving your teeth much more exposed and vulnerable to acid attacks. Eating disorders, particularly those involving vomiting (like bulimia), expose teeth to powerful stomach acids which can cause severe erosion and decay. Your diet’s content matters too – highly acidic foods and drinks (like citrus fruits, sodas, sports drinks) can directly erode enamel, even without bacterial action, making the teeth weaker and more susceptible to subsequent acid attacks from bacteria. Teeth that have deep grooves or pits (especially molars and premolars) are harder to clean effectively, making them natural traps for plaque and food particles and thus more prone to decay. Lack of sufficient fluoride exposure is a significant risk. Fluoride is a mineral that strengthens enamel, making it more resistant to acid attacks and promoting remineralization. If you don’t use fluoride toothpaste, drink fluoridated water, or receive professional fluoride treatments, your enamel is weaker than it could be. Age can also be a factor; older adults may experience gum recession, exposing the tooth roots (which are softer than enamel) to decay, or have reduced saliva flow due to medication or health conditions. Dental restorations like fillings or crowns can sometimes have margins that aren’t perfectly sealed, creating tiny gaps where bacteria and food can hide, leading to decay underneath or around the restoration. Even factors like heredity might play a small role in enamel strength or tooth shape. It’s clear that cavity risk isn’t just one thing; it’s a confluence of diet, hygiene, biology, and even lifestyle choices, all combining to create an environment where decay can flourish, highlighting the importance of a holistic approach to prevention.
What Are the Symptoms and Signs of Cavities?
Now, let’s talk about how your body tries to tell you something’s up, or sometimes, how it doesn’t. One of the truly sneaky things about cavities is that they often start silently. In their earliest stages, when the decay is confined to the outer enamel layer, you might not feel a thing. No pain, no sensitivity, nothing obvious to see unless you’re looking very closely – or a dentist spots it on an X-ray. This is why regular dental check-ups are so critical; they can catch problems before they become symptomatic. As the decay progresses deeper into the tooth, breaching the enamel barrier and reaching the softer dentin underneath, that’s usually when symptoms begin to appear. Dentin contains microscopic tubules that lead towards the pulp, where the tooth’s nerves reside. When acid or temperature changes reach these tubules, they can irritate the nerves, leading to sensitivity. This might manifest as a sharp twinge or discomfort when you eat or drink something hot, cold, or sweet. The sensitivity might be mild at first, maybe just a fleeting moment, but as the cavity deepens, it can become more pronounced and persistent. As the decay eats further into the tooth, a visible sign might emerge – a small pit, a brown or black spot, or even a noticeable hole. You might feel a rough edge with your tongue. Sometimes, trapped food particles in the cavity can cause localized discomfort or pressure. Pain, often described as a toothache, usually signifies that the decay has reached the pulp, causing inflammation of the nerve tissue within. This pain can range from dull and throbbing to sharp and severe, and it might worsen when you bite down or expose the tooth to extreme temperatures. It can also be spontaneous, starting seemingly out of nowhere, and might be particularly troublesome at night. Beyond pain and sensitivity, other potential signs include bad breath (halitosis) and a foul taste in your mouth, which can result from the bacteria and decaying tooth structure within the cavity. The tooth might become discolored, appearing brown or black, although not all discoloration indicates a cavity. Ultimately, the symptoms vary widely depending on the size and depth of the cavity. A small, early cavity might be completely asymptomatic, while a large, deep one can cause excruciating pain. Never wait for pain to seek dental attention; it’s often a sign that the problem is already quite advanced and requires professional care to prevent further complications and preserve the tooth.
What are the Signs of Cavities?
Before pain sets in, your mouth might be trying to give you subtle hints. Knowing what to look for can make a significant difference in catching cavities early when they are easier to treat and potentially even reverse. The very first visible sign of decay isn’t usually a hole, but rather a change in the appearance of the enamel. This often starts as a white spot on the tooth surface. These white spots indicate an area where the enamel has lost minerals (demineralization) but hasn’t yet broken down completely. It’s a sign that the enamel is weakened and vulnerable, a sort of pre-cavity lesion. While these white spots can sometimes be arrested or even remineralized with good oral hygiene and fluoride, they are a clear indicator that the acidic environment is winning and intervention is needed. As the decay progresses, these white spots can turn light brown, then darker brown or even black, indicating further mineral loss and breakdown of the enamel structure. You might then start to notice a visible pit or hole forming, particularly in the chewing surfaces of back teeth or the sides of teeth. Sometimes, the surface might look intact, but the decay is spreading underneath the enamel, a process called undermined enamel. In these cases, the enamel might look discolored or feel soft when examined by a dentist. You might also feel a rough spot or edge on the tooth with your tongue that wasn’t there before. Another early sign, which often precedes pain, is heightened sensitivity to temperature or sweetness. This happens when the decay has just barely penetrated the enamel and reached the outer layer of the dentin, allowing external stimuli to irritate the underlying nerve pathways. While not always a cavity, persistent sensitivity definitely warrants a dental check. Keep an eye out for any unusual discoloration, texture changes, or spots on your teeth. These visual cues, even without accompanying pain, can be critical early warning signals that decay is beginning to take hold and requires attention from a dental professional. Recognizing these signs early is your best defense against more extensive damage.
Do Cavities Cause Bad Breath or Smell?
Absolutely. It’s one of the less-talked-about, but definitely noticeable, potential side effects of a developing cavity. While bad breath, or halitosis, can be caused by many things – diet, dry mouth, gum disease, or even issues elsewhere in the body – an active cavity is certainly a possible culprit. Here’s why: a cavity is, at its core, a damaged, often open area in your tooth. This damaged area becomes a perfect little trap for food particles, bacteria, and decaying tissue. Bacteria, especially those involved in the decay process and other anaerobic bacteria (those that thrive in low-oxygen environments), tend to produce volatile sulfur compounds (VSCs) as they break down food debris and tissue. These VSCs are notorious for their foul, often sulfurous smell, the characteristic odor of bad breath. Think of the smell of rotten eggs – that’s VSCs at work. Inside a cavity, trapped food and plaque are actively decomposing, providing a constant source for these odor-producing bacteria. Furthermore, the decay itself involves the breakdown of tooth structure, and the necrotic (dying) tissue within the cavity can also contribute to an unpleasant odor. So, yes, if you notice persistent bad breath that doesn’t seem to improve much with brushing, or you detect a foul taste originating from a specific tooth, it could definitely be a sign that a cavity is present and acting as a breeding ground for odor-causing bacteria and decomposing material. It’s not the cavity itself that smells, but the microbial activity and trapped debris within it. This symptom, often coupled with one of the others like sensitivity or a visible spot, reinforces the need for a dental examination to identify and address the source of the problem. Addressing the underlying cavity is the only way to eliminate this specific cause of halitosis.
What Does a Cavity Feel Like?
The sensation of a cavity is a bit of a chameleon, changing depending on its size and depth. In its earliest stages, a cavity feels like… well, nothing at all. The enamel is hard and has no nerves, so decay confined to this outer layer is typically asymptomatic. You might only discover it during a routine dental check-up or when your tongue catches on a slightly rough spot that wasn’t there before. As the decay progresses into the dentin, which is softer and contains those microscopic tubules leading to the pulp, that’s when you might start to feel something. The most common sensation at this stage is sensitivity. This is often triggered by temperature changes (hot liquids like coffee, cold drinks or ice cream, even cold air inhaled through the mouth) or by sweet foods and drinks. The feeling might be a quick, sharp twinge, or a brief ache that disappears once the stimulus is removed. It’s often localized to the affected tooth, but sometimes it can be hard to pinpoint exactly which tooth is the culprit. The sensitivity might be mild initially but can become more intense or linger longer as the cavity gets deeper. If the decay continues unchecked and reaches the pulp chamber, where the nerves and blood vessels reside, the pain escalates significantly. This is when you experience a true toothache. The pain can be constant and throbbing, sharp and shooting, or worsen significantly when pressure is applied to the tooth (like biting down). Heat, in particular, tends to aggravate pulpitis (inflammation of the pulp), leading to intense pain. Sometimes, the pain can radiate to the jaw, ear, or temple. Paradoxically, in some very advanced cases where the pulp tissue has died due to overwhelming infection, the intense sensitivity might disappear, but a different kind of pain might arise – pressure and swelling around the root of the tooth as an abscess forms. So, the feeling of a cavity ranges from completely undetectable to mild sensitivity, to moderate discomfort when exposed to certain stimuli, to severe, persistent, or throbbing toothache, sometimes accompanied by swelling or a bad taste. The absence of pain doesn’t rule out a cavity; it just means it might not have reached the most sensitive layers yet, emphasizing the need for regular dental check-ups regardless of symptoms.
The Appearance, Stages, and Types of Tooth Cavities
Tooth decay isn’t a single event; it’s a journey, a progressive dismantling of your tooth’s structure that unfolds over time, and its appearance changes dramatically along the way. Understanding these stages is key to knowing how serious a cavity might be and what kind of intervention is needed. The process begins invisibly at the microscopic level with demineralization, the loss of minerals from the enamel surface. Visually, this often first appears as a white spot, indicating the enamel is porous and weakened. At this very early stage, the decay process might actually be reversible through remineralization if conditions improve (better hygiene, fluoride exposure). If the demineralization continues, the white spot will likely turn brownish or black, signaling that the enamel structure is starting to break down, and a surface lesion is forming. This is when a true, though possibly still very small, cavity begins. From there, the decay progresses inwards, breaching the enamel and entering the dentin. Dentin is softer than enamel, so the decay tends to spread more rapidly once it reaches this layer. As the cavity expands in the dentin, it often creates a larger area of decay underneath a smaller opening in the enamel – like a mushroom shape. Visually, this might appear as a larger brown or black area, and a noticeable hole might be present. The surface of the tooth around the decay might feel soft or crumbly when probed gently. If left untreated, the decay will continue its relentless march towards the pulp, the innermost part of the tooth containing nerves and blood vessels. Decay reaching the pulp is a significant problem, often leading to severe pain, infection, and potentially an abscess. At this advanced stage, a large, often visible hole is typically present, and the tooth structure may be significantly compromised. The appearance also depends on the type of cavity, which is often classified by where it occurs on the tooth. Pit and fissure cavities form on the chewing surfaces of back teeth (molars and premolars) and the back of front teeth, areas with natural grooves that trap plaque. Smooth surface cavities form on the flat exterior surfaces of teeth, usually where plaque is not effectively removed, often between teeth. Cavities between teeth (called interproximal cavities) are tricky because you can’t see them easily, and they require flossing to remove the plaque that causes them. Dentists often rely on X-rays to detect these hidden smooth surface cavities. Root cavities occur on the root surface of the tooth, below the gum line, and are common in older adults with gum recession; root surfaces are covered by cementum, which is even softer than dentin, making these cavities progress very quickly. A specific form, Early Childhood Caries (ECC), formerly known as baby bottle tooth decay, affects very young children. It’s often severe and rapidly progressive, typically affecting the upper front teeth first. It’s strongly associated with prolonged exposure to sugary liquids, such as sleeping with a bottle containing milk or juice, or frequent sipping of sugary drinks from a sippy cup throughout the day. Each type presents slightly differently and may require different treatment approaches, underscoring the importance of a dentist’s expertise in diagnosis and management.
What Does a Stage 1 Cavity Look Like?
Ah, the sneaky beginnings! A Stage 1 cavity, or more accurately, an initial or early lesion of tooth decay, often doesn’t look like a cavity at all in the traditional sense of a black hole. Instead, the classic appearance of early enamel demineralization, which is the very first stage of the decay process before a cavity truly forms, is a **white spot lesion**. Imagine the tooth surface losing its translucency and uniformity; it starts to look dull or chalky white in a specific area. These white spots typically appear just below the surface of the enamel. They represent areas where the acidic environment created by plaque bacteria has dissolved calcium and phosphate minerals from the enamel’s crystalline structure. The enamel is still intact on the surface, but beneath it, the porous structure reflects light differently, making the spot appear opaque white. These white spot lesions are often easier to see when the tooth surface is dried; when wet with saliva, they can be less apparent. They can occur on any tooth surface, but are commonly seen near the gum line, particularly on the front teeth, and around orthodontic brackets. While technically not yet a cavity (a physical hole), they are a strong indicator that the decay process is active and that if left unaddressed, the enamel surface will eventually break down, leading to a proper cavity (a Stage 2 or beyond lesion). The critical thing about the white spot stage is that it is potentially reversible. With diligent oral hygiene, increased fluoride exposure (through fluoride toothpaste, mouthwash, or professional application), and dietary changes to reduce sugar frequency, the minerals can be redeposited into the weakened enamel structure, essentially healing the lesion before a hole forms. So, if you spot a suspicious white area on your tooth, don’t dismiss it – it’s your tooth waving a tiny, white flag of distress, signalling a critical point where intervention can prevent a cavity from forming. It requires careful monitoring and proactive steps to encourage remineralization and arrest the decay process at this early stage, ideally under the guidance of a dental professional who can assess the lesion and recommend the most effective strategies for reversal or management.
What Does a Stage 3 Cavity Look Like?
By the time a cavity reaches Stage 3, or more generally, a moderate to advanced stage of decay, it’s usually moved well beyond the subtle white spot. This is often what people picture when they hear the word “cavity.” A Stage 3 cavity typically means the decay has progressed through the outer enamel layer and significantly into the underlying dentin. At this point, the appearance is usually quite noticeable. You’re likely looking at a visible **hole or pit** in the tooth surface. The size of the hole can vary – it might still be relatively small on the enamel surface, but the decay can have spread laterally within the softer dentin underneath, creating a larger area of damage below the surface. The color of the decayed area is usually dark – **brown, dark brown, or black**. This discoloration comes from staining of the demineralized and damaged tooth structure by food, drinks, and bacterial byproducts, as well as the physical breakdown of the dentin itself. The texture around the cavity will likely feel soft or crumbly to the touch (though you shouldn’t probe it yourself!). You might feel a definite indentation or snag with your tongue when you run it over the tooth surface. In some cases, a large portion of the tooth structure might appear missing or hollowed out. If the cavity is on a chewing surface, it might look like a dark, sunken area in the grooves. If it’s between teeth, it might only be visible on an X-ray, or you might see a dark shadow through the enamel on the side of the tooth, or feel a definite catch when flossing. A Stage 3 cavity is past the point of simple reversal with hygiene and fluoride; it represents a significant structural defect in the tooth. It usually requires professional dental intervention, most commonly a filling, to remove the decayed tissue and restore the tooth’s shape and function. Waiting at this stage allows the decay to continue its advance towards the pulp, increasing the risk of pain, infection, and the need for more complex treatment like a root canal. Timely treatment is crucial to prevent these more severe complications and preserve the tooth structure.
