Table of Contents
ToggleKey Takeaways
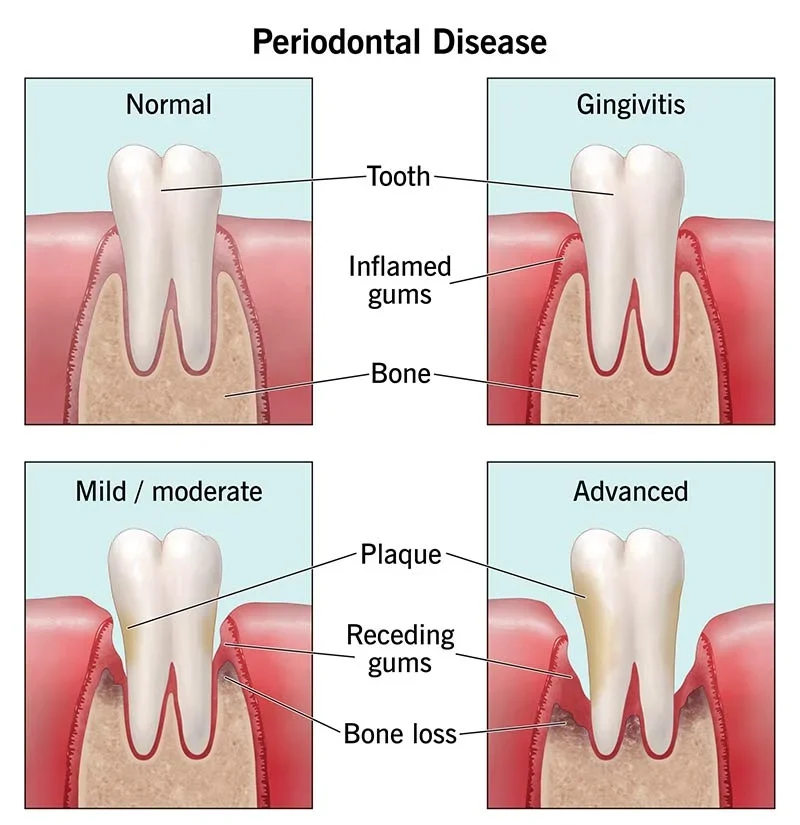
- Gum disease is a serious bacterial infection affecting tooth support structures.
- It starts as reversible *gingivitis* and can progress to irreversible *periodontitis*.
- Early detection via specific warning signs is **crucial** for successful treatment.
- Common early signals include **bleeding gums**, redness, and swelling.
- Later signs involve gum recession, persistent bad breath, tooth looseness, and bone loss.
- Ignoring symptoms can lead to tooth loss and may impact overall systemic health.
- Consulting a **dental professional** is essential if you notice any signs.
sign of gum disease: What Are the Warning Signs You Shouldn’t Ignore?
Look, let’s be blunt. Gum disease isn’t something you just shrug off like a slightly off-key karaoke performance. It’s a serious bacterial infection that attacks the tissues supporting your teeth, a slow-burn kind of crisis that, left unchecked, can lead to teeth loosening, falling out, and a cascade of health issues far beyond your mouth. Think of your gums and the underlying bone as the foundation of your smile – sturdy, reliable, essential. Gum disease, scientifically known as periodontal disease, is like structural rot setting in. It typically begins as gingivitis, the milder, often reversible form where inflammation rears its angry head, usually caused by plaque buildup along the gumline. This sticky film of bacteria is the primary culprit, turning your once-healthy tissue into a battleground. If this early skirmish isn’t decisively won through proper oral hygiene and professional cleaning, the infection can escalate into periodontitis. This is the serious, often irreversible phase where the bacteria burrow deeper, causing the gums to pull away from the teeth, forming pockets that collect more bacteria, leading to the destruction of the bone and connective tissue holding your teeth in place. The truly tricky part? Gum disease, especially in its initial stages, can be remarkably subtle. It doesn’t always scream for attention with throbbing pain. It might start with the soft whispers of bleeding during brushing, or a slight swelling that you barely notice. This quiet entry is precisely why early detection is absolutely paramount. Catching it when it’s just gingivitis means you can often reverse the damage. Letting it slide into periodontitis means you’re managing a chronic condition with permanent consequences. Ignoring the warning signs, no matter how faint they seem, is like hearing a faint smoke alarm and deciding it’s probably just the neighbours burning toast. By the time you see the flames, the damage is significantly harder, maybe even impossible, to undo entirely. Understanding what those early signals are, and perhaps more importantly, *not* dismissing them, is your first and best line of defence against losing not just your teeth, but potentially impacting your overall health. Your gums are giving you signals; it’s time to tune in and listen.
sign of gum disease: How to Identify the Early Warning Signs?
Decoding the language of your gums requires a bit of observation, a willingness to pay attention to the details often overlooked in the morning rush of brushing and flossing. Gum disease doesn’t typically announce itself with a dramatic flourish; its early manifestations are often quiet, subtle shifts that are easy to rationalise away or simply miss altogether. At its core, gum disease is an inflammatory response to bacterial plaque, that sticky, colourless film that constantly forms on your teeth. When this plaque isn’t effectively removed through diligent brushing and flossing, the bacteria within it produce toxins that irritate the gum tissue. This irritation triggers an inflammatory reaction – the body’s natural defence mechanism kicking into gear. This initial stage, gingivitis, is your body sending out preliminary flares. The gums become inflamed, which is why you might see changes in their colour, texture, or behaviour. These early signs are the crucial window of opportunity. Recognising them allows for prompt action, often leading to a full reversal of the condition. However, because gingivitis usually isn’t painful, people frequently ignore it. They might see a little pink in the sink after brushing and assume they were just brushing too hard, or notice a slight puffiness and attribute it to a lack of sleep. This complacency is dangerous. Early detection hinges on being observant and knowing what to look for. It requires a degree of self-awareness about your oral health baseline – understanding what *healthy* gums feel and look like for *you*. The symptoms, though subtle individually, collectively paint a picture that shouldn’t be dismissed. They are your gums’ way of saying, “Hey, something isn’t right down here! We’re under attack!” Think of it as a dental early warning system. Are you paying attention, or are you hitting the snooze button on your oral health? Spotting these initial signals before the problem entrenches itself and progresses to more severe periodontitis is the game-changer. It’s the difference between a relatively simple fix and a complex, ongoing battle. So, let’s peel back the layers and understand exactly what those early, crucial signals look like.
How to know if you have gum disease?
