Table of Contents
ToggleKey Takeaways
- Dental implant procedures are a multi-stage process involving surgical placement and osseointegration for a long-term tooth replacement.
- Costs for dental implants can be significant, varying by case complexity and clinic, with limited NHS availability in the UK.
- Potential risks include infection, implant failure, nerve damage, and peri-implantitis, though overall success rates are very high with proper care.
- Sedation options such as local anesthesia, oral sedation, and IV sedation are available to manage comfort and anxiety during the implant procedure.
- Recovery involves an initial healing phase of 1-2 weeks, followed by 3-6 months for osseointegration; specific dietary guidelines are crucial post-surgery.
Losing a tooth, or several, can feel like a significant blow. It’s not merely an aesthetic concern; it impacts how you eat, how you speak, and often, how you feel about yourself. For centuries, the solutions were rudimentary – think basic dentures or bridges that, while functional to a degree, often came with their own set of compromises. But dental science, much like a determined vine, has consistently reached for better, more sophisticated solutions. Enter the era of dental implants, a revolutionary approach that has fundamentally transformed the landscape of tooth replacement. This isn’t just about plugging a space; it’s about recreating a tooth from the root up, offering a permanence and stability that previous methods could only dream of. The benefits are manifold: imagine biting into an apple without a second thought, speaking with clarity and confidence, and smiling without the shadow of self-consciousness. Dental implants offer a return to normalcy, a way to turn back the clock on tooth loss and embrace a future where your dental health supports your overall well-being. This article aims to be your trusted co-pilot on this journey. We’ll navigate the intricacies of the implant procedure, from that crucial first conversation with your dentist to the moment you walk out with your fully restored smile, and even the care that follows. We’ll demystify the jargon, address the common anxieties, and provide a clear, comprehensive overview, ensuring you’re well-informed and empowered every step of the way. Consider this your A-to-Z guide, meticulously crafted to answer your questions before you even think to ask them, shining a light on the path to new teeth and a renewed sense of self. The journey to a restored smile is a significant one, and understanding each milestone will make the experience smoother and more predictable. We’re talking about a long-term investment in your health and happiness, and knowledge, as they say, is power.
What Does the General Dental Implant Procedure Entail? A Look at Having a Dental Implant
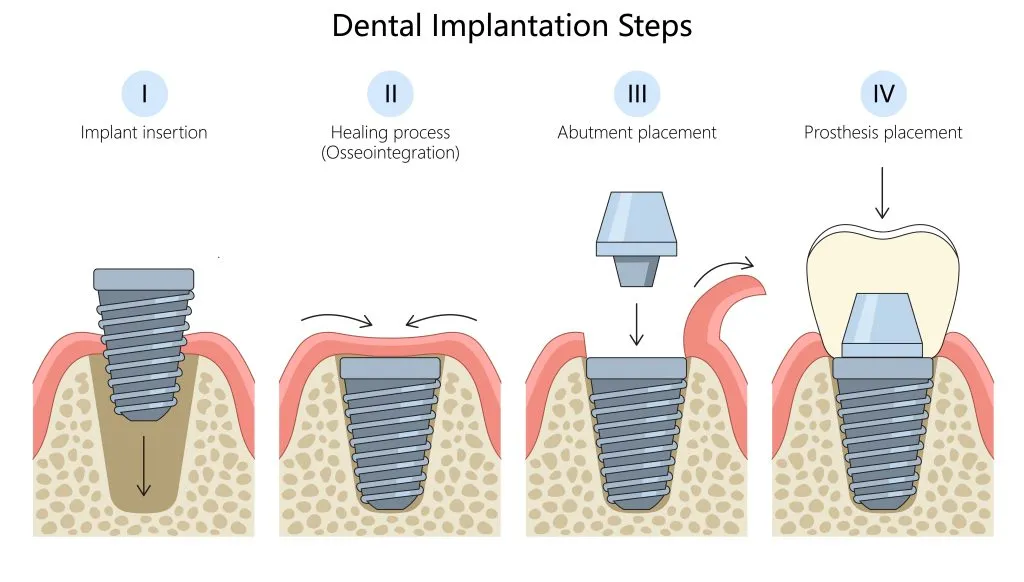
So, you’re contemplating “having a dental implant,” or perhaps several. It sounds futuristic, almost bionic, but at its core, the general dental implant procedure is a meticulously planned, multi-stage surgical and restorative process designed to provide a strong, durable, and aesthetically pleasing replacement for missing teeth. Think of it as engineering a new tooth from the ground up, starting with a new ‘root’. The procedure involves the surgical placement of a small, typically titanium, post into the jawbone where a tooth is missing. This post acts as an artificial tooth root, providing a sturdy foundation. Over time, a remarkable biological process called osseointegration occurs, where the jawbone fuses directly with the implant, creating an incredibly strong and stable base. Once this fusion is complete, an abutment, or connector, is attached to the implant, and finally, a custom-made crown (the visible part of the tooth) is fixed onto the abutment. The result? An artificial tooth that not only looks but also functions remarkably like your natural teeth. You can chew, speak, and smile with renewed confidence. It’s crucial to understand that this isn’t a quick, one-visit fix. “Having a dental implant” is a significant decision and a journey that requires careful planning, patience, and collaboration between you and your dental team. The initial consultations will involve thorough examinations, imaging (like X-rays or 3D scans), and discussions about your medical history and specific needs. This ensures that the treatment plan is tailored precisely to you, maximising the chances of a successful and long-lasting outcome. The beauty of the modern dental implant procedure lies in its predictability and high success rates when performed by experienced clinicians. It’s a sophisticated blend of surgical skill, advanced materials science, and artistic dentistry, all working in concert to restore not just a tooth, but a vital part of your daily life. It’s more than just filling a gap; it’s about restoring full function and aesthetics in a way that feels incredibly natural. The procedure itself is performed under local anaesthesia, meaning you’ll be awake but the area will be completely numb, ensuring comfort throughout the surgical phase. Many clinics also offer sedation options for patients who feel anxious, making the experience as stress-free as possible.
What are Dental Implants and What are Tooth Implants Made Of?
Let’s break it down further. When we talk about dental implants, we’re referring to sophisticated, medical-grade artificial tooth roots. Imagine a small, screw-like or cylindrical post. This isn’t just any piece of metal; it’s a marvel of bioengineering. These implants are surgically inserted into the jawbone, right where your natural tooth root once resided. Their primary purpose is to serve as a robust anchor for a replacement tooth or a set of teeth, such as a crown, bridge, or denture. The magic lies in their ability to integrate with your body.
The most common material used for tooth implants, and the gold standard for decades, is titanium. Why titanium? This remarkable metal possesses a unique combination of properties that make it exceptionally well-suited for this role. Firstly, it’s incredibly strong and durable, capable of withstanding the significant forces exerted during chewing and biting, year after year. Secondly, it’s surprisingly lightweight, which contributes to patient comfort. Most importantly, titanium is highly biocompatible. This means that the human body generally doesn’t recognize it as a foreign object, so it doesn’t trigger an immune rejection response. Instead, the bone actively grows onto and fuses with the titanium surface in that crucial process known as osseointegration, forming a permanent and incredibly stable bond.
While titanium reigns supreme, another material gaining traction is zirconia. Zirconia implants are a ceramic, metal-free alternative. They offer excellent biocompatibility and strength, and their tooth-like colour can be an aesthetic advantage, particularly for patients with thin gum tissue where a metal implant might subtly show through. The choice between titanium and zirconia will depend on various factors, including the patient’s specific clinical situation, aesthetic desires, and any (extremely rare) metal sensitivities.
Beyond the material, there are different types of implants designed for various scenarios. For instance, if you’re missing a single tooth, a single implant topped with a crown is a common solution. If multiple teeth are missing, several implants might be used to support a fixed bridge. For those missing all their teeth, a few strategically placed implants can securely anchor a full denture, often referred to as “implant-supported dentures” or “all-on-4” / “all-on-6” solutions, providing a significant upgrade from traditional removable dentures. You might also hear terms like “dental implant molar tooth” or “molar implant,” which simply refer to an implant specifically placed to replace a molar, one of the large chewing teeth at the back of your mouth, demanding robust support.
What is Implant Dentistry and How Does it Offer Dental Replacement?
Implant dentistry is a specialized and highly sophisticated branch of dental science dedicated entirely to the diagnosis, planning, surgical placement, and subsequent restoration of dental implants. It’s not just about filling a space; it’s about providing a comprehensive, long-term dental replacement solution that aims to replicate the form, function, and aesthetics of natural teeth as closely as possible. This field requires a deep understanding of oral anatomy, bone physiology, surgical techniques, and restorative principles. Dentists who specialize or have advanced training in implant dentistry are adept at evaluating a patient’s suitability for implants, developing precise treatment plans (often using advanced 3D imaging and digital planning tools), performing the surgical insertion of the implant posts, and then creating and fitting the final artificial teeth.
The way implant dentistry offers tooth replacement is fundamentally different from older, more traditional methods. For example, conventional bridges rely on adjacent natural teeth for support, often requiring these healthy teeth to be ground down to accommodate the bridge. Dentures, while effective for many, can sometimes feel unstable, slip, or cause discomfort. Implant dentistry, however, offers a standalone solution. The implant itself acts as an artificial root, embedded directly into the jawbone. This not only provides unparalleled stability for the replacement tooth but also helps to preserve the surrounding bone. When a natural tooth is lost, the jawbone in that area can begin to resorb or shrink over time due to lack of stimulation. Dental implants stimulate the bone, much like natural tooth roots, helping to maintain its volume and density, which is crucial for long-term oral health and facial structure. It’s important to distinguish this from a “tooth transplant,” which is a biological procedure involving the transplantation of a natural tooth from one location to another, a much rarer and different concept. Implant dentistry focuses on engineered replacements.