Types of Cavities You Can Get
Cavities aren’t a one-size-fits-all problem; they are classified based on where they form on the tooth surface, which often relates to how they start and how they are treated. Understanding the different types helps explain why some cavities are easy for your dentist to spot while others remain hidden. The most common type is **Pit and Fissure Caries**. These form in the chewing surfaces of your back teeth (molars and premolars) and sometimes on the back surface of your front teeth. These areas have natural grooves and pits that are notoriously difficult to clean thoroughly with a toothbrush, making them ideal hiding spots for plaque, food particles, and acid-producing bacteria. Decay here often starts invisibly deep within the fissure and spreads outwards. **Smooth Surface Caries** occur on the flat, smooth exterior surfaces of the teeth. These are less common than pit and fissure cavities in adults, but they can develop in areas where plaque isn’t removed effectively, particularly along the gum line or, very commonly, between teeth. Cavities between teeth (called interproximal cavities) are tricky because you can’t see them easily, and they require flossing to remove the plaque that causes them. Dentists often rely on X-rays to detect these hidden smooth surface cavities. **Root Caries** develop on the tooth root surface. This surface is normally protected by gum tissue. However, if your gums recede (due to gum disease, aggressive brushing, or age), the root surface, which is covered by a softer material called cementum, becomes exposed. Cementum decays much faster than enamel, so root cavities can progress rapidly and are a significant concern, especially for older adults. A specific form, Early Childhood Caries (ECC), formerly known as baby bottle tooth decay, affects very young children. It’s often severe and rapidly progressive, typically affecting the upper front teeth first. It’s strongly associated with prolonged exposure to sugary liquids, such as sleeping with a bottle containing milk or juice, or frequent sipping of sugary drinks from a sippy cup throughout the day. Understanding these different types helps dentists diagnose and treat cavities effectively, recognizing the distinct challenges each type presents and tailoring treatment and prevention strategies accordingly.
Dealing with Pain from Tooth Cavities
Okay, let’s cut to the chase: tooth pain. For many, this is the symptom that finally sends them scrambling for a dental appointment. And for good reason – when a cavity starts to hurt, it usually means the decay has reached a critical point. Pain from a cavity isn’t just random discomfort; it’s a clear signal that the decay has breached the outer, non-sentient layers (enamel and potentially much of the dentin) and is now irritating or infecting the dental pulp, the living core of the tooth containing nerves, blood vessels, and connective tissue. The pulp is highly sensitive, and when it becomes inflamed due to bacterial invasion or irritation from temperature changes reaching the deeper layers, it sends pain signals. This condition is called pulpitis. Initially, the pain might only occur when triggered by hot, cold, or sweet stimuli, because the fluid movement within the dentinal tubules or direct contact with temperature changes excites the nerve endings in the pulp. But as the inflammation increases and the infection potentially sets in, the pain can become spontaneous – starting without any external trigger – and persistent. It might be a dull ache, a sharp throbbing, or an intense, unbearable sensation, often worsening when you lie down or at night because of increased blood flow to the head. Pain also signifies that the cavity is now past the point of being reversible or treatable with just a simple filling; depending on the severity of the pulp involvement, it might require a root canal or even extraction. While you might desperately seek immediate relief, and there are certainly home remedies and over-the-counter options that can help manage the pain temporarily, it is absolutely crucial to understand that these do not address the underlying problem. Popping painkillers or rinsing with salt water will numb the signal, but the decay and potential infection are still advancing within the tooth. Relying solely on pain relief is like ignoring the smoke alarm while the house is burning down. Therefore, while you might need to manage the discomfort until you can see a dentist, pain from a cavity is a siren call urging you to seek professional treatment promptly. It signals a more advanced stage of decay that needs expert attention to save the tooth and prevent complications. Don’t underestimate the significance of tooth pain; it’s your body telling you it’s time to act.
Why Is a Cavity Painful?
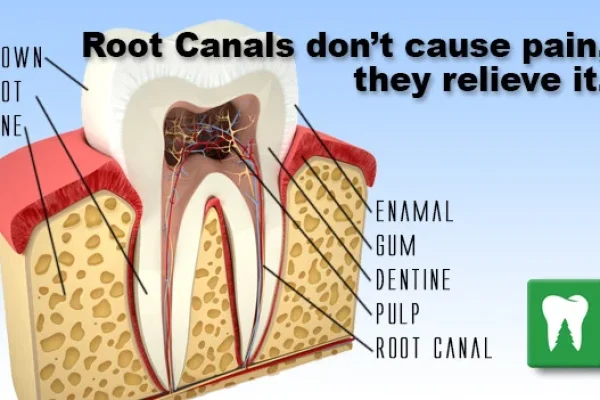
The architecture of your tooth holds the key to understanding cavity pain. The outermost layer, the enamel, is the hardest substance in your body and contains no nerves, making it impervious to pain. You can have decay completely eroding your enamel, and you might not feel a thing. Beneath the enamel lies the dentin, a softer layer composed of tiny tubules stretching from the enamel-dentin junction inwards towards the pulp. These tubules contain fluid and cellular extensions from the pulp. Dentin itself has some sensitivity, but the intense pain associated with cavities primarily comes from the pulp. The dental pulp is the living tissue at the center of the tooth, housed within the pulp chamber and root canals. It’s rich in blood vessels, connective tissue, and crucially, nerves. When a cavity penetrates through the enamel and reaches the dentin, particularly as it gets closer to the pulp, external stimuli like hot, cold, or sweet foods and drinks can travel through those dentinal tubules and irritate the nerves in the pulp. This irritation causes inflammation of the pulp, a condition known as pulpitis. Initially, if the pulp is only mildly inflamed and the cause (like a cold drink) is removed, the pain subsides quickly (reversible pulpitis). However, as the decay gets deeper, potentially allowing bacteria to enter the pulp, the inflammation becomes more severe and irreversible (irreversible pulpitis). This causes sustained pressure within the confined pulp chamber due to swelling, and the nerves become highly sensitized and constantly irritated. This leads to the classic toothache pain – throbbing, constant, or spontaneous discomfort that doesn’t go away, even after the stimulus is removed. In essence, the pain signifies that the infection and decay have reached the tooth’s nerve center, triggering a protective response that, unfortunately, manifests as significant discomfort. It’s the tooth’s way of screaming for help because its vital core is under attack and requires professional intervention to resolve the infection and prevent further damage. Understanding this process reinforces why cavity pain is a symptom that should never be ignored.
How to Stop Cavity Pain at Night?
Toothache often seems to worsen when you’re trying to sleep. This isn’t just bad luck; it’s partly due to physiological changes. When you lie down, blood flow to your head increases, which can heighten the pressure within the inflamed pulp of the tooth, intensifying the pain. Plus, without the distractions of the day, you’re simply more aware of the discomfort. While waiting for a dental appointment (which is crucial for definitive treatment), there are a few strategies that might offer temporary relief and help you catch some much-needed rest. Firstly, elevating your head with an extra pillow can help reduce some of that blood flow and pressure in the head, potentially easing the throbbing pain. Over-the-counter pain relievers are often the most effective immediate measure. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin) or naproxen (Aleve) are particularly good because they help reduce inflammation as well as block pain signals. Acetaminophen (Tylenol) can also help with pain, but it doesn’t reduce inflammation. Make sure to follow the dosage instructions on the packaging. Topical pain relievers, such as gels or liquids containing benzocaine (like Orajel), can be applied directly to the affected tooth and surrounding gum tissue to numbs the area, providing localized relief. However, be cautious with these; they are only for temporary use and shouldn’t be applied to open wounds or for extended periods. Rinses are also helpful. Rinsing your mouth with warm salt water can be soothing. Mix half a teaspoon of salt in a glass of warm water and swish it around your mouth, then spit it out. This can help reduce swelling and clean out debris around the tooth. A cold compress or ice pack applied to the outside of your cheek over the painful area might help numb the pain and reduce swelling; don’t apply ice directly to the tooth itself, as temperature sensitivity might worsen the pain. Avoid hot foods or drinks, which can exacerbate pulpitis pain. Also, avoid lying on the side of the painful tooth. While these methods offer temporary respite, remember they are not a cure. Cavity pain at night usually indicates a significant problem that requires professional dental treatment as soon as possible. Don’t delay seeing a dentist; these are just stop-gap measures.
How to Reduce Toothache at Home?
When toothache strikes, the immediate instinct is often to find a quick fix using whatever’s available at home. While no home remedy can cure a cavity or replace professional dental treatment, some methods can help alleviate the pain temporarily while you wait to see a dentist. As mentioned for night pain, over-the-counter pain relievers are your most reliable first line of defense. NSAIDs like ibuprofen are often recommended due to their anti-inflammatory properties, which target the underlying cause of pulp-related pain. Acetaminophen can also help with pain relief. Always follow the dosage instructions carefully. Rinsing with warm salt water (half a teaspoon of salt in a glass of warm water) is a classic and often effective remedy. It helps cleanse the area, reduce swelling, and can draw out some fluid, potentially easing pressure. Swish gently and spit. Some people find relief using a cold compress or ice pack applied to the outside of the cheek near the affected tooth for 15-20 minutes at a time. This can help numb the area and reduce inflammation. Be sure to wrap the ice in a cloth; don’t apply it directly to your skin or, critically, to the tooth itself if it’s sensitive to cold. Clove oil is another traditional remedy. It contains eugenol, a natural anesthetic and antiseptic. You can apply a tiny amount of clove oil to a cotton swab and dab it gently on the painful tooth and surrounding gum. Be careful, as it can have a strong taste and may irritate soft tissues if too much is used or if it contacts the gums excessively. Some people chew on a whole clove near the tooth. However, use clove oil sparingly and ensure it’s food-grade. Avoid remedies that haven’t been proven effective or could cause harm, such as placing aspirin directly on the gum (it’s acidic and can cause chemical burns). While these home methods can offer a temporary truce with the pain, they are not solutions for a cavity. They cannot remove decay or fill the hole. Use them as a stopgap measure and prioritize getting to a dentist as soon as possible. Delaying professional treatment will only allow the decay to worsen and the problem to become more complex and painful in the long run. Seek professional help; home remedies are not a substitute for treatment.
Do Cavities Always Hurt?
This is a crucial point to understand: **No, cavities do not always hurt.** In fact, many cavities, especially in their early stages, are completely painless. This is precisely why relying on pain as the sole indicator of a dental problem is a dangerous game to play with your oral health. When decay is limited to the outer enamel layer, there are no nerves involved, so there’s no sensation of pain. You might have a significant amount of demineralization or even a small enamel-only cavity forming, and be totally unaware of it. The only way these early, asymptomatic cavities are typically detected is through regular dental check-ups, where a dentist uses visual examination, probing the tooth surface, and taking X-rays. X-rays are particularly vital as they can reveal cavities forming between teeth or underneath existing fillings, areas invisible during a routine visual exam. Pain usually doesn’t begin until the decay has eaten its way through the enamel and started to penetrate the underlying dentin, which is more sensitive, or, more significantly, when it reaches the pulp, the nerve center of the tooth. By the time you experience pain, the cavity is often already moderately to severely advanced. This means the treatment required might be more involved (like a root canal) compared to a simple filling needed for an earlier-stage cavity. Furthermore, sometimes even very large cavities might cause intermittent pain or no pain at all if the pulp has already died due to chronic infection – in such cases, an abscess might form, causing different symptoms like swelling and persistent pressure. So, the absence of pain is not a green light to skip dental visits. It simply means the decay hasn’t hit a nerve (yet), emphasizing the importance of regular check-ups for early detection and intervention. Regular dental check-ups are your best defense against silent, progressing cavities; don’t wait for pain to see your dentist.
If a Cavity Hurts, Is It Too Late?
The onset of pain from a cavity is certainly a wake-up call, a sign that the decay is no longer superficial. It indicates that the infection or inflammation has likely reached the dentin and is getting close to or has entered the pulp (the tooth’s nerve). While the pain signifies a more advanced stage of the cavity, it does *not* automatically mean it’s too late to save the tooth. Think of it as reaching a critical point, but often not a point of no return regarding tooth preservation. If the pain is due to inflammation of the pulp (pulpitis), a dentist will assess if the pulp is reversibly or irreversibly inflamed. If caught early enough, sometimes simply removing the decayed tissue and placing a filling can allow the pulp to recover (reversible pulpitis). More often, if the pain is significant and persistent, it indicates irreversible pulpitis, where the pulp is too damaged or infected to heal on its own. In these cases, the treatment required is typically a root canal. This procedure involves removing the infected or inflamed pulp tissue from within the tooth, cleaning and disinfecting the root canal system, and then filling and sealing the space. After a root canal, the tooth often needs a crown to protect the weakened structure. While more complex and costly than a filling, a root canal is a way to save the tooth and eliminate the infection and pain, avoiding extraction. Extraction is usually considered a last resort, necessary only when the tooth is too severely damaged by decay or fracture to be restored, or if an infection has spread extensively and cannot be resolved with root canal therapy. So, while pain signals that the decay is advanced and the necessary treatment might be more involved than a simple filling, it’s usually *not* too late to save the tooth with procedures like a root canal. However, it’s a clear indication that you need to see a dentist *immediately* to get a proper diagnosis and initiate treatment to prevent further complications and determine the best course of action for preserving your natural tooth if possible. Delaying care once pain begins significantly reduces the chances of saving the tooth and increases the risk of serious infection spreading, potentially leading to tooth loss.
Can a Tooth Cavity Heal or Be Cured on Its Own?