Determining whether you have gum disease isn’t always as straightforward as diagnosing a cavity; it requires a combination of self-awareness and professional evaluation. While you can certainly conduct a basic ‘self-check’ at home, relying solely on your own assessment can be misleading, especially in the early stages where symptoms are mild and can be misinterpreted. Your home inspection should involve a visual check and an awareness of sensations. Look at your gums in the mirror – are they consistently pink and firm, or are there areas of redness, swelling, or tenderness? Do they look shiny or puffy? Gently probe the gumline with a clean finger – does it feel sore? Do you notice any part of the gum pulling away from a tooth, making the tooth appear longer? Pay close attention when you brush and floss. Is there *any* amount of bleeding? Even a little pink on your toothbrush or floss string is a warning sign, contrary to the old belief that bleeding meant you were brushing too hard. Notice your breath throughout the day – is there a persistent bad odour that doesn’t go away after brushing? These self-checks are invaluable for raising your suspicion and prompting you to seek professional advice. However, they cannot replace a dental examination. A dentist or periodontist uses specific tools and techniques to accurately diagnose gum disease. They will perform a periodontal probing, using a small ruler to measure the depth of the pockets between your teeth and gums. Healthy pockets are typically 1-3 millimetres deep. Deeper pockets indicate that the gum has detached from the tooth root due to infection. They will also examine your gums for inflammation, bleeding, and recession, assess tooth mobility, and take X-rays to check for bone loss around the teeth, which is a hallmark of periodontitis. A professional diagnosis is absolutely necessary because they can identify the presence and *severity* of the disease, differentiate it from other oral conditions, and determine the underlying causes and risk factors specific to you. Your home observations are the alarm bell, but the dental professional is the one who confirms the nature of the emergency and charts the course for intervention. Don’t guess about your gum health; get it professionally assessed.
What are bad signs in gums?
Identifying “bad signs” in your gums involves recognising deviations from the state of health – specific visual and tactile indicators that suggest inflammation, infection, or damage is occurring. Healthy gums, regardless of your ethnicity (which can influence the natural shade from pale pink to darker, more pigmented tones), share certain key characteristics: they are typically firm to the touch, fit snugly around the neck of each tooth, and do not bleed during routine brushing or flossing. They have a matte appearance, sometimes described as resembling orange peel texture, rather than being puffy or shiny. Bad signs are essentially the opposite of this healthy state, manifesting in various ways depending on the severity and progression of the disease. One of the most common bad signs is a change in colour – healthy pink gives way to angry redness or a purplish hue, indicating inflammation. Another significant visual indicator is swelling or puffiness; the gum tissue appears enlarged, often losing its defined contour and looking smooth and shiny. Tenderness or soreness when touched is a tactile sign that often accompanies inflammation. Bleeding is arguably one of the most critical and frequently overlooked bad signs; any bleeding, whether during brushing, flossing, or even spontaneously, is a strong indicator of inflamed gums compromised by bacterial infection. Recession, where the gum tissue pulls away from the tooth, is a clear bad sign, making the tooth look longer and potentially exposing the sensitive root surface. While more associated with advanced stages, the presence of pus between the gums and teeth, sometimes noticeable when pressing on the gum, is an undeniable sign of active infection. Chronic bad breath or a persistent bad taste in your mouth that isn’t resolved by brushing can also be a bad sign, often caused by the volatile sulfur compounds produced by bacteria trapped in periodontal pockets. It’s crucial to understand that these signs can vary in their intensity and combination. Someone with early gingivitis might only show slight redness and bleeding, while a person with advanced periodontitis could exhibit severe recession, pus, and significant tooth mobility. The key takeaway is that any deviation from your normal, healthy gum appearance and feel should be noted and investigated. Don’t ignore these signals; they are your body’s way of flagging a potential problem that requires attention.
Symptoms of gum disease include:
The catalogue of gum disease symptoms is varied and provides a roadmap to understanding the state of your oral health, encompassing everything from subtle visual cues to more pronounced discomfort and functional issues. While not everyone will experience every symptom, the presence of even one or two should trigger suspicion and prompt a dental visit. At the top of the list, because it’s often the earliest and most common, is bleeding gums. This isn’t normal; healthy gums shouldn’t bleed from routine mechanical cleaning. Bleeding indicates inflammation and fragile tissue, a response to bacterial irritation. Next is swollen, red, or tender gums. Inflammation causes tissues to become engorged with blood and fluid, making them appear redder, puffier, and sensitive to touch. This swelling can make the gums look smooth and shiny rather than having the typical stippled texture. Gum recession is another key symptom, where the gum line moves down, making the teeth appear longer. This happens as the underlying supporting tissues are lost, causing the gum to pull away. Exposed tooth roots can lead to increased tooth sensitivity, especially to hot and cold temperatures, because the enamel-covered crown is protected, but the root surface is not. Persistent bad breath (halitosis) or a bad taste in your mouth is a frequently reported symptom that is often resistant to standard oral hygiene methods. This is due to the anaerobic bacteria thriving in deep gum pockets, releasing foul-smelling waste products. As the disease progresses and the bone supporting the teeth is lost, you might notice changes in the way your teeth fit together when you bite, or even that your dentures no longer fit properly. In more advanced stages, the loss of support leads to loose or shifting teeth. You might notice small gaps appearing between teeth that weren’t there before. The formation of pus between the teeth and gums is a definitive sign of active infection, often accompanied by pain and swelling. Finally, while less common in early stages, pain when chewing can occur if the disease has significantly impacted the stability of the teeth or if there are abscesses present. It’s vital to remember that gum disease can progress silently, particularly in smokers or individuals with certain systemic conditions, meaning you might have advanced disease with surprisingly few noticeable symptoms. Therefore, recognising this comprehensive list of potential indicators and understanding the ‘why’ behind them is crucial for taking proactive steps towards diagnosis and treatment.
Exploring the Beginning Stages and Early Signs of Gum Disease
The journey of gum disease typically begins quietly, in a realm often overlooked: the subtle inflammation known as gingivitis. This is the entry point, the earliest manifestation of the body’s reaction to bacterial overload along the gumline. Think of it as the initial skirmish in the war against oral bacteria. This stage is almost universally caused by the inadequate removal of dental plaque – that tenacious, biofilm-forming colony of microbes that accumulates on tooth surfaces, particularly near where they meet the gums. When plaque lingers, the bacteria within it proliferate and release toxins that irritate the delicate gum tissue. In response, the body mounts an inflammatory defence, increasing blood flow to the area, which leads to the characteristic signs of gingivitis. Critically, at this stage, the infection is generally confined to the gum tissue itself. It hasn’t yet breached the deeper structures – the periodontal ligaments that anchor the teeth to the bone, or the alveolar bone that forms the tooth sockets. This confinement is precisely what makes gingivitis potentially reversible. Remove the cause (the plaque), and the inflammation subsides, allowing the gum tissue to heal and return to a healthy state. The common characteristics of gingivitis are therefore centred around this localised inflammation: changes in colour, texture, and a tendency to bleed easily. While it might not sound dramatic, identifying and addressing gingivitis is perhaps the most important step you can take in preventing serious periodontal issues down the line. It’s the clear warning flare before the situation escalates into the far more damaging and complex condition of periodontitis, where the support structures for your teeth begin to erode, leading to irreversible consequences. Understanding this initial phase and knowing what to look for is paramount for maintaining long-term oral health. It’s about recognising the early whispers of trouble before they become a roar.
