Table of Contents
ToggleKey Takeaways
- Modern dentistry offers diverse tooth replacement options, far beyond traditional “false teeth”.
- Choices include removable partial and full dentures, and fixed or removable implant-supported dentures.
- The “best” option is *highly personal*, depending on oral health, number of missing teeth, jawbone condition, budget, and lifestyle.
- Dental implants provide superior stability and jawbone preservation compared to traditional dentures but are more costly and require surgery.
- Proper daily care and regular dental check-ups are *essential* for the longevity and health of any prosthetic type.
Right then, let’s dive tooth-first into this, shall we? SPARKLE’s got the bit between the teeth and is ready to craft something truly engaging. Forget the dry dental pamphlets; we’re aiming for something with a bit more bite.
Losing teeth is, let’s be frank, a bit of a shocker. Whether it happens due to accident, age, or simply the cruel march of time and decay, the gap it leaves isn’t just physical. It affects how you eat, how you speak, and perhaps most significantly, how you feel about yourself when you flash a smile (or, indeed, whether you feel like smiling at all). For centuries, humanity’s quest for a convincing replacement has driven innovation, from surprisingly elaborate historical examples crafted from bone or ivory to the remarkable options available today. What we used to just call “false teeth” – a somewhat clunky, slightly intimidating term – has evolved dramatically. Modern dentistry offers a veritable smorgasbord of solutions, far beyond the single, one-size-fits-all approach of yesteryear. We’re talking about sophisticated, often highly customised prosthetics designed to restore not just function, but confidence, aesthetics, and a genuinely natural feel. The journey back to a complete smile is no longer limited to one well-trodden path. Instead, it’s a landscape dotted with various routes, each with its own terrain, suitability, and destination. Navigating this landscape requires understanding the different options on offer, appreciating that the ‘best’ choice is profoundly personal, depending on everything from the number of missing teeth and the condition of your existing jawbone to your lifestyle, your aesthetic desires, and, yes, the financial realities. From plates you pop out at night to structures permanently anchored in bone, the variety available today is frankly astonishing, offering solutions that were pure science fiction just a generation or two ago.
What are the different types of false teeth you can get?
False teeth, or dentures as they are more formally and frequently known in dental circles, represent a broad category of prosthetic devices designed to replace missing teeth. The very phrase “false teeth” might conjure images of grandma’s teacups and a denture soaking in a glass overnight, a rather quaint and perhaps slightly unappealing picture. However, the reality of modern dental prosthetics is far more nuanced and significantly more advanced than those historical stereotypes suggest. Contemporary dentistry has, quite literally, rebuilt the possibilities for tooth replacement. Gone are the days when your only option after losing teeth was a bulky, ill-fitting plate that made eating a chore and speaking a whistly adventure. Today, the range of choices available is vast and impressive, a testament to decades of material science, surgical technique refinement, and a deeper understanding of oral biology. These advancements mean that finding a solution that fits your specific needs, rather than simply making do with a generic alternative, is now not just possible but expected.
The selection of the ‘right’ type of false teeth is a deeply personal decision, one that should never be made lightly or in isolation. It hinges on a complex interplay of factors unique to each individual. How many teeth are missing? Is it just one, a few scattered here and there, or an entire arch? What is the state of your remaining natural teeth, if any? Crucially, what is the health and density of your jawbone, which provides the foundation for any prosthetic? Your overall health, pre-existing medical conditions, and even lifestyle habits (like smoking) can influence the suitability of certain options. And, of course, there are practical considerations: what is your budget, and how much are you willing to invest in terms of time and potential discomfort during the treatment process?
Understanding this variety means moving beyond the simple “full or partial” dichotomy. Today’s options span a spectrum from traditional, removable appliances to cutting-edge fixed solutions anchored by dental implants. Each type offers distinct advantages and potential drawbacks, catering to different levels of tooth loss, different clinical situations, and different patient priorities. Some prioritise affordability and minimal invasiveness, while others focus on maximum stability, bone preservation, and a feel that mimics natural teeth as closely as possible. We’ll explore these categories in detail, giving you a clearer picture of the landscape so you can approach a consultation with a dental professional armed with knowledge and a better sense of the possibilities that await. The goal isn’t just to fill a gap; it’s to restore function, enhance appearance, and ultimately, give you your smile – and all that comes with it – back.
Understanding the Main Kinds of Dentures
When we talk about dentures, it’s helpful to first establish the primary classifications. Think of these as the major highways in our navigation guide to false teeth. While the specific types and materials within these classifications can be numerous, understanding these fundamental divisions provides a solid framework. The categorisation primarily revolves around two key factors: the extent of tooth loss and the method of support or retention for the prosthetic. Are you missing just a few teeth, or are you missing an entire set in your upper or lower jaw (or both)? And how will the replacement teeth be held securely in place – relying on the gums, clinging to remaining natural teeth, or anchored firmly to the jawbone itself?
Historically, dentures were primarily split into two camps: partial and complete (or full). This remains a fundamental distinction, based on whether some natural teeth are still present or if an entire arch requires replacement. However, the advent and widespread success of dental implants have introduced a third major category that is fundamentally different in its support mechanism: implant-supported dentures. This crucial addition has revolutionised the field, offering levels of stability and bone preservation previously unattainable with conventional methods. While traditional partial and complete dentures rest on the gum tissue and sometimes rely on remaining teeth for retention, implant-supported dentures gain their stability from titanium posts surgically placed within the jawbone. This difference in support is not just a technical detail; it profoundly impacts the function, comfort, and long-term health of the mouth. Within each of these main classifications – partial, complete, and implant-supported – there exists a fascinating array of sub-types and variations, differing in design, materials used, the number of implants needed, and whether they are removable or fixed. Understanding these main kinds is the essential first step in comprehending the diverse options available for replacing missing teeth effectively in the modern era.
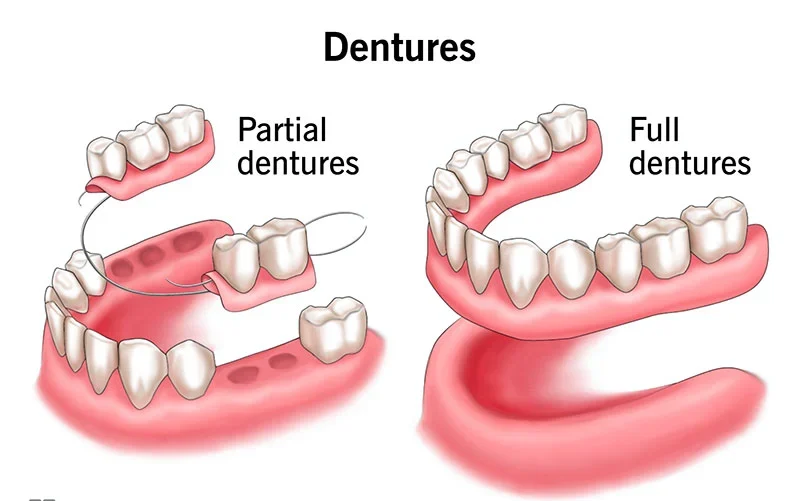
What are partial dentures?
Partial dentures are precisely what they sound like: prosthetic devices designed to replace one or more, but not all, missing teeth in a single dental arch. They become necessary when some healthy natural teeth still remain in the jaw. Their primary function isn’t just aesthetic, though filling those gaps certainly improves the look of your smile. They play a crucial role in maintaining the integrity of your remaining oral structure. When a gap is left open, adjacent teeth have a tendency to drift or tilt into the space, disrupting your bite and potentially leading to further tooth loss or gum problems. Partial dentures prevent this shifting, helping to preserve the alignment of your natural teeth. Furthermore, replacing missing teeth with a partial denture restores chewing efficiency, making it easier to eat a wider variety of foods. They also provide support for your facial muscles and can significantly improve speech, which can sometimes become affected by missing teeth, particularly front ones.