Let’s address one of the most common questions and, sadly, one of the most persistent myths surrounding dental health: the idea that a tooth cavity can heal itself. The short, definitive answer is **no, an established tooth cavity (a hole in the tooth structure) cannot heal on its own**. Once the enamel surface is physically broken, creating a cavity, that structural loss is permanent. Unlike bones, which can knit themselves back together, or skin, which can regenerate tissue, tooth enamel and dentin don’t have living cells that can reproduce and repair a significant structural defect. The tooth is mineralized tissue, and while the very earliest stages of demineralization on the enamel surface (those white spots we discussed) can be reversed or arrested through remineralization (the process where minerals are redeposited into the enamel), this only works before a true hole forms. Once the surface barrier is breached and the decay has created a physical cavity, the natural repair mechanisms of the mouth, like saliva and fluoride, are no longer sufficient to rebuild the missing tooth structure. In fact, if left untreated, the decay process will continue its advance into the tooth, making the cavity larger and deeper over time. Think of it like a pothole forming in a road; you can’t just wait for it to fill itself in. It requires intervention – someone needs to fill it with new material. Similarly, an established cavity requires professional dental treatment, most commonly a filling, to remove the decayed material, clean the affected area, and restore the tooth’s form and function with a restorative material like composite resin, amalgam, or ceramic. More extensive cavities may require crowns, root canals, or even extraction if the tooth is too severely damaged. So, while you can take steps to *stop* the decay process from progressing at the very earliest white spot stage, and you can certainly prevent *new* cavities from forming, you cannot reverse or “cure” a cavity once a physical hole has developed through natural means alone. Any claims of home remedies or natural methods that can magically heal a cavity are simply untrue and potentially harmful, as delaying necessary professional treatment allows the decay to worsen significantly and increases the risk of severe complications.
Can a Cavity Heal on Its Own?
No, let’s be unequivocally clear: **a true tooth cavity, meaning a hole or structural defect in the enamel or dentin, cannot heal on its own.** The process of tooth decay involves the loss of mineral structure from the tooth surface, followed by the physical breakdown of that weakened material, creating a void – the cavity. Human teeth, particularly the enamel and dentin which form the bulk of the tooth’s structure, are not living tissues in the same way that skin or bone are. They are highly mineralized tissues with limited cellular components that cannot regenerate lost structure once it’s gone. The mouth does have natural defense mechanisms, primarily saliva, which contains minerals like calcium and phosphate and helps neutralize acids. Fluoride, whether from toothpaste, water, or dental treatments, also plays a critical role in strengthening enamel and promoting remineralization. These natural and preventative tools are highly effective at *preventing* cavities from forming in the first place, and they can even help to *arrest* or *reverse* very early-stage decay when it’s just a microscopic loss of minerals from the enamel surface (a white spot) and hasn’t yet caused a physical break in the enamel. This process of remineralization can repair the porous, demineralized enamel. However, once the acid attack has progressed to the point of causing a macroscopic breakdown – a visible pit, lesion, or hole – the tooth cannot rebuild that missing structure. The cavity is a permanent defect that will only get larger and deeper over time if left untreated. Think of it as a crack in a windowpane; the window cannot repair itself. It needs patching or replacement. Similarly, a cavity needs patching (a filling) or other restorative work by a dental professional. Any assertion that you can heal a cavity with diet, supplements, or other home methods once a hole has formed is medically inaccurate and dangerous, as it encourages delaying the necessary treatment, leading to potential complications and tooth loss. Professional dental care is the only effective “healing” for an established cavity.
Can Tooth Cavity Be Cured?
Yes, tooth cavities can be “cured,” but the definition of “cured” here means **repaired and treated by a dental professional**. It doesn’t mean the tooth magically regenerates the lost tissue. A cavity is cured by stopping the decay process in that specific area, removing the damaged tooth structure, and restoring the tooth with a filling or other restoration. This involves a dental professional cleaning out all the decayed material from the cavity, disinfecting the prepared space, and then filling the cavity with a material designed to restore the tooth’s strength, shape, and function. Common filling materials include composite resin (tooth-colored plastic and glass mixture), amalgam (a silver-colored alloy), gold, or porcelain. The type of filling used depends on the size and location of the cavity, as well as cost considerations. For larger cavities that have weakened a significant portion of the tooth structure, a crown (a cap that covers the entire tooth) might be needed after removing the decay to protect the tooth from breaking. If the decay has reached the pulp, the tooth requires a root canal procedure to remove the infected nerve tissue before it can be restored. In very severe cases where the tooth is extensively damaged and cannot be saved, extraction (removing the tooth) is the only option, after which replacement with an implant, bridge, or denture might be considered. So, while the tooth itself cannot heal the cavity, the cavity can be *treated* or *cured* through professional dental procedures that remove the disease (the decay) and repair the damage (the hole). This intervention stops the progression of the decay in that tooth and restores its integrity, effectively curing the immediate problem with that specific cavity. However, curing one cavity doesn’t make you immune to future cavities; preventing those requires ongoing good oral hygiene and preventative care. Think of the filling or crown as the “cure” – it fixes the problem and prevents it from continuing to worsen in that spot.
Can You Fix a Stage 1 Cavity?
This is where the nuance comes in! While a true hole (a cavity) cannot heal itself, you *can* potentially fix, reverse, or arrest the progression of a very early-stage lesion, often referred to as a **Stage 1 cavity** or an **initial lesion** or **white spot lesion**. At this earliest point, the decay process has only just begun to demineralize the enamel. The enamel surface is still largely intact, but the subsurface has become porous due to mineral loss, appearing as that characteristic chalky white spot. This stage is a critical window of opportunity because the process *can* be reversed or stopped *before* it progresses to a cavitation (the formation of an actual hole). How is this “fixed”? Primarily through remineralization. This involves strengthening the enamel by promoting the redeposition of minerals like calcium, phosphate, and fluoride back into the weakened structure. The key strategies for fixing a Stage 1 lesion are: **Increased Fluoride Exposure:** Using a fluoride toothpaste twice a day is essential. Your dentist might also recommend a higher-concentration prescription fluoride toothpaste, a fluoride mouth rinse, or in-office fluoride varnish treatments. Fluoride makes the enamel crystals more resistant to acid attacks and actively helps attract minerals back into the weakened areas. **Improved Oral Hygiene:** Regular and thorough brushing and flossing remove the plaque containing the acid-producing bacteria and food debris, thereby reducing the frequency and intensity of acid attacks. **Dietary Changes:** Reducing the frequency of consuming sugary and acidic foods and drinks limits the fuel source for bacteria and reduces direct acid erosion, allowing the mouth’s pH to recover between meals. **Saliva Stimulation:** Chewing sugar-free gum can stimulate saliva flow, helping to neutralize acids and aid remineralization. **Regular Dental Monitoring:** Your dentist can monitor the white spot lesion over time to ensure it’s not progressing and recommend targeted preventative measures. If these steps are successful, the enamel can reharden, and the white spot might even become less noticeable or disappear entirely. However, if the white spot continues to progress and the enamel surface breaks down, forming a true cavity, then professional restorative treatment (a filling) becomes necessary, as the point of natural reversal has passed. So, yes, you can often fix a Stage 1 cavity, but it requires proactive measures to stop the decay process and encourage the tooth to remineralize, rather than just waiting for it to disappear on its own. This early intervention is the closest thing to “healing” a cavity naturally.
Preventing Tooth Cavities
Alright, enough talk of holes and decay. Let’s shift gears to the good stuff: keeping cavities from crashing the party in the first place! Preventing cavities is infinitely better, simpler, and cheaper than treating them. It’s a proactive approach, building a strong defense against the bacterial invaders and acid attacks. The cornerstones of cavity prevention are surprisingly straightforward, centering on consistent, mindful oral care. It starts, of course, with **excellent daily oral hygiene**. This means brushing your teeth thoroughly twice a day, ideally in the morning and before bed, using a fluoride toothpaste. Proper brushing technique involves cleaning all surfaces of the teeth, including the front, back, and chewing surfaces, and paying attention to the area along the gum line where plaque tends to accumulate. Equally vital is **daily flossing** (or using interdental brushes). Brushing alone cleans only about 60% of your tooth surfaces; flossing is essential for removing plaque and food particles from between your teeth, areas where cavities commonly form and are hard to detect visually. The role of **fluoride** cannot be overstated. Fluoride is a natural mineral that significantly strengthens tooth enamel, making it more resistant to acid attacks. It also promotes remineralization, helping to repair early demineralization before a cavity forms. Ensure your toothpaste contains fluoride. Drinking fluoridated tap water (if available in your area) is another effective way to get consistent, low-level fluoride exposure. Your dentist might also recommend professional fluoride treatments (varnishes or gels) during your check-ups, particularly if you are at higher risk for cavities. **Your diet** plays a massive role. Limiting the frequency of consuming sugary and starchy foods and drinks reduces the fuel available for acid-producing bacteria. Instead of grazing on sugary snacks or sipping on soda throughout the day, try to consume these items less frequently and, if possible, rinse your mouth with water afterward. Choosing healthier snacks like fruits (in moderation, as they contain natural sugars and acids, but with fiber that helps clean teeth), vegetables, cheese, or plain yogurt is better for your teeth. Staying hydrated, especially with water, helps maintain good saliva flow, aiding in cleansing and acid neutralization. Finally, and perhaps most importantly, **regular dental check-ups and professional cleanings** are indispensable. Your dentist and dental hygienist can remove hardened plaque (calculus or tartar) that you can’t remove with brushing and flossing, identify early signs of decay (like white spots) before they become cavities, apply protective sealants to vulnerable chewing surfaces of back teeth (especially for children and teenagers), and provide personalized advice on improving your oral hygiene routine. They can also assess your individual risk factors and recommend additional preventative measures. Prevention is an ongoing effort, a daily commitment to keeping your mouth healthy, but the rewards – a healthy smile and avoiding the discomfort and cost of treating cavities – are absolutely worth it. It’s the foundation of long-term oral wellness. Source: Preventive Dentistry
How to Avoid Cavities Effectively
Avoiding cavities effectively boils down to consistently implementing a few key strategies that target the root causes: bacteria, acid, and weakened enamel. First, the absolute foundation is **superior oral hygiene**. This means brushing for two minutes, twice daily, with a fluoride toothpaste. Use a soft-bristled brush and ensure you’re cleaning all surfaces – fronts, backs, tops, and along the gumline. Don’t forget to brush your tongue to remove bacteria that contribute to bad breath. Equally non-negotiable is **daily interdental cleaning**. Use dental floss, floss picks, or interdental brushes to clean between *all* your teeth, as this removes plaque and food particles from areas where cavities often start unnoticed. If you find flossing difficult, ask your dental hygienist for tips or alternative tools. Next, **harness the power of fluoride**. Use a toothpaste with fluoride. If your community water supply is fluoridated, drink tap water. Your dentist might recommend fluoride mouth rinses or prescription-strength fluoride toothpaste if you’re at high risk. Professional fluoride treatments during dental visits provide a concentrated boost to enamel strength. **Control your diet, particularly sugar exposure frequency**. It’s not just about how much sugar you eat, but how often. Limit snacking between meals, especially on sugary or starchy foods. If you do indulge, try to do it as part of a main meal. Avoid sipping on sugary drinks (sodas, juices, sweetened teas/coffees, sports drinks) for extended periods. Instead, drink them relatively quickly, and ideally, rinse your mouth with water afterward. Choose water as your primary beverage between meals. **Chewing sugar-free gum** after eating can help stimulate saliva flow, which helps neutralize acids and wash away food particles. Look for gums containing Xylitol, as some studies suggest it may have additional benefits in reducing decay-causing bacteria. Finally, **don’t skip your regular dental check-ups and cleanings**. For most people, this means visiting the dentist every six months. These visits allow professionals to remove hardened plaque, spot early signs of decay or gum disease that you might miss, and provide protective treatments like sealants on molars, which create a barrier over the vulnerable pits and fissures. These combined efforts create a powerful defense system, significantly reducing your risk of developing cavities and preserving your smile for the long term. Consistency in these habits is the most effective strategy.
How to Stop a Cavity From Growing?
Once a true cavity (a physical hole) has formed, you cannot stop it from growing through just brushing and flossing alone. While excellent oral hygiene is absolutely crucial for *preventing* new cavities and keeping the rest of your mouth healthy, it cannot remove the decayed tooth structure that has already broken down. Brushing and flossing will help remove the plaque and food particles that are *feeding* the decay process within the cavity, potentially slowing it down slightly, but they won’t eliminate the decay itself or rebuild the missing tooth material. Think of it this way: if you have rust eating a hole in a piece of metal, cleaning the rust off regularly might slow the progression a little, but it won’t make the hole disappear or prevent the rust from continuing to spread deeper into the metal. To stop a cavity from growing, you need **professional dental intervention**. A dentist must physically remove all the decayed tooth tissue using dental instruments, essentially cleaning out the “infected” part of the tooth. Once the decay is removed, the resulting hole needs to be filled with a restorative material to seal the tooth, prevent bacteria from re-entering and resuming the decay process, and restore the tooth’s structural integrity. The type of restoration needed depends on how far the cavity has progressed. For smaller cavities, a filling is used. For larger cavities that have compromised more tooth structure, a crown might be necessary. If the decay has reached the pulp, a root canal is required to remove the infected tissue before the tooth can be restored. Delaying treatment will allow the decay to continue spreading deeper and wider within the tooth. This not only makes the cavity larger but also increases the risk of the decay reaching the pulp, leading to pain, infection, and potentially the need for more complex (and expensive) procedures like a root canal, or even tooth extraction if the damage is too extensive to repair. So, while maintaining good hygiene is vital for overall oral health, the only way to definitively *stop* an existing cavity from growing is to have it professionally treated by a dentist who can remove the decay and restore the tooth. Prompt treatment is essential.
How Can I Prevent Cavities?