What is the early stage of gum disease?
The early stage of gum disease is known specifically as gingivitis. This is the initial inflammatory response of the gums to the presence of bacterial plaque that has accumulated along the gumline. Imagine plaque as a tiny, thriving city of bacteria on the surface of your teeth. If this city isn’t regularly disrupted and removed through effective brushing and flossing, it expands, particularly into the small crevice (the sulcus) between the tooth and the gum. The bacteria within the plaque produce metabolic byproducts and toxins that are profoundly irritating to the surrounding gum tissue. In response to this irritant, the body triggers an inflammatory process. This is a protective mechanism, bringing immune cells and increased blood flow to the area to try and combat the bacterial insult. However, this inflammation is also what causes the visible and palpable signs of gingivitis. At this stage, the key distinguishing feature is that the damage is *limited* to the soft gum tissue. The infection and inflammation have not yet progressed below the gumline to affect the periodontal ligament, which connects the tooth root to the bone, or the alveolar bone itself, which provides the socket structure for the tooth. This is absolutely crucial because it means the support system for your teeth is still intact. Because the deeper structures are unaffected, gingivitis is often fully reversible. By diligently removing the plaque through improved brushing and flossing techniques, and typically with the help of a professional dental cleaning (scaling) to remove hardened plaque (calculus or tartar), the inflammation can subside, and the gum tissue can return to health. There is usually no bone loss or irreversible attachment loss at this stage. Therefore, recognising gingivitis early is paramount. It represents a critical opportunity to intervene with relatively simple, non-surgical methods and prevent the progression to the more destructive and complex stages of periodontitis, where the supporting bone and connective tissues *are* compromised, leading to potentially irreversible damage and tooth loss.
What are two early signs of gum disease?
When it comes to the absolutely earliest and most commonly noticeable indicators that something might be amiss with your gums, two signs consistently stand out from the crowd, serving as critical red flags that demand your attention. These are bleeding gums and redness/swelling of the gum tissue. Let’s break these down, as they are the fundamental distress signals of gingivitis, the initial stage of gum disease. First, bleeding gums. This is perhaps the most overlooked yet significant early sign. Healthy gums should not bleed when you brush or floss effectively. Period. The act of brushing or flossing is a normal mechanical process; if it causes bleeding, it indicates that the gum tissue is inflamed, weakened, and fragile due to the presence of bacterial plaque and the body’s inflammatory response. Even a tiny bit of pink on your toothbrush or floss is a warning. It’s not a sign that you’re brushing too hard; it’s a sign that your gums are irritated by bacteria. This bleeding can be startling the first time it happens, but many people unfortunately become accustomed to it and dismiss it, which is a serious mistake. It signifies that the barrier function of your gums is compromised. The second key early sign is redness and swelling. Healthy gums are typically a shade of pink and have a firm, sometimes slightly textured appearance. With gingivitis, the inflammation causes increased blood flow to the area, leading to a change in colour from healthy pink to a brighter red or even a purplish hue. The tissues also become puffy and swollen as fluid accumulates due to the inflammatory process. This swelling can make the gums look smooth and rounded where they meet the teeth, losing their normal tight contour. These two signs, bleeding and visual changes like redness and swelling, are so often the first to appear because they are direct manifestations of the body’s initial inflammatory reaction to the bacterial toxins in plaque. They are your gums’ explicit way of telling you, “Hey, we’re irritated! There’s too much bacteria here!” Recognizing these specific, easily observable indicators is the first and most crucial step in identifying potential gum disease at its most treatable stage. Ignoring them allows the underlying bacterial challenge to persist, paving the way for progression to more severe, irreversible damage.
What can I expect if I have gingivitis?
If you receive a diagnosis of gingivitis, the earliest stage of gum disease, you can expect a condition primarily characterised by inflammation of the gum tissue, usually caused by accumulated dental plaque. The typical experience for someone with gingivitis involves noticing some or all of the early signs we’ve discussed: your gums might appear redder than usual, perhaps a brighter red or leaning towards purple in certain areas. You will likely observe swelling, making the gums look puffy, rounded, and perhaps a bit shiny compared to the firm, stippled texture of healthy gums. A very common and often alarming symptom is bleeding. You will probably notice that your gums bleed relatively easily when you brush your teeth or use dental floss, sometimes even just when you eat something firm. This bleeding might be consistent or intermittent. You might also experience some tenderness or mild soreness in the gums, particularly when you touch them or during oral hygiene practices, though significant, throbbing pain is usually *not* a characteristic of gingivitis. This lack of significant pain is precisely why many people overlook gingivitis; it’s easy to tolerate mild discomfort or occasional bleeding compared to the sharp pain of a cavity. Another possible symptom is persistent bad breath or a slightly unpleasant taste in your mouth, caused by the bacteria in the plaque. However, unlike later stages of gum disease, gingivitis typically does *not* involve gum recession (the gums pulling away from the teeth to expose the roots), tooth mobility (loose teeth), or bone loss. The underlying support structures for your teeth remain intact at this stage. The good news is that because the damage is confined to the soft tissues and hasn’t affected the bone or ligaments, gingivitis is almost always reversible with proper treatment. You can expect your dental professional to recommend a thorough professional cleaning (scaling) to remove all traces of plaque and tartar (hardened plaque) from below the gumline. Crucially, you will be instructed on improved daily oral hygiene practices, including effective brushing techniques and consistent flossing or interdental cleaning, to keep plaque from re-accumulating. With diligent home care and professional support, the inflammation should resolve, bleeding should stop, and your gums can return to a healthy state, effectively reversing the condition and preventing its progression to more serious periodontitis.