The process often involves collaboration between different dental specialists, such as an oral surgeon or periodontist for the surgical phase, and a general or cosmetic dentist for the restorative phase (placing the crown or bridge), though many dentists are now trained to handle both aspects. Ultimately, implant dentistry offers a durable, reliable, and aesthetically superior method of tooth replacement, allowing patients to eat, speak, and smile with confidence, often for many decades.
What Are the Key Stages of the Process for Dental Implants?
The “process for dental implants” is not a single event but rather a carefully orchestrated series of stages, each playing a vital role in the journey towards a fully restored smile. Think of it as building a bespoke piece of architecture – there’s the blueprint phase, foundation work, construction, and finally, the finishing touches. While the specifics can be tailored to individual patient needs, the overarching framework generally follows a consistent path. It’s crucial to understand that this journey requires patience, as some stages involve healing periods that are essential for long-term success.
The number and exact nature of these stages can indeed vary. For instance, a patient with ample healthy jawbone might have a more streamlined process than someone who requires preliminary procedures like bone grafting to build up sufficient bone volume to support an implant. Your dental professional will walk you through your personalized treatment plan, ensuring you understand each step, its purpose, and the anticipated timeline.
Generally, the main stages we’ll delve into include the initial pre-operative assessment, which is all about planning and diagnosis. Then, if necessary, there’s the bone grafting stage, a preparatory step for some. This is followed by the core surgical stage: the actual placement of the implant. After a period of healing and osseointegration (where the implant fuses with the bone), the restorative treatment stage begins, which involves placing the abutment and the final crown or prosthetic. Each of these phases is critical. Rushing through them, especially the healing components, can compromise the outcome. Therefore, a clear understanding of this multi-step “process for dental implants” helps set realistic expectations and fosters a collaborative relationship between you and your dental team. This systematic approach is what underpins the high success rates associated with modern dental implants, ensuring that every aspect, from bone health to the final aesthetic outcome, is meticulously addressed. The journey is designed to be as comfortable and predictable as possible, leveraging advanced diagnostics and techniques to guide each decision.
What Occurs During Stage 1: The Pre-operative Assessment for Teeth Implantation?
The pre-operative assessment is the foundational cornerstone of the entire “teeth implantation” journey. This initial stage is paramount because meticulous planning here directly translates to predictable and successful outcomes. It’s far more than a quick look in your mouth; it’s a comprehensive deep-dive into your oral and general health. Typically, this stage involves several key components.
First, there’s a thorough comprehensive dental exam. Your dentist will meticulously examine your teeth, gums, and surrounding oral tissues, checking for any existing issues like gum disease or decay that need to be addressed before implant treatment can commence.
Next comes a detailed review of your medical history. This is crucial because certain systemic conditions (like uncontrolled diabetes or autoimmune disorders) or medications (such as bisphosphonates) can influence healing and implant success. Honesty and completeness here are vital.
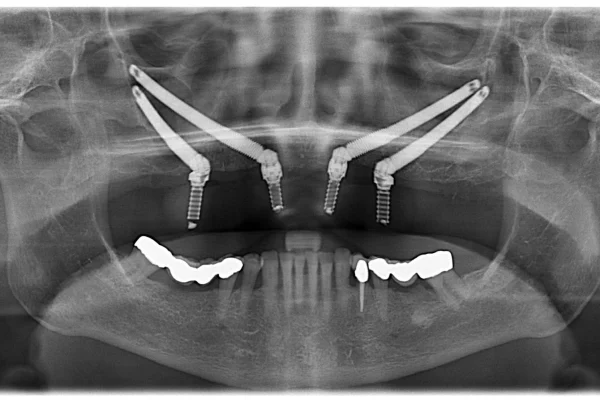
The most critical diagnostic tool in this phase is dental imaging. This usually starts with standard dental X-rays (2D panoramic X-rays) to get an overview of your jawbone structure and the position of existing teeth and nerves. However, for precise implant planning, a Cone Beam Computed Tomography (CBCT) scan is often employed. This advanced 3D imaging provides incredibly detailed cross-sectional views of your jawbone, allowing the dentist to assess bone density, volume, and height with remarkable accuracy. This information is indispensable for determining the optimal implant size, type, and exact placement location, while carefully avoiding vital structures like nerves and sinuses.
The importance of this stage for planning the “teeth implantation” cannot be overstated. It’s where your dentist determines if you are a suitable candidate, identifies if any preparatory procedures like bone grafting or a sinus lift are needed, and begins to map out the entire surgical and restorative strategy.
Finally, based on all this gathered information, a personalized treatment plan is created. This plan will outline the proposed number of implants, the type of restoration (crown, bridge, denture), the sequence of procedures, estimated timelines, and associated costs. This is also your opportunity to ask questions, discuss your goals and concerns, and ensure you feel completely comfortable and informed before proceeding. This meticulous groundwork ensures the subsequent stages of your implant journey are built on a solid, well-understood foundation.
Is Stage 2: Bone Grafting Always Part of the Tooth Implant Process?
A common question patients have regarding the “tooth implant process” is whether bone grafting is an inevitable step. The straightforward answer is no, bone grafting is not always required for every patient seeking dental implants. However, it is a relatively common and often crucial preparatory procedure for a significant number of individuals.
The necessity for bone grafting hinges entirely on the condition of your jawbone, specifically its volume and density in the area where the implant is to be placed. For a dental implant to be successful in the long term, it needs a solid foundation of healthy bone to integrate with and anchor into. If the jawbone is too thin, too soft, or has insufficient height, it may not be able to adequately support an implant. This lack of bone can occur for several reasons: it might be due to bone resorption that naturally happens after a tooth has been missing for a while (the bone shrinks because it’s no longer stimulated by a tooth root), severe periodontal (gum) disease that has eroded bone, trauma, or even developmental defects.
Bone grafting is a surgical procedure designed to augment or rebuild this missing bone, creating a more suitable environment for implant placement. During the procedure, bone material (or a bone-like substitute) is added to the deficient area of the jaw. This material can come from various sources: autograft (the patient’s own bone, often taken from another site in the mouth or hip – considered the gold standard by many), allograft (processed bone from a human donor, sourced from reputable tissue banks), xenograft (bone from an animal source, typically bovine, which is specially processed for safety and compatibility), or alloplast (synthetic, biocompatible materials). The grafted material acts as a scaffold, encouraging your own body to grow new bone cells into that area over time. This regeneration process can take several months, and the implant placement surgery is typically delayed until the graft has successfully integrated and matured into solid bone.
So, while not a universal step, bone grafting is an indispensable tool in the “tooth implant process” for many, enabling patients who might otherwise not be candidates for implants to benefit from this life-changing treatment. Your dentist will determine the need for a bone graft during the pre-operative assessment using X-rays and CT scans.
What is Involved in Stage 3: Having the Implant Put In?
This is the pivotal moment in the implant journey: the surgical procedure of “having the implant put in.” While the thought of surgery can be daunting for some, it’s important to know that this is a highly refined, predictable, and typically well-tolerated procedure, especially when performed by an experienced clinician.
The process is usually carried out under local anesthesia, meaning the area being worked on will be completely numb, much like when you have a filling. You’ll be awake and aware, but you shouldn’t feel any pain. For patients who experience dental anxiety, various sedation options, such as oral sedatives or IV (intravenous) sedation, can be discussed with your dentist to ensure a more relaxed experience.
The actual surgical steps are quite precise. First, your dentist or surgeon will make a small incision in the gum tissue to expose the underlying jawbone in the predetermined location (guided by the detailed planning from Stage 1). Then, using a series of specialized, progressively wider drills, a precise channel, known as an osteotomy, is carefully prepared in the jawbone. This channel is meticulously sized to match the specific implant being used. The dentist takes great care during this drilling phase to avoid overheating the bone and to ensure the correct depth and angulation for optimal implant stability and prosthetic outcome.
Once the site is prepared, the dental implant post (the titanium screw) is gently and precisely screwed or tapped into place within the prepared bone. In some cases, a ‘healing cap’ or ‘healing abutment’ might be placed on top of the implant at this stage, which pokes slightly through the gum tissue and helps shape the gums for the future crown. In other cases, the implant might be completely covered by the gum tissue (a ‘two-stage’ approach), requiring a minor second procedure later to expose it.
After the implant is securely in position, the gum tissue is typically repositioned and sutured (stitched) closed. The final, crucial part of this stage isn’t surgical but biological: osseointegration. This is the remarkable natural process where your living jawbone cells grow onto and fuse directly with the biocompatible surface of the implant. This biological bonding is what gives dental implants their incredible strength and stability, effectively making the implant a part of your jaw. This healing and integration period typically takes anywhere from three to six months, or sometimes longer, depending on individual healing factors and bone quality.
What Does Stage 4: Restorative Treatment Entail After Dental Implantation?