The structure of a typical partial denture involves replacement teeth, usually made of resin or porcelain, attached to a gum-colored base. This base is often made of acrylic resin, though some partials feature a thin, strong metal framework (commonly a cobalt-chromium alloy) that provides support and retention. Clasps, made either of metal (visible or hidden) or gum-colored acrylic/nylon, extend from the base to grip onto some of your natural teeth. These clasps are essential for holding the partial denture in place. While designs vary, most traditional partial dentures are removable, meaning you can and should take them out for cleaning, usually after meals and definitely overnight. There are different types of partial dentures, including cast metal framework partials (strong, thin, and durable), acrylic partials (often used as temporary solutions or when the tooth loss pattern is simple, but bulkier and less stable than metal), and flexible partials (made of thermoplastic material, often more comfortable and aesthetically pleasing due to gum-colored clasps, but with limitations in adjustability). Choosing the right type depends heavily on the number and location of missing teeth, the health of the remaining teeth, and the patient’s preference for aesthetics and comfort.
What are full dentures?
Full dentures, often referred to simply as complete dentures, step onto the stage when an entire arch of teeth is missing – either the upper or the lower jaw, or both. They represent a complete replacement solution for those who have lost all their natural teeth in a specific arch. Unlike partial dentures which anchor to existing teeth, full dentures rest directly on the gum tissue and the underlying bone ridge. This means their stability and retention rely on different principles.
For the upper jaw, a complete denture typically covers the palate (the roof of the mouth), creating a seal that generates suction to help hold the denture in place. This suction, combined with the precise fit against the gums, provides the primary means of retention. Upper dentures are often more stable and easier to adapt to for this reason. The lower jaw presents a different challenge. A lower complete denture is horseshoe-shaped, following the curve of the jaw, and does not have the benefit of palatal suction. Its stability depends more heavily on the shape of the bony ridge, the patient’s control of their tongue and cheek muscles to keep the denture in place, and often, the assistance of denture adhesive for added security.
Both upper and lower complete dentures consist of a full set of replacement teeth mounted on a gum-colored acrylic base. The teeth themselves are usually made of resin or porcelain. The fit of full dentures is critical for both function and comfort. A well-made, properly fitting full denture can significantly restore chewing ability, allowing wearers to enjoy a much wider range of foods than they could without teeth. They also provide support for the lips and cheeks, helping to maintain facial structure and prevent a sunken appearance that can occur after tooth loss. Furthermore, they restore the ability to speak clearly, as missing teeth can significantly impact articulation. Like most partial dentures, conventional full dentures are removable. They need to be taken out daily for thorough cleaning and ideally overnight to allow the gum tissues to rest and remain healthy. While traditional full dentures are a widely used and often cost-effective solution, it’s important to manage expectations regarding their stability, particularly the lower denture, compared to options anchored by implants.
What kinds of fixed dentures are there?
Fixed dentures represent a significant leap in tooth replacement technology, offering a solution that is permanently attached and cannot be removed by the patient for daily cleaning – only a dentist can remove them if necessary. This permanent fixture provides a level of stability and function that traditional removable dentures simply cannot match. The key difference lies in their support structure. Unlike conventional dentures that rest on the gums, fixed dentures are securely anchored, typically to dental implants embedded within the jawbone. In some specific cases, they might be cemented to existing strong natural teeth, but implant support is the most common and robust method for replacing multiple or all teeth with a fixed solution.
The appeal of fixed dentures is immense. Because they are anchored in place, they feel much more like natural teeth. There’s no worry about slippage or movement while talking, eating, or laughing. Chewing power is significantly increased compared to removable options, allowing for a much broader and healthier diet. Furthermore, implant-supported fixed dentures help stimulate the jawbone, preventing the bone loss that naturally occurs after teeth are lost and is accelerated by wearing traditional dentures. This preservation of bone is crucial for maintaining facial structure over the long term.
The main types of fixed dentures are essentially bridges or full-arch prostheses that are either cemented onto prepared natural teeth (less common for full arches) or, more typically, screwed or cemented onto dental implants. An implant-supported bridge, for example, can replace a section of missing teeth, being anchored to implants on either side of the gap. For replacing an entire arch, a full-arch fixed prosthesis, often referred to simply as a “fixed denture” or “hybrid denture,” is used. These are typically made with a strong framework (metal or zirconia) with artificial teeth and gum-colored material attached, which is then securely attached to multiple dental implants (commonly four to six or more) placed strategically in the jawbone. The “All-on-4” concept, which we’ll discuss further, is a specific, popular example of a fixed full-arch prosthesis supported by a minimum of four implants. The advantage of fixed dentures is their natural feel and function, eliminating the need for adhesives and the routine of removing and cleaning them outside the mouth (though they still require diligent cleaning around the implants and under the prosthesis). The trade-off is that they are generally more expensive and require surgical procedures for implant placement.
What are implant dentures?
Implant dentures represent a modern, highly effective category of tooth replacement solutions that leverage the stability and long-term benefits of dental implants. At their core, implant dentures are prosthetic teeth structures that are supported by dental implants rather than solely resting on the gums. Dental implants are small, biocompatible titanium posts surgically placed into the jawbone to act as artificial tooth roots. Once integrated with the bone, these implants provide a incredibly sturdy foundation for various types of dental prosthetics, including dentures. The key benefit of using implants for denture support is the dramatic increase in stability and retention compared to traditional, gum-supported dentures. This enhanced stability translates into improved chewing ability, clearer speech, and significantly greater confidence for the wearer.
Furthermore, and critically important for long-term oral health, dental implants stimulate the jawbone, much like natural tooth roots do. This stimulation helps to prevent the progressive bone loss (resorption) that inevitably occurs after teeth are lost and is a common problem for wearers of conventional dentures. By preserving bone volume, implant dentures help maintain facial structure and prevent the sunken appearance that can develop over time with bone loss. Implant dentures come in two main forms, distinguished by whether they are removable or fixed:
- Implant-Retained Dentures (Overdentures / Snap-In Dentures): These are removable dentures that attach to a small number of implants (typically 2 to 4 per arch) via special attachments (like ball or locator attachments) on the underside of the denture. The denture “snaps” onto these attachments, providing much greater retention and stability than a traditional denture, but they are still designed to be removed by the patient daily for cleaning. They reduce movement, improve chewing, and are often less bulky than conventional dentures, especially in the upper jaw where the palate can often be left uncovered.
- Implant-Supported Dentures (Fixed Implant Bridges / Fixed Hybrid Dentures): As discussed in the ‘fixed dentures’ section, these prosthetics are securely attached to a larger number of implants (often 4 to 6 or more) and are not removable by the patient. They feel and function very much like natural teeth, offering maximum stability and chewing power. Examples include fixed full-arch bridges or concepts like All-on-4.
Both types of implant dentures offer significant advantages over traditional removable dentures, but the fixed options provide the highest level of function and feel. While the initial cost and surgical procedure for implant placement are considerations, the long-term benefits in terms of stability, function, and bone health make them an increasingly popular choice for suitable candidates.
Exploring Specific Types of False Teeth Options
Beyond the main classifications of partial, complete, and implant-supported, the world of false teeth offers a fascinating array of specific types, variations, and material choices. Think of these as the different models or customisation options available within the broader categories we’ve just discussed. These specific types are designed to meet a diverse range of patient needs, taking into account everything from the particular pattern of tooth loss and the patient’s aesthetic priorities to considerations of comfort, budget, and convenience. The sheer number of options reflects the ongoing efforts in dental science and technology to provide solutions that are not only functional but also comfortable, natural-looking, and durable. It’s within this exploration of specific types that the true artistry and engineering of modern dental prosthetics become apparent.
Understanding these specific options is crucial because the details matter. A flexible partial denture, for instance, offers a vastly different experience than a traditional cast metal partial, even though both fall under the umbrella of ‘partial dentures.’ Similarly, an immediate denture serves a completely different purpose and has a different lifespan than a conventional or implant-supported full denture. These variations in design, material, and intended use mean that what is ideal for one person might be completely unsuitable for another. Factors like the presence of allergic sensitivities to certain materials, the dexterity of the patient (important for cleaning some complex designs), or even specific occupational needs (e.g., public speaking) can influence the recommendation of one specific type over another.