Specific Physical Symptoms: More Than Just Bleeding Gums
While bleeding gums often serve as the initial wake-up call for potential trouble, the physical manifestations of gum disease extend far beyond a bit of pink in the sink. These specific, tangible symptoms are not merely cosmetic issues; they are direct indicators of active inflammation, bacterial infection, and progressive damage occurring within your oral tissues. They represent the body’s ongoing battle against the bacterial assault and the resulting breakdown of the structures that support your teeth. Each symptom tells a story about the severity and nature of the disease process. Understanding these distinct physical signs helps paint a more complete picture of what gum disease *is* doing to your mouth. They can range from readily apparent visual changes to persistent, bothersome sensations. These symptoms don’t just appear arbitrarily; they are direct consequences of the underlying biological processes – the immune response, the destruction of tissue by bacterial enzymes and toxins, and the loss of structural integrity. For instance, the redness and swelling are the classic hallmarks of inflammation, a response to the bacterial presence. Gum recession is a visual representation of lost connective tissue and bone support, causing the gum line to migrate downwards. Bad breath, often dismissed as simply a hygiene issue, is a chemical signature of the specific types of bacteria flourishing in the infected environment. These symptoms, whether mild irritation in the early stages or significant structural changes later on, serve as tangible evidence that the disease is active and requires intervention. Ignoring them is akin to ignoring warning lights on your car’s dashboard – the problem isn’t going to fix itself, and delaying action only increases the potential for more severe, long-lasting consequences. Let’s delve into some of these specific physical symptoms and understand the mechanisms behind them, recognising that gum disease is a complex issue with multiple, interconnected signs of distress.
Why do gums bleed when brushing or flossing?
Gums bleed during brushing or flossing not because you are cleaning too aggressively (though overly harsh technique can exacerbate existing issues), but primarily because the gum tissue is inflamed and weakened by bacterial plaque buildup. Think of healthy gum tissue as being robust and resilient, capable of withstanding the normal mechanical forces of brushing and flossing. However, when plaque accumulates along the gumline, the bacteria within it release toxins. These toxins trigger an inflammatory response from your immune system. The body increases blood flow to the area to deliver defensive cells, and the blood vessels in the gums become engorged and more fragile. The tissue itself becomes less dense and more permeable due to the inflammatory process. In this inflamed state, the delicate blood vessels just beneath the surface are easily ruptured by even the gentle pressure of toothbrush bristles or dental floss. This is why you see blood – it’s escaping from these compromised, inflamed vessels. It’s a clear signal that the tissue is not healthy and is reacting negatively to mechanical stimulation that it should easily tolerate. People often mistakenly believe that bleeding means they should *stop* brushing or flossing that area to avoid further irritation. This is precisely the wrong approach! The bleeding is a sign of infection and inflammation caused by plaque; stopping cleaning means the plaque remains, the inflammation worsens, and the bleeding is likely to continue or increase. Instead, bleeding during brushing or flossing should be interpreted as a crucial warning sign of gingivitis or periodontitis and should prompt you to improve your cleaning technique and frequency, and crucially, to seek professional dental advice. A dentist or hygienist can confirm the cause of the bleeding, provide a thorough cleaning to remove the irritant (plaque and tartar), and instruct you on effective, yet gentle, techniques to manage the bacterial load at home. Bleeding is not a sign of healthy cleaning; it’s a sign of underlying gum issues that need to be addressed.
Why are your gums swollen and red?
The appearance of swollen and red gums is a classic and undeniable sign of inflammation, which, in the context of gum disease, is almost always a direct result of a bacterial infection caused by plaque accumulation. When bacteria in the plaque release toxins, the body perceives this as an assault and mounts an immune response. This response is what we clinically refer to as inflammation. Think of inflammation as your body sending reinforcements to a troubled area. To do this, it increases blood flow to the gum tissue surrounding the teeth. This surge in blood flow causes the tissue to become engorged with blood, which is what gives the gums their characteristic angry red or purplish hue, a stark contrast to the healthy pink of normal gums. Simultaneously, the inflammatory process involves the release of various chemical mediators and the movement of fluid and immune cells into the tissue spaces. This accumulation of fluid and cells within the gum tissue causes it to swell and become puffy. The normal contours of the gum tissue, which should fit tightly and neatly around the teeth and often have a slightly stippled texture like an orange peel, become rounded, enlarged, and often smooth and shiny as the tissue stretches from the internal swelling. This swelling can also make the gums feel tender or sore to the touch. This redness and swelling are essentially the visual signature of your body actively fighting the bacterial irritant. While inflammation is a necessary part of the healing process when triggered appropriately (like healing a cut), chronic inflammation, as seen in gum disease, becomes destructive. The persistent presence of bacteria means the inflammatory response never fully resolves; instead, it continues, eventually starting to break down the very tissues it’s meant to protect, including the connective tissue and bone. Therefore, redness and swelling aren’t just cosmetic issues; they are palpable evidence of an active, ongoing inflammatory process driven by bacterial infection, signaling that the gums are in distress and require intervention to remove the underlying cause.
What causes persistent bad breath?
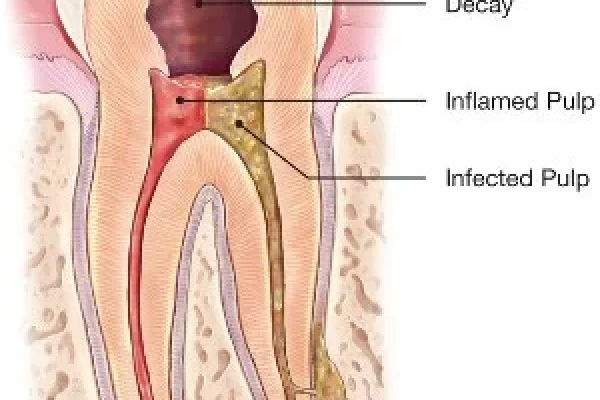
Persistent bad breath, medically known as halitosis, that doesn’t resolve after brushing and rinsing, is a common and often distressing symptom of gum disease. Unlike transient bad breath caused by certain foods or morning mouth, the odour associated with gum disease is often chronic and emanates directly from the ongoing bacterial activity and tissue breakdown occurring within the infected areas of the mouth, particularly in periodontal pockets. The primary culprits behind this foul odour are specific types of anaerobic bacteria that thrive in oxygen-poor environments, such as the deep pockets that form between the teeth and gums when gum disease progresses from gingivitis to periodontitis. These bacteria feast on food particles, plaque, and the proteins from saliva and shedding oral tissues. As a byproduct of their metabolism, they release volatile sulfur compounds (VSCs), such as hydrogen sulfide and methyl mercaptan. These same compounds are responsible for the smell of rotten eggs or decay, and they are the main source of the offensive odour. As gum disease causes the gums to pull away from the teeth, deeper pockets are created. These pockets become ideal, protected havens for these odour-producing anaerobic bacteria, which are difficult to reach and remove with standard brushing and flossing. Furthermore, as the disease progresses, tissue breakdown occurs, providing even more protein material for these bacteria to break down, exacerbating the smell. While poor oral hygiene in general can cause bad breath due to superficial plaque and food debris, persistent bad breath that lingers despite regular cleaning is highly indicative of a deeper issue like gum disease, where the bacteria are lodged in areas inaccessible to your toothbrush. The presence of deep pockets allows these odour-producing bacteria to flourish undisturbed, constantly releasing VSCs. Therefore, if you or someone close to you notices chronic bad breath that isn’t resolved by simple brushing and mouthwash, it’s a strong signal that bacterial activity may be occurring below the gumline, likely a symptom of underlying gum disease requiring professional evaluation and treatment.