Once the remarkable process of osseointegration has successfully run its course, and your dental implant has become firmly fused with your jawbone, it’s time for Stage 4: the restorative treatment. This is the exciting phase where the “dental implantation” process culminates in the placement of your new, visible, and functional tooth or teeth. This stage transforms the securely anchored implant post beneath your gums into a beautiful, natural-looking restoration.
The first step in this restorative phase usually involves exposing the top of the implant if it was covered by gum tissue during the healing period (a ‘two-stage’ procedure). This is a minor procedure, often done with local anaesthesia, where a small incision is made to access the implant. A healing abutment or cap may then be placed to help shape the gum tissue around the implant site, creating a natural emergence profile for the future crown.
After a short period allowing the gums to heal and contour around the healing abutment, the next step is to take impressions. These highly accurate moulds of your mouth, including the implant site and surrounding teeth, are crucial. They can be taken using traditional putty-like dental materials or with advanced digital intraoral scanners, which create a 3D virtual model. These impressions are sent to a dental laboratory where skilled technicians will meticulously craft your custom-made final restoration – whether it’s a single crown, a multi-unit bridge, or a component for an implant-supported denture.
The placement of the abutment is a key part of this stage. The abutment is a small connector piece that is screwed or cemented onto the top of the dental implant. It serves as the interface between the implant in your jawbone and the final crown that you will see.
Finally, once your custom restoration is ready, you’ll return to the dentist for it to be fitted. The custom-made crown, bridge, or denture is then securely attached to the abutment(s). Your dentist will check the fit, colour match, and your bite to ensure everything is perfect and comfortable. This stage is where the artistry of dentistry truly shines, as the goal is to create a replacement tooth that blends seamlessly with your natural teeth in shape, size, colour, and function. This final step completes the “dental implantation,” providing you with a durable, stable, and aesthetically pleasing solution that allows you to eat, speak, and smile with renewed confidence. Regular check-ups and good oral hygiene will then ensure your new implant serves you well for many years to come.
How Painful Are Dental Implants, or Getting a Single Tooth Implant?
One of the most prevalent anxieties surrounding any dental procedure, and especially one involving surgery, is the question of pain: “How painful are dental implants?” It’s a completely valid concern, and thankfully, the reality is often much less daunting than people imagine. The overwhelming majority of patients who undergo the dental implant procedure report that the discomfort experienced is surprisingly minimal and manageable. Many describe the sensation during the recovery period as being similar to, or even less intense than, that following a routine tooth extraction.
If you’re specifically wondering “how painful is getting one dental implant?” versus multiple, the immediate surgical experience under local anaesthesia should be pain-free regardless of the number. The post-operative discomfort for a single implant might logically be more localized and potentially resolve quicker than if multiple sites are healing, but individual pain tolerance and the complexity of the surgery (e.g., if bone grafting was also performed) are significant variables.
During the actual implant placement surgery, your dentist will use local anesthesia to completely numb the area being treated. This ensures that you will not feel any pain during the procedure itself. You might feel some pressure or vibrations, but not sharpness or pain. For patients who are particularly anxious, various sedation options, ranging from oral sedatives taken before the appointment to IV sedation administered by a trained professional, can be employed to help you relax and make the experience more comfortable.
Post-operatively, it’s normal to expect some level of discomfort, swelling, and possibly bruising once the anaesthesia wears off. This is a natural part of the body’s healing response. However, this discomfort is typically well-managed with recommendations for post-operative pain relief. Your dentist will likely advise you to take over-the-counter painkillers such as ibuprofen (which also helps with inflammation) or paracetamol. In some cases, prescription pain medication might be provided for a short period if deemed necessary. Applying ice packs to the outside of your face over the surgical area for the first 24-48 hours can also significantly help to reduce swelling and discomfort. Most patients find that any significant discomfort subsides within a few days to a week, with residual tenderness diminishing thereafter. Adhering closely to your dentist’s post-operative care instructions, including oral hygiene practices and dietary recommendations, is crucial for a smooth recovery and minimising pain.
What is the Typical Timeline for Dental Implant Surgery Recovery and Fitting?
Navigating the timeline for dental implant surgery, recovery, and the final fitting of your new tooth is a common point of curiosity and planning for patients. It’s important to understand from the outset that there isn’t a one-size-fits-all answer; the typical timeline can vary significantly from one individual to another. The entire process, from the initial consultation to walking away with your final, fully functional restoration, can span anywhere from a few months to over a year in more complex cases.
Several key factors influence this duration. One of the most significant is whether bone grafting is required. If your jawbone needs augmentation to create a stable foundation for the implant, this procedure will be performed first, and the site will need several months to heal and mature before the implant itself can be placed. Another major factor is your body’s own healing capabilities. General health, age (though less of a factor than overall health), smoking habits, and adherence to post-operative care instructions all play a role in how quickly you heal and how successfully the implant osseointegrates with your jawbone.
The number of implants being placed and the complexity of the overall treatment plan also contribute to the timeline. For instance, replacing a single tooth with an implant in an area with excellent bone quality might be on the shorter end of the spectrum, while a full mouth reconstruction with multiple implants and extensive grafting will naturally take longer. Your dentist will provide you with a personalized, estimated timeline during your initial consultation and planning phase, but it’s good to approach this with an understanding that biological processes can sometimes have their own pace.
The commitment to this timeline is an investment in a long-lasting, high-quality dental solution. Rushing critical healing phases, particularly osseointegration, can compromise the long-term success and stability of your new implant. Therefore, patience and adherence to the planned stages are key components of a successful outcome. The goal is not just speed, but a durable and aesthetically pleasing result that will serve you well for years, potentially even a lifetime, so allowing your body the time it needs to heal properly is paramount.
How Long Does it Take to Recover From Dental Implant Surgery?
When considering “how long does it take to recover from dental implant surgery?”, it’s helpful to think about recovery in a couple of distinct phases. First, there’s the initial recovery period immediately following the implant placement surgery. During this phase, which typically lasts from a few days to about a week or two, you can expect some common post-surgical effects. These may include mild to moderate discomfort, swelling in the gums and face around the surgical site, and possibly some bruising on the skin. The intensity and duration of these symptoms vary from person to person, often depending on the complexity of the surgery (e.g., number of implants, if bone grafting was done simultaneously). Most patients find that they can manage any discomfort effectively with over-the-counter pain relievers like ibuprofen or paracetamol, and by applying ice packs as recommended by their dentist. Many people feel well enough to return to work or their normal daily activities within a day or two, although it’s wise to avoid strenuous physical activity for a short period to allow your body to focus on healing.
Then, there’s the longer healing period, which is primarily about osseointegration. This is the crucial biological process where the dental implant fuses with your jawbone. This isn’t something you’ll actively ‘feel’ in terms of recovery symptoms like pain or swelling, but it’s a vital, silent healing phase happening beneath the surface. Osseointegration typically takes anywhere from 3 to 6 months, though it can sometimes be longer depending on factors like bone quality, your overall health, and the specific type of implant used. During this time, the implant is gradually becoming an integral part of your jaw, creating the incredibly strong foundation needed for the final crown.
To ensure a smoother recovery and promote successful osseointegration, your dentist will provide specific tips for recovery. These will include instructions on how to keep the surgical area clean (e.g., gentle rinsing with salt water or an antimicrobial mouthwash after a day or two), advice on eating soft foods initially to avoid putting pressure on the implant site, avoiding smoking (as it significantly impairs healing), and attending any scheduled follow-up appointments. Adhering strictly to these post-operative care guidelines is paramount for minimising complications and ensuring the implant heals properly, setting the stage for a successful long-term outcome.
How Long Do You Go Without Teeth When Getting Implants, and Are Temporary Teeth Provided?
A significant concern for many patients embarking on the dental implant journey is the aesthetic and functional impact of being without teeth, even temporarily: “How long do you go without teeth when getting implants?” This is particularly pertinent if the missing tooth or teeth are in a visible part of your smile. The good news is that in most cases, your dentist will ensure you don’t have to endure a noticeable gap for an extended period. Solutions are often available, and the question “do you get temporary teeth while waiting for implants?” can frequently be answered with a reassuring ‘yes’.
The type of temporary solution provided will depend on several factors, including the location of the missing tooth (front versus back), the number of teeth being replaced, your overall oral health, and the specific treatment plan. For instance, if you’re replacing a single front tooth, a temporary crown might be fabricated. This could be attached to adjacent teeth in a non-invasive way (like a Maryland bridge with wings bonded to the back of neighbouring teeth) or sometimes, if conditions allow for immediate loading, a temporary crown might even be placed directly onto the newly inserted implant (though this is not suitable for all cases and carries specific risks and benefits).
If multiple teeth are missing, a temporary partial denture (often called a ‘flipper’) or a temporary bridge might be options. These removable appliances can fill the gaps, restoring aesthetics and some function while the underlying implants are healing and integrating with the bone. For patients undergoing full arch replacement (all teeth in an upper or lower jaw), temporary full dentures are often provided.
In some specific clinical situations, particularly with advancements in implant technology and techniques, immediate implants (where the implant is placed on the same day as a tooth extraction) or immediate loading (where a temporary or sometimes even a final crown is attached to the implant shortly after its placement) might be possible. However, these approaches are not suitable for every patient and depend heavily on factors like bone quality and initial implant stability. Your dentist will thoroughly discuss the most appropriate temporary solution for your specific case during the treatment planning phase, ensuring your aesthetic and functional needs are addressed as comprehensively as possible throughout the healing journey. The goal is to make the transition as smooth and comfortable as possible, minimizing any social or personal discomfort associated with missing teeth.