This section delves into some of the most common and notable specific types you might encounter during your research or a consultation with a dentist. It highlights how slight differences in construction or application can lead to significant differences in patient experience, cost, and outcome. While this guide provides an overview, it’s paramount to reiterate that this information is for educational purposes. The selection of the most suitable specific type of false teeth for your unique situation absolutely requires a thorough examination and consultation with a qualified dental professional. They can assess your oral health status, evaluate the condition of your bone and gums, discuss your expectations and priorities, and recommend the specific denture type, material, and design that offers the best potential for long-term success and satisfaction.
What are snap-in dentures?
Snap-in dentures, formally known as implant-retained overdentures, offer a compelling middle ground between traditional removable dentures and fixed implant-supported prosthetics. They fall under the broader category of implant dentures but are specifically designed to be removable by the patient. The key innovation here is their attachment mechanism: they “snap” onto a small number of dental implants – usually just 2 to 4 implants strategically placed in the jawbone per arch. This connection is facilitated by special attachments embedded in the underside of the denture that clip onto corresponding abutments on the implants.
The “snapping” action provides a much higher level of retention and stability compared to conventional full dentures that rely solely on suction and the shape of the jawbone. This increased stability dramatically reduces movement and slippage, which are common complaints with traditional dentures. Wearers often report feeling much more secure when speaking, eating, and laughing. Chewing efficiency is improved, allowing for a more varied and enjoyable diet. Another significant benefit, particularly for upper snap-in dentures, is the potential to fabricate the denture without covering the entire palate. Leaving the palate open can significantly improve the sense of taste and temperature perception, making the denture feel less bulky and more comfortable.
Despite their enhanced stability, snap-in dentures are still designed to be removed daily for cleaning. This is crucial for maintaining oral hygiene, cleaning the implants and attachments, and allowing the gum tissue under the denture to rest. While they don’t offer the same level of biting force or the permanent, ‘feels-like-natural-teeth’ experience of fixed implant-supported dentures, snap-in dentures provide a substantial upgrade in function and comfort over traditional removable options. They are also typically less costly than fixed implant prostheses because they require fewer implants and a simpler prosthetic design. They are an excellent option for individuals who struggle with the looseness of conventional dentures but are not candidates for, or prefer not to undergo the more extensive surgery or higher cost associated with, fixed implant solutions.
What Are Standard Dentures?
The term “standard dentures,” often interchangeable with “conventional” or “traditional” dentures, generally refers to the most common and historically prevalent types of removable full and partial dentures that are not supported by implants. These are the dentures that primarily rely on the natural contours of the mouth, the underlying gum tissue, and sometimes remaining natural teeth (in the case of partials) for support and retention. They are often the baseline option in terms of cost and complexity.
Standard dentures are typically constructed with a pink, gum-colored base, which is usually made from acrylic resin. This base is molded to fit snugly over the alveolar ridge (the part of the jawbone that used to hold the teeth) and the palate (for upper dentures). The artificial teeth, which are mounted on this base, are commonly made from resin or sometimes porcelain, designed to look and function like natural teeth. Resin teeth are softer and wear down faster but are kinder to opposing natural teeth (if any), while porcelain teeth are harder, more durable, and less prone to staining but can cause wear on natural teeth or opposing dentures and are more brittle.
These dentures are removable, requiring daily removal for cleaning and usually worn during the day and removed at night. Their primary advantages include their affordability compared to implant-based options, the minimal or non-existent surgical procedure required (beyond necessary extractions), and their suitability for a wide range of patients, including those who may not be candidates for implants due to health issues or insufficient bone density. However, they do come with limitations. Conventional full dentures, especially lower ones, can be prone to movement, affecting speaking and eating, and often require denture adhesive for stability. They also don’t prevent bone loss over time, leading to changes in the fit and requiring periodic relining or replacement. Partial dentures using metal clasps, while functional, may have visible metal clasps that affect aesthetics, or if made entirely of acrylic, can be bulky and less stable than metal framework partials. Despite these potential drawbacks, standard dentures remain a vital and accessible tooth replacement option for millions worldwide.
Flexible dentures explained
Flexible dentures represent a notable evolution in partial denture design, offering an alternative to traditional acrylic or metal-based partials. As their name suggests, the defining characteristic of flexible dentures is the material used for their base and clasps: a thin, thermoplastic material, often a form of nylon, that is notably more pliable than the rigid acrylic used in conventional dentures. This flexibility provides several distinct advantages that appeal to certain patients.
Firstly, the flexibility can translate into greater comfort. The material can conform more readily to the subtle contours of the mouth, potentially reducing pressure points and irritation that some people experience with rigid dentures. This makes them particularly comfortable for those with bony prominences or irregular gum shapes. Secondly, flexible dentures are often less bulky than acrylic partials, offering a more streamlined feel in the mouth. Thirdly, and perhaps most appealing aesthetically, the clasps that hold flexible dentures in place are typically made from the same gum-colored thermoplastic material. Unlike the visible metal clasps of many traditional partial dentures, these clasps blend in with the natural gums, making the denture much less noticeable when you smile or talk. This is a significant aesthetic advantage for patients concerned about the appearance of their prosthetic.
Flexible dentures are generally suitable for replacing one or a few missing teeth, often in cases where the remaining teeth are healthy and capable of supporting the flexible clasps. They can be a good option for small partials or as a cosmetic solution. However, flexible dentures are not without their limitations. Because the material is flexible, they may not be suitable for replacing a large number of teeth or for situations where significant chewing force is required, as they can lack the rigidity needed for efficient mastication. They can also be more challenging to reline or repair than acrylic dentures, and adjustments can be more difficult. Proper cleaning is essential, as the flexible material can be slightly more porous than acrylic, requiring specific cleaning solutions and techniques. While not a universal solution, flexible dentures offer a valuable, comfortable, and aesthetically pleasing option for many individuals needing partial tooth replacement.
What are immediate dentures?
Immediate dentures serve a specific, crucial purpose in the tooth replacement process: they are dentures that are fabricated *before* the natural teeth are removed and are inserted into the mouth *immediately* after the extractions occur. This might sound counterintuitive – making a denture for a mouth that still has the teeth it’s meant to replace – but the process involves taking precise measurements and impressions of the mouth with the teeth still in place, predicting the likely shape of the gums and bone after extraction, and then crafting the denture based on these estimates.
The primary benefit of immediate dentures is that the patient is never without teeth. This is a significant advantage both aesthetically and functionally. You leave the dental office after extractions with a full set of teeth already in place, avoiding the potentially embarrassing period of being toothless while the gums heal and a conventional denture is being made. Immediate dentures help maintain your appearance, allow you to speak relatively normally from the outset, and aid in the transition to chewing with dentures during the initial healing phase.
However, it’s vital to understand that immediate dentures are considered a *temporary* or *transitional* solution. After teeth are extracted, the gums and underlying bone undergo significant changes as they heal. The swelling subsides, and the bone remodels and shrinks. Because the immediate denture was made based on the mouth *before* these changes occurred, its fit will inevitably become loose over the healing period (which can last for several months). This loosening requires multiple adjustments and often one or more relines (adding material to the base to improve the fit) to keep the denture fitting as well as possible during the healing process. Once the mouth has fully healed and the tissues have stabilised, the immediate denture typically needs to be replaced with a new, conventional denture that is custom-made to the final healed contours of the mouth, or the patient transitions to an implant-supported solution. While they require extra appointments for adjustments and are not a long-term permanent denture solution, immediate dentures play an invaluable role in providing continuity, function, and confidence during the sometimes challenging healing phase following tooth extractions.