What does gum recession look like?
Gum recession is one of the most visually clear and concerning signs of progressing gum disease, representing the actual loss of gum tissue around the teeth. It literally looks like the gum line is moving away from the crown of the tooth, exposing more of the tooth structure, specifically the root surface, which is normally covered and protected by the gum. In a healthy mouth, the gum tissue fits snugly and tightly around the neck of each tooth, creating a protective seal where the tooth meets the gumline. When gum recession occurs, this seal is compromised. Visually, you might notice that your teeth appear longer than they used to. This isn’t because the tooth itself is growing, but because the gum tissue that once covered part of the root is receding downwards (or sometimes sideways). You might be able to see the root surface, which is typically a slightly different colour and texture than the enamel-covered crown – often appearing more yellow or brown, and feeling softer if you were able to touch it. Small gaps or ‘black triangles’ can sometimes appear between teeth near the gumline, where the papillae (the points of gum tissue that fill the space between teeth) have receded. You might also be able to feel a notch or step at the point where the enamel of the crown meets the exposed root surface. As recession worsens, more of the root becomes visible, increasing the tooth’s apparent length and potentially leading to sensitivity problems because the root surface is not protected by hard enamel. From a professional perspective, recession is measured by probing from the CEJ (Cementoenamel Junction – the line where the enamel meets the root) to the crest of the gum tissue. Greater distances indicate more recession. Recession is a significant sign because it directly reflects the loss of the attachment of the gum to the tooth and often indicates underlying bone loss, as the gum tissue tends to follow the level of the supporting bone. It’s not just a cosmetic issue; it exposes the vulnerable root to decay and contributes to tooth instability in advanced stages. Seeing your gum line noticeably pulling back is a critical visual warning that requires immediate dental attention.
Visual Appearance: What Do Healthy and Unhealthy Gums Look Like?
Comparing the visual appearance of healthy gums side-by-side with gums affected by disease offers one of the most impactful ways to understand the warning signs. Your mouth is not a static environment; the tissues respond visibly to health and disease. Observing these visual cues – changes in colour, shape, texture, and position relative to the teeth – provides a powerful, albeit sometimes alarming, diagnostic tool, even for the untrained eye. Healthy gums present a picture of vitality and robustness; they are the firm, stable foundation that holds your teeth securely and protects the underlying bone. They have a specific look and feel that signifies their health. Unhealthy gums, conversely, display a range of visual abnormalities that broadcast their distress. These changes aren’t merely aesthetic; they reflect the underlying pathological processes of inflammation, infection, and tissue destruction driven by bacterial presence. By providing this visual guide, we can empower you to become a better observer of your own oral health. Understanding the subtle differences in hue, the change from a firm texture to puffiness, or the alarming sight of the gum line creeping away from the tooth can prompt you to seek professional help much sooner. These visual indicators evolve as gum disease progresses from its mildest form (gingivitis) to more severe stages (periodontitis). What might start as a barely noticeable change in colour can escalate to significant recession and visible signs of damage. Paying attention to these visual signs during your daily oral hygiene routine is like checking the structural integrity of your home’s foundation – it allows you to spot potential problems early, when they are most manageable. Let’s delineate the specific visual characteristics that differentiate a healthy gum from one under siege by disease.
What do healthy gums look like?
Healthy gums exhibit specific characteristics that signify their vitality and proper function in supporting your teeth. Visually, they present a picture of robust health. One of the most noticeable features is their colour. While the exact shade can vary depending on an individual’s ethnicity and natural pigmentation (ranging from a coral pink to darker, almost brownish or greyish tones in people of African, Asian, or Mediterranean descent), healthy gums are generally consistent in colour and should not show patches of angry redness or purple. More importantly than the specific shade, healthy gums are firm to the touch. When gently pressed, they feel dense and resilient, not soft, spongy, or swollen. They fit snugly and tightly around the neck of each tooth, like a well-fitting collar, with no gaps or pockets where debris and bacteria can easily accumulate. The gum line should follow a smooth, scalloped edge around each tooth. The tissue between the teeth, called the papilla, should be pointed and fill the space completely, creating a tight seal. The surface texture of healthy gums is often described as having a stippled appearance, resembling the surface of an orange peel, although this texture can be less pronounced in some individuals. Crucially, healthy gums do not bleed during routine, effective brushing or flossing. Seeing blood after cleaning is a deviation from health, not a sign of it. They also typically do not cause pain or tenderness when touched or during chewing. In essence, healthy gums are calm, stable, and show no signs of inflammation, swelling, or detachment from the teeth. They are the quiet, strong foundation, fulfilling their protective role without drawing undue negative attention. Recognising these characteristics is key to identifying when your gums deviate from this healthy baseline.
What does gum disease look like?
The visual appearance of gums afflicted by gum disease presents a stark contrast to the picture of health, displaying a range of distressing signs that reflect underlying inflammation, infection, and tissue destruction. The specific look can vary depending on the stage and severity of the disease, transitioning from the initial signs of gingivitis to the more profound damage of periodontitis. In the early stage, gingivitis, the gums primarily show signs of inflammation. Their colour shifts from a healthy pink (or normal pigmented shade) to red or purplish. They appear swollen or puffy, losing their firm texture and often looking smooth and shiny rather than stippled. This swelling makes the gums look engorged and less tightly adapted around the teeth. You will also likely see bleeding when these gums are brushed or flossed. There is typically no visible recession or tooth mobility at this point. As the disease progresses to periodontitis, the visual changes become more significant and indicative of deeper tissue damage. A key visual hallmark is gum recession, where the gum line visibly pulls away from the teeth, making the teeth appear longer and exposing the tooth roots (which may look yellower or different in texture). This recession can also lead to the appearance of gaps or “black triangles” between teeth. In moderate to severe periodontitis, you might see pus oozing from between the gums and teeth, a clear sign of active infection. Teeth may start to look misaligned or develop noticeable spaces as they shift due to bone loss. In the most advanced stages, teeth may become visibly loose or mobile, potentially even shifting position significantly within the mouth. While gingivitis is characterised by inflamed, red, swollen gums that bleed, periodontitis includes these signs *plus* visual evidence of structural breakdown (recession, exposed roots, gaps, tooth looseness). Observing any of these visual cues is a strong indicator that gum disease is present and active, requiring prompt professional evaluation to halt or manage the progression of the damage.