How Long Does it Usually Take to Fit One Dental Implant?
When patients ask, “How long does it usually take to fit one dental implant?”, it’s important to clarify that this question typically refers to the duration of the actual surgical procedure for placing a single implant post into the jawbone, not the entire treatment journey from start to finish. The surgical placement of one dental implant is generally a surprisingly efficient procedure. For a straightforward case, where there’s adequate bone and no complex anatomical considerations, the surgery to place a single implant often takes approximately 1 to 2 hours.
This timeframe includes the administration of local anaesthesia, the preparation of the surgical site (making the incision and drilling the osteotomy – the channel in the bone), the precise insertion of the implant post, and the suturing (stitching) of the gum tissue. Of course, this is an estimate, and the exact duration can vary. Factors that might influence this include the specific location of the implant in the mouth (e.g., front versus back, upper versus lower jaw), the quality and quantity of the patient’s jawbone, and the experience of the surgeon. If any additional minor procedures are performed concurrently, such as a very small bone graft or gum contouring, this could add a little more time.
It’s crucial to differentiate this surgical appointment duration from the overall treatment timeline. As discussed earlier, the entire process for a dental implant involves much more than just the fitting surgery. There’s the initial consultation and planning phase, potentially a separate bone grafting procedure with its own healing time if needed (which can add several months), the critical osseointegration period after the implant is placed (typically 3-6 months where the bone fuses to the implant), and then the subsequent restorative phase where the abutment and final crown are made and fitted (which can take a few weeks and involve a couple of appointments). So, while the act of “fitting” or surgically placing the implant itself is relatively quick, the journey to your final, functional tooth is a more extended, multi-stage process. Your dentist will always allocate sufficient time for the surgical appointment to ensure it’s performed meticulously and without rushing, prioritising precision and your comfort.
How Soon After a Tooth Extraction Can an Implant Be Done?
The timing of dental implant placement following a tooth extraction is a common question, and the answer “how soon after a tooth extraction can an implant be done?” depends on various clinical factors and the specific approach chosen by your dentist. There isn’t a single ‘best’ time for everyone; rather, there are several well-established protocols, each with its own indications and advantages.
One option is immediate implant placement. In this scenario, the dental implant is placed into the socket at the very same appointment that the natural tooth is extracted. This approach can be advantageous as it can reduce the overall treatment time and potentially help preserve more of the surrounding bone and gum tissue architecture. However, immediate placement is not suitable for all cases. It requires that the extraction site be free of acute infection and that there is sufficient bone available in the socket to provide initial stability for the implant.
Another common approach is early implant placement. This typically occurs a few weeks to a few months (often 2-3 months) after the tooth extraction. This delay allows for initial healing of the soft tissues (gums) and some bone fill in the socket, which can create a more favorable environment for implant placement, especially if there was some infection or minor bone loss around the extracted tooth. The gum tissue healing makes the surgical site easier to manage.
The third option is delayed implant placement (also known as late placement). This involves waiting for more complete healing of the extraction socket, which usually means waiting 4-6 months or even longer after the tooth is removed. This approach is often chosen when there has been significant bone loss due to infection, trauma, or a difficult extraction, or if a substantial bone grafting procedure is needed to rebuild the site before an implant can be safely and successfully placed.
The factors determining the best timing include the reason for the tooth extraction (e.g., decay, trauma, infection), the presence and severity of any infection, the amount and quality of bone remaining in the socket and surrounding area, the patient’s overall oral health, and aesthetic considerations (especially for front teeth). Your dentist will carefully evaluate your specific situation, often using X-rays or 3D CBCT scans, to determine the most appropriate and predictable timing for your implant placement to maximize the chances of long-term success.
What Should You Know About Sedation and Diet After Your Dental Implant Treatment?
Undergoing dental implant treatment is a significant step towards restoring your smile and oral function. Beyond the technical aspects of the surgery itself, there are practical considerations that can greatly impact your comfort and the success of your recovery. Two common areas of inquiry for patients are the availability of sedation during the procedure and the necessary dietary adjustments afterwards. Understanding these aspects can help alleviate anxiety and ensure you’re well-prepared for both the implant placement and the crucial healing phase that follows.
“Do they put you to sleep for dental implants?” is a frequent question stemming from understandable apprehension about dental surgery. The answer involves exploring various sedation options tailored to patient comfort and the complexity of the procedure. Equally important is knowing “what foods should you not eat after dental implants?” because your diet plays a direct role in protecting the surgical site, minimizing irritation, and promoting optimal healing. Adhering to dietary guidelines, especially in the initial days and weeks post-surgery, is a key component of successful aftercare. Information like that found in leaflets titled “After Your Dental Implant Treatment in Southampton” (or similar advice from your specific clinic) will provide tailored guidance.
Being well-informed about these practicalities contributes significantly to a smoother, more comfortable experience and a better overall outcome. Let’s delve deeper into the specifics of sedation options and post-operative dietary recommendations. This knowledge empowers you to have informed discussions with your dental team and to take an active role in your recovery process, ensuring that every measure is taken to support the integration and longevity of your new dental implant. These aren’t minor details; they are integral parts of a comprehensive care approach designed around your well-being.
Do They Put You to Sleep for Dental Implants? Exploring Sedation Options
The question, “Do they put you to sleep for dental implants?” is a very common one, reflecting a natural concern about comfort and anxiety during a surgical procedure. While general anesthesia (where you are completely “put to sleep” and unconscious) is an option, it is less common for routine, straightforward dental implant procedures. General anaesthesia is typically reserved for more complex or extensive surgical cases, such as full mouth reconstructions, patients with certain medical conditions, or individuals with extreme dental phobia that cannot be managed by other means. It requires an anaesthesiologist and specialized monitoring equipment.
However, the vast majority of dental implant placements are comfortably and successfully performed using other highly effective sedation methods. The standard and most common approach is local anesthesia. This involves injecting an anaesthetic medication directly into the area where the implant will be placed, which completely numbs the site. You remain fully awake and aware, but you will not feel any pain during the surgery – perhaps just some pressure or vibration.
For patients who experience mild to moderate anxiety, oral sedation is a popular choice. This involves taking a prescribed sedative pill (like Valium or Halcion) about an hour before the appointment. By the time the procedure begins, you will feel significantly more relaxed and calm, although you will still be conscious and able to respond to your dentist.
Another widely used and very effective option is IV sedation (Intravenous Sedation), sometimes referred to as “twilight sleep” or “conscious sedation.” With IV sedation, sedative medications are administered directly into your bloodstream through a vein. This allows for a deeper level of relaxation than oral sedation, and you may have little to no memory of the procedure afterwards. You remain conscious enough to respond to verbal cues but are in a profoundly relaxed state. IV sedation requires specialized training and monitoring by the dental team.
The best option for you will depend on your level of anxiety, the complexity of your implant procedure, your medical history, and your personal preferences. It’s crucial to have an open discussion with your dentist about your concerns. They can explain the benefits and considerations of each available sedation method and help you choose the one that will make your experience as comfortable and stress-free as possible. The primary goal is to ensure your safety and comfort throughout the entire process.
What Foods Should You Not Eat After Dental Implants for Optimal Healing?
Following your dental implant surgery, your diet plays a surprisingly crucial role in ensuring optimal healing and the long-term success of your new implant. Knowing “what foods should you not eat after dental implants” is just as important as knowing what you can eat. The primary goal during the initial healing phase is to protect the surgical site, prevent irritation or infection, and allow the implant to integrate undisturbed. Your dentist or oral surgeon will provide specific post-operative dietary guidelines, similar to advice you might find in a patient leaflet like “After Your Dental Implant Treatment in Southampton,” tailored to your procedure.
Generally, for the first few days to a week (or longer, depending on your dentist’s advice), you’ll want to stick to a soft food diet. Think smooth soups (not too hot!), yogurts, scrambled eggs, mashed potatoes, smoothies (but avoid using straws, as the suction can dislodge blood clots), applesauce, oatmeal, and well-cooked, soft pasta.
As for foods to avoid, the list typically includes anything that is hard, crunchy, sticky, spicy, or very hot. Hard foods like nuts, hard candies, popcorn (especially the kernels that can get stuck), and raw crunchy vegetables (like carrots or celery) can put undue pressure on the implant site or even damage the healing tissues. Sticky foods, such as caramels, taffy, or very chewy breads, can pull at the surgical site or sutures. Spicy foods can irritate the sensitive healing gums, causing discomfort and inflammation. Very hot foods and beverages can also increase blood flow to the area and potentially cause bleeding or discomfort.
It’s also wise to avoid small, seedy foods (like sesame seeds or poppy seeds) that can get lodged in the surgical site and be difficult to remove, potentially leading to irritation or infection. Chewing directly on the implant site should be avoided until your dentist gives you the go-ahead. The importance of diet in preventing irritation and promoting healing cannot be overstated. A gentle diet allows the gum tissues to heal properly and protects the underlying implant as it undergoes osseointegration. Gradually, as healing progresses and with your dentist’s approval, you can start reintroducing more textured foods back into your diet. Always follow your specific clinician’s advice, as they will provide the most relevant guidance for your individual case.
What Are the Potential Downsides, Long-Term Side Effects, and Risks of Dental Implants?