All-on-4 Dentures
The All-on-4 technique is a specific, popular protocol for providing a full arch of *fixed*, implant-supported teeth using a minimum of just four dental implants. Developed as a way to maximise the use of available bone, particularly in areas where bone density might be lower (like the back of the jaw), the implants are strategically placed: two straight in the front and two tilted implants in the back. The tilted implants help to avoid anatomical structures like the sinus cavity in the upper jaw and the nerve canal in the lower jaw, often eliminating the need for complex and costly bone grafting procedures.
The beauty of the All-on-4 concept is that it allows for the placement of a full-arch prosthesis – a fixed bridge resembling a complete set of teeth – shortly after the implants are placed, sometimes even on the same day, depending on the patient’s bone quality and initial implant stability (this is often referred to as “immediate loading”). The prosthesis is securely screwed onto the four implants. Crucially, this prosthetic is *fixed*; the patient cannot remove it. Only a dentist can unscrew it if necessary for maintenance.
The benefits of All-on-4 are substantial. Because the prosthesis is fixed, it provides excellent stability, chewing efficiency, and a feel very close to natural teeth. There’s no need for denture adhesives, no worry about the denture moving or clicking, and no bulky palate coverage (in the upper jaw). The implants also help to preserve the jawbone, preventing the bone loss associated with traditional dentures. Furthermore, by using only four implants per arch, the procedure is often less invasive and potentially less costly than fixed solutions requiring six or more implants. All-on-4 is a highly effective solution for individuals who have lost or are about to lose all their teeth in an arch and desire a permanent, stable, and functional tooth replacement that significantly improves their quality of life. It requires careful planning and execution by experienced dental professionals, but for suitable candidates, it can be genuinely life-changing.
Overdentures
Overdentures are a type of removable denture that gets its name from the fact that it “rests over” or attaches to something in the mouth for retention, rather than solely relying on the underlying gums like traditional dentures. That “something” can be either a few remaining natural tooth roots or, more commonly in modern dentistry, dental implants. We’ve already touched on implant-retained overdentures (snap-in dentures) in a previous section, highlighting their removable nature and attachment to implants. However, the term “overdenture” is broader and includes dentures that use carefully prepared and preserved tooth roots as anchors.
In the case of root-retained overdentures, a few healthy tooth roots (typically those of canine or premolar teeth) are intentionally kept in the jaw. These roots are treated (often with root canal therapy) and then covered with a cap or fitted with an attachment (like a ball or magnet attachment). The overdenture is then fabricated with corresponding attachments on its underside that fit over the roots. This provides a significant increase in stability and retention compared to a full denture resting on gums alone. Retaining even a few roots also has the benefit of helping to preserve the bone around those roots, slowing down the rate of bone loss in those areas.
The most common type of overdenture today is the implant-retained overdenture, which attaches to dental implants. As discussed with snap-in dentures, this method provides even greater stability than root-retained options and offers the significant benefit of preserving bone across the entire arch where implants are placed.
The key feature of all overdentures, whether root or implant-retained, is that they are removable by the patient. While they offer enhanced stability and comfort over traditional complete dentures, they are not fixed in place like implant-supported bridges or All-on-4 prosthetics. Overdentures are often an excellent option for individuals who require a full denture but desire better retention and stability than conventional dentures can provide, or for those who want to preserve existing bone or cannot have a fully fixed solution due to cost, bone limitations, or other factors. They represent a valuable intermediate step between traditional dentures and fully fixed implant solutions.
Types of Denture Materials: Acrylic Resin and Metal
Delving into the specifics of dentures inevitably brings us to the materials from which they are crafted. The choice of material impacts not just the aesthetics but also the strength, weight, durability, and cost of the prosthesis. The most ubiquitous material in denture fabrication is acrylic resin. This versatile plastic is widely used for the pink, gum-colored base (or ‘saddle’) of most types of dentures – traditional full dentures, immediate dentures, snap-in dentures, and even the non-framework parts of some partial dentures. Acrylic resin is relatively easy to mold, adjust, and repair, making it a practical choice for many applications. It can be tinted to match the natural color of gum tissue, contributing to a natural appearance. However, acrylic can be somewhat brittle and, especially when used for the base of full dentures, needs sufficient bulk to provide strength, which can sometimes make the denture feel thick or bulky in the mouth.
For the artificial teeth themselves, the most common materials are either acrylic resin or porcelain. Acrylic teeth are softer, more resilient, and generally kinder to any opposing natural teeth or restorations. They are also easier to adjust and bond well to the acrylic base. Porcelain teeth, on the other hand, are harder, more durable, and resistant to staining, often maintaining their shape and color longer. They can provide a very natural appearance, reflecting light much like natural enamel. However, their hardness means they can cause wear on opposing natural teeth or other prosthetic teeth, and they are more brittle, prone to chipping or breaking if dropped.
Metal, specifically a strong alloy like cobalt-chromium (chrome-cobalt), plays a significant role in the construction of some partial dentures. Unlike acrylic partials which have a bulkier acrylic base covering the palate or lingual area (behind the lower teeth), cast metal partial dentures feature a thin, strong metal framework onto which the acrylic base and artificial teeth are attached. This metal framework provides exceptional strength, stability, and durability while being significantly thinner and less bulky than an all-acrylic base. The metal clasps are also highly retentive, gripping onto remaining teeth securely. While metal partials are highly functional and durable, a potential drawback is the visibility of the metal clasps, though sometimes designs can minimise this or alternative attachment methods can be used. Flexible dentures, as discussed, introduce thermoplastic materials like nylon, offering flexibility and aesthetic clasps as an alternative material choice for the base and clasps of partials.
Cosmetic, Custom, and Economy Dentures
Beyond the functional classification by type (partial, full, fixed), dentures can also be categorised by their quality, the level of customisation, and consequently, their cost. This is where terms like “Economy,” “Standard,” “Custom,” and “Cosmetic” dentures come into play, reflecting the spectrum of craftsmanship and materials used in their creation.
At the entry level, we often find Economy or basic Standard dentures. These are typically the most affordable option. They are often fabricated using pre-manufactured teeth and standard acrylic materials, based on average measurements rather than highly personalised details. While they provide basic function, the level of customisation in terms of fit, tooth shade, shape, and arrangement to match individual facial features is minimal. The focus is on providing a functional replacement at the lowest possible cost.
Moving up the scale are Custom or mid-range Standard dentures. These involve more detailed measurements and impressions of the patient’s mouth. The dentist and dental lab technician put more effort into selecting and arranging the artificial teeth to better suit the patient’s face, age, and desired appearance. Better quality acrylics and potentially higher-grade teeth might be used. The fit is generally better than economy dentures, leading to improved comfort and stability.
At the higher end are Premium or Cosmetic dentures. These represent the pinnacle of denture craftsmanship and aesthetic potential. They are highly customised, involving detailed assessments of facial structure, lip line, gum contours, and even personality to create teeth that look incredibly natural and are specifically designed for the individual. High-quality, multi-layered artificial teeth that mimic the subtle variations in natural tooth color and translucency are used. The acrylic base is often crafted with more realistic color variations to resemble natural gum tissue more closely. Premium dentures require greater skill and time from both the dentist and the dental technician, often involving multiple try-in appointments to fine-tune the aesthetics and fit before the final processing. The focus is equally on optimal function, maximum comfort, and achieving the most natural and aesthetically pleasing result possible. While significantly more expensive than economy options, premium dentures can provide a level of confidence and natural appearance that is truly transformative.
What’s the Difference Between Full & Partial Dentures?
The fundamental difference between full and partial dentures lies in the extent of tooth loss they are designed to address. It’s a key distinction that dictates the design, support mechanism, and suitability for a patient’s specific situation.
Full dentures are indicated when a patient has lost *all* the natural teeth in a single arch (either the upper or the lower jaw). They are a complete replacement for an entire set of teeth in that arch. The prosthetic consists of a full complement of artificial teeth mounted on a gum-colored base. As previously mentioned, traditional full dentures rely primarily on the underlying gum tissue and bone for support, using suction (especially in the upper jaw) and muscular control of the tongue and cheeks (especially in the lower jaw) to stay in place. They effectively restore the ability to chew and speak when the entire arch is edentulous, and they also provide essential support for the facial muscles, preventing the collapsed appearance that can occur after complete tooth loss. They are removable for cleaning.