Preventing cavities is a multi-faceted approach, requiring consistent effort and partnership with your dental professional. It’s not about one magic bullet, but a combination of daily habits and regular care. Here is a comprehensive breakdown of how you can effectively prevent cavities: **1. Brush Your Teeth Regularly with Fluoride Toothpaste:** Brush for two minutes, twice a day, using a toothpaste that contains fluoride. Ensure you cover all tooth surfaces and the gumline. **2. Clean Between Your Teeth Daily:** Use dental floss, interdental brushes, or a water flosser to remove plaque and food particles from between teeth where your toothbrush can’t reach. **3. Limit Sugary and Acidic Food and Drink Frequency:** Reduce how often you consume items like candies, cookies, cakes, sodas, fruit juices, sports drinks, and even starchy snacks like chips and bread. If you do consume them, try to do so as part of a meal and ideally rinse your mouth with water afterward. **4. Choose Tooth-Friendly Foods:** Opt for snacks like fresh fruits and vegetables, cheese, nuts, and plain yogurt, which are less likely to promote decay. **5. Drink Fluoridated Water:** If your tap water is fluoridated, make it your primary beverage throughout the day. **6. Use Fluoride Products as Recommended:** Depending on your risk level, your dentist might recommend using a fluoride mouth rinse or a prescription-strength fluoride toothpaste. **7. Consider Dental Sealants:** Discuss dental sealants with your dentist, especially for children and teenagers. These plastic coatings are applied to the chewing surfaces of back teeth to seal off the pits and fissures where decay often starts. More info: Dental Sealants **8. Don’t Skip Regular Dental Check-ups and Cleanings:** Visit your dentist typically every six months (or as recommended) for professional cleanings and examinations. They can identify early signs of decay, provide preventative treatments, and offer personalized advice. **9. Address Dry Mouth:** If you suffer from dry mouth (xerostomia), talk to your dentist or doctor. They can help identify the cause and recommend strategies or products (like artificial saliva or medications) to manage it, as reduced saliva flow significantly increases cavity risk. **10. Maintain Good Overall Health:** Some systemic health conditions can impact oral health, so managing conditions like diabetes is important. By incorporating these steps into your routine, you create a powerful defense system for your teeth, dramatically reducing your chances of developing cavities and maintaining a healthy, pain-free smile for years to come. It’s a lifelong commitment to proactive care.
How Are Cavities Diagnosed by Dentists?
Diagnosing cavities isn’t always as simple as peering into someone’s mouth and spotting a black spot. While advanced cavities can be visually obvious, many others are hidden from plain sight, requiring a professional eye and specialized tools. Dentists use a combination of methods to accurately detect the presence and extent of tooth decay. The process usually begins with a **thorough visual examination** of your teeth. Find out more about Dental Examination. The dentist will look for visible signs of decay, such as white spots (early demineralization), brown or black areas, or noticeable pits and holes on the tooth surfaces. They’ll check the chewing surfaces, the smooth surfaces, and the areas along the gum line. Next, the dentist uses a dental instrument called an **explorer**. This is a slender, pointed metal tool that the dentist uses to gently probe the surfaces of your teeth, especially in the pits and fissures. Healthy enamel and dentin are hard and resistant; if the explorer “sticks” in a groove or pit, or if the tooth surface feels soft or rough in a suspicious area, it can indicate that the enamel has lost its mineral integrity and decay is present. While this probing technique is helpful, dentists rely less on heavy probing in recent years due to the risk of damaging remineralizable enamel; it’s often used more gently now to feel for texture changes. A critical diagnostic tool is **dental X-rays (radiographs)**. These are essential for detecting cavities that cannot be seen during a visual exam, particularly cavities forming between teeth (interproximal cavities) and decay that is developing underneath existing fillings or crowns. Bitewing X-rays, taken periodically, show the upper and lower back teeth in biting position and are excellent for revealing interproximal decay. Periapical X-rays show the entire tooth from crown to root and are useful for assessing decay near the root or detecting abscesses. The X-ray image allows the dentist to see through the outer layers of the tooth and visualize areas of demineralization or structural breakdown that appear as darker areas on the film. Dentists may also use **other diagnostic aids**, such as intraoral cameras (which project magnified images of your teeth onto a screen), special dyes that stain decayed areas, or newer technologies like laser fluorescence devices or digital imaging that can help detect early demineralization. The dentist will combine all this information – your reported symptoms, their visual and tactile findings, and the radiographic evidence – to arrive at a diagnosis. If a cavity is found, they will explain where it is, how large or deep it appears, and recommend the appropriate treatment plan. This multi-pronged approach ensures even hidden decay is identified early.
Cavity Diagnosis: What to Expect at the Dentist
Walking into the dentist’s office for a check-up might feel routine, but the process they follow for cavity diagnosis is a systematic investigation designed to catch problems early. Here’s what typically happens. First, you’ll usually have a **discussion about your medical history, any medications you’re taking, and any changes in your oral health**, including sensitivity, pain, or anything unusual you’ve noticed. This provides the dentist with valuable context. Then, a dental hygienist or the dentist will perform a **professional cleaning** to remove plaque and calculus (hardened plaque) from your teeth. This is important because plaque can hide decay, and a clean surface allows for a more accurate examination. Following the cleaning, the **visual and tactile examination** takes place. The dentist will meticulously look at each tooth surface using a small mirror and good lighting. They’ll look for obvious signs of decay – discoloration (white, brown, or black spots), changes in enamel texture, or visible holes. They will use a gentle explorer instrument to feel the surface, checking for softness or stickiness in pits and fissures that might indicate compromised enamel. They will also examine your gums and other oral tissues. A crucial part of the diagnosis is **taking dental X-rays**. This isn’t done at every single appointment for every patient, but is typically recommended periodically (e.g., annually for bitewings) based on your age, risk factors, and dental history. X-rays are non-negotiable for finding cavities between teeth or under existing restorations, areas impossible to see otherwise. The X-ray image shows the internal structure of the teeth, and decay appears as darker areas because the demineralized tissue is less dense than healthy tooth structure. Depending on the dentist’s practice and your specific needs, they might also use **additional diagnostic tools**, such as intraoral cameras to show you what they’re seeing on a screen, or newer technologies like digital caries detection devices that use light or laser fluorescence to identify early decay that isn’t yet visible or apparent on X-rays. The dentist will combine all this information – your reported symptoms, their visual and tactile findings, and the radiographic evidence – to arrive at a diagnosis. If a cavity is found, they will explain where it is, how large or deep it appears, and recommend the appropriate treatment. This comprehensive approach ensures that both obvious and hidden cavities are identified, allowing for timely intervention and preserving oral health.
Professional Treatment Options for Tooth Cavities
Once a cavity is diagnosed, especially if it’s past the very early, reversible white spot stage, professional dental treatment is necessary. The goal is always to stop the decay process, remove the damaged tooth structure, and restore the tooth’s form, function, and integrity to prevent further problems. The type of treatment recommended depends primarily on the size, location, and depth of the cavity – essentially, how much tooth structure has been affected and whether the pulp (nerve) is involved. For the most common cavities, particularly those that are relatively small to moderate in size and haven’t reached the pulp, the treatment is a **tooth filling**. This procedure involves the dentist numbing the area around the tooth with a local anesthetic to ensure you don’t feel pain. Then, they use dental drills and instruments to carefully remove all the decayed and softened tooth material. The cleaned-out space is then prepared and filled with a restorative material. As discussed earlier, common filling materials include composite resin (tooth-colored and popular for its aesthetics), amalgam (a durable silver alloy, often used for back teeth), gold, or porcelain. The chosen material is placed into the prepared cavity, shaped, and then hardened (often with a special light for composite fillings). The filling seals the space, preventing bacteria from re-entering and further damaging the tooth, and restores the tooth’s original shape and function. Learn more about Tooth Filling. For larger cavities, where the decay has removed a significant amount of tooth structure, leaving the remaining tooth weakened and susceptible to fracture, a **dental crown** might be necessary after the decay is removed. Read about Dental Crown. A crown is a custom-made cap that covers the entire visible portion of the tooth above the gum line, providing strength and protection. This is often the case after a root canal procedure as well, as teeth requiring root canals are typically brittle. If the decay has progressed deep enough to reach the pulp, causing irreversible inflammation or infection (pulpitis), the treatment is a **root canal**. Discover Root Canal Therapy. This involves removing the infected pulp tissue from the pulp chamber and root canals, thoroughly cleaning and disinfecting the internal space, and then filling and sealing the canals. This saves the tooth structure itself but removes the living tissue within. After a root canal, the tooth usually requires a filling or a crown to restore it. In situations where the tooth is too severely damaged by decay, fracture, or infection to be saved with a filling, crown, or root canal, **tooth extraction** (removal) becomes the only option. Following extraction, options for replacing the missing tooth might include a dental implant Dental Implant, a bridge Dental Bridge, or a partial denture Dentures to restore function and prevent surrounding teeth from shifting. The dentist will evaluate your specific situation and discuss the most appropriate treatment plan to address the cavity and preserve your oral health, aiming for the least invasive effective option.
How Do Dentists Treat Cavities?
When you visit a dentist with a cavity, their primary goal is to remove the decay and restore the tooth’s structure and health. The specific method they use depends entirely on how advanced the cavity is. For **small cavities** confined to the enamel or just beginning in the dentin, the most common treatment is a **filling**. First, the dentist will likely numb the area with a local anesthetic injection to ensure you are comfortable and pain-free during the procedure. Then, they will use a high-speed dental drill and other hand instruments to carefully and precisely remove all the decayed tooth material. It’s crucial that all the softened, infected tissue is removed to stop the progression of the decay. Once the cavity is clean and the healthy tooth structure is prepared, the space is filled with a restorative material. The choice of material – composite resin (tooth-colored), amalgam (silver), gold, or porcelain – depends on factors like the location of the cavity, the amount of chewing force the tooth receives, aesthetic considerations, and cost. The filling material is placed in the prepared space, shaped to match the tooth’s contour, and hardened. This filling seals the tooth, protecting it from bacteria and restoring its function. For **larger cavities** where a significant portion of the tooth structure has been lost, a simple filling might not be strong enough to support the remaining tooth. In these cases, the dentist might recommend an **onlay or a crown**. Onlays and crowns are custom-made in a dental laboratory (or sometimes in-office with CAD/CAM technology) and cemented onto the tooth after the decay is removed. A crown covers the entire visible part of the tooth and is used when the tooth is extensively weakened, such as after a root canal. If the decay is very deep and has reached the **pulp**, causing inflammation or infection (pulpitis), a **root canal procedure** is necessary. The dentist (or an endodontist, a specialist in root canals) removes the infected pulp tissue, cleans and disinfects the inner chambers of the tooth, and seals them. This saves the tooth but removes the nerve. A tooth that has had a root canal often requires a crown for protection because it can become brittle. In the unfortunate case where the tooth is **too severely damaged** by decay to be restored by any of the above methods, **extraction** (removing the tooth) is the final option. The dentist will discuss all options and the potential prognosis for the tooth with you before proceeding with any treatment. The dentist’s expertise is crucial in selecting the appropriate treatment to ensure the best possible outcome for the affected tooth and overall oral health.
Understanding Tooth Fillings
Think of a tooth filling as essentially patching a hole in your tooth. When decay creates a cavity, it removes a portion of your natural tooth structure. A filling is the way dentists repair this damage and restore the tooth’s integrity. The process starts after the dentist has diagnosed the cavity and removed all the decayed material. This cleaned-out space is then carefully prepared to receive the filling material. The goal is to create a clean, strong surface for the filling to bond to or mechanically lock into, ensuring it lasts. Once prepared, the void is filled with a restorative material. There are several types, each with pros and cons. **Composite fillings** are made of a mixture of plastic and fine glass particles. They are popular because they can be color-matched to your natural teeth, making them very discreet, especially for front teeth or visible areas of back teeth. Composite bonds directly to the tooth structure, which can help support the weakened tooth. However, they can be more expensive than amalgam and may not be as durable for very large cavities under heavy chewing stress, though materials are constantly improving. **Amalgam fillings** are made from a mixture of metals, including silver, tin, copper, and mercury. They are strong, durable, and typically less expensive than composite fillings. Amalgam fillings are often used for cavities in back teeth, which bear significant chewing forces. While there has been some public concern about the mercury content, dental organizations worldwide confirm that amalgam fillings are safe and stable when used for dental restorations. **Gold fillings** are made from gold alloys. They are very durable, biocompatible, and long-lasting, but they are the most expensive option and require multiple dental visits to place. **Porcelain (ceramic) fillings**, often called inlays or onlays depending on how much of the tooth they cover, are custom-made in a lab and then bonded to the tooth. They are aesthetic and durable but are also costly and require more than one appointment. The dentist will choose the most appropriate filling material based on the size and location of the cavity, your bite, aesthetic preferences, and budget. The filling material is placed into the prepared cavity, shaped to restore the tooth’s contour, and then hardened (either by setting on its own, as with amalgam, or with a curing light, as with composite). The filling effectively seals the cavity, preventing bacteria from re-entering and continuing the decay process, and restores the tooth’s function. Fillings are the cornerstone of restorative dentistry for cavities.
Can You Treat or Fix a Cavity at Home?
This is a topic fraught with misinformation, and it’s critical to get this right. The definitive answer is **no, you cannot treat or fix a cavity at home once a physical hole or structural breakdown has occurred in your tooth**. The internet is rife with claims and supposed home remedies – everything from garlic and clove paste to various oils, herbs, and even specific dietary changes touted as cavity cures. Let’s be clear: none of these methods can remove decayed tooth structure or replace the missing material that constitutes a cavity. As we’ve discussed, tooth enamel and dentin cannot regenerate lost tissue once a hole has formed. While some natural substances might have antimicrobial properties (like clove oil’s eugenol, which can temporarily soothe pain) or even help slightly with remineralizing very early demineralization (white spots), they cannot penetrate the tooth to clear out infected dentin or fill a physical void. Attempting to treat a cavity at home with unproven remedies is not only ineffective but genuinely dangerous. It provides a false sense of security, causing you to delay the necessary professional dental treatment. While you’re experimenting with garlic or miracle pastes, the bacteria and acid within the cavity are continuing their destructive work, eating deeper into the tooth. This delay can turn a problem that could have been fixed with a simple filling into one requiring a root canal, a crown, or even extraction. It also increases the risk of pain, infection, and the infection potentially spreading beyond the tooth. The only way to effectively treat an established cavity is through professional dental intervention, which involves removing the decayed tissue and restoring the tooth with a filling or other restoration. Home care is essential for *preventing* cavities and *managing* pain temporarily until you see a dentist, but it cannot repair the structural damage caused by decay. Don’t fall for the myths; trust the science and seek professional help for a diagnosed cavity. Your long-term oral health depends on it, and professional treatment is the only reliable solution for an existing cavity.
How to Fix a Cavity at Home?