What does stage 1 gum disease look like?
Stage 1 gum disease, often referred to as early periodontitis, represents the point where the disease has progressed beyond the initial, reversible gingivitis and has begun to affect the supporting structures of the teeth, specifically the periodontal ligament and the alveolar bone. Visually, differentiating early periodontitis from severe gingivitis can sometimes be subtle to the untrained eye, but there are key indicators that signify this progression. At this stage, you will still likely see the classic signs of inflammation inherited from gingivitis: the gums will appear red or swollen and may still bleed during brushing or flossing. However, Stage 1 is defined by the *initiation* of attachment loss and minimal bone loss, which starts to manifest visually and functionally. While not always immediately obvious to the individual, there is typically slight gum recession occurring. The gum line may have started to pull back minimally from the teeth, making the teeth look slightly longer. This recession indicates that the connective tissue attachment between the gum and the tooth root has begun to break down, a process that does not happen in gingivitis. Accompanying this, though not visible externally without an X-ray, is minimal bone loss around the roots of the teeth. This bone loss is the hallmark differentiating periodontitis from gingivitis. Visually, this minimal bone loss might not cause teeth to become loose yet, but the slight recession is often the first visual cue related to the deeper problem. Periodontal pockets, the spaces between the tooth and gum, are typically slightly deeper than healthy pockets (usually measuring 4-5mm) at this stage, though probing is required to confirm this. You might notice increased tooth sensitivity due to the newly exposed root surface resulting from recession. While the visual changes beyond redness, swelling, and slight recession might not be dramatic, the key difference in Stage 1 is that the damage is no longer confined to the gum tissue; the disease process has started its destructive march towards the tooth’s supporting bone. Therefore, even if the visual signs seem minor compared to advanced disease, they represent a critical turning point where intervention is essential to prevent further, more significant, and irreversible damage.
Understanding the Later Stages of Gum Disease
When gum disease moves beyond the initial, potentially reversible stage of gingivitis and enters the realm of periodontitis, it signifies a critical shift in the disease process. This is no longer just an inflammation of the gum tissue; it’s a full-blown infection that is actively destroying the structures that hold your teeth firmly in place. Periodontitis is progressive, meaning that without intervention, the damage tends to worsen over time. The later stages represent increasing severity of this destruction, impacting not just the superficial gum tissue but crucially the periodontal ligament – the network of fibres connecting the tooth root to the jawbone – and the alveolar bone itself, which forms the sockets that cradle the teeth. Think of it this way: if gingivitis is like termites nibbling at the paint on your house, periodontitis is the termites eating away at the structural beams and foundation. The damage incurred in these later stages, particularly the loss of bone and connective tissue, is often irreversible. While treatment can halt the progression of the disease, the lost bone and gum tissue generally do not grow back naturally. This is why early detection is so paramount – to prevent the disease from reaching these devastating later stages. As periodontitis advances through its stages (often classified from Stage 1 to Stage 4 or 5, depending on the system used), the symptoms become more pronounced, the damage more extensive, and the treatment more complex. The pockets around the teeth deepen significantly, allowing bacteria to colonise further down the root. Bone loss increases, compromising the stability of the teeth. Gums recede further, exposing more root surface. Ultimately, the very foundation supporting the teeth is eroded to the point where the teeth become loose, shift, and may eventually be lost. Understanding what these later stages entail underscores the importance of addressing gum disease aggressively once it progresses beyond gingivitis. It’s about managing a chronic condition and fighting to preserve as much function and tooth structure as possible in the face of significant damage.
What is Stage 3 gum disease?
Stage 3 gum disease, often classified as moderate periodontitis (though classification systems can vary slightly), signifies a significant progression from the early stage, involving more extensive damage to the supporting structures of the teeth. At this stage, the infection has firmly established itself below the gumline, and the body’s inflammatory response has caused noticeable breakdown of the periodontal ligament and substantial loss of alveolar bone. Visually, you would typically observe more pronounced gum recession compared to Stage 1, with a greater portion of the tooth roots becoming exposed. This often leads to more significant tooth sensitivity, particularly to temperature changes, as the root surfaces lack the protective enamel found on the crown. Periodontal pockets, the spaces between the gum and the tooth, are significantly deeper at Stage 3, often measuring 5-7mm or more. These deeper pockets are problematic because they are very difficult, if not impossible, for you to clean effectively at home with a toothbrush or floss, creating reservoirs where bacteria can proliferate and continue their destructive work. Bone loss, which started minimally in Stage 1, is now clearly evident on X-rays and is considered moderate to severe depending on the classification system and extent around the teeth. This loss of bony support can lead to the teeth becoming slightly loose or mobile. You might start to notice that some teeth feel less stable, or perhaps that they have shifted slightly, creating new gaps or changing your bite. Chronic bad breath and a persistent bad taste are also common at this stage due to the increased bacterial load and deeper pockets harbouring odour-producing microbes. While pain is still not a constant feature for everyone with periodontitis, the increased inflammation and potential for localized abscesses can lead to discomfort or soreness. Treatment at Stage 3 is more involved than for gingivitis or early periodontitis. It typically requires deep cleaning procedures (scaling and root planing) under local anaesthetic to remove bacteria and calculus from the deep pockets, and may involve surgical interventions to reduce pocket depth, regenerate lost tissue, or extract teeth that are too severely compromised. The prognosis at Stage 3 is less favourable than earlier stages regarding complete tissue regeneration, but prompt and effective treatment can often stabilise the condition and prevent further progression, helping to retain teeth for a longer period.
What is the last stage of gum disease?