While dental implants boast impressively high success rates – often exceeding 95% – and offer a transformative solution for tooth loss, it’s crucial for any prospective patient to have a balanced understanding of the treatment. This means acknowledging that, like any surgical procedure, there are potential downsides, long-term side effects, and risks associated with dental implants. Being well-informed about these possibilities allows you to make a truly educated decision in consultation with your dental professional and helps set realistic expectations. It’s not about fear-mongering, but about comprehensive patient education.
Most complications are rare and often preventable or manageable with proper planning, skilled execution, and diligent post-operative care. However, understanding what could happen is a vital part of the consent process. We will explore common questions such as “What is the downside to dental implants?” and “What are the disadvantages of the implant?”. We’ll also delve into the incidence of issues by asking “How common are problems with dental implants?” and address concerns about the body’s reaction, like “Will my body reject dental implants?” or even “Can your body reject dental implants years later, including metal implants?”. Furthermore, it’s important to know who might not be an ideal candidate (“Who should not get dental implants?”) and if age plays a limiting role (“At what age might they be inadvisable?”).
A transparent discussion of these factors ensures that you embark on the implant journey with your eyes wide open, fully aware of both the remarkable benefits and the less common, but possible, challenges. This comprehensive awareness empowers you to ask pertinent questions and collaborate effectively with your dental team to mitigate risks and optimise your outcome. The aim is always to achieve a successful, long-lasting restoration, and understanding potential hurdles is the first step in navigating them effectively.
What is the Downside to Dental Implants and What Are the Disadvantages of the Implant?
While the benefits of dental implants are significant and well-documented, it’s equally important to consider “what is the downside to dental implants” and understand the potential “disadvantages of the implant” before committing to the procedure. One of the primary considerations for many is the cost. Dental implant treatment is generally more expensive upfront compared to other tooth replacement options like traditional dentures or bridges. This investment, however, is often justified by their longevity and the superior function and aesthetics they provide, potentially saving costs on replacements or repairs of less durable options down the line.
Another factor is the length of treatment. The entire process, from initial consultation to final restoration, can take several months, and sometimes up to a year or more if procedures like bone grafting are required. This requires patience and commitment from the patient.
The surgical nature of the procedure is another aspect to consider. While generally safe and performed under local anaesthesia or sedation, any surgery carries inherent risks, such as infection, bleeding, or an adverse reaction to anaesthesia, though these are typically rare and manageable. There’s also a period of healing and potential discomfort post-surgery.
Furthermore, the need for good oral hygiene is paramount for the long-term success of dental implants. Just like natural teeth, implants require regular brushing, flossing, and routine dental check-ups to prevent complications like peri-implantitis (inflammation and infection around the implant). Neglecting oral hygiene can lead to implant failure.
Some specific disadvantages can include the potential for surgical complications, though rare, such as nerve damage (which can cause numbness or tingling in the lip, chin, or tongue), sinus perforation (if an upper implant encroaches on the sinus cavity), or damage to adjacent teeth if not planned meticulously. Another point is that not everyone is a candidate for dental implants. Sufficient bone density and volume are required to support the implant, and while bone grafting can often address deficiencies, it adds complexity and time to the treatment. Certain medical conditions (like uncontrolled diabetes or severe osteoporosis) or lifestyle factors (heavy smoking) can also increase the risk of complications or failure. While the success rates are very high, implant failure, though uncommon, can occur, necessitating removal of the implant and potentially further treatment. Understanding these downsides allows for a fully informed decision-making process.
How Common Are Problems with Dental Implants, and Will My Body Reject Them?
It’s natural to wonder, “How common are problems with dental implants?” and to harbor concerns like, “Will my body reject dental implants?” Thankfully, the news on this front is largely positive. Dental implants have one of the highest success rates of any implanted medical device, typically reported to be above 95%, and often even higher (97-98%) over a 5 to 10-year period when placed by experienced clinicians and properly maintained by the patient. This means that outright “problems with dental implants” leading to failure are not common.
However, like any medical or surgical procedure, complications can occur, though they are generally infrequent and often manageable. Some potential problems include infection at the implant site (peri-implantitis), which is similar to gum disease around natural teeth and is often linked to poor oral hygiene or smoking. Nerve damage, resulting in tingling or numbness in the lip, chin, or tongue, is a rare complication that can occur if an implant is placed too close to a nerve; meticulous planning with 3D imaging helps to minimise this risk. Implant failure can manifest as the implant becoming loose or failing to integrate with the bone (osseointegration failure). This can be due to factors like insufficient bone quality, smoking, uncontrolled systemic diseases, or premature overloading of the implant.
Regarding the question, “will my body reject dental implants?”, it’s important to clarify what “rejection” means in this context. True immunological rejection, like that seen with organ transplants where the body’s immune system attacks the foreign tissue, is extremely rare with dental implants. This is because materials like titanium (and zirconia) are highly biocompatible, meaning the body generally accepts them without an adverse immune response. Instead of rejection, what can occur is a failure to osseointegrate. This means the bone doesn’t fuse properly with the implant surface. This isn’t the body “rejecting” the implant in an allergic sense, but rather a failure of the biological bonding process. This can be influenced by local factors (infection, poor bone quality, surgical technique) or systemic factors (certain medical conditions, smoking). If an implant fails to integrate or becomes problematic, it may need to be removed. Often, after a healing period, another attempt at implant placement can be made, frequently with a high chance of success.
Can Your Body Reject Dental Implants Years Later, Including Metal Implants?
The question, “Can your body reject dental implants years later, including metal implants?” touches upon the concern of long-term stability and potential late-onset complications. While the initial success rates of dental implants are very high, and true immunological “rejection” of biocompatible materials like titanium (the most common “metal implant”) is exceedingly rare at any stage, late-term implant failure or complications can indeed occur years after successful placement and integration. However, it’s more accurate to describe these as “failures” or “complications” rather than the body suddenly “rejecting” a previously integrated implant in an allergic sense.
One of the primary causes of late-term implant problems is peri-implantitis. This is an inflammatory condition affecting the soft and hard tissues surrounding an implant, similar to periodontitis (gum disease) around natural teeth. It’s often caused by bacterial infection, usually linked to suboptimal oral hygiene, smoking, or sometimes a poorly fitting restoration that creates plaque traps. If left untreated, peri-implantitis can lead to progressive bone loss around the implant and eventually cause it to become loose and fail.
Another potential issue years later is mechanical failure. While implants and their components are designed to be very strong, excessive biting forces (like from teeth grinding or clenching, known as bruxism), trauma, or component fatigue over many years can potentially lead to the fracture of the implant itself, the abutment, or the overlying crown.
Systemic health changes can also impact implants “years later.” The development or poor management of certain chronic diseases, such as diabetes or osteoporosis, or undergoing treatments like radiation therapy to the head and neck, can affect bone metabolism and healing, potentially compromising the long-term stability of an implant.
Regarding “metal implants” (titanium), as mentioned, true allergic rejection is exceptionally uncommon. However, if a patient were to develop a very rare allergy to titanium or an alloy component (which is often commercially pure titanium but can have trace other elements), it could theoretically cause issues. More commonly, late problems are related to the biological environment (peri-implantitis) or mechanical factors rather than a material rejection. Regular dental check-ups and meticulous oral hygiene are crucial for monitoring the health of dental implants long-term and catching any potential issues early, significantly improving the chances of sustained success for many years, even decades.
Who Should Not Get Dental Implants, and At What Age Might They Be Inadvisable?
While dental implants are a versatile and highly successful solution for many, they are not suitable for everyone. There are certain conditions and factors that can increase the risk of complications or implant failure, leading to the question, “Who should not get dental implants?” It’s not always a strict ‘no,’ but rather a case of carefully weighing the risks and benefits, and sometimes needing to address underlying issues first.
Key contraindications or factors increasing risk include uncontrolled chronic diseases. For example, individuals with poorly controlled diabetes may experience impaired healing and a higher risk of infection, which can compromise osseointegration. Severe osteoporosis, especially if treated with certain bisphosphonate medications (particularly IV forms), can affect bone healing and quality, potentially increasing the risk of complications like osteonecrosis of the jaw, though this is more nuanced and requires careful assessment. Patients undergoing active cancer treatment, such as chemotherapy or radiation therapy to the head and neck region, may need to delay implant procedures until their treatment is complete and their oncologist approves.
Heavy smoking is a significant risk factor, as it constricts blood vessels, impairs healing, and increases the likelihood of infection and implant failure. While not an absolute contraindication, smokers are often advised to quit or significantly reduce smoking before and after implant surgery.
Certain medications, beyond bisphosphonates, such as long-term immunosuppressants, can also impact healing. A crucial factor is insufficient bone that cannot be adequately grafted. While bone grafting can solve many deficiencies, some cases may be too severe or the patient may not be a candidate for extensive grafting.
Regarding age, the question “At what age might they be inadvisable?” usually pertains to both ends of the age spectrum. For younger individuals, dental implants are generally not recommended for individuals whose jawbones haven’t fully developed. This typically means waiting until the late teens for girls and a bit later for boys (early twenties). Placing an implant in a still-growing jaw can lead to aesthetic and functional problems as the jaw continues to change around the static implant.
For older adults, chronological age (“at what age should you not get implants?”) is far less of a determining factor than their overall health and bone quality. Healthy older adults can be excellent candidates for dental implants and can benefit greatly from the improved quality of life they offer. The key considerations are their medical status, ability to undergo the surgical procedure, and capacity to maintain good oral hygiene. Each case is assessed individually, with a thorough medical history and dental examination being paramount.