To be absolutely blunt: **You cannot fix a cavity at home.** The idea is appealing – a quick, DIY solution to avoid the dentist’s chair. However, it’s rooted in a fundamental misunderstanding of what a cavity is and how teeth are structured. A cavity is a physical hole or area of significant structural damage caused by the progressive loss of tooth mineral and subsequent breakdown of the tooth’s hard tissues (enamel and/or dentin). Fixing this damage requires two critical steps that are impossible to perform outside of a dental office: 1) **Complete and sterile removal of all decayed and infected tooth tissue.** Decayed tissue is soft and teeming with bacteria. If any of this is left behind, the decay will continue under any material you place over it. Dentists use specialized instruments (drills, excavators) in a sterile environment to ensure all the compromised material is removed. 2) **Filling the resulting void with a biocompatible, durable, and properly sealed restorative material.** Dental filling materials (like composite, amalgam, etc.) are specifically designed to withstand the harsh environment of the mouth (constant moisture, chewing forces, temperature changes) and bond or mechanically adhere to the remaining healthy tooth structure, creating a seal that prevents bacteria from re-entering. There is no substance you can buy over-the-counter or create in your kitchen that can effectively clean out deep decay and permanently fill a cavity to the standards required for long-term oral health. Any attempt to patch a cavity with temporary materials (like some emergency dental kits) is just that – temporary. It might offer very brief relief or protection, but it’s not a fix and can’t be relied upon. Claims about natural remedies like garlic, specific diets, or herbs “healing” a cavity are unsubstantiated and dangerous because they cause people to delay seeking actual treatment while the decay worsens. Save your time and your tooth by consulting a dentist immediately if you suspect or know you have a cavity. Professional treatment is the *only* way to properly fix it and prevent further damage or complications.
Can Toothpaste Fill a Cavity?
No, toothpaste absolutely cannot fill a cavity. This is another common misconception, perhaps stemming from the fact that fluoride toothpaste is crucial for *preventing* cavities and helping to reverse *very early* demineralization. Here’s the distinction: Toothpaste, particularly fluoride toothpaste, works by strengthening enamel (remineralization) and making it more resistant to acid attacks. When decay is in its initial, invisible or white-spot phase – meaning minerals are being lost from the enamel, but the surface hasn’t broken down into a hole yet – fluoride from toothpaste (and other sources) can help draw minerals back into the weakened area, potentially reharden the enamel and arrest or even reverse the process *before* a cavity forms. Think of it as patching tiny, microscopic pores in the enamel surface. However, once the demineralization has progressed to the point where the enamel surface physically breaks down, creating a discernible pit or hole – a true cavity – toothpaste has no capacity to rebuild that missing structure. It’s a paste, not a restorative material designed to fill a void and withstand chewing forces. Applying toothpaste to a cavity might provide fleeting relief if the cavity is sensitive, but it won’t remove the decayed tissue within the hole, prevent bacteria from multiplying inside, or restore the tooth’s integrity. In fact, toothpaste (and food) can get trapped *in* the cavity, potentially making the situation worse by providing more fuel for bacteria. The only way to fill a cavity is with professional dental restorative materials like composite resin or amalgam, which are specifically engineered to bond to tooth structure, seal the area, and function under oral conditions. While toothpaste is a vital tool in your daily defense *against* cavities and can help manage early-stage demineralization, it has zero capability to fill an established cavity. Professional treatment is the only way to repair a physical hole in your tooth.
Products for Tooth Cavity Management and Prevention
While professional dental treatment is necessary to fix an existing cavity, there are several oral care products that play a vital role in *managing* the risk of developing cavities in the first place, and helping to prevent new ones from forming. These products work primarily by strengthening enamel, controlling the bacterial population, and facilitating the cleaning of tooth surfaces. The absolute king of anti-cavity products is **fluoride toothpaste**. Using fluoride toothpaste at least twice a day is the foundation of cavity prevention for most people. Fluoride works in multiple ways: it makes tooth enamel stronger and more resistant to acid attacks, it helps to speed up the natural remineralization process that repairs early enamel damage, and it can even interfere with the acid production of bacteria. Look for toothpaste approved by major dental associations (like the ADA in the US or the Oral Health Foundation in the UK), as these are guaranteed to contain an effective concentration of fluoride. The concentration matters; for adults and children over 6, toothpaste typically contains 1000-1500 parts per million (ppm) fluoride. Children under 6 should use a smaller amount (pea-sized) with adult supervision to minimize swallowing, and toothpastes specifically for children often have slightly lower concentrations (though increasing evidence supports slightly higher levels even for young children, consult your dentist). **Fluoride mouthwashes** can be a useful addition to your routine, particularly if you are at higher risk of cavities (e.g., due to dry mouth, orthodontic treatment, or a history of decay). Mouthwashes containing fluoride provide an extra dose of this enamel-strengthening mineral. They are typically used after brushing and flossing, rinsing for about 30-60 seconds. However, mouthwash should be seen as a supplement to, not a replacement for, brushing and flossing. **Antiseptic mouthwashes** containing ingredients like chlorhexidine or essential oils can help reduce the overall bacterial load in the mouth, which might indirectly reduce the number of acid-producing bacteria. However, chlorhexidine is often prescription-strength, can stain teeth with long-term use, and is usually recommended for specific purposes like gum disease or after surgery, not routine cavity prevention unless advised by a dentist. For cavity prevention specifically, fluoride rinses are usually preferred. Other products that can help in prevention include **dental floss and interdental brushes** (essential for cleaning between teeth), **xylitol-containing products** (chewing gum, mints) which some studies suggest can reduce levels of Streptococcus mutans bacteria, and **sugar-free gum** in general (stimulates saliva). Your dentist may also recommend **high-concentration prescription fluoride products**, such as gels, rinses, or varnishes applied in-office, for individuals with very high cavity risk. The best products for you depend on your individual needs and risk factors, so it’s always best to discuss these options with your dentist or dental hygienist to tailor your preventative strategy. Using these products consistently is key to maintaining a healthy mouth.
What is the Best Toothpaste for Cavities?
When it comes to protecting your teeth from cavities and helping to manage the early stages of decay, the single most important ingredient to look for in a toothpaste is **fluoride**. Therefore, the “best” toothpaste for cavities is, quite simply, a **fluoride toothpaste**. Fluoride is scientifically proven to be effective in preventing tooth decay. As we’ve covered, it strengthens the enamel, making it more resistant to acid attacks from bacteria, and it helps to repair early damage (remineralization) before it turns into a full-blown cavity. When choosing a fluoride toothpaste, look for one that carries an endorsement from a recognized dental authority, such as the American Dental Association (ADA) Seal of Acceptance or similar endorsements from dental organizations in other countries. This seal indicates that the product has been tested and meets specific criteria for safety and effectiveness. For adults and children over six, the standard recommendation is toothpaste containing at least 1000 parts per million (ppm) of fluoride, and ideally between 1350 ppm and 1500 ppm for maximum benefit in a standard over-the-counter product. Children aged three to six should use a smaller, pea-sized amount of toothpaste with a fluoride concentration of at least 1000 ppm. Children under three should have their teeth brushed with just a smear of toothpaste containing at least 1000 ppm fluoride. It’s vital that children’s brushing is supervised to ensure they don’t swallow large amounts of toothpaste. Beyond the fluoride content, other features like sensitivity formulas, whitening agents, or specific flavors are matters of personal preference or secondary concerns compared to the primary need for effective fluoride delivery. If you are at high risk for cavities, your dentist might recommend a prescription-strength toothpaste with a higher concentration of fluoride (e.g., 5000 ppm), which provides an even stronger protective effect. So, focus on finding a toothpaste with an adequate fluoride concentration that you like the taste of and will use consistently, twice a day, as directed. The fluoride content is the key to its effectiveness against cavities; make sure fluoride is the active ingredient you prioritize when selecting your toothpaste.
What is the Best Mouthwash for Cavities?
While not a replacement for brushing and flossing with fluoride toothpaste, a **fluoride mouthwash** can be a beneficial *adjunct* to your oral hygiene routine, particularly if you have a higher risk of developing cavities. Just like fluoride toothpaste, a fluoride mouthwash works by bathing the teeth in fluoride, helping to strengthen the enamel and promote remineralization, making teeth more resistant to acid attacks. Rinsing with a fluoride mouthwash after brushing (or at a different time of day, as sometimes recommended to maximize fluoride exposure) can provide an extra layer of protection, especially for individuals who might struggle with thorough brushing and flossing, have orthodontic appliances, experience dry mouth, or have a history of multiple cavities. Look for over-the-counter mouthwashes that contain fluoride and carry an endorsement from a recognized dental association, ensuring their effectiveness and safety. Common fluoride compounds found in rinses include sodium fluoride or stannous fluoride. The concentration of fluoride in over-the-counter rinses is typically lower than in toothpaste, but still beneficial when used regularly. It’s generally recommended to use fluoride mouthwash *after* you’ve brushed and flossed, and avoid eating or drinking for at least 30 minutes afterward to allow the fluoride to remain on the tooth surfaces. Antiseptic mouthwashes that reduce overall bacterial count might also contribute indirectly to cavity prevention by reducing the acid-producing bacteria, but fluoride rinses are more directly targeted at strengthening the tooth structure against decay. For individuals with a very high risk of cavities, a dentist might prescribe a stronger, higher-concentration fluoride rinse for daily or weekly use. However, it’s important to use mouthwash responsibly. Don’t swallow it, and fluoride rinses are generally not recommended for children under six years old due to the risk of swallowing too much fluoride. While mouthwash can be a helpful tool, remember it cannot remove the physical plaque and food debris that gets stuck between teeth – only flossing or interdental cleaning can do that effectively. So, choose a fluoride mouthwash as a complementary step if recommended by your dentist, but always prioritize brushing with fluoride toothpaste and cleaning between your teeth for comprehensive cavity prevention.
What Happens If You Leave a Cavity Untreated?
Ignoring a cavity is like ignoring a tiny crack in a dam; it will only get worse, and the consequences can be significant. Unlike many minor bodily ailments that might resolve on their own, a tooth cavity is a progressive disease process that, once a hole forms, will not stop or heal naturally. If you leave a cavity untreated, the decay process will continue its relentless march deeper into the tooth structure. It starts in the enamel, then penetrates the dentin, which is softer and decays much more rapidly. As the decay spreads in the dentin, it undermines the overlying enamel, making it prone to fracture. Eventually, if the decay isn’t stopped, it will reach the pulp, the innermost part of the tooth containing the nerves and blood vessels. This is where the situation becomes more serious. When bacteria from the cavity reach the pulp, they cause infection and inflammation (pulpitis), leading to significant pain. If the infection is not treated, the pulp tissue will eventually die (necrosis). Once the pulp is necrotic, the tooth may temporarily stop hurting because the nerves are dead, but the infection is still present and can spread. Bacteria can travel through the root canals out of the tip of the root and into the surrounding bone and tissues, leading to the formation of a dental abscess – a pocket of pus. A dental abscess can cause severe pain, swelling in the gum, cheek, or jaw, fever, and general malaise. If left untreated, the infection from an abscess can spread to other parts of the body, potentially leading to serious, even life-threatening, systemic infections in the jaw bone, sinuses, brain, or bloodstream (sepsis). Beyond infection, leaving a cavity untreated weakens the tooth’s structure significantly, making it prone to fracture. Large sections of the tooth can break off, sometimes down to the gum line, making it impossible to restore the tooth with a simple filling or even a crown. Untreated decay can also spread to adjacent teeth, causing new cavities. Eventually, the tooth may become so damaged by decay or infection that it cannot be saved and must be extracted. This loss of a tooth can affect your ability to chew, your speech, your appearance, and can lead to surrounding teeth shifting, impacting your bite and potentially causing problems with the jaw joint (TMJ). In summary, leaving a cavity untreated is a gamble with high stakes, inevitably leading to worsening pain, infection, potential tooth loss, and serious health complications that could have been avoided with timely intervention. Don’t risk these severe outcomes.
Is It OK to Leave a Cavity Untreated?
Let’s be absolutely unambiguous here: **No, it is definitely *not* OK to leave a cavity untreated.** While it might be tempting to ignore a cavity, especially if it’s not causing pain yet, thinking it might go away or isn’t a big deal, this approach is fundamentally flawed and harmful to your oral and overall health. A cavity is a progressive disease process – it represents active bacterial infection and structural breakdown of the tooth. Once a cavity has formed, it will not heal or reverse on its own. It will only get larger and deeper over time. The longer you wait, the more tooth structure is destroyed. This means a small cavity that could have been fixed quickly and inexpensively with a simple filling might progress to require a more complex, time-consuming, and costly treatment like a root canal and crown, or eventually, extraction. Beyond the increasing complexity and cost of treatment, delaying care significantly raises the risk of complications. As the decay reaches the tooth’s pulp, you’ll likely experience significant pain. The bacteria can cause a severe infection (abscess) in the pulp, bone, and surrounding tissues. Dental infections can be serious and potentially spread to other parts of the body, leading to systemic health issues. A severely decayed tooth can also fracture, sometimes irreparable. Leaving a cavity untreated is choosing a path that leads to worsening pain, higher treatment costs, increased risk of infection and systemic health problems, and a greater likelihood of eventually losing the tooth. There is literally no upside to delaying treatment for a diagnosed cavity. Even if you’re concerned about the cost or anxiety associated with dental visits, addressing the cavity early is always the better option for your health and your wallet in the long run. Don’t make the mistake of thinking an untreated cavity is benign; it is an active disease process that requires professional care.
How Fast Do Cavities Grow?
The speed at which a cavity progresses isn’t a fixed, predictable timeline; it varies considerably from person to person and even from tooth to tooth within the same mouth. Several factors influence the rate of decay. These include: **Oral Hygiene:** Poor brushing and flossing allow plaque to build up quickly, providing a constant source of acid and accelerating decay. Excellent hygiene slows it down. **Diet:** Frequent consumption of sugary and acidic foods and drinks provides bacteria with a constant fuel source, speeding up acid production and decay. **Saliva Flow and Composition:** Saliva helps neutralize acids and remineralize enamel. People with dry mouth or saliva with poor buffering capacity are at higher risk of rapid decay. **Fluoride Exposure:** Adequate exposure to fluoride (from toothpaste, water, treatments) makes enamel more resistant to acid and promotes repair, significantly slowing decay progression. **Tooth Location and Structure:** Cavities in deep pits and fissures or on root surfaces (which are softer than enamel) tend to progress faster than those on smooth enamel surfaces. Decay in dentin is faster than in enamel because dentin is softer. **Genetics and Individual Susceptibility:** Some people’s teeth may be inherently more or less resistant to decay, although lifestyle factors are usually more significant. **Age:** Root cavities in older adults with gum recession can progress very quickly. **General Health:** Conditions like diabetes or medications causing dry mouth can accelerate decay. In some individuals with poor hygiene and high sugar intake, a cavity can potentially progress from the enamel into the dentin within a matter of months, sometimes causing rapid destruction. In others with good hygiene and low sugar intake, it might take years for a white spot to progress into a detectable cavity, or it might even be arrested. Decay tends to spread laterally once it hits the dentin before continuing its downward path towards the pulp, sometimes creating a large area of decay under a small enamel opening. Once the decay reaches the pulp, the progression of infection can be rapid. So, while there’s no precise “cavity growth rate,” it’s generally understood that decay is a progressive process that *will* continue if left untreated, and the speed is heavily influenced by the oral environment. A small cavity today *will* be a larger cavity in the future, leading to more significant problems down the line. Don’t assume a slow start means it will stay small indefinitely.