Partial dentures, conversely, are used when a patient is missing *some* teeth in an arch, but still retains several natural, healthy teeth. They are designed to fill the gaps created by the missing teeth while leaving the existing natural teeth untouched or incorporating them into the denture’s support structure. A partial denture consists of replacement teeth attached to a base, which is often connected to the remaining natural teeth via clasps or other attachments. These remaining natural teeth serve as anchors, providing stability and support for the partial denture alongside the gum tissue under the base. Partial dentures prevent the remaining teeth from shifting into the spaces left by the missing teeth, maintain proper bite alignment, and restore chewing function in the areas where teeth are missing. Like most traditional partial dentures, they are typically removable for daily cleaning.
In summary: if you’re missing *all* teeth in an arch, you need a full denture (or a full-arch fixed prosthetic). If you’re missing *some* teeth but still have others, a partial denture is the appropriate traditional solution. The choice between them is directly determined by the patient’s remaining natural dentition status. While this is the basic distinction, the introduction of implant-supported options complicates things slightly, as you can have both full and partial *implant-supported* prosthetics, providing a fixed or more stable removable alternative to their traditional counterparts.
Which type of denture is best?
Ah, the million-dollar question! Or perhaps, given the costs of some options, the multi-thousand-dollar question. It’s the query most people have when starting their journey to replace missing teeth: “Which one is *the best*?” The answer, as with many things in life and especially in healthcare, is not a simple one-size-fits-all. There is no single “best” type of false teeth that suits everyone. The optimal choice is inherently subjective and depends entirely on the individual patient’s unique circumstances, needs, desires, and limitations.
Think of it like choosing a mode of transport. A bicycle is great for a short commute on a sunny day, but utterly useless for crossing an ocean. A sports car is thrilling but impractical for hauling furniture. Similarly, the ‘best’ denture for you is the one that most effectively addresses your specific situation while aligning with your priorities. Several critical factors come into play when determining the most suitable type:
- Number and Location of Missing Teeth: Are you missing a single tooth, a few spread out, or all of them in an arch? This immediately narrows down the options between partial and full replacements.
- Jawbone Health and Density: Sufficient healthy bone is crucial, particularly for implant-supported options. If bone loss is significant, grafting might be needed, or some implant options might be impossible, steering you towards traditional or different implant solutions.
- Overall Health: Chronic health conditions, certain medications, and habits like smoking can affect healing and the success rate of surgical procedures like implant placement.
- Budget: Denture options vary significantly in cost, from basic removable dentures being the most affordable to fixed implant-supported prostheses being the most expensive. Financial resources play a major role in the decision-making process.
- Lifestyle and Expectations: How important is maximum stability for eating and speaking? Do you want a solution that feels as close to natural teeth as possible? Are you comfortable with a removable appliance? Your daily habits and what you hope to achieve will influence the choice.
- Aesthetic Goals: How important is the natural appearance of the prosthetic? Some options offer higher levels of customisation and aesthetic realism than others.
- Manual Dexterity: Cleaning some types of dentures, particularly fixed implant-supported ones which require cleaning under the bridge, demands good dexterity. Removable dentures might be easier for some individuals to keep clean.
While implant-supported options, particularly fixed ones, are often considered the “gold standard” in terms of stability, function, and bone preservation – arguably offering the closest experience to natural teeth – they are not suitable or desirable for everyone due to cost, health, or surgical considerations. Traditional removable dentures, while having limitations, remain an excellent, accessible, and often perfectly satisfactory option for many people. The “best” denture is ultimately the one recommended by your dentist after a thorough examination and discussion, the one that you can afford, and the one that meets your most important needs and allows you to smile confidently and function comfortably.
Different types of dentures – pros and cons explained
Every tooth replacement option comes with its own set of advantages and disadvantages. There’s no perfect solution that is simultaneously the most affordable, least invasive, most stable, most comfortable, and longest-lasting for every single person. Understanding the trade-offs associated with each major type is crucial for making an informed decision alongside your dental professional. Here, we break down the key pros and cons of the main categories and notable specific types we’ve discussed:
Removable Full Dentures (Conventional):
- Pros: Generally the most affordable option. Non-invasive procedure (beyond necessary extractions). Relatively quick fabrication process. Restores basic chewing and speaking ability. Provides facial support.
- Cons: Can be unstable, particularly the lower denture, often requiring adhesive. May affect speech and eating initially. Does not prevent bone loss over time, leading to potential changes in fit and facial structure. Require daily removal for cleaning. Can sometimes feel bulky or cover the palate (upper). Reduced chewing efficiency compared to natural teeth or implant options.
Removable Partial Dentures (Conventional – Acrylic or Metal Framework):
- Pros: Fills gaps left by missing teeth. Prevents remaining teeth from shifting. Restores chewing and speech in missing areas. Less costly than bridges or implants.
- Cons: Can put strain on the natural anchor teeth over time (especially with clasps). May not be as stable as fixed options. Requires daily removal for cleaning. Metal clasps can be visible (with metal framework types). Acrylic types can be bulky.
Fixed Dentures (Implant-Supported Bridges / Full Arch Fixed):
- Pros: Highly stable and secure – feels and functions most like natural teeth. No need for removal by the patient. Excellent chewing power and ability to eat a wide range of foods. Preserves jawbone, maintaining facial structure. Eliminates need for adhesives. High confidence and comfort level. No palate coverage (upper).
- Cons: Highest initial cost. Requires surgical procedure for implant placement. Longer treatment time (including healing period). Requires diligent cleaning around implants and under the bridge using special tools. Cannot be easily adjusted by the patient.
Implant-Retained Overdentures (Snap-In Dentures):
- Pros: Significantly more stable and retentive than conventional full dentures. Improves chewing and speaking compared to traditional full dentures. Less bulky than traditional full dentures (especially upper, can often leave palate open). Helps preserve jawbone where implants are placed. Removable for easy cleaning. Less costly than fixed implant dentures as fewer implants are typically needed.
- Cons: Still removable, not a fixed solution. Less chewing power than fixed implant dentures. Requires daily removal and cleaning of both denture and implant attachments. Initial cost is higher than traditional dentures.
Immediate Dentures:
- Pros: Provides teeth immediately after extractions, ensuring no toothless period. Aids in initial healing and transition to wearing dentures. Maintains aesthetics, speech, and initial function.
- Cons: Temporary solution; fit will change significantly as gums and bone heal. Requires multiple adjustments and relines. Will eventually need replacement with a conventional or implant-supported denture. Fit is based on pre-extraction predictions, not healed tissues.
Flexible Partial Dentures:
- Pros: Comfortable due to flexible material. Often less bulky than acrylic partials. Aesthetic, gum-colored clasps are less noticeable than metal.
- Cons: May not be suitable for replacing many teeth or for heavy chewing areas. Can be difficult to reline or repair. Potential hygiene challenges if not cleaned properly. Lacks the rigidity needed for maximum stability in some cases.
This summary provides a quick glance at the major trade-offs involved. Your dentist will discuss these in detail and help you weigh which pros are most important to you and which cons you are willing to accept based on your specific clinical picture and priorities.
Can false teeth be permanent?
The concept of “permanent” when applied to false teeth or dentures requires careful definition. In the context of traditional, removable dentures (both full and partial), the answer is a definitive no. These prosthetics are not permanent. The materials from which they are made, primarily acrylic resin and artificial teeth (resin or porcelain), are subject to wear and tear over time. The fit of traditional dentures also changes as the underlying bone and gums resorb (shrink) following tooth loss. While a conventional denture might last for several years, the acrylic base typically needs to be relined (material added to improve fit) every couple of years due to tissue changes, and the entire denture usually requires replacement every 5 to 10 years as the fit becomes too poor or the materials degrade significantly. The teeth might wear down or stain over time as well.