How Long Do Dental Implants Last and Are Dental Implants Worth the Money?
Two of the most pivotal questions on any prospective implant patient’s mind are undoubtedly: “How long do dental implants last?” and “Are dental implants worth the money?” These questions strike at the heart of the value proposition of this advanced dental treatment. Understanding the longevity and the overall cost-benefit analysis is crucial when making such a significant investment in your oral health and quality of life.
Dental implants are renowned for their durability, designed to be a long-term, if not permanent, solution for tooth loss. Unlike other dental prosthetics that may require more frequent replacement or adjustment, implants have the potential to serve you reliably for many, many years. When exploring their worth, it’s not just about the initial financial outlay; it’s about weighing that against the profound improvements in functionality – the ability to eat what you love, speak with clarity – and the boost in aesthetics and self-confidence that a secure, natural-looking smile can bring.
Furthermore, when comparing costs, one must consider the potential long-term expenses associated with alternative, less durable tooth replacement options, which might involve repeated treatments, repairs, or replacements over time, potentially equalling or even exceeding the cost of implants in the long run. The intrinsic value of preserving jawbone health, a unique benefit of implants, also contributes significantly to their worth, preventing the sunken facial appearance that can accompany long-term tooth loss and traditional denture wear. Let’s delve deeper into the specifics of implant longevity and the multifaceted factors that contribute to whether they are indeed “worth the money” for you as an individual, considering both the tangible and intangible benefits. This involves looking beyond the price tag to the comprehensive impact on your daily life and long-term well-being.
What is the Cost of Dental Implants in the UK, and Can the NHS Pay for My Dental Implants?
The financial aspect of dental implant treatment is, understandably, a major consideration for patients in the United Kingdom. Questions like “What is the cost of dental implants in the UK?” and “Can the NHS pay for my dental implants?” are frequently asked and are crucial for planning and decision-making. Dental implants are a significant investment, and the cost can vary widely based on a multitude of factors. It’s important to approach this with an understanding that pricing is not standardized across the board.
The availability of implants on the National Health Service (NHS) is another key area of concern, as NHS dental provision has specific criteria and limitations, especially for more advanced and often cosmetically driven treatments like dental implants. Most implant treatments are carried out in the private dental sector, where costs are determined by the individual clinic and the complexity of the case.
Understanding the typical price ranges, what influences these costs, and the realities of NHS funding will help you navigate your options more effectively. We will explore the general costs you might encounter for single implants or even a “full set of fake teeth” (implant-supported dentures/bridges) in the UK, citing some example pricing structures where available (like “single implant placement from £945” or “fully restored from £1,595” as indicative starting points). We’ll also clarify the typical NHS stance on funding implant treatment, explaining the specific, often restrictive, clinical circumstances under which they might be available. Furthermore, we’ll touch upon whether “affordable dental implants” are a realistic option, perhaps looking at examples like those in “Southampton,” and what factors might contribute to more accessible pricing, while also cautioning against compromising on quality or expertise solely for cost. This financial transparency is key to making an informed choice that aligns with both your dental needs and your budget.
What is the Cost of Dental Implants in the Albania?
What is the Cost of Dental Implants in Albania?
Albania offers some of the most competitive prices for dental implants in Europe, making it a top destination for dental tourism. While prices can vary based on the clinic, implant brand, and whether additional procedures (like bone grafts) are needed, here’s a detailed breakdown of average costs in 2025:
Average Prices for Dental Implants in Albania
| Treatment Type | Average Price (EUR) | Details |
|---|---|---|
| Single Dental Implant (Titanium) | €400 – €700 | Implant post only (surgical placement) |
| Zirconia Dental Implant | €600 – €900 | Metal-free, more aesthetic and biocompatible |
| Abutment + Crown (Zirconia) | €250 – €400 | Added after healing (3–6 months) |
| Complete Single-Tooth Implant | €650 – €1,100 | Includes implant, abutment, and zirconia crown |
| All-on-4 (Full Arch) | €2,800 – €4,500 | Fixed full-arch bridge supported by 4 implants |
| All-on-6 or All-on-8 | €3,500 – €6,500+ | More implants for stability and long-term durability |
| Bone Grafting (if needed) | €150 – €400 | Required when bone volume is insufficient |
| Sinus Lift (if needed) | €300 – €700 | Common for upper jaw bone elevation |
| Temporary Denture (provisional) | €100 – €250 | Optional during healing phase |
✈️ Dental Tourism Bonus: What’s Often Included
Many Albanian clinics provide value-added packages that make dental travel easy:
✅ Free consultation and panoramic X-ray
✅ Airport transfer and accommodation support
✅ Multilingual staff (English, Italian, German)
✅ 5–10 year guarantees on implants and crowns
✅ Express treatment options (3–7 days for immediate load cases)
Cost Comparison: Albania vs. UK/Italy
| Treatment | Albania (EUR) | UK (EUR) | Italy (EUR) |
|---|---|---|---|
| Single Tooth Implant | €650 – €1,100 | €2,000 – €3,500 | €1,500 – €2,800 |
| All-on-4 | €2,800 – €4,500 | €12,000 – €18,000 | €7,000 – €12,000 |
| All-on-6 | €3,500 – €6,500 | €15,000 – €25,000 | €9,000 – €15,000 |
Factors That Influence the Final Price
Implant brand (Straumann, Megagen, Neodent, etc.)
Type of crown (zirconia vs. porcelain-fused-to-metal)
Skill of the surgeon and clinic reputation
Need for bone grafts or sinus lifts
Accommodation and travel costs
✅ Summary
| Feature | Benefit |
|---|---|
| Cost Savings | Up to 70% cheaper than Western Europe |
| High-Quality Clinics | Modern technology, certified implants, expert dentists |
| ✈️ Tourism Option | Combine dental care with vacation |
| Flexible Scheduling | Fast appointments and short wait times |
How Much Are Dental Implants in the UK, Including a Full Set of Fake Teeth?
Determining “how much are dental implants in the UK” requires understanding that there isn’t a single fixed price. The cost is highly variable and depends on numerous factors. For a single dental implant, which includes the implant post, the abutment, and the final crown, patients in the UK can generally expect prices to range anywhere from £1,800 to £3,500 or even more. Some clinics might advertise a lower starting price for “single implant placement from £945,” but it’s crucial to clarify if this includes just the surgical placement of the implant post itself, or if the abutment and final crown are additional costs, leading to a “fully restored from £1,595” or higher figure.
The cost for a “full set of fake teeth” supported by dental implants (such as an implant-supported bridge or an implant-retained denture for a full arch) will, naturally, be significantly higher. For a full arch replacement (e.g., “All-on-4” or “All-on-6” systems), prices can range dramatically, often from £10,000 to £25,000 per arch, and sometimes even more, depending on the specifics.
Several factors influence these costs: the geographical location of the dental clinic (prices in major cities like London may be higher than in other areas); the experience and qualifications of the dentist or specialist performing the procedure; the type and brand of implant system used (premium brands may cost more); the material of the final crown or bridge (e.g., porcelain-fused-to-metal, all-ceramic, zirconia); whether any preparatory procedures are needed, such as tooth extractions, bone grafting, or sinus lifts (these will add to the overall cost); and the complexity of the individual case. The use of advanced technology, like 3D CBCT scanning for diagnosis and planning, or computer-guided surgery, can also influence the price but often contributes to more predictable outcomes.
It’s absolutely essential to obtain a personalized quote from your chosen dental clinic after a thorough consultation and examination. This quote should clearly itemize all aspects of the treatment, including consultations, imaging, surgery, implant components, temporary restorations (if any), the final prosthesis, and any follow-up care, so you have a comprehensive understanding of the total investment involved. Many clinics also offer payment plans or dental finance options to help make the treatment more manageable.
Are Dental Implants Now Available on the NHS?
The question, “Are dental implants now available on the NHS?” is a common one, and the answer is nuanced but generally leans towards limited availability for most routine cases. The typical NHS stance is that dental implants are usually only available on the NHS in very specific and often complex clinical circumstances. They are not routinely provided for the replacement of missing teeth where other, less expensive options (like dentures or conventional bridges) could be considered adequate from an NHS perspective, which primarily focuses on essential dental health rather than optimal or cosmetic solutions.
The criteria for NHS-funded implant treatment are quite strict and often include situations such as: patients who have lost teeth due to significant trauma (e.g., a serious accident); individuals who are congenitally missing multiple teeth (hypodontia) where implants are deemed the most appropriate solution for function and development; or patients who have undergone radical surgery for oral cancer leading to tooth and jawbone loss, where implants can play a crucial role in rehabilitation.
Even in these specific circumstances, funding is not guaranteed and often requires application to and approval from local NHS commissioning bodies, which can be a lengthy process with no certainty of a positive outcome. Therefore, routine cosmetic or elective implant treatment – for example, replacing a single missing molar for improved chewing comfort or enhancing the appearance of a smile – is generally not covered by the NHS. So, when patients ask, “Can NHS pay for my dental implants?”, the answer for the vast majority of cases seeking implants for common tooth loss scenarios will unfortunately be ‘no’. Most dental implant procedures in the UK are carried out on a private basis. If you believe you might meet the strict NHS criteria, the first step would be to discuss your situation with your NHS dentist, who can advise on your eligibility and the potential referral process. However, for most individuals considering implants, exploring private treatment options and their associated costs will be the more realistic pathway.