Do Cavities Stay for Life if Untreated?
Yes, this is a fundamental truth about cavities: **Once a cavity forms, it stays for life if left untreated by a dental professional.** A tooth cavity is a permanent structural defect, a physical loss of tooth material caused by bacterial acid erosion. Human teeth, particularly the enamel and dentin, do not have the capacity to regenerate and rebuild lost tissue once a hole has formed. Think of it like losing a piece of glass from a window – the window pane cannot magically recreate the missing shard. While the very earliest stage of decay (demineralization or a white spot) *can* potentially be reversed through remineralization (redepositing minerals onto the weakened enamel surface) *before* the surface breaks down, a true cavity, a discernible hole, is past this point of natural reversal. If you leave a cavity untreated, it won’t get smaller, it won’t disappear, and it certainly won’t heal over. Instead, the decay process initiated by the bacteria and acid will continue to eat away at the tooth structure, making the cavity progressively larger and deeper over time. This untreated cavity will eventually lead to symptoms like pain and can cause serious complications such as infection, abscess formation, weakening of the tooth leading to fracture, and potentially the loss of the tooth entirely. Even if the tooth becomes non-vital (the nerve dies), the physical cavity itself remains, and the infection associated with the necrotic pulp can spread. So, yes, unless it is treated by a dentist who removes the decay and restores the tooth, a cavity remains a permanent area of damage in your tooth, a constant vulnerability that will worsen over time. The only way to get rid of a cavity permanently is through professional dental treatment.
What Happens if You Have a Cavity for a Long Time?
Having a cavity for a significant period without getting it treated is essentially allowing a slow-motion disaster to unfold within your tooth. The decay will relentlessly march through the tooth’s layers. It starts in the enamel, which can take some time depending on hygiene and diet. Once it hits the softer dentin, it accelerates and spreads more rapidly, often undermining the enamel above. As the decay deepens, you’ll likely experience increasing sensitivity, particularly to cold, hot, and sweet things. Eventually, the decay will reach the tooth’s nerve center, the pulp. This usually leads to pulpitis, causing significant pain – a throbbing, persistent toothache that might worsen at night or when biting. At this point, a simple filling is no longer sufficient; the tooth will likely require a root canal to save it, involving the removal of the infected pulp tissue. If the infection in the pulp is not treated, it can spread out through the root tips and into the surrounding bone and tissues, forming a dental abscess. This is a serious infection that can cause severe pain, swelling of the face or jaw, fever, and a bad taste in the mouth if the abscess drains. Left untreated, a dental abscess can lead to the destruction of the surrounding bone and can spread infection to other parts of the head, neck, or even the bloodstream (sepsis), which can be life-threatening. Beyond infection, a long-standing cavity severely weakens the tooth structure. The tooth becomes brittle and prone to fracture, potentially breaking off large sections or splitting completely. If the tooth breaks below the gum line or is too severely compromised by decay and infection, it may become unrestorable and require extraction. Furthermore, an untreated cavity can act as a reservoir for bacteria, potentially contributing to gum disease and even facilitating the formation of new cavities on adjacent teeth. So, a cavity left untreated for a long time transforms from a relatively simple problem into a potentially complex, painful, expensive, and even dangerous situation involving severe pain, widespread infection, significant tooth destruction, and possible tooth loss, with potential impacts on overall health. Timely treatment is critical to avoid these severe outcomes.
Severe Tooth Cavity Complications and Treatments
When tooth decay goes unchecked and progresses past the point where a simple filling is sufficient, the complications can become severe, and the required treatments more complex. The most significant complication arises when the decay reaches the dental pulp – the living tissue containing the tooth’s nerves and blood vessels, located in the center of the tooth (pulp chamber) and extending down into the roots (root canals). When bacteria from the cavity invade the pulp, it causes inflammation (pulpitis) and infection. This infection can be excruciatingly painful. If the infection is not addressed, the pulp tissue will eventually die (necrosis). Once the pulp is necrotic, the tooth may temporarily stop hurting because the nerves are dead, but the infection is still present and can spread. Bacteria can travel through the root canals out of the tip of the root and into the surrounding bone and tissues, leading to the formation of a dental abscess – a pocket of pus. A dental abscess can cause severe pain, swelling in the gum, cheek, or jaw, fever, and general malaise. If left untreated, the infection from an abscess can spread to other parts of the body, potentially leading to serious, even life-threatening, systemic infections in the jaw bone, sinuses, brain, or bloodstream (sepsis). Beyond infection, leaving a cavity untreated weakens the tooth’s structure significantly, making it prone to fracture. Large sections of the tooth can break off, sometimes down to the gum line, making it impossible to restore the tooth with a simple filling or even a crown. Untreated decay can also spread to adjacent teeth, causing new cavities. Eventually, the tooth may become so damaged by decay or infection that it cannot be saved and must be extracted. This loss of a tooth can affect your ability to chew, your speech, your appearance, and can lead to surrounding teeth shifting, impacting your bite and potentially causing problems with the jaw joint (TMJ). In summary, severe cavity complications require prompt and expert dental care to prevent further spread of infection, alleviate pain, and preserve as much natural tooth structure as possible. These complications highlight the critical importance of addressing cavities early.
What Causes a Root Canal to Be Necessary?
A root canal procedure becomes necessary when the soft, inner tissue of the tooth, known as the dental pulp, becomes irreversibly inflamed or infected. This usually happens as a direct consequence of deep, untreated tooth decay. As a cavity grows larger and deeper, it progresses through the outer layers of the tooth (enamel and dentin). Dentin contains tiny tubules that connect to the pulp. When the decay reaches the dentin, bacteria and irritants get closer to the pulp. Initially, this might just cause sensitivity or reversible inflammation (pulpitis). However, if the decay continues its advance and breaches the final barrier to the pulp chamber, bacteria can directly invade the pulp tissue. The pulp, being soft tissue housed within rigid walls, swells when it becomes inflamed or infected, but it has nowhere to expand. This leads to pressure and pain, which is often severe and persistent – this is irreversible pulpitis. The infection can eventually cause the pulp tissue to die (become necrotic). Once the pulp is necrotic, the infection is contained within the tooth’s root canal system and can spread out through the tip of the root into the surrounding bone and ligaments, forming an abscess. Other causes of pulpitis requiring root canal treatment include traumatic injury to the tooth (like a fracture or crack that exposes the pulp), extensive dental procedures on the tooth, or repeated dental work that irritates the pulp over time. However, deep decay is by far the most common reason. When the pulp is irreversibly damaged or infected, it cannot heal itself. Leaving it untreated will lead to excruciating pain, abscess formation, and potentially the loss of the tooth and spread of infection. A root canal procedure is the treatment designed to address this specific problem – removing the diseased pulp tissue, cleaning and disinfecting the inner tooth structure, and sealing it to save the tooth from extraction and eliminate the source of infection and pain. It’s a vital procedure for preserving teeth with damaged or infected pulp.
Root Canal Treatment or Tooth Removal Explained
When tooth decay or injury leads to irreversible damage or infection of the dental pulp, you’re typically faced with two primary options: root canal treatment or tooth removal (extraction). The choice depends on various factors, including the extent of the damage, the overall health of the tooth and surrounding bone, the patient’s general health, cost considerations, and the patient’s preference. **Root Canal Treatment** is a procedure aimed at saving the natural tooth. Learn about Root Canal Therapy. It’s performed when the pulp is inflamed or infected, but the tooth structure itself is still significantly intact and can be restored. The process involves cleaning out the infected pulp from the root canals, disinfecting the canals, and filling them. The goal is to eliminate the infection and prevent it from spreading, allowing the bone around the root to heal, while preserving the tooth’s place in the mouth. Root canal treated teeth, while no longer “alive” in the sense of having a nerve, remain functional, capable of chewing and maintaining the alignment of adjacent teeth. They usually require a filling and often a crown afterward for protection and restoration. The success rate of root canal therapy is generally high, allowing teeth to function for many years, sometimes a lifetime. **Tooth Removal (Extraction)** is the option chosen when the tooth is too severely damaged by decay, fracture, or periodontal (gum) disease to be saved with a root canal or other restorative procedures. If the decay has destroyed too much tooth structure, if there’s extensive bone loss supporting the tooth, or if a root canal has failed and reinfection has occurred, extraction might be the most practical or necessary option. Extraction eliminates the infected tooth and resolves associated pain and swelling. However, removing a tooth creates a gap in the smile. This gap can lead to surrounding teeth shifting, affecting the bite, causing issues with the jaw joint, and potentially leading to bone loss in the jaw over time. Therefore, after extraction, dentists usually recommend replacing the missing tooth with a dental implant Dental Implant (a titanium post surgically placed in the bone, topped with a crown), a dental bridge Dental Bridge (a false tooth anchored to adjacent teeth), or a partial denture Dentures. While extraction is sometimes unavoidable, preserving the natural tooth with a root canal is generally preferred when possible because it avoids the complications and costs associated with tooth loss and replacement, maintaining the integrity of your dentition.
Will Treatment for Tooth Cavities Be Painful?
It’s completely understandable to feel anxious about pain when facing dental treatment for a cavity. After all, you might already be experiencing pain *from* the cavity itself! However, modern dental techniques are designed to make the treatment process as comfortable as possible. For most common cavity treatments, particularly fillings and root canals, **local anesthesia** is used. This involves injecting a numbing agent into the gum tissue surrounding the tooth. This anesthetic blocks the pain signals from reaching the brain, effectively numbing the tooth and the surrounding area. During a filling, once the area is numb, you should not feel any sharp pain while the dentist removes the decay with a drill. You might feel pressure, vibration, or hear sounds, but the sensation of pain should be absent. Similarly, during a root canal, the area is thoroughly numbed. While the reason for the root canal (infected pulp) might have been causing significant pain beforehand, the procedure itself is done under anesthesia specifically to *relieve* that pain by removing the inflamed or infected tissue. You might feel some pressure or pushing sensations during the procedure, but not pain. Even tooth extractions are performed under local anesthesia, ensuring the removal itself is painless. For patients with significant anxiety, dentists may also offer conscious sedation (like nitrous oxide or oral sedatives) or even deeper sedation options to help them relax or feel less aware during the procedure. It’s true that you might experience some discomfort or sensitivity *after* the anesthetic wears off, particularly with deeper fillings, root canals, or extractions. This is part of the normal healing process as the tissues recover. Over-the-counter pain relievers (like ibuprofen or acetaminophen) are usually sufficient to manage this post-treatment soreness. Your dentist will provide specific aftercare instructions and pain management recommendations. So, while the *idea* of cavity treatment might seem painful, the actual procedures themselves are performed with effective pain control, making them significantly more comfortable than dealing with the pain of an untreated cavity. Don’t let fear of pain prevent you from seeking necessary treatment; modern dentistry is equipped to minimize discomfort.
Do Cavity Fillings Hurt?
Generally speaking, the process of getting a cavity filling **should not hurt** thanks to the use of local anesthesia. Before the dentist begins working on your tooth, they will administer a local anesthetic injection near the tooth being treated. This numbs the tooth, the gum tissue around it, and potentially part of your cheek or tongue on that side. Once the area is completely numb – which might take a few minutes after the injection, and the injection itself can feel like a small pinch or sting initially – the dentist will proceed to remove the decayed tissue using a dental drill. During this stage, you will likely feel pressure, vibration, or hear sounds, but you should not feel sharp pain. The drill only affects the hard tooth structure and decayed material; the nerve is either too deep to be affected by the drilling or is numbed by the anesthetic. After the decay is removed and the cavity is prepared, the filling material is placed. You might feel the dentist shaping and packing the material, but this is also typically painless. Once the filling is completed and hardened, the numbness will gradually wear off over a few hours. It’s common to experience some **post-filling sensitivity or discomfort** after the anesthetic wears off. The tooth might be sensitive to hot and cold temperatures, or biting pressure, especially if the cavity was deep or close to the nerve. This sensitivity is usually temporary and can last anywhere from a few hours to a few days or sometimes a couple of weeks. Over-the-counter pain relievers like ibuprofen can help manage this. If sensitivity persists or is severe, contact your dentist. In rare cases, issues can arise (e.g., the filling being too high, persistent nerve irritation), but the actual procedure of getting the filling while numbed is designed to be a pain-free experience. Communicate with your dentist during the procedure if you feel any sensation that indicates the area isn’t adequately numb; they can administer more anesthetic if needed.
Does a Root Canal Hurt?
It’s a widespread misconception, fueled by old stereotypes and negative experiences, that root canals are agonizing procedures. In reality, **a root canal is performed *because* you are in pain (usually from an infected pulp), and the procedure itself is designed to *relieve* that pain**. It’s done under local anesthesia, meaning the tooth and surrounding tissues are completely numbed before the procedure begins. The initial anesthetic injection might cause a brief sting, but once the numbness sets in, you should not feel sharp pain during the root canal procedure itself. The goal of the root canal is to access the tooth’s interior, remove the source of the pain (the inflamed or infected pulp tissue), clean and disinfect the root canal system, and then seal it off. While you might feel pressure, vibration, or hear sounds during the various steps (like using instruments to clean the canals), the removal of the nerve tissue and cleaning occurs in a numbed environment. In fact, many people report feeling relief as the infected pressure within the tooth is alleviated during the procedure. Similar to fillings, some **post-procedure discomfort or soreness** is common after a root canal, especially once the anesthesia wears off. This is due to the manipulation of the tissues around the tooth and the normal healing process. The jaw might also feel sore from being open during the procedure. This post-treatment pain is usually manageable with over-the-counter or prescription pain medication as recommended by your dentist or endodontist and typically subsides within a few days. Compared to the severe, persistent pain caused by an infected tooth nerve, the temporary discomfort after a root canal is usually minimal and signifies that the infection has been addressed and healing has begun. If you experience severe pain or swelling after a root canal, you should contact your dentist immediately, as this could indicate a complication. But the procedure itself is performed under effective pain control, aiming to resolve the painful infection and save the tooth. The relief from the original toothache is often the most significant outcome.