However, when we consider fixed, implant-supported dentures (like fixed bridges or All-on-4), the term “permanent” becomes more applicable, though perhaps still not in the sense of ‘lasting forever without any maintenance’. The dental implants themselves, which are surgically placed into the jawbone to act as roots, are designed to be a permanent fixture in the bone, potentially lasting a lifetime with proper care and oral hygiene. The *prosthetic* (the fixed bridge or denture structure) that is attached to these implants is highly durable and fixed in place, not removable by the patient. This makes it the closest thing to a permanent tooth replacement currently available. While the implants are permanent, the prosthesis attached to them is still a dental restoration made of materials that can wear or be subject to damage over a very long period. It may require maintenance, repair, or eventual replacement (typically after 10-20 years or even longer, depending on materials, wear, and patient care) though this is far longer than the lifespan of traditional removable dentures.
So, while you won’t have a removable denture for life, fixed implant-supported options offer a form of tooth replacement that is permanently anchored and designed for very long-term service, bringing it much closer to the idea of a permanent solution for missing teeth. It’s best to discuss with your dentist what “permanent” means in the context of your specific chosen treatment plan.
What type of dentures are the most comfortable?
Comfort is a highly subjective sensation, and what one person finds comfortable, another might not. However, based on patient feedback and the biomechanics of different denture types, certain options are generally reported as being more comfortable than others. The primary driver of denture comfort is often stability and fit. A denture that stays securely in place, doesn’t rub, pinch, or move excessively while speaking or eating is inherently more comfortable than one that is loose or ill-fitting.
Considering this, implant-supported dentures, particularly the fixed types, are widely regarded as the most comfortable. Because they are anchored directly to the jawbone via implants, they do not move or slip. There’s no friction against the gums caused by movement, and the chewing forces are transmitted more naturally through the implants to the bone, rather than pressing down on the gum tissue. Fixed implant dentures also don’t cover the palate (in the upper jaw), which can significantly improve comfort, taste, and temperature perception, making them feel less like a foreign object in the mouth. Even removable snap-in overdentures, by virtue of their attachment to implants, are significantly more stable and generally more comfortable than traditional full dentures.
Among removable options, flexible partial dentures are often cited as being particularly comfortable, especially for small partials. Their flexible nature allows them to adapt well to the contours of the mouth, and the lightweight material can feel less intrusive than rigid acrylic or metal framework partials.
Traditional removable full dentures, while a viable solution, are frequently cited as being less comfortable than implant options, especially the lower denture due to its inherent lack of stability and reliance on muscle control. The upper traditional denture, with its palatal coverage and suction, can be more stable and comfortable than the lower, but some people find the palate coverage reduces comfort and interferes with taste.
Ultimately, achieving comfort with *any* type of denture relies heavily on two things: a precise fit, initially and maintained over time (through relines or adjustments), and proper care and adaptation by the wearer. A well-made traditional denture can be relatively comfortable, while a poorly fitting implant denture can still cause problems. Regular dental check-ups are essential to ensure the fit remains optimal for maximum comfort, regardless of the type chosen.
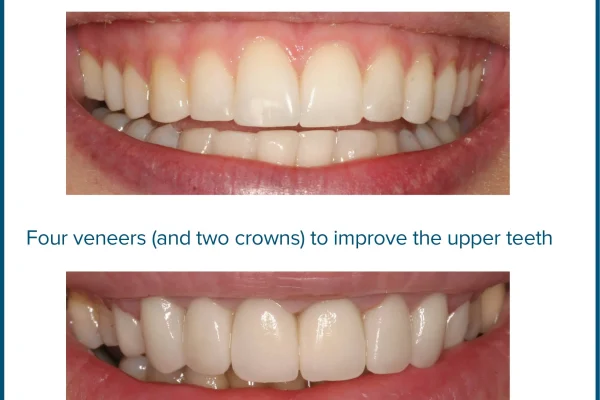
What type of dentures are most natural looking?
Achieving a natural look with false teeth is a major priority for many people, profoundly impacting self-confidence and social interactions. Several factors contribute to how natural a denture appears, and certain types offer greater potential for realism than others.
The key elements of a natural-looking denture are:
- Tooth Appearance: The shape, size, color, and arrangement of the artificial teeth. High-quality teeth mimic the subtle variations, translucency, and surface characteristics of natural teeth.
- Gum Appearance: The color, contour, and texture of the acrylic base. A skilled technician can customise the base to look like healthy gum tissue, matching the patient’s natural gum color and even sculpting it to mimic the look of natural roots or bone contours.
- Fit and Positioning: How the denture sits in the mouth relative to the lips and face. A well-fitting denture supports the facial tissues properly, preventing a sunken look, and the teeth should be positioned to look harmonious with the patient’s facial features and age.
Considering these factors, premium or cosmetic custom dentures (both removable and fixed) offer the highest potential for a natural look. These involve significant chair time with the dentist for precise measurements and try-ins, and meticulous work by a skilled dental technician using high-quality materials. The dentist and technician work together to select teeth that are individually chosen and arranged to look like the patient’s original teeth (if photos are available) or designed to be aesthetically pleasing and appropriate for their face. The gum base is also highly customised for a realistic appearance.
Fixed implant-supported dentures (like fixed bridges or All-on-4) often achieve a very natural look because they emerge from the gum line in a way that closely resembles natural teeth. They don’t have a bulky base covering the palate, and the fixed nature allows for precise positioning that feels and looks authentic. Because the implants preserve bone, they help maintain the natural facial contours over time, which is essential for long-term aesthetics.
Removable dentures, even premium ones, can sometimes have limitations. Traditional partial dentures with visible metal clasps are less aesthetic than flexible partials with gum-colored clasps or those using precision attachments. Traditional full dentures, while capable of looking quite natural in the teeth themselves, sometimes have a bulkier gum base or cover the palate, which can affect the overall perception of naturalness compared to fixed options.
Ultimately, the most natural-looking dentures are not just about the *type* (though implant-supported and high-end custom options have an edge) but equally about the *quality* of the materials, the *skill* of the dental team, and the level of *customisation* applied to the prosthesis to make it uniquely suited to the individual wearer.
What is the longest lasting fake teeth?
When considering the longevity of different false teeth options, it’s important to distinguish between the lifespan of the anchoring mechanism (if any) and the lifespan of the prosthetic teeth and base themselves.
The components designed for the longest potential lifespan are dental implants. The titanium posts surgically placed into the jawbone are intended to integrate with the bone and, with diligent oral hygiene and regular dental check-ups, can last a lifetime. They are not subject to the same wear and tear as the prosthetic teeth.
The prosthetic structures attached to implants – specifically fixed implant-supported bridges or dentures – are generally the longest-lasting *false teeth* structures. While the implants themselves are permanent, the bridge or denture attached to them is typically made of durable materials like high-quality acrylic, porcelain, zirconia, or composite bonded to a strong framework. These prosthetics are designed to withstand daily chewing forces and can last significantly longer than traditional removable dentures. The lifespan of a fixed implant prosthesis is often cited as 10 to 20 years, and sometimes even longer, before needing significant repair or replacement, although components like artificial teeth can wear down or the acrylic can require maintenance over this period.
In contrast, traditional removable dentures (both full and partial) have a considerably shorter lifespan. The acrylic base changes fit as the jawbone shrinks over time, and the materials are less durable under daily stress. Conventional dentures typically require relining every 2-3 years to improve fit and comfort and usually need to be replaced entirely every 5 to 10 years. Flexible partial dentures may also have a shorter lifespan than traditional acrylic or metal partials due to potential challenges with repair and relining.
Therefore, if longevity of the prosthetic itself is a primary concern, fixed implant-supported dentures represent the longest-lasting option, built upon the potentially lifelong foundation of dental implants. This long-term durability contributes to their higher initial cost but can offer value over time compared to the need for periodic replacement of traditional dentures.