Are Affordable Dental Implants an Option, for Example in Southampton?
The quest for “affordable dental implants” is understandable, given that the treatment can represent a significant financial commitment. While “affordable” is a relative term, it is possible to find clinics that offer competitive pricing, and patients often wonder if certain locations, perhaps like “Southampton” (as an example of a city outside of a major capital), might offer more accessible options. Indeed, factors such as clinic overheads, local market competition, and the specific business models of dental practices can lead to variations in pricing across different regions and even within the same city.
To find “affordable dental implants,” patients can explore several avenues. One approach is to research and compare clinics, looking for those that might have more competitive pricing structures. Some practices, such as one hypothetically advertising “Affordable Dental Implants In Southampton | Low Dental Prices,” might position themselves as offering value. However, it’s crucial to look beyond just the headline price. Ensure you understand exactly what is included in any quoted fee (e.g., are consultations, X-rays, the implant, abutment, crown, and follow-up appointments all covered?).
Many dental practices offer payment plans or dental finance options, which can make the cost more manageable by spreading it over several months or years. This doesn’t reduce the total cost but can make it more accessible from a cash flow perspective. Sometimes, considering different material options for the final crown, if clinically appropriate and discussed with your dentist, might slightly influence the cost, though the core implant components are usually fairly standard.
Some patients also explore options like treatment at dental university hospitals where procedures might be performed by postgraduate students under strict supervision, often at a reduced cost, though waiting lists can be long. However, a critical caution must be sounded: do not choose a dental implant provider solely on price. While affordability is important, the quality of the materials used, the skill and experience of the dental surgeon, the thoroughness of the diagnostic and planning process, and the standards of sterilization and aftercare are paramount for the long-term success and safety of your implant. Opting for a significantly cheaper option without due diligence could lead to complications, implant failure, and ultimately higher costs in the long run to rectify problems. Always prioritise expertise, reputation, and a comprehensive treatment plan when making your decision.
What is the Best Alternative to Dental Implants for Fixing Missing Teeth?
While dental implants are often lauded as the gold-standard solution for tooth replacement, they may not be the ideal choice for everyone due to factors like cost, surgical aversion, medical contraindications, or simply personal preference. This leads to the important question: “What is the best alternative to dental implants for fixing missing teeth?” Fortunately, modern dentistry offers several viable options for “how to fix missing teeth without implants,” each with its own set of advantages, disadvantages, and suitability for different clinical scenarios.
The “best” alternative is subjective and depends heavily on individual needs, the number and location of missing teeth, the condition of remaining teeth and gums, budget, and lifestyle considerations. Traditional dental bridges are a common fixed alternative. These involve creating a false tooth (or teeth) that is anchored to the natural teeth on either side of the gap. This often requires the adjacent teeth (abutment teeth) to be crowned, meaning some of their natural tooth structure needs to be removed.
Another widely used option, especially for multiple missing teeth or when adjacent teeth are not suitable for supporting a bridge, is a removable partial denture. These consist of replacement teeth attached to a gum-colored plastic base, sometimes with a metal framework for support, which clips onto existing natural teeth. For those missing all teeth in an arch, a complete removable denture is a long-standing solution. Understanding why someone might opt not to replace teeth with implants (“Why not replace teeth with implants?”) often comes down to these factors. Exploring these alternatives with your dentist will help you make an informed decision that aligns with your specific circumstances and goals for your oral health and smile. Each alternative comes with different implications for oral hygiene, longevity, comfort, and impact on surrounding teeth, all of which should be carefully discussed.
Why Might One Opt Not to Replace Teeth with Implants?
The decision of “why not replace teeth with implants?” is a personal one, influenced by a variety of valid considerations, even when implants are presented as a highly effective solution. Understanding these reasons is key to appreciating why alternative tooth replacement methods remain relevant and widely used.
One of the most significant factors is often cost. Dental implant treatment typically involves a higher upfront financial investment compared to options like traditional bridges or removable dentures. For some individuals, this initial expense can be a prohibitive barrier, leading them to seek more budget-friendly, albeit potentially less permanent, solutions.
Another common reason is an aversion to surgical procedures. The placement of dental implants is a surgical intervention, and while generally safe and minimally invasive for many, some people are naturally apprehensive about undergoing any form of surgery, no matter how routine. Concerns about pain, recovery time, or potential surgical complications can lead them to prefer non-surgical alternatives if available.
Medical contraindications also play a role. As discussed earlier, certain uncontrolled systemic diseases (e.g., severe diabetes, significant immunosuppression), ongoing treatments like radiation to the jaw, or specific medications can increase the risks associated with implant surgery or impair healing, making implants a less suitable or even inadvisable option for some patients.
The length of the treatment process for dental implants, which can span several months from start to finish, especially if bone grafting is needed, might also deter individuals who are looking for a quicker resolution to their missing teeth. In contrast, procedures for bridges or dentures can often be completed in a shorter timeframe.
Personal preference and lifestyle factors can also contribute. Some individuals may simply prefer a less invasive option or may have had positive experiences with dentures or bridges in the past. Additionally, if the remaining natural teeth are already compromised and may require crowns anyway, incorporating them into a bridge might seem like a more efficient approach to some. Finally, if there’s insufficient bone volume and the patient is unwilling or unable (due to medical or financial reasons) to undergo bone grafting procedures, implants may not be feasible. These are all legitimate reasons why someone might choose an alternative path for their tooth replacement needs.
Is a Bridge or Implant Better for Tooth Replacement?
When faced with a missing tooth, one of the most common dilemmas patients and dentists navigate is: “Is a bridge or implant better?” This question, often phrased as “Which is better, implant or bridge?”, doesn’t have a universal, one-size-fits-all answer. Both dental implants and traditional fixed bridges are excellent, well-established methods for tooth replacement, but they operate on different principles and come with distinct sets of pros and cons.
The “better” choice truly depends on a careful evaluation of the individual patient’s specific clinical situation, their oral health status, the condition of the teeth adjacent to the gap, bone density, aesthetic goals, long-term expectations, lifestyle, and budget. A dental implant is a standalone solution that replaces the tooth root and crown without impacting adjacent teeth. It involves surgically placing a titanium post into the jawbone, which then integrates with the bone to provide a strong foundation for a crown.
A traditional dental bridge, on the other hand, literally “bridges” the gap by suspending a false tooth (pontic) between two crowns that are placed on the natural teeth on either side of the space (abutment teeth). This requires preparation (grinding down) of these adjacent teeth, even if they are perfectly healthy. Understanding the fundamental differences in how they function, their impact on surrounding structures, their longevity, maintenance requirements, and overall costs is key to making an informed decision in consultation with your dentist. We will explore these aspects to help illuminate why one might be favoured over the other in different circumstances.
What is Considered the Best Age for Dental Implants?
The question “What is considered the best age for dental implants?” is one that frequently arises, particularly from parents of adolescents with missing teeth or from older adults wondering if they’ve “missed the boat.” The good news is that suitability for dental implants is determined far more by an individual’s jawbone development and overall health than by their chronological age. There isn’t a specific “best age” in terms of a number, but rather an optimal set of physiological conditions.
For younger individuals, the primary consideration is ensuring that jaw growth is complete. Placing an implant in a jaw that is still growing can lead to aesthetic and functional problems down the line, as the natural teeth will continue to erupt and shift with growth, while the implant remains fixed in its original position. This can result in the implant appearing submerged or misaligned over time. Therefore, dentists typically wait until the late teens for girls (around 17-18) and a bit later for boys (around 19-21), or until skeletal maturity is confirmed, before considering implant placement.
On the other end of the spectrum, there is generally no upper age limit for dental implants. Healthy older adults can be excellent candidates and can significantly benefit from the improved chewing ability, nutritional intake, and quality of life that implants provide. As long as an older individual is in good general health, has adequate bone density (or is a candidate for bone grafting), and is capable of maintaining good oral hygiene, they can successfully receive and maintain dental implants. The focus for older patients is on their physiological age (health status) rather than their chronological age. Factors like uncontrolled systemic diseases (e.g., unmanaged diabetes, severe osteoporosis treated with certain medications), a history of radiation therapy to the jaws, or heavy smoking can be more significant contraindications than age itself. Thus, a thorough medical and dental evaluation is crucial for patients of all ages to determine their suitability for this transformative treatment.
How Can You Fix Your Teeth if You Don’t Have Money, Especially in the UK?
Addressing dental problems, especially significant ones requiring tooth replacement, can be a major financial concern, leading many to ask, “How can I fix my teeth if I don’t have money, especially in the UK?” The reality is that accessing comprehensive dental care without sufficient funds can be challenging, but there are avenues to explore and strategies that might help, particularly within the UK’s healthcare landscape which includes the National Health Service (NHS) alongside private options. It’s important to manage expectations, as “free” extensive dental work is rare, but understanding the system can reveal potential support.
For those on low incomes, the first port of call is often to understand NHS entitlements. While complex treatments like implants are usually not covered for cosmetic reasons, essential dental care to relieve pain, treat infection, and maintain basic oral function is a priority. We will explore questions like “Do over 60s get free dental treatment that could cover tooth replacement?” to clarify specific age-related entitlements (which are often more about exemption from standard NHS charges rather than automatic access to all treatments). We’ll also address dire situations: “What are the options if your teeth are rotting and you can’t afford to fix it in the UK?” and the broader, challenging query: “Can you get teeth replaced for free or fix your teeth when you’re poor?”