The last stage of gum disease, often classified as Stage 4 or potentially Stage 5 in some detailed periodontal staging systems, represents severe periodontitis with potentially complex or advanced functional impairment. This is the culmination of unchecked disease progression, where the destruction of the tooth’s supporting structures has reached a critical level, significantly impacting the stability, function, and overall prognosis of the affected teeth. At this stage, the visual signs are usually dramatic and unmistakable. There is extensive gum recession, often exposing a large portion of the tooth roots. Significant bone loss is clearly evident on X-rays, with 50% or more of the original supporting bone structure potentially gone around many teeth. Periodontal pockets are typically very deep, often exceeding 7mm, making them major reservoirs of bacteria and incredibly challenging to maintain. The most defining characteristic of the last stage is often marked tooth mobility. Teeth can become significantly loose, sometimes even shifting noticeably within their sockets or drifting into different positions, affecting the bite (how your teeth come together). This mobility can make chewing difficult and painful. You may notice large gaps or spaces appearing between teeth that were previously close together. Chronic pain can be a factor for some individuals, especially if abscesses (collections of pus) develop. Persistent severe bad breath and a foul taste are almost always present due to the massive bacterial load in the deep pockets. Functionally, this stage often results in impaired chewing ability and can lead to tooth loss. Teeth may become so loose they fall out on their own, or they may require extraction because they can no longer be saved or provide stable function. Treatment at the last stage is complex and focuses primarily on managing the condition to prevent further deterioration and preserving teeth that can realistically be maintained. This may involve extensive deep cleaning, various surgical procedures (including complex regenerative techniques where possible, though often limited by the extent of damage), and potentially extractions of unsalvageable teeth. Rehabilitation often involves dentures, bridges, or implants to replace lost teeth. Severe periodontitis in the last stage is a devastating condition that profoundly impacts oral health, quality of life, and can even have systemic health implications. It underscores the critical importance of early detection and intervention to prevent reaching this level of irreversible damage.
Why You Shouldn’t Ignore Gum Disease Symptoms
Ignoring gum disease symptoms is akin to ignoring foundational cracks in your house – what starts as a minor issue inevitably escalates into a major, costly, and potentially irreparable disaster. The consequences of allowing gum disease to advance unchecked are profound, extending far beyond merely losing a tooth or two. At its most immediate and visible level, untreated gum disease is the leading cause of tooth loss in adults. As the infection destroys the periodontal ligament and alveolar bone that support your teeth, their anchors weaken. Imagine the root of your tooth like a pole planted in the ground; the bone is the soil, and the ligament is the concrete holding it firm. Gum disease erodes that soil and concrete. As the bone recedes and the ligaments break down, the tooth loses its stable foundation. It becomes loose, shifts, and eventually, without the necessary support, it will detach or need to be extracted. Losing teeth impacts your ability to chew, speak, and affects your facial appearance. But the ramifications don’t stop there. The mouth is not an isolated system; it’s intimately connected to the rest of your body. The bacteria and inflammatory mediators associated with gum disease can enter your bloodstream through the damaged gum tissue. Research has increasingly shown links between chronic gum disease and systemic health conditions. It is considered a risk factor for heart disease and stroke, potentially contributing to the hardening of arteries. For individuals with diabetes, gum disease can make it harder to control blood sugar levels, and conversely, uncontrolled diabetes can worsen gum disease. Links have also been explored with respiratory diseases, rheumatoid arthritis, and even complications during pregnancy. Ignoring the symptoms isn’t just risking your smile; it’s potentially putting your overall health at risk. The chronic inflammation in your mouth can contribute to the overall inflammatory burden on your body. Addressing gum disease isn’t just about saving your teeth; it’s about safeguarding your general well-being. The early symptoms are warning signals for a reason – heeding them is an investment in both your oral health and your systemic health, preventing a potentially devastating cascade of problems down the line.
What Should I Do If I Notice These Signs?
If you notice any of the signs and symptoms of gum disease discussed – whether it’s bleeding gums, redness, swelling, persistent bad breath, recession, or anything else that seems unusual or concerning – the most crucial and impactful step you can take is to consult a dental professional immediately. Do not delay, do not try to self-treat with over-the-counter rinses alone, and certainly do not ignore it hoping it will magically disappear. A dentist or a periodontist (a specialist in gum disease) is the only one who can accurately diagnose the presence and severity of gum disease. They have the knowledge, tools, and expertise to examine your gums thoroughly, measure pocket depths, assess bone levels via X-rays, and identify the specific type and stage of gum disease you may have. What looks like simple redness to you could be the early stages of gingivitis, or it could be a sign of more advanced periodontitis requiring urgent intervention. Attempting to manage the issue solely with improved brushing and flossing, while essential for prevention and support, will not be sufficient if tartar has built up below the gumline or if bone loss has already occurred. Your dental professional will perform a comprehensive evaluation and then discuss their findings with you. Based on the diagnosis, they will develop a personalised treatment plan. This plan will be tailored to your specific condition, ranging from professional cleaning (scaling) to remove bacteria and tartar below the gumline, prescribing antibiotics, recommending surgical procedures to manage deep pockets or regenerate lost tissue, or even extractions in severe cases. Your dentist will also provide crucial guidance on effective daily oral hygiene practices tailored to your condition and schedule follow-up appointments to monitor your progress and maintain your oral health. Acting quickly upon noticing these signs is paramount because early intervention can often reverse gingivitis and can significantly slow or halt the progression of periodontitis, preserving your teeth and protecting your overall health. Your prompt action is the first step in taking control of your gum health.
Frequently Asked Questions About sign of gum disease
How to know if you have gum disease?
Determining if you have gum disease involves paying close attention to your oral health and seeking professional evaluation, as it’s not always overtly painful in its early stages. You can start by conducting a simple self-check at home. Look closely at your gums in a mirror under good light. Do they look consistently healthy pink and firm, or are there areas that appear redder, swollen, puffy, or shiny? Gently touch your gums – do they feel tender or sore? Inspect your gum line – are there any areas where the gum seems to be pulling away from the tooth, making the tooth look longer? Pay close attention when you brush and floss: Is there any bleeding, even a small amount? Healthy gums shouldn’t bleed from routine cleaning. Do you have persistent bad breath or a bad taste that doesn’t go away after brushing? Have you noticed any changes in how your teeth fit together, or do any teeth feel slightly loose? While these observations can raise suspicion, the definitive way to know if you have gum disease is through a comprehensive dental examination. Your dentist or dental hygienist is trained to identify the subtle signs you might miss. They will visually inspect your gums, look for recession, check for tooth mobility, and crucially, perform a periodontal probing – using a small instrument to measure the depth of the pockets between your teeth and gums. Deep pockets (more than 3mm) are a key indicator that the gum has detached from the tooth due to infection. They will also take X-rays to assess the level of bone supporting your teeth, as bone loss is a hallmark of periodontitis. Only this professional evaluation can confirm the diagnosis, determine the specific type and stage of gum disease, and identify contributing factors, allowing for the development of an effective treatment plan tailored to your needs. Don’t rely solely on self-diagnosis; if you have any concerns based on your observations, schedule a dental appointment.