What is the most expensive fake teeth?
Without question, the most expensive false teeth options are those that involve dental implants, particularly fixed implant-supported full-arch prostheses like the All-on-4 technique or full bridges supported by multiple implants (6 or more). The cost is driven by several factors:
- The Implants Themselves: Each dental implant is a precision-engineered medical device made of biocompatible titanium (or sometimes zirconia). The implants themselves are costly.
- Surgical Procedure: Placing dental implants is a surgical procedure requiring the skill and expertise of a trained implant dentist or oral surgeon. The surgical fee is a significant component of the overall cost.
- Number of Implants: The more implants needed, the higher the cost. Fixed full-arch solutions typically require 4 to 6+ implants per arch, while removable overdentures might use 2-4.
- The Prosthetic: The fixed bridge or denture attached to the implants is a complex, often highly customised restoration made from durable materials. Crafting this prosthetic requires skilled lab work and potentially more expensive materials (like zirconia frameworks).
- Ancillary Procedures: Sometimes, additional procedures like tooth extractions, gum disease treatment, or bone grafting (essential if there isn’t enough bone for implants) adds significantly to the total cost.
- Complexity: Full-arch fixed restorations are more complex than single-tooth implants or simple removable dentures.
Consequently, replacing an entire arch of teeth with a fixed implant-supported denture can be a substantial investment, often ranging from several thousand to tens of thousands of dollars per arch, depending on the factors above, geographic location, and the specific dental practice.
In contrast, traditional removable full and partial dentures are generally the least expensive options. They do not require surgical placement of implants (beyond necessary extractions) and involve less complex fabrication processes and materials compared to fixed implant solutions. Flexible partial dentures might fall somewhere between traditional partials and basic implant overdentures in terms of cost.
So, while traditional dentures offer an accessible entry point in terms of cost, the most significant investment in tooth replacement comes with the stability, function, and bone preservation benefits offered by implant-supported solutions.
What are the newest types of dentures?
The field of dental prosthetics is constantly evolving, driven by advancements in materials science, digital technology, and surgical techniques. While the fundamental concepts of partial and full tooth replacement remain, the “newest” types of dentures often represent refinements, technological integration, and innovative approaches within these categories, particularly leveraging digital workflows and implantology.
One significant area of advancement isn’t necessarily a completely *new* type of denture but rather new *methods* of designing and fabricating existing types. Digital Denture Design and Manufacturing (CAD/CAM) is increasingly prevalent. Dentists can now take digital impressions of the mouth, and dentures can be designed on a computer (CAD – Computer-Aided Design) and then milled or 3D printed from high-quality materials (CAM – Computer-Aided Manufacturing). This offers the potential for greater precision, faster fabrication, and more consistent results compared to traditional manual laboratory processes. Digital workflows can be applied to both removable and fixed prosthetics.
In terms of specific types, the focus continues to be on enhancing the stability and biological compatibility of dentures, primarily through implant-based solutions. While implant-supported dentures aren’t brand new, ongoing research and development lead to:
- Improved Implant Designs: Implants with surfaces that promote faster and stronger bone integration.
- New Abutment Designs: The connectors between the implant and the prosthetic are constantly refined for better load distribution and ease of cleaning.
- Advancements in Materials for Fixed Prostheses: Materials like monolithic zirconia (a highly strong and aesthetic ceramic) are increasingly used for fixed implant bridges, offering greater durability and natural aesthetics than previous acrylic-based options on metal frameworks.
- Streamlined Implant Protocols: Techniques like All-on-4 or other ‘immediate load’ protocols continue to be refined, allowing patients to receive fixed or snap-in prosthetics sooner after implant placement.
There are also ongoing developments in the materials used for removable dentures, aiming for better aesthetics, comfort, and durability, such as newer generations of thermoplastic materials for flexible partials or more advanced acrylics for bases and teeth.
So, the “newest” types aren’t always revolutionary concepts but often represent the integration of cutting-edge technology and materials into existing treatment modalities, making them more predictable, efficient, comfortable, and aesthetically pleasing, particularly within the realm of implant dentistry.
Are false teeth better than implants?
This is a classic comparison, and much like “Which type of denture is best?”, the answer is that one isn’t universally “better” than the other. They are fundamentally different solutions for tooth replacement, each with its own strengths, weaknesses, and ideal use cases. The choice depends entirely on the individual’s specific clinical situation, health status, financial resources, and treatment goals.
Traditional False Teeth (Removable Dentures – Partial or Full):
- Pros: Generally less expensive. Non-surgical (beyond extractions). Faster treatment time. Suitable for patients who cannot undergo surgery or have significant bone loss that makes implant placement difficult or impossible without extensive grafting.
- Cons: Less stable, prone to movement (especially lower full dentures). Lower chewing efficiency. Can affect speech. Do not prevent bone loss over time, leading to changes in fit and potential facial collapse. Need to be removed for cleaning. Can cause sore spots.
Dental Implants (used to support crowns, bridges, or dentures):
- Pros: Replaces the tooth root, providing unmatched stability for the prosthetic. Preserves jawbone, preventing bone loss and maintaining facial structure. Feels and functions most like natural teeth. High chewing efficiency. Does not rely on adjacent natural teeth for support (as with traditional bridges or partials using clasps). Can last a lifetime (the implant itself). High patient satisfaction.
- Cons: Higher initial cost. Requires surgical procedure(s) and healing time. Not suitable for all patients (e.g., those with certain medical conditions, uncontrolled diabetes, heavy smokers, or significant bone deficiency without grafting). Treatment time can be longer.
So, are false teeth *better* than implants?
* If your priority is the lowest upfront cost, minimal invasiveness, and a relatively quick solution, then traditional removable dentures might be “better” for you.
* If your priority is maximum stability, preservation of jawbone, a feel and function closest to natural teeth, and long-term value, and you are a suitable candidate, then dental implants (supporting either single crowns, bridges, or dentures) are likely “better”.
Often, the conversation isn’t *Implants vs. Dentures* but rather *Traditional Removable Dentures vs. Implant-Supported Dentures*. In this comparison, the implant-supported option almost always offers significant advantages in terms of stability, function, and bone health, effectively combining the benefits of implants with a denture-like prosthetic. The choice should always be made in consultation with a dentist who can fully evaluate your situation and explain which option is most appropriate for *your* needs and circumstances.
Types of Dentures and Cost: What Should I Consider When Getting Dentures?
The cost of dentures is a major factor for most people considering tooth replacement, and it varies dramatically based on the type of denture chosen and several other contributing elements. Understanding what goes into the price can help you budget and make informed decisions during your consultation. The range can be vast, from a few hundred dollars for a basic temporary partial to tens of thousands for a full-arch fixed implant-supported prosthesis.
Here’s what influences the overall cost:
- Type of Denture: As we’ve discussed, traditional removable dentures are the least expensive. Partial dentures typically cost less than full dentures of the same quality level. Implant-retained overdentures (snap-in) are more expensive than traditional removable dentures but less than fixed implant-supported dentures, which are the most costly.
- Quality and Customisation: Economy or standard dentures made with basic materials and less customisation are cheaper than premium or cosmetic dentures that use high-quality materials, precise techniques, and significant chair time for customisation and fitting.
- Materials Used: Metal framework partials are often more expensive than acrylic partials but less so than flexible partials in some cases. The type of teeth used (resin vs. porcelain vs. higher-end multi-layered teeth) also affects the price. For implant prosthetics, the framework material (e.g., titanium vs. zirconia) is a cost factor.
- Number of Implants (for Implant Options): More implants mean higher costs for the implants and the associated surgical procedures.
- Associated Procedures: The need for preliminary work like tooth extractions, gum disease treatment, or bone grafting (essential if there isn’t enough bone for implants) adds significantly to the total cost.
- Laboratory Fees: The cost charged by the dental laboratory to fabricate the denture or prosthesis is a significant portion of the total fee. Lab fees vary based on the complexity, materials, and technology used (e.g., traditional vs. digital design/manufacturing).