Is Tooth Extraction Painful?
Having a tooth extracted might sound daunting, conjuring images of forceful pulling and significant pain. However, like other dental procedures, **tooth extraction is performed under effective pain control, primarily local anesthesia, meaning the procedure itself is typically not painful.** Before starting, the dentist or oral surgeon will numb the tooth and the surrounding gum and bone tissue with a local anesthetic injection. You might feel a brief pinch or sting from the injection, but once the area is fully numb, you should not feel pain during the extraction. You will likely feel pressure as the dentist gently rocks the tooth to loosen it from the socket, and you might hear sounds associated with the instruments or the tooth loosening. These sensations are normal and indicate that the tooth is being removed, but they are not painful. If you feel any sharp pain during the procedure, raise your hand immediately so the dentist can administer more anesthetic. **Post-extraction pain and discomfort** are normal once the anesthesia wears off. This is because the extraction process causes trauma to the surrounding tissues. The severity of post-operative pain varies depending on the complexity of the extraction (e.g., a simple pull versus a surgical removal of an impacted tooth). Your dentist will provide instructions on how to manage this discomfort, which typically involves taking prescribed pain medication or over-the-counter pain relievers, using ice packs on the cheek, and following specific aftercare instructions regarding diet, cleaning the socket, and avoiding activities that could dislodge the blood clot (like smoking or using a straw, which can lead to a painful “dry socket”). Post-extraction pain is temporary and typically decreases significantly within a few days, although complete healing takes longer. While the extraction itself is done painlessly with anesthesia, managing the recovery discomfort is an important part of the process. Discuss pain management options with your dentist beforehand if you are concerned.
How Long Do Tooth Cavity Treatments Last?
The longevity of a dental restoration used to treat a cavity isn’t indefinite; it depends on several factors, but they are designed to last for many years. A filling or crown doesn’t make the tooth impervious to future problems, either around the restoration or elsewhere. The lifespan of a cavity treatment varies significantly based on the type of material used, the size and location of the restoration, the amount of stress the tooth endures (like chewing forces, teeth grinding), the patient’s oral hygiene habits, and whether new decay forms around the edges of the restoration. **Fillings**, the most common treatment for cavities, have varying lifespans depending on the material. Amalgam (silver) fillings are known for their durability and can last, on average, **10 to 15 years or even longer**. Composite (tooth-colored) fillings are also quite durable but may not last quite as long as amalgam under heavy chewing loads, typically lasting **7 to 10 years**, although newer materials and techniques are improving their longevity. Gold fillings are exceptionally durable and biocompatible and can last **15 to 20 years or much longer**. Porcelain (ceramic) fillings (inlays/onlays) can also be very durable, lasting **10 to 15 years or more**. Factors that can shorten the lifespan of a filling include clenching or grinding teeth (bruxism), chewing hard foods, developing new decay around the edge of the filling (recurrent decay), or the filling material breaking down or fracturing over time. **Crowns**, used for more extensive damage or after root canals, are generally very durable restorations designed to protect the entire tooth. They are typically made of porcelain, porcelain fused to metal, gold, or zirconia. A well-maintained crown can last, on average, **10 to 15 years or sometimes 20 years or more**. Like fillings, their lifespan is affected by oral hygiene (preventing decay around the crown margin), bite forces, clenching/grinding, and proper dental care. **Root canal treatment** itself, which addresses the infected pulp, is considered a permanent solution for the infection within the tooth. However, the tooth restored after a root canal (usually with a filling and a crown) relies on the integrity of the restoration and the remaining tooth structure. The success rate of root canal therapy combined with a proper restoration is high, with most teeth remaining functional for many years. The longevity ultimately depends on the quality of the root canal and the subsequent restoration, and the patient’s ongoing oral hygiene. Regular dental check-ups are essential for monitoring the condition of fillings, crowns, and root canal treated teeth, allowing the dentist to identify any issues early and potentially extend the life of the restoration or tooth. While dental restorations are robust, they are not maintenance-free and will eventually need to be repaired or replaced. Their longevity relies heavily on both the quality of the work and consistent patient care.
How Long Do Fillings Last?
The typical lifespan of a tooth filling varies significantly based on the material used, the size of the filling, the location of the tooth in the mouth (and the chewing forces it experiences), and the individual’s oral hygiene habits and diet. On average: **Amalgam (silver) fillings** are known for their durability and ability to withstand chewing forces. They are often placed in back teeth. Amalgam fillings generally last the longest of the common filling materials, typically ranging from **10 to 15 years**, and often remaining functional for much longer with good care, sometimes even decades. **Composite resin (tooth-colored) fillings** are popular for their aesthetic appeal, especially in visible areas. They bond directly to the tooth structure. While improving constantly, composite fillings may not be as durable as amalgam under very heavy chewing stress. Their typical lifespan is generally estimated to be around **7 to 10 years**, though this can vary widely based on placement and care. **Gold fillings** (inlays/onlays) are the most expensive but are also extremely durable, biocompatible, and resistant to corrosion. A gold filling can easily last **15 to 20 years or even much longer** if well-maintained, often considered the longest-lasting restorative material. **Porcelain or Ceramic fillings** (inlays/onlays) are aesthetic and durable, often custom-made in a lab. They typically last around **10 to 15 years** or more, offering a good balance of aesthetics and longevity. Factors that can cause any filling to fail or require replacement include: the development of new decay (recurrent caries) around the edges of the filling due to poor hygiene or frequent sugar exposure; the filling material fracturing or wearing down over time; the tooth structure around the filling fracturing; or the bond between the filling and the tooth failing. Chewing hard items, grinding or clenching teeth, and a highly acidic diet can all reduce the lifespan of a filling. Regular dental check-ups are important to monitor your fillings. Your dentist can spot issues like recurrent decay or marginal breakdown early, potentially allowing for a repair rather than a full replacement, and ultimately extending the life of your restoration. Fillings are a significant investment in your oral health and their durability is influenced by multiple factors.
Oral Hygiene and Care When a Tooth Cavity is Present
So, you know you have a cavity. Now what? Does your oral hygiene routine change? Can you even touch the tooth? It’s crucial to understand that while brushing and flossing cannot *fix* an existing cavity, maintaining excellent oral hygiene is absolutely vital when a cavity is present. Firstly, continuing to brush and floss thoroughly around the affected tooth is necessary for overall oral health. Skipping cleaning in that area will only allow plaque to build up on the *rest* of the tooth and adjacent teeth, increasing the risk of new cavities or gum disease. However, approach the tooth with the cavity gently. If the cavity is large or causing sensitivity or pain, aggressive brushing can irritate the area. Use a soft-bristled toothbrush and be gentle when cleaning around the visible cavity or area of discomfort. The goal is to remove plaque and food particles *from the surfaces around* the cavity, not to try and scrub the cavity away (which isn’t possible and will likely be painful). Flossing around the tooth is also important, especially if the cavity is located between teeth. Gently slide the floss down to the gumline and clean the adjacent tooth surfaces. If the floss shreds or catches in the cavity, be extra gentle to avoid irritating the gum or breaking off weakened tooth structure. Rinsing your mouth, especially after eating, can help remove food debris that might get trapped in the cavity. Warm salt water rinses can be particularly soothing if the area is inflamed or sensitive, and they help keep the area clean. Using a fluoride mouthwash, if recommended by your dentist, can also provide extra protection to the *remaining* healthy tooth structure and potentially help remineralize any early decay elsewhere in the mouth. The most important aspect of care when you have a cavity is **seeking professional dental treatment promptly**. While good hygiene is essential for preventing further decay, it does not address the existing cavity. The only way to manage a cavity effectively is to have a dentist remove the decayed material and restore the tooth. Maintaining good hygiene while you wait for your appointment will help keep the rest of your mouth healthy and prevent the cavity from worsening *as rapidly*, but it’s not a substitute for the necessary treatment. It’s about damage limitation and overall oral health maintenance while awaiting professional repair.
Is It OK to Brush a Cavity?
Yes, it is generally OK and even recommended to brush a tooth that has a cavity, but you need to do it **gently and mindfully**, not aggressively. The primary purpose of brushing is to remove plaque and food particles from the tooth surfaces. These are the very things that feed the bacteria causing the decay. While brushing won’t fill the hole or remove the decay within the cavity itself, it’s crucial for keeping the *rest* of the tooth surface clean and for cleaning the surfaces of surrounding teeth. Neglecting to brush around a tooth with a cavity will allow plaque to accumulate, potentially causing the existing cavity to worsen faster and increasing the risk of new cavities forming on the same tooth (around the existing one) or on adjacent teeth. When brushing a tooth with a cavity: **Use a soft-bristled toothbrush.** Hard bristles can be abrasive and potentially irritate the gum tissue around the cavity or even cause discomfort on the exposed dentin. **Be gentle around the cavity itself.** Avoid scrubbing aggressively. You’re not trying to “clean out” the hole; you’re trying to clean the surfaces *around* it. If the cavity is sensitive or painful, be particularly careful in that area. **Focus on removing plaque from the surfaces** of the tooth, especially near the gum line and on the chewing surfaces. If there’s a visible hole, food might get trapped in it. Gentle rinsing after brushing and eating can help dislodge trapped particles, but don’t try to force things out with a toothbrush. **Use fluoride toothpaste.** The fluoride in the toothpaste will help strengthen the enamel on the *remaining* healthy parts of the tooth and other teeth, providing protection against further decay elsewhere. So, while brushing doesn’t fix the cavity, it’s a necessary part of maintaining overall oral hygiene and preventing the situation from deteriorating further on the affected tooth and spreading to others. Just remember the emphasis on gentleness, especially if the tooth is symptomatic. Proper, gentle brushing is still a crucial part of caring for a tooth with a cavity while you await professional treatment.
What’s the Outlook for People with Cavities?
The outlook for someone with cavities is highly dependent on one major factor: **whether they seek timely professional dental treatment.** With prompt and appropriate care, the outlook is generally very good. Cavities are treatable, and the vast majority can be successfully repaired, allowing the affected teeth to remain functional for many years, often a lifetime. If a cavity is caught early, when it’s small and confined to the enamel or outer dentin, a simple filling is usually sufficient. The procedure is relatively straightforward, the tooth is restored, and with good ongoing oral hygiene and regular dental check-ups, the tooth can remain healthy. Even if the cavity is larger and requires a crown or root canal, these procedures have high success rates and can effectively save the tooth from extraction, eliminating pain and infection and restoring function. A tooth treated with a root canal and crowned can serve you well for many years. The key to a positive outlook after cavity treatment is **consistent follow-up care**. This means maintaining excellent daily oral hygiene (brushing twice daily with fluoride toothpaste, flossing daily), limiting sugary and acidic foods and drinks, and attending all recommended regular dental check-ups and cleanings. These preventative measures are crucial for preventing new cavities from forming on other teeth and preventing recurrent decay around existing restorations. Your dentist will also monitor your fillings, crowns, or root canal treated teeth during these visits to ensure they are in good condition and identify any potential issues early. On the other hand, the outlook for people who leave cavities untreated is poor. As discussed, untreated cavities will inevitably grow larger, cause pain and infection, potentially lead to serious systemic health problems, weaken the tooth to the point of fracture, and ultimately result in the loss of the tooth. Replacing a missing tooth is often more complex and expensive than treating the original cavity. So, while cavities are common, they are not a life sentence of dental problems. With timely diagnosis, appropriate treatment, and diligent preventative care, people with cavities can expect to manage the condition, save their teeth, and maintain good oral health for the long term. The future of your tooth (and your smile) after a cavity largely rests on the actions you take now to seek treatment and commit to preventative habits. A proactive approach yields a significantly better prognosis.
What Can I Expect If I Have Cavities?
If your dentist tells you that you have one or more cavities, don’t panic – it’s a common diagnosis, and in most cases, it’s a very manageable problem. Here’s a general idea of what you can expect: **1. Diagnosis and Explanation:** Your dentist will show you where the cavities are, perhaps using X-rays or an intraoral camera, and explain the extent of the decay. They will discuss the recommended treatment options based on the size and depth of each cavity, tailored to your specific needs. **2. Treatment Planning:** For small to moderate cavities, the recommended treatment will likely be a filling. For deeper cavities nearing the pulp, they might discuss the possibility of sensitivity or the need for a root canal if the pulp is affected. For very extensive decay, a crown or even extraction might be discussed. You’ll agree on a treatment plan that addresses all detected cavities. **3. Scheduling the Appointment(s):** You’ll schedule an appointment (or multiple appointments, depending on the number and complexity of the cavities) to have the treatment performed. Don’t delay scheduling, especially if you’re experiencing pain; timely treatment is crucial. **4. The Treatment Procedure(s):** For a filling, you’ll receive local anesthesia, the decay will be removed, and the tooth will be filled with the chosen material. For a root canal, the numbed tooth will be cleaned internally and sealed, likely followed by a crown later. Extraction involves numbing and careful removal of the tooth. Throughout the procedure, the dental team will work to ensure your comfort and answer any questions. **5. Post-Treatment Care:** After the anesthesia wears off, you might experience some temporary sensitivity or soreness, which can usually be managed with over-the-counter pain relievers as directed. Your dentist will give you specific instructions on caring for the treated tooth, including what to eat and drink, and how to brush and floss around the new restoration. **6. Ongoing Prevention and Maintenance:** Having cavities treated doesn’t make you immune to new ones. You’ll need to commit to consistent, excellent daily oral hygiene (brushing twice, flossing daily), limit sugar/acid frequency, and attend your regular dental check-ups and cleanings as recommended by your dentist. Your dentist will monitor the treated teeth and restorations during subsequent visits to ensure their longevity and detect any new issues early. Expect that the process will stop the decay in the treated areas and restore the tooth’s function, allowing you to keep your natural teeth healthy with continued care.