The focus will be on navigating NHS dental services, understanding eligibility for help with health costs, exploring options like dental schools or community dental services, and considering phased treatment plans or more basic, functional restorative care that might be more financially accessible than high-end cosmetic solutions. This section aims to provide practical information and potential pathways for individuals facing dental issues with limited financial resources in the UK.
Do Over 60s Get Free Dental Treatment That Could Cover Tooth Replacement?
The question “Do over 60s get free dental treatment that could cover tooth replacement?” in the UK often stems from a misunderstanding of NHS dental charging policies. While there are certain groups exempt from NHS dental charges, simply being over the age of 60 does not automatically grant free NHS dental treatment for all procedures, especially not for complex tooth replacement options like dental implants or extensive cosmetic bridgework.
NHS dental treatment is categorised into bands, and patients typically pay a set fee for their course of treatment unless they qualify for an exemption. Exemptions from NHS dental charges are primarily based on income-related benefits or specific circumstances, not solely on age once past 60. For example, individuals receiving benefits like the Guarantee Credit part of Pension Credit, Income Support, income-based Jobseeker’s Allowance, or income-related Employment and Support Allowance may be entitled to free NHS dental treatment. Some individuals may also qualify for partial help with NHS costs through the NHS Low Income Scheme (LIS) by filling out an HC1 form.
So, while someone over 60 might also be receiving one of these qualifying benefits (like Pension Credit Guarantee Credit), it’s the benefit that grants the exemption, not their age per se. When it comes to “tooth replacement” on the NHS, the options provided are typically those considered clinically necessary and cost-effective from an NHS perspective. This usually means dentures or, in some cases, basic conventional bridges if criteria are met. As discussed previously, dental implants are rarely available on the NHS except in very specific clinical circumstances (e.g., severe trauma, congenital absence of teeth, post-oral cancer surgery). Therefore, even if an individual over 60 qualifies for free NHS dental treatment due to their benefit status, this entitlement would typically cover standard NHS-provided tooth replacement options (like dentures), not automatically extend to high-cost treatments like implants unless they meet the very strict separate NHS criteria for implant funding. It’s always best to check current NHS England (or a respective devolved nation’s) guidelines and discuss eligibility with an NHS dentist.
What Are the Options if Your Teeth Are Rotting and You Can’t Afford to Fix It in the UK?
Facing a situation where “your teeth are rotting and you can’t afford to fix it in the UK” is incredibly distressing and can have a significant impact on health, well-being, and confidence. The immediate priority in such cases should be to seek advice from an NHS dentist about essential treatments to address pain, infection, and prevent further deterioration. Even if comprehensive restorative work seems unaffordable, an NHS dentist can assess the situation, provide emergency care if needed (like extractions to remove sources of infection or pain), and discuss what essential treatments fall within NHS bands that you might be able to manage or for which you might get help with costs.
If you are on a low income, you should inquire about the NHS Low Income Scheme (LIS) by completing an HC1 form. This scheme can help with the cost of NHS dental treatment, potentially making essential care more accessible. Depending on your assessment, you might qualify for full or partial help.
Another avenue to explore for potentially reduced-cost treatment is dental schools or university dental hospitals. These institutions often have clinics where dental students, under the close supervision of experienced qualified dentists, provide treatment. While waiting lists can sometimes be long, and treatment may take more appointments, the costs are often significantly lower than private practice for a range of procedures.
Community Dental Services (CDS) are another part of the NHS dental framework. They primarily provide care for patients who may have difficulty accessing treatment in a general dental practice, such as those with special needs, significant medical complexities, or severe dental anxiety. While not a route for generally “affordable” care for everyone, they can be a crucial service for eligible individuals.
In some limited cases, dental charities might exist that offer support, but these are often very specific in their remit and capacity. The most important first step is to not let fear of cost prevent you from seeking an initial assessment with an NHS dentist. They can diagnose the extent of the problem, offer advice on immediate management, explain available NHS treatment options, and guide you on how to apply for help with costs if you might be eligible. While complex cosmetic “fixes” might be out of reach without funds, addressing the “rotting” aspect to secure oral health is the primary goal the NHS aims to support.
Can You Get Teeth Replaced for Free or Fix Your Teeth When You’re Poor?
The challenging questions, “Can you get teeth replaced for free?” or “How to fix your teeth when you’re poor?” resonate with many individuals facing financial hardship and dental issues in the UK. The straightforward answer is that completely “free” comprehensive tooth replacement, especially with advanced options like dental implants or extensive cosmetic bridgework, is generally not available to everyone simply based on low income.
However, the NHS system is designed to ensure that everyone has access to clinically necessary dental care, and there are provisions to help those on low incomes with the associated costs. As previously mentioned, eligibility for free NHS dental treatment (or help with costs) is primarily tied to receiving certain income-related benefits (e.g., Pension Credit Guarantee Credit, Income Support, income-based Jobseeker’s Allowance, Universal Credit if meeting specific criteria) or through successful application to the NHS Low Income Scheme (LIS via form HC1). If you qualify, this will cover the cost of NHS-banded treatments, which can include basic tooth replacement options like dentures or, in some circumstances, conventional bridges if deemed clinically necessary by your NHS dentist.
However, it’s crucial to reiterate the limited NHS provision for complex treatments like dental implants. These are typically only funded by the NHS in very specific, often severe, clinical cases (e.g., major trauma, congenital issues, post-cancer reconstruction) and not for routine tooth loss. So, while you might get essential treatment and basic replacements “for free” (or at a reduced cost) if you qualify for help, this doesn’t usually extend to the most advanced or aesthetically driven solutions.
For those who are “poor” but don’t qualify for full exemption, the NHS Low Income Scheme can still offer partial help. Exploring options like dental schools for reduced-cost treatment by supervised students, or seeking advice from an NHS dentist about the most cost-effective, clinically sound basic restorative care (e.g., fillings, extractions to manage pain and infection, and then simple dentures) is a practical approach. The goal of the NHS is to secure oral health and provide functional solutions, and while it may not always be the “fix” one ideally desires aesthetically, it provides a crucial safety net.
Frequently Asked Questions About ‘implant procedure’
What Are the Key Stages of the Process for Dental Implants?
The “process for dental implants” is a meticulously planned, multi-stage journey. The first key stage is the Pre-operative Assessment, involving exams, medical history review, and diagnostic imaging (X-rays, CBCT scans) for personalized treatment planning. The second stage, if needed, is Bone Grafting to ensure sufficient bone volume; this requires months of healing. The third stage is Having the Implant Put In – surgical placement of the titanium post, followed by several months for osseointegration (implant fusing with jawbone). The fourth and final key stage is Restorative Treatment: an abutment is attached, and then the custom-made crown, bridge, or denture is fitted, completing your new tooth/teeth.
How Painful Are Dental Implants, or Getting a Single Tooth Implant?
Most patients find discomfort from dental implants surprisingly manageable, often less than a tooth extraction. “Getting a single tooth implant” or multiple should be pain-free during surgery due to local anesthesia. Sedation options (oral, IV) are available for anxiety. Post-surgery, expect some discomfort, swelling, and bruising, typically controlled with over-the-counter pain relievers (e.g., ibuprofen) and ice packs. Significant discomfort usually subsides within a few days to a week. Following post-op instructions is key to minimizing pain.
How Long Does it Take to Recover From Dental Implant Surgery?
Recovery has two phases. The initial recovery (swelling, mild discomfort) lasts about a few days to one or two weeks. The more significant phase is osseointegration, where the implant fuses with the jawbone. This crucial, silent healing period typically takes 3 to 6 months, sometimes longer, depending on bone quality and health. During osseointegration, you won’t feel active “recovery” symptoms. Adhering to post-op care (soft diet, hygiene, no smoking) is vital for both phases.
What Are the Potential Downsides, Long-Term Side Effects, and Risks of Dental Implants?
Potential downsides include cost (higher upfront), a lengthy treatment timeline, and the surgical nature carrying risks like infection, bleeding, or rare nerve damage. Though uncommon (less than 5% failure rate), implant failure (non-integration or later loosening) can occur. A significant long-term risk is peri-implantitis (inflammation/infection around the implant, like gum disease), often due to poor hygiene or smoking, which can lead to bone loss and failure. Mechanical issues (component fracture/loosening) or rare allergic reactions are also possible. Contraindications include uncontrolled diseases, heavy smoking, or insufficient bone not amenable to grafting.
How Soon After a Tooth Extraction Can an Implant Be Done?
Timing varies. Immediate Implant Placement occurs on the same day as extraction, suitable if the site is infection-free with good bone. Early Implant Placement happens a few weeks to 2-3 months post-extraction, allowing initial soft tissue healing. Delayed Implant Placement involves waiting 4-6 months or longer for more complete socket healing and bone fill, often chosen after significant infection, bone loss, or if extensive grafting is needed. Your dentist determines the best timing based on a thorough clinical evaluation and imaging.









![Dental-Implants-NHS-e1747325783549-1024×915[1] Dental-Implants-NHS-e1747325783549-1024x915[1]](https://dentale-albania.com/wp-content/uploads/elementor/thumbs/Dental-Implants-NHS-e1747325783549-1024x9151-1-r5xyg5ea74oh73k9z5uv5amgw2c45uxhewp2r8hqqo.webp)