What are the warning signs of gum disease?
The warning signs of gum disease are varied signals from your gums indicating that something is wrong, primarily driven by inflammation and infection. These signs can range from subtle changes in the early stages to more dramatic indicators in advanced disease, and it’s crucial to be aware of the spectrum. The most common initial warning signs include gums that are red, swollen, or tender to the touch – a direct result of inflammation caused by bacterial plaque. A critical, frequently ignored warning sign is bleeding gums, particularly during brushing, flossing, or eating firm food. Healthy gums should not bleed under these circumstances. As the disease progresses, other warning signs become apparent: persistent bad breath or a bad taste in the mouth that doesn’t clear with cleaning, indicating a deeper bacterial issue. Gum recession, where the gums pull away from the teeth, making the teeth look longer and potentially exposing the roots, is a clear sign of attachment loss. You might notice increased tooth sensitivity, especially to hot and cold, due to exposed root surfaces. Changes in the fit of dentures or partials can occur as the underlying gum and bone structures change. In more advanced stages, warning signs include teeth that are loose or shifting, creating new spaces between them, which indicates significant bone loss. The presence of pus between the teeth and gums is also a definite warning sign of active infection. Sometimes, there might be pain when chewing, though periodontitis can also be painless, making regular dental check-ups even more important. Any of these signs should serve as a red flag prompting you to seek professional dental evaluation. They are your body’s way of alerting you to a problem that requires diagnosis and intervention to prevent further damage and potential tooth loss.
What are two early signs of gum disease?
Focusing specifically on the very earliest indicators that gum disease might be setting in, two signs are overwhelmingly the most common and should immediately raise your suspicion: bleeding gums and redness/swelling of the gum tissue. These are the foundational warning signals of gingivitis, the initial and often reversible stage of gum disease, stemming directly from the body’s immediate inflammatory response to bacterial plaque accumulation along the gumline. Firstly, bleeding gums is perhaps the most prevalent early sign that people notice, although they often dismiss it. Any bleeding when you brush your teeth or use dental floss indicates that the gum tissue is inflamed and fragile due to the presence of bacterial toxins. Healthy gums are resilient enough to withstand these routine cleaning actions without bleeding. Seeing pink on your brush or floss is not a sign of brushing too hard; it’s a sign your gums are irritated by bacteria. Secondly, redness and swelling are visible indicators of this early inflammation. Healthy gums are typically a firm, consistent pink (or appropriately pigmented shade). When gingivitis is present, increased blood flow to the area causes the gums to appear redder, sometimes even moving towards a purplish hue. The tissues also become puffy and swollen as fluid accumulates, losing their firm texture and appearing rounded or shiny instead of snug and contoured around the teeth. These two signs are often the first to appear because they are direct manifestations of the body’s acute response to bacterial irritants before deeper tissues are affected. Recognising these specific early signals – any instance of bleeding during cleaning and any noticeable change in gum colour or puffiness – is crucial because gingivitis is usually reversible with proper oral hygiene and professional care. Ignoring these clear initial warnings allows the underlying bacterial challenge to persist, increasing the risk of progression to irreversible periodontitis.
What does gum disease look like?
The appearance of gum disease is a departure from the visual characteristics of healthy gums, displaying various signs that indicate inflammation, infection, and damage. What gum disease “looks like” depends heavily on its stage of progression. In the earliest stage, gingivitis, the visual signs are primarily those of inflammation. The gums appear red or purplish, a noticeable shift from healthy pink (or normal darker pigmentation). They look swollen or puffy, losing their tight, scalloped contour around the teeth and often appearing smooth and shiny instead of having a stippled texture. You will also likely see bleeding when these gums are stimulated by brushing or flossing. There is typically no visible recession or tooth mobility at this point. As gingivitis progresses to periodontitis, the visual signs become more indicative of deeper tissue destruction. A key visual hallmark is gum recession, where the gum line pulls away from the teeth, making the teeth appear longer and exposing the tooth roots (which may look yellower or different in texture). This recession can also lead to the appearance of gaps or “black triangles” between teeth. In moderate to severe periodontitis, you might see pus oozing from between the gums and teeth, a clear sign of active infection. Teeth may start to look misaligned or develop noticeable spaces as they shift due to bone loss. In the most advanced stages, teeth may become visibly loose or mobile, potentially even changing position significantly within the mouth. While gingivitis is characterised by inflamed, red, swollen gums that bleed, periodontitis includes these signs *plus* visual evidence of structural breakdown (recession, exposed roots, gaps, tooth looseness). Observing any of these visual deviations from a healthy gum appearance is a strong indicator of gum disease and necessitates a professional dental check-up to determine the extent of the problem and the necessary steps for treatment.
What should I do if I have any of these signs?
If you identify any of the warning signs or symptoms of gum disease discussed – whether it’s bleeding during brushing, swollen or red gums, persistent bad breath, noticing your teeth look longer due to recession, or anything else that seems unusual or concerning – the absolute most important action you must take is to consult a dental professional immediately. Do not delay, do not try to self-treat with over-the-counter rinses alone, and certainly do not ignore it hoping it will magically disappear. A dentist or a periodontist (a specialist in gum disease) is the only one who can accurately diagnose the presence and severity of gum disease. They have the knowledge, tools, and expertise to examine your gums thoroughly, measure pocket depths, assess bone levels via X-rays, and identify the specific type and stage of gum disease you may have. What looks like simple redness to you could be the early stages of gingivitis, or it could be a sign of more advanced periodontitis requiring urgent intervention. Attempting to manage the issue solely with improved brushing and flossing, while essential for prevention and support, will not be sufficient if tartar has built up below the gumline or if bone loss has already occurred. Your dental professional will perform a comprehensive evaluation and then discuss their findings with you. Based on their diagnosis, they will develop a customised treatment plan. This plan will be tailored to your specific condition, ranging from professional cleaning (scaling) to remove bacteria and tartar below the gumline, prescribing antibiotics, recommending surgical procedures to manage deep pockets or regenerate lost tissue, or even extractions in severe cases. Your dentist will also provide crucial guidance on effective daily oral hygiene practices tailored to your condition and schedule follow-up appointments to monitor your progress and maintain your oral health. Acting quickly upon noticing these signs is paramount because early intervention can often reverse gingivitis and can significantly slow or halt the progression of periodontitis, preserving your teeth and protecting your overall health. Your prompt action is the first step in taking control of your gum health.