Understanding Other Meanings of “Cavity” in the Human Body
While our focus has been squarely on those unwelcome guests in your teeth, the word “cavity” has a broader meaning in the realm of human anatomy. It refers to a hollow space or a space within a solid structure. In the context of the human body, anatomical cavities are literally compartments or spaces within the body that contain organs. These cavities serve crucial functions, primarily protecting delicate internal organs from external shock and trauma, supporting them, and allowing them space to change size and shape (like the lungs expanding or the stomach filling). The major body cavities are typically lined with membranes that secrete lubricating fluid, reducing friction between the organs as they move. They are separated from each other by bones or muscles. Understanding these anatomical cavities is fundamental to fields like medicine, surgery, and physiology, as they define the locations of various organ systems. The human body is structured into several large and smaller cavities, providing organized compartments for its complex machinery. Without these protective and organizational spaces, our internal organs would be far more vulnerable to injury and wouldn’t function as efficiently within the body’s structure. From the space housing your brain to the compartments containing your digestive organs, these anatomical cavities are essential architectural features of the human form, distinct in purpose and location from the small, pathological holes we’ve been discussing in teeth, yet sharing the same root word meaning: a hollow space. Recognizing this broader definition helps clarify the different contexts in which the term “cavity” is used in biology and health.
What is a Cavity in the Human Body?
In the context of human anatomy, a “cavity” is a **hollow space or compartment within the body** that is typically filled with organs. These cavities are distinct areas defined by bones, muscles, or other tissues. They are not like the pathological hole in a tooth caused by decay; rather, they are natural, structural spaces that serve vital functions. The main body cavities are divided into two major groups: the dorsal (posterior) body cavity and the ventral (anterior) body cavity. The dorsal body cavity is located on the back side of the body and includes the Cranial Cavity (within the skull, housing the brain) and the Spinal Cavity (within the vertebral column, housing the spinal cord). The ventral body cavity is located on the front side of the body and is much larger. It is further subdivided by the diaphragm muscle into the Thoracic Cavity (above the diaphragm) and the Abdominopelvic Cavity (below the diaphragm). The Thoracic Cavity contains the lungs and the heart, among other structures, and is protected by the rib cage. The Abdominopelvic Cavity is a large space in the trunk that contains the abdominal organs (stomach, intestines, liver, pancreas, spleen, kidneys) and the pelvic organs (bladder, reproductive organs, rectum). These major cavities and their subdivisions provide essential space for organs, protect them from physical injury, and allow them room to expand and contract. They are lined by serous membranes (like the pleura, pericardium, and peritoneum) that produce lubricating fluid, enabling the organs to slide smoothly against each other during movements and bodily functions. These anatomical cavities are fundamental to the organization and protection of the body’s internal structures.
What is the Main Purpose of a Cavity in Anatomy?
The main purposes of anatomical cavities in the human body are multifaceted and essential for survival. Primarily, they serve as **protective spaces** for vital internal organs. The bony and muscular walls that define these cavities act as shields against external forces and trauma, much like a protective shell. For instance, the rigid skull encases the delicate brain in the cranial cavity, and the strong rib cage protects the heart and lungs within the thoracic cavity from external impacts. Secondly, anatomical cavities provide **space for organs to function and change size**. Organs like the lungs need to expand during inhalation, the stomach needs to stretch when filled with food, and the bladder needs to accommodate increasing volumes of urine. The cavities provide the necessary room for these changes without compressing surrounding structures excessively, ensuring proper physiological function. Thirdly, these cavities help to **compartmentalize organ systems**, providing organization and separating functionally distinct groups of organs. This organization helps prevent the spread of infection or disease from one system to another by creating natural barriers. Finally, many cavities are lined with **membranes that secrete lubricating fluids**. This fluid reduces friction between organs as they move against each other during bodily activities (like breathing, digestion, or the beating heart), allowing for smooth, efficient function and preventing wear and tear on organ surfaces. In essence, anatomical cavities are the body’s internal architecture, providing crucial protection, necessary space, logical organization, and smooth operation for our vital internal organs, ensuring overall bodily integrity and function.
Which Cavity Contains the Heart?
The heart, a vital organ responsible for pumping blood throughout the body, is located within the **Thoracic Cavity**. This large cavity is located in the chest, superior to the diaphragm, and is protected by the rib cage, sternum, and vertebral column. More specifically, the thoracic cavity is not just one open space; it is divided into several smaller compartments by membranes. The lungs are housed within the two lateral pleural cavities, one on the left and one on the right. The central compartment of the thoracic cavity, located in the space between the two pleural cavities, is called the **mediastinum**. This mediastinum is a complex region that contains several vital structures, including the trachea, esophagus, major blood vessels (such as the aorta and vena cavae), lymph nodes, and the thymus gland. The heart itself is situated within this mediastinum, slightly to the left of the midline. It is enclosed within a specialized fibrous sac called the pericardium. The potential space between the outer layer of the heart muscle (epicardium) and the inner layer of the pericardial sac is known as the pericardial cavity. This pericardial cavity contains a small amount of lubricating fluid that allows the heart to beat smoothly without friction against the surrounding tissues. So, while the heart is broadly located within the thoracic cavity, its immediate and specific anatomical home is the pericardial cavity, which is situated within the mediastinum, the central division of the thoracic cavity. This layered protection is essential for the heart’s continuous and vital function.
What Organs Are in Each Main Body Cavity?
Let’s take a quick tour of the major body cavities and the primary organs they house, illustrating the fundamental compartmentalization of the human body that provides organization and protection for its complex systems:
1. Dorsal Body Cavity: Located on the posterior (back) side of the body.
- Cranial Cavity: Located within the skull. It primarily houses the **Brain**, the central processing unit of the nervous system.
- Spinal Cavity (also called the Vertebral Cavity): Located within the vertebral column. It contains the **Spinal Cord**, which transmits nerve signals between the brain and the rest of the body.
2. Ventral Body Cavity: Located on the anterior (front) side of the body, much larger than the dorsal cavity. It is divided by the diaphragm.
- Thoracic Cavity: Located superior to the diaphragm, protected by the rib cage. This cavity is further subdivided.
* Pleural Cavities (two, left and right): Each houses a **Lung**, essential for respiration.
* Mediastinum (central region): Contains the **Heart** (within the pericardial cavity), the **Esophagus** (part of the digestive tract), the **Trachea** (windpipe), the **Thymus gland** (part of the immune system), and major **Blood Vessels** (like the aorta, superior and inferior vena cavae). - Abdominopelvic Cavity: Located inferior to the diaphragm, extending from the diaphragm down to the pelvic floor. It is also divided, though less distinctly, into:
* Abdominal Cavity (superior portion): Houses a wide array of digestive, excretory, and regulatory organs, including the **Stomach**, **Intestines** (small intestine and most of the large intestine), **Liver**, **Gallbladder**, **Pancreas**, **Spleen** (part of the immune system), **Kidneys**, and **Adrenal Glands**.
* Pelvic Cavity (inferior portion, within the bony pelvis): Houses organs of the urinary, reproductive, and lower digestive systems, such as the **Urinary Bladder**, portions of the **Large Intestine** (rectum and sigmoid colon), and internal **Reproductive Organs** (uterus, ovaries, fallopian tubes in females; prostate gland, seminal vesicles, parts of the vas deferens in males).
These main cavities and their subdivisions provide essential organizational structure, protection, and space for expansion and movement for the body’s vital internal organs, facilitating their complex physiological functions in a protected environment.
Frequently Asked Questions About Cavity
Alright, let’s wrap this up by hitting those most common, burning questions you might still have swirling around. We’ve delved deep into the nitty-gritty of what cavities are, where they come from, what they look like, and how professionals tackle them. But sometimes, you just need the punchy, direct answer. These are the queries that pop up most often when people start thinking about those troublesome holes in their teeth. We’ll revisit the key takeaways, providing concise summaries drawn from the detailed information we’ve covered, because clarity is king, especially when it comes to your health. Think of this as the quick-reference guide, perfect for solidifying your understanding or sharing the basics with a friend. From the fundamental definition to the crucial question of self-healing and treatment, we’ll hit the highlights one more time, reinforcing the vital importance of professional dental care and consistent preventative habits. So, lean in, and let’s knock out these FAQs, leaving you armed with confidence and knowledge about protecting your smile. This section consolidates the essential information from the previous sections into easy-to-digest questions and answers, providing quick access to the most important facts about tooth cavities and their management.
What is a Cavity?
A cavity, also known as dental caries or tooth decay, is **a permanently damaged area on the surface of a tooth that develops into a small opening or hole.** It is the result of a progressive disease process where acids produced by bacteria in plaque break down the tooth’s hard outer layers (enamel and dentin). Think of it as structural damage to the tooth, a literal void created by the decay. While often referred to simply as a “hole,” it represents a significant area of demineralized and broken-down tooth tissue caused by ongoing bacterial activity and acid erosion. It starts microscopically as mineral loss (demineralization), which can sometimes appear as a white spot, and progresses to a physical breakdown of the tooth surface, forming the cavity itself. Cavities can vary in size and depth, ranging from small pits to large areas of destruction that can affect multiple tooth surfaces. They are a sign that the tooth structure has been compromised by decay and, once formed, require professional intervention to remove the decayed material and restore the tooth’s integrity. A cavity is not just a passive hole; it’s an area of active disease where bacteria can continue to proliferate and extend the damage deeper into the tooth if left untreated. Therefore, identifying and treating a cavity is essential to stop the disease process and prevent further destruction of the tooth and potential infection of the pulp.
What Causes Cavities?
Cavities are caused by a complex interaction between several factors present in your mouth over time. The primary culprits are **acid-producing bacteria** that live in the sticky film on your teeth called plaque. These bacteria feed on **sugars and other fermentable carbohydrates** from the foods and drinks you consume. As they metabolize these substances, they produce **acids** as a waste product. These acids attack the minerals in your tooth enamel, causing demineralization and weakening the tooth structure. If these acid attacks happen frequently (due to frequent snacking or sipping on sugary/acidic drinks) and are not balanced by factors that promote remineralization (like saliva and fluoride), the enamel will eventually break down, leading to the formation of a cavity. Risk factors that contribute to this process include poor oral hygiene (not removing plaque regularly), a diet high in sugars and frequent snacking, inadequate fluoride exposure (toothpaste, water), dry mouth (reduced saliva flow), and the presence of deep pits and fissures on tooth surfaces that trap food and bacteria. In essence, cavities are caused by an imbalance in the mouth where acid attacks from bacteria feeding on sugar overpower the tooth’s natural defenses and repair mechanisms, leading to the breakdown of the tooth structure and the creation of a hole. It’s a direct consequence of the oral environment created by a combination of bacterial presence, diet, and cleaning habits.
What Are the Symptoms of Cavities?
The symptoms of a cavity can vary widely depending on its size and depth, and many cavities, especially in their early stages, cause no symptoms at all. However, as decay progresses, common symptoms may include: **Sensitivity:** A sharp or fleeting discomfort when consuming hot, cold, or sweet foods and drinks. This often occurs when the decay reaches the dentin layer beneath the enamel. **Pain:** A toothache, which can range from a dull ache to sharp, throbbing, or persistent pain. Pain usually indicates that the decay has reached or is close to the pulp (nerve) of the tooth, causing inflammation or infection. The pain might be spontaneous or worsen when biting down, or particularly troublesome at night. **Visible Changes:** A white spot (early demineralization), a brown or black spot, or a noticeable pit or hole on the tooth surface. Sometimes, decay between teeth can cause a dark shadow to be visible. **Roughness:** Feeling a rough spot or edge on the tooth surface with your tongue. **Bad Breath or Bad Taste:** An unpleasant odor or taste coming from the affected tooth, caused by bacteria and trapped debris within the cavity. It’s crucial to remember that the absence of pain does not mean the absence of a cavity. Many cavities are detected by dentists during routine check-ups using visual examination, probing, and X-rays before they cause any noticeable symptoms. If you experience any of these signs, or simply suspect something isn’t right with a tooth, it’s important to see a dentist for a proper diagnosis.
Can a Cavity Heal on Its Own?
**No, an established tooth cavity – a physical hole or structural breakdown in the tooth’s enamel or dentin – cannot heal on its own.** Once the tooth structure has been physically lost, it cannot regenerate naturally. While the very earliest stage of decay, which involves the loss of minerals from the enamel surface (demineralization or a white spot), can potentially be reversed or arrested with improved oral hygiene, increased fluoride exposure, and dietary changes before a hole forms, this natural repair process (remineralization) is insufficient to rebuild missing tooth structure once a cavity has developed. Think of a cavity as a permanent scar or void left by the decay process. Leaving a cavity untreated will not result in it getting smaller or disappearing; instead, the decay process will continue to eat away at the tooth, making the cavity larger and deeper over time, leading to pain, infection, and potential tooth loss. Therefore, once a cavity is diagnosed, it requires professional dental treatment – such as a filling, crown, or root canal – to remove the decayed material, stop the progression of the disease in that tooth, and restore the tooth’s structure and function. Relying on home remedies or hoping a cavity will heal itself is dangerous and leads to delaying necessary care, often resulting in more complex problems down the line.
How Do Dentists Treat Cavities?
Dentists treat cavities by first **removing all the decayed and damaged tooth tissue** using dental drills and hand instruments. The goal is to eliminate the infected and softened tooth structure completely, leaving behind only healthy tooth material. Once the decay is removed, the resulting space (the prepared cavity) is cleaned and then **filled with a restorative material** to seal the tooth and restore its shape, strength, and function. The most common treatment for small to moderate cavities is a **filling**, using materials like composite resin (tooth-colored) or amalgam (silver). For larger cavities where significant tooth structure is missing, the dentist might recommend an **onlay or a crown**, which covers a larger portion or the entire visible part of the tooth after the decay is removed, providing greater support and protection. If the decay has reached the tooth’s pulp (nerve), causing irreversible inflammation or infection, the treatment required is a **root canal procedure**, which involves removing the infected pulp, cleaning and sealing the interior of the tooth’s roots. After a root canal, the tooth usually needs a filling and often a crown for protection. In cases of very severe decay where the tooth cannot be saved by any of the above methods, **tooth extraction** (removal) is the final option, followed by discussion of replacement options like an implant, bridge, or denture. All these treatments are performed using local anesthesia to ensure the patient’s comfort throughout the procedure. The specific treatment plan is tailored to the individual cavity’s size, location, and depth, aiming to preserve as much natural tooth structure as possible while eliminating the decay and restoring the tooth’s health and function.