- Dentist’s Fees: The cost of consultations, impressions, fittings, adjustments, and the dentist’s professional fees vary based on their experience, specialisation (e.g., general dentist vs. prosthodontist vs. oral surgeon for implants), and geographic location. Dental costs are often higher in urban areas or regions with a higher cost of living.
When getting dentures, it’s crucial to have a detailed discussion with your dentist about the total cost of the proposed treatment plan. This should include the cost of the denture itself, any necessary preliminary procedures (like extractions), potential costs for adjustments or relines down the line (for removable dentures), and the cost of implant surgery and the final prosthetic (if choosing an implant option). Inquire about payment plans, financing options, and what portion of the cost, if any, might be covered by your dental insurance or government programs. Don’t choose a denture solely based on the lowest price; consider the long-term value, potential maintenance costs, comfort, and impact on your quality of life when making your decision.
How to Care for Different Types of Dentures?
Proper care is essential for maintaining the longevity, function, and hygiene of any type of false teeth, as well as ensuring the health of your remaining oral tissues. While specific instructions may vary slightly depending on the type of denture, some fundamental principles apply across the board.
General Denture Care (Applies primarily to Removable Types):
- Daily Cleaning: Dentures should be cleaned daily, similar to natural teeth. Use a soft-bristled brush specifically designed for dentures or a regular soft toothbrush. Clean all surfaces – the teeth, the base, and any surfaces that touch your gums or palate. Use a non-abrasive denture cleaner or mild soap; regular toothpaste can be too abrasive and cause microscopic scratches where bacteria can accumulate.
- Rinse After Eating: After meals, remove your denture and rinse it under running water to remove food particles.
- Soaking: Most removable dentures should be soaked daily in a denture cleaning solution (following the product instructions). Soaking helps remove stains, kills bacteria, and keeps the denture moist, preventing it from drying out and losing its shape. *Check manufacturer instructions, as some flexible materials should not be soaked in certain solutions.*
- Handling with Care: Always handle your denture over a soft towel or basin of water. If you drop it, it can easily break.
- Removing Overnight: For most traditional removable dentures, it is recommended to remove them at night to allow your gums to rest and receive adequate blood circulation. Store them in water or a soaking solution to prevent drying out. (Implant-retained overdentures might have slightly different overnight instructions depending on the attachment type).
- Clean Your Mouth: Even if you have no natural teeth, it’s important to clean your gums, tongue, and palate every morning and evening with a soft brush or cloth to remove plaque and stimulate circulation. If you have a partial denture, brush your remaining natural teeth thoroughly, paying extra attention to the surfaces that the denture clasps touch.
Care for Fixed Implant-Supported Dentures:
- While fixed dentures aren’t removed by the patient, they still require meticulous daily cleaning. Food particles and plaque can accumulate around the implants and under the bridge structure.
- Special cleaning tools are necessary, such as interdental brushes, floss threaders, water flossers (oral irrigators), and proxy brushes, to clean around the implants and under the fixed bridge.
- Your dentist or hygienist will show you the specific techniques and tools required for your particular type of fixed prosthesis.
- Regular professional cleanings with a hygienist who is trained in implant maintenance are crucial.
Regardless of Type:
- Regular Dental Check-ups: Even if you have no natural teeth, regular visits to your dentist (usually every 6-12 months) are vital. The dentist will examine your mouth for signs of gum disease, oral cancer, and check the fit and condition of your denture. For implant dentures, they will also check the health of the implants and the integrity of the prosthesis.
- Adjustments and Relines: Over time, the fit of dentures can change. If your denture feels loose, uncomfortable, or causes sore spots, do not try to adjust it yourself. See your dentist for a professional adjustment or reline.
Following proper care instructions is key to protecting your investment, maintaining your oral health, and ensuring your dentures remain functional and comfortable for as long as possible.
What Are the 9 Different Types of Dentures?
The idea of numbering the types of dentures – whether it’s 4, 7, 9, or another number – often arises from attempts to simplify and categorise the wide array of options available. However, there isn’t one universally agreed-upon list that results in exactly nine distinct types. The number can change depending on how you group or sub-categorise the different options based on materials, support, removability, or intended use.
Instead of adhering strictly to a number, it’s more useful to understand the main categories and the common variations within them. If we were to attempt to arrive at a number like nine by breaking down the options discussed in this guide, a possible (though not definitive) list might look something like this:
- Traditional Complete Full Dentures: Removable, replacing all teeth in one arch, resting on gums.
- Traditional Removable Partial Dentures (Acrylic Base): Replacing some teeth, using acrylic base and clasps on remaining teeth.
- Traditional Removable Partial Dentures (Metal Framework): Replacing some teeth, using a thin metal framework and clasps on remaining teeth.
- Flexible Partial Dentures: Replacing some teeth, using flexible thermoplastic material and aesthetic clasps.
- Immediate Dentures: Temporary dentures inserted immediately after extractions.
- Implant-Retained Overdentures (Snap-In Dentures): Removable full dentures supported by 2-4 implants.
- Implant-Supported Fixed Partial Dentures (Implant Bridge): Fixed bridge replacing a section of teeth, anchored to implants.
- Implant-Supported Fixed Full Dentures (Full Arch Fixed Prosthesis / Hybrid Denture): Fixed full arch replacement anchored to multiple implants (e.g., 4 or more).
- Root-Retained Overdentures: Removable dentures supported by retained natural tooth roots.
This list reaches nine by separating traditional partials by material, distinguishing immediate dentures, and splitting implant dentures into removable overdentures, fixed partials, and fixed full prostheses, plus adding the less common root-retained type. Other counts might group partials differently, or include temporary flippers as a distinct type, or perhaps list upper and lower dentures separately for some categories. The exact number is less important than grasping the core concepts: the difference between removable and fixed, the impact of implant support, and the various designs and materials available to address different levels of tooth loss and patient needs. Focus on understanding the characteristics and suitability of each option rather than memorizing a numbered list.
Frequently Asked Questions About types of false teeth
Navigating the world of false teeth can bring up a host of questions. Here are some of the most frequently asked ones, offering concise answers based on what we’ve explored:
What types of dentures are available?
A wide array of types exists today, far beyond the simple “plate.” The main categories include removable dentures (partial and complete/full), and implant-supported dentures (which can be either removable or fixed). Within these, there are variations based on materials (acrylic, metal, flexible thermoplastics), specific designs (immediate dentures, overdentures, fixed bridges, All-on-4), and quality levels (economy, standard, custom, cosmetic). The available type depends on your specific needs, oral health, and budget.
What are partial dentures?
Partial dentures are removable prosthetic devices used to replace one or more missing teeth in an arch when some healthy natural teeth still remain. They prevent the remaining teeth from shifting, restore chewing function in the gaps, and improve aesthetics. They typically consist of replacement teeth on a gum-colored base, often with clasps that attach to the natural teeth for support.
What are full dentures?
Full dentures, also known as complete dentures, are removable prosthetics designed to replace all the natural teeth in a single dental arch (upper or lower). They consist of a full set of artificial teeth on a gum-colored base that rests directly on the gums and bone ridge. Upper full dentures rely on suction for retention, while lower ones depend more on muscle control and fit, often requiring adhesive.
What are snap-in dentures?
Snap-in dentures are a type of removable full or partial denture that attaches to a small number of dental implants (usually 2-4) via special connectors. They “snap” onto these implants, providing significantly greater stability and retention than traditional removable dentures, while still allowing the wearer to remove them for cleaning. They are a popular option for those seeking more security than traditional dentures but not requiring a fully fixed solution.
Which type of denture is best?
There is no single “best” type of denture for everyone. The ideal choice is highly individual, depending on the number of missing teeth, jawbone health, overall health, budget, lifestyle, and personal preferences. While implant-supported dentures are often considered the most stable and functional, traditional dentures remain a suitable and accessible option for many. A consultation with a dental professional is essential to determine the best type for your specific